Abstract
The risk stratification of B-acute lymphoblastic leukemia (B-ALL) is based on clinical and biological factors. However, B-ALL has significant biological and clinical heterogeneity and 50% of B-ALL patients do not have defined prognostic markers. In this sense, the identification of new prognostic biomarkers is necessary. Considering different cohorts of childhood B-ALL patients, gene (DPP4/CD38/ENTPD1/NT5E) and protein (CD38/CD39/CD73) expressions of ectonucleotidases were analyzed in silico and ex vivo and the association with prognosis was established. In univariate analyses, expression of NT5E was significantly associated with worse progression-free survival (PFS) in bone marrow (BM) samples. In multivariate analyses, Kaplan–Meier analysis, and log-rank test, higher NT5E expression predicted unfavorable PFS in BM samples. Considering minimal residual disease (MRD), higher levels of cellularity were associated with the high NT5E expression at day 8 of induction therapy. In addition, we observed that white blood cells (WBC) of childhood B-ALL patients had more CD38 compared to the same cell population of healthy donors (HD). In fact, MRD > 0.1% patients had higher CD38 protein expression on WBC in comparison to HD. Noteworthy, we observed higher CD38 expression on WBC than blasts in MRD > 0.1% patients. We suggest that NT5E gene and CD38 protein expression, of the ectonucleotidases family, could provide interesting prognostic biomarkers for childhood B-ALL.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute lymphoblastic leukemia (ALL) is a hematopoietic malignancy resulting from clonal proliferation and accumulation of cells displaying cellular markers associated with the early stages of lymphoid maturation [1]. B-acute lymphoblastic leukemia (B-ALL), derived from B-cell progenitors, is the most common ALL subtype and is characterized by significant biological and clinical heterogeneity [2, 3]. B-ALL is one of the top leading causes of malignancy-related death of children and adolescents [4]; however, refined treatment regimens result in cure rates reaching 80% [5, 6].
Risk stratification of childhood B-ALL is based on clinical and biological factors including age at diagnosis, initial white blood cell (WBC) count, cytogenetics characteristics within the leukemic blast population, the rapidity of early treatment response assessed by minimal residual disease (MRD), and involvement of the central nervous system and testes [6, 7]. MRD assessment is the most important follow-up for all leukemias; generally, biomarkers are considered candidates if their presence correlates negatively or positively of MRD [8, 9]. Some abnormalities in chromosome number or structure are prognostic markers but are absent in many ALL patients and, in a significant number of cases, are not conclusive [10]. Therefore, despite biomedical research efforts, approximately 50% of ALL patients lack defined genetic hallmarks of biological or clinical relevance [11, 12]. For this reason, genetic biomarkers currently have limited value as prognostic markers for childhood B-ALL.
Deregulated gene expression of several key cellular pathways has been suggested as a useful tool to refine prognosis and identify novel therapeutic targets in ALL [13]. Among all of B-ALL biomarkers, the family of genes involved in purinergic signaling that encodes ectonucleotidases has received little attention from the field. Purinergic signaling involves purines (ATP and its hydrolysis products) and pyrimidines (mainly UTP) which act as extracellular ligands for the widely expressed purinergic receptors, P2 (activated by nucleoside tri-/diphosphates among others) and P1 (activated by adenosine and others) [14,15,16]. Extracellular levels of ATP and adenosine (ADO) are controlled by extracellular ectonucleotidases: CD39 (ENTPD1), CD38 (CD38), CD73 (NT5E), and CD26 (DPP4), among others. The conversion of ATP to ADP and then to AMP is predominantly catalyzed by CD39, while CD73 catalyzes the conversion of AMP to ADO, this being the canonical pathway of ADO production [17,18,19]. ATP and ADO can participate in creating favorable tumor microenvironmental conditions, which promote tumor growth and survival, while suppressing the host’s immune system responses [20]. Positive regulation of ENTPD1, NT5E, and DPP4 genes is linked to poor prognosis in many cancers, including B-cell chronic lymphocytic leukemia, gastric carcinoma, rectal adenocarcinoma, and urothelial carcinoma [21,22,23,24]. On the other hand, positive regulation of the CD38 gene is associated with good prognosis in adult acute leukemias [25]. Association between ectonucleotidases expression level and clinical outcomes has been reported in other cancers, but not in childhood B-ALL. In this study, we evaluated mRNA expression of four genes involved in purinergic signaling, DPP4, CD38, ENTPD1, NT5E, corresponding to four ectonucleotidases, CD26, CD38, CD39, and CD73, respectively, and their association with prognosis in childhood B-ALL patients using data from the Therapeutically Applicable Research to Generate Effective Treatment (TARGET) Program. In addition, we evaluated the protein expression of CD38, CD39, and CD73 in cell populations at the moment of diagnosis, in a cohort of childhood B-ALL patients from a university hospital in the Brazilian city of Porto Alegre.
Materials and methods
The mRNA expression of the DPP4, CD38, ENTPD1, NT5E genes was analyzed in the TARGET childhood B-ALL cohort and the protein expression of CD38, CD39, and CD73 in cell populations at the time of diagnosis was analyzed in the Hospital de Clínicas de Porto Alegre (HCPA) childhood B-ALL cohort.
TARGET childhood B-ALL cohort
The results used were generated from publicly available data by the Therapeutically Applicable Research to Generate Effective Treatments (https://ocg.cancer.gov/programs/target) initiative, phs000218. Data can be accessed at https://portal.gdc.cancer.gov/projects. According to the publication guidelines, a limited dataset (less than 5 genes) can be used for publication without restriction or limitation (https://ocg.cancer.gov/programs/target/target-publication-guidelines).
We used the datasets corresponding to TARGET ALL Pilot Project and TARGET ALL Expansion (Phase II) Project. Both projects have produced comprehensive genomic profiles (molecular characterization and other sequencing data) and clinical data, such as MRD status by flow cytometry at days 8 and 29 of induction therapy, from B-cell ALL patient cases. Each fully characterized TARGET ALL case includes data from nucleic acid samples extracted from peripheral blood (PB) or bone marrow (BM) tissues. PB-BM samples are not necessarily obtained from the same patient (independent analysis).
Tissue and clinical data used from TARGET ALL Pilot and TARGET ALL Phase II project was obtained from patients enrolled on studies managed by the Children’s Oncology Group (COG). In both projects, patients’ samples for full characterization were chosen based on the same criteria and can be accessed at https://ocg.cancer.gov/programs/target/projects/acute-lymphoblastic-leukemia. The nucleic acid sample processing and RNA isolation were performed with Invitrogen TRIzol (http://ocg.cancer.gov/sites/default/files/RNA_Trizol_ALL.pdf) and for gene expression data generation protocol, Gene Chip® Human Genome U133 Plus 2.0 Array (Affymetrix) was used (https://ocg.cancer.gov/programs/target/target-methods#396, https://ocg.cancer.gov/programs/target/target-methods#3222).
HCPA childhood B-ALL cohort
Patients and controls
PB samples of childhood B-ALL patients and healthy donors were collected. This study included the cohort of 15 newly diagnosed childhood B-ALL patients (ages 1–17 years old, median age 7.7 years, where 53% are female and 47% male) and 10 healthy donors (ages 1–17 years old, median age 7.5 years, where 20% are female and 80% male). Diagnosis and MRD status on day 15 of induction therapy of childhood B-ALL, based on immunophenotypic antigen expression accordingly to EuroFlow protocols [26], were performed by the Serviço de Diagnóstico Laboratorial do Hospital de Clínicas de Porto Alegre (HCPA). Patients received treatment according to the BFM 2009 protocol conducted by the Serviço de Hematologia Clínica and Serviço de Oncologia Pediátrica, HCPA. The Institutional Ethics Review Board has approved the study and informed consent was obtained from patients and healthy donors, their parents, or guardians in accordance with the Declaration of Helsinki (Project no.: 2018–0401; CAAE no.: 93973218110015327).
Flow cytometry assays
In addition to diagnostic and MRD status antibodies accordingly to EuroFlow protocols [26], the following mouse anti-human monoclonal antibodies (mAbs) were used for each patient in this study: CD38 FITC, clone HIT2; CD39 APC, clone TU66; CD45 V500, clone HI30; and CD73 PE, clone AD2 (all from BD Bioscience, San Diego, CA). Antibodies were pipetted in their respective validated volumes in 100µL of pure sample. Then, they were incubated for 30 min at room temperature in the dark. Erythrocyte lysis was performed after staining the samples, using 2-mL FACS Lyse Solution (BD Bioscience) and incubated for 10 min at room temperature in the dark. Then, centrifugation was performed for 5 min at 540 g, discarding the supernatant, and resuspending the cell pellet. Afterwards, 2 mL PBS (BD Bioscience) was used and a centrifugation for 5 min at 540 g was performed. The supernatant was discarded, and the cell pellet resuspended with 250µL of azide-free PBS assessed in FACSCanto II Flow Cytometer (BD-Becton Dickinson, San Jose, CA, USA), which had been set-up and calibrated following the standardized EuroFlow guidelines [26]. Throughout the study, the flow cytometer was subjected to daily quality assessment using fluorescent beads of the same lot (Sphero Rainbow Calibration Particles, Spherotech, Lake Forest, IL, USA) and the EuroFlow guidelines for monitoring instrument performance, in order to ensure the reproducibility of the obtained staining [26]. For data analysis, the Infinicyt® software version 1.7 was used (Cytognos, Salamanca, Spain).
Gating strategies and cell population definitions
The information about the gating strategies and cell population definitions can be found in Fig. 5a. After exclusion of debris and dead cells based on forward and side scatter (FSC/SSC), three distinct cell populations were identified using CD45 expression and FSC/SSC properties to analyze CD38, CD39 and CD73: \({SSC}^{low/int}/{CD45}^{dim}\) cells, \({SSC}^{all}/{CD45}^{dim/bright}\) cells, and \({SSC}^{low}/{CD45}^{bright}+{SSC}^{high}/{CD45}^{dim/bright}\) cells. The protein expressions were quantified as the mean fluorescence intensity (MFI).
Statistical analysis
In silico analysis (TARGET childhood B-ALL cohort)
The mRNA expression levels were separated into low- and high-expression, designated using the gene distribution’s median expression value as a cut-off. Gene expression value distribution graphs were generated using GraphPad Prism 7 (GraphPad Software, Inc.—San Diego, CA, USA). Univariate Cox analysis was used to select the related variables. Multivariate Cox analysis was applied to the influence of gene expression on the overall survival (OS) and progression-free survival (PFS) of patients. Kaplan–Meier analysis was performed to estimate the survival and recurrence curves of the different subgroups and log-rank test was used to compare the curves. Odds ratio was used to compare the probability of an event occurring between groups.
Ex vivo analysis (HCPA childhood B-ALL cohort)
Two-tailed independent Student’s t-tests were performed for comparison of two groups. For the analysis of three groups or more, one-way ANOVA (Turkey’s HSD post hoc test) or two-way ANOVA (Bonferroni’s post hoc test) was used.
The statistical analyses were performed using the SPSS software, 19.0 version (SPSS Inc., Chicago, IL) and R statistical software (version 3.4.1) [27]. All p-values were two sided. A p-value less than 0.05 was considered statistically significant (*p < 0.05, **p < 0.01, ***p < 0.001).
Results
TARGET childhood B-ALL cohort—relation of ENTPD1, CD38, NT5E, and DPP4 expression to selected clinicopathological features of childhood B-ALL and survival outcome
The TARGET childhood B-ALL cohort consisted of 289 patients, with 198 BM and 91 PB samples. The clinical characteristics, including CNS status and survival time, are shown in Table 1.
Table 2 displays the associations between the mRNA expression values of ectonucleotidases family genes and survival outcomes with univariate Cox regression analysis. An association between the expression of NT5E with worse PFS in BM (HR = 1.38, 95% CI: 1.14–1.66, p = 0.0006) samples was found.
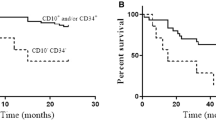
After univariate Cox regression analysis, patients were categorized into low- and high-expression groups (Fig. 1). All genes were expressed in both samples and NT5E (p = 0.0005) and DPP4 (p = 0.0180) genes showed significantly higher median expression in PB than in BM. As NT5E was the only gene to present a statistically significant difference in univariate Cox regression analysis, we compared the survival in low- vs high-expression of NT5E (PFS, Fig. 2; and OS, Fig. 3). In agreement with the univariate analysis, it was observed that the NT5E high-expression group had worse PFS (p = 0.0022, Fig. 2a) compared to the low-expression group in BM samples, whereas PFS was not influenced by NT5E expression levels on PB (p = 0.18, Fig. 2b). In addition, the NT5E expression levels in BM and PB did not influence OS (Fig. 3 a–b).
mRNA expression level of genes in BM (N = 198) and PB (N = 91) samples. mRNA expression levels were divided by the distribution’s median. For each gene, patients were labeled as high-expression (red) for expression values above median (values > 50%), while patients were labeled as low-expression (blue) for expression values below median (values ≤ 50%). *p < 0.05, ***p < 0.001. BM, bone marrow; PB, peripheral blood
Kaplan–Meier curves of childhood B-ALL patients stratified by NT5E (a–b) expression levels. Progression-free survival curve of patients in discovery set with high versus low NT5E expression levels in bone marrow (a) and peripheral blood (b) samples. p-values for significance of difference between high and low expression were calculated using the log-rank test
Kaplan–Meier curves of childhood B-ALL patients stratified by NT5E (a–b) expression levels. Overall survival curve of patients in discovery set with high versus low NT5E expression levels in bone marrow (a) and peripheral blood (b) samples. p-values for significance of difference between high and low expression were calculated using the log-rank test
Since NT5E gene was the only one that showed significant statistical differences in the previous analyses (p-value < 0.05), univariate Cox regression analysis, Kaplan–Meier analysis, and log-rank test, we explored the association between NT5E and survival outcome in a multivariate context (Table 3). In multivariate Cox regression analysis, after adjusting for clinical factors, NT5E remained an independent poor prognostic indicator for PFS in BM samples. Higher NT5E expression level was associated with shorter PFS in BM samples with an adjusted hazard ratio of 1.75 (95% CI: 1.22–2.51, p = 0.002).
Considering the prognosis potential of NT5E, we attempted identifying whether the expression of this gene is associated with MRD. Figure 4 illustrates the prevalence of MRD on days 8 and 29 of induction therapy in two groups of patients with low and high levels of NT5E expression in BM samples, respectively. On day 8, MRD > 0.1% was detected in 43 from 65 patients with low expression of this gene versus 51 from 65 with high expression. On day 29, these prevalence rates were 15 out of 65 versus 16 out of 65 patients, respectively. Higher levels of cellularity were associated with the high NT5E subset at day 8. Therefore, patients with a feature typically associated with a dismal outcome (MRD > 0.1%) are 18.6% more likely to have high NT5E expression than low NT5E expression at day 8. Moreover, the NT5E low-expression group, at day 8, had approximately 1.6-fold more patients with MRD < 0.1% when compared to the high-expression group: 22 out of 65 in NT5E low expression versus 14 out of 65 in NT5E high expression. On the other hand, at day 29, patients had similar MRD probability reinforcing the relevance of NT5E expression measurement in the first MRD analysis.
Prevalence of MRD (% of cellularity) at days 8 and 29 of induction therapy in two groups of patients with low and high expression of NT5E in BM samples. From an initial cohort of 198 patients with BM samples, only 130 patients, who had MRD data on both days, were selected. MRD, minimal residual disease
HCPA childhood B-ALL cohort - High CD38 expression associated with high leukemic and cell maturation stage dependence
To further explore possible purinergic biomarkers, we used an ex vivo approach that permits immediate and short-term evaluation of a particular effect on cells and their components, in this case the protein expression of ectonucleotidases (CD38, CD39, and CD73) in different PB cell populations of childhood B-ALL patients at the time of diagnosis.
First, we compared \({SSC}^{low}/{CD45}^{bright}+{SSC}^{high}/{CD45}^{dim/bright}\) cells (Fig. 5a) from healthy donors and childhood B-ALL patients (excluding the blasts’ region on dot plots) and compared the expressions of CD38, CD39, and CD73 (Fig. 5b–d). Cells from newly diagnosed childhood B-ALL patients had a significantly higher CD38 expression when compared to those from healthy donors (p = 0.0429, Fig. 5b). There was no significant difference on CD39 or CD73 expression in childhood B-ALL patients when compared to healthy donors in this cell population (p = 0.4212, Fig. 5c; p = 0.9337, Fig. 5d, respectively). Furthermore, we aimed on identifying if the expressions of CD38, CD39, and CD73 have the same gating strategy \(({SSC}^{low}/{CD45}^{bright}+{SSC}^{high}/{CD45}^{dim/bright}\) cells) are associated with MRD, stratifying the childhood B-ALL patients into MRD < 0.1% and MRD > 0.1% (Fig. 5e–g). Nine (60%) childhood B-ALL patients had MRD > 0.1%, and six (40%) patients had MRD < 0.1%. A significant difference was found on CD38 expression when we compared MRD > 0.1% patients to healthy donors (p < 0.05, Fig. 5e). Again, CD39 and CD73 subgroups were not significantly different (Fig. 5f and Fig. 5g).
Gating strategies and cell population definitions (a) and representative plot of CD38 (b and e), CD39 (c and f), and CD73 (d and g) expression on \({\mathrm{SSC}}^{\mathrm{low}}\)/\({\mathrm{CD}45}^{\mathrm{bright}}\)+\({\mathrm{SSC}}^{\mathrm{high}}\)/\({\mathrm{CD}45}^{\mathrm{dim}/\mathrm{bright}}\) cells from HD vs. B-ALL patients (b–d)/B-ALL patients categorized as MRD < 0.1% or MRD > 0.1% (e–g). p values were calculated with non-parametric Mann–Whitney U-test (b–d) and one-way ANOVA test (e–g). *p < 0.05. B-ALL, childhood B acute lymphoblastic leukemia; HD, healthy donors; MRD, minimal residual disease; MFI, mean fluorescence intensity
We then compared the expression of CD38, CD39, and CD73 first gating white blood cells and blasts second gating WBC excluding blasts’ region (\({SSC}^{low}/{CD45}^{bright}+{SSC}^{high}/{CD45}^{dim/bright})\); and finally gating only on blasts’ region \(({SSC}^{low/int}/{CD45}^{dim})\) in childhood B-ALL patients. No significant difference was found in protein expression when comparing these cell populations among cell groups (Fig. 6a–c). However, when we stratified the childhood B-ALL patients into MRD < 0.1% and MRD > 0.1% and compared the groups (Fig. 6d–f), a significant difference was found in CD38 expression between WBC and cells from the blasts’ region in MRD > 0.1% patients (p < 0.05, Fig. 6d).
Representative summary plot of CD38 (a and d), CD39 (b and e), and CD73 (c and f) expression on \({SSC}^{all}/{CD45}^{dim/bright}, { SSC}^{low}\)/\({CD45}^{bright}\)+\({SSC}^{high}\)/\({CD45}^{dim/bright}\), and \({SSC}^{low/int}/{CD45}^{dim}\) cells from B-ALL patients (a–c)/B-ALL patients categorized as MRD < 0.1% or MRD > 0.1% (d–f). p values were obtained with one-way ANOVA (a–c) and two-way ANOVA (d–f) tests. *p < 0.05. MRD, minimal residual disease; MFI, mean fluorescence intensity
Discussion
The purinergic system is a signaling pathway composed of nucleotides/nucleosides (mainly adenosine triphosphate (ATP), and adenosine (ADO)) and their corresponding membrane receptors, presenting defined transduction mechanisms. The conversion of ATP to adenosine monophosphate (AMP) is predominantly catalyzed by CD39 (ectonucleoside thiphosphate diphosphohydrolase-1, ENTPD1), while CD73 (ecto-5′-nucleotidase, NT5E) catalyzes the conversion of AMP to ADO, this being the canonical pathway to produce ADO. There is also a non-canonical pathway for the production of ADO, where NAD + is converted by CD38 (NAD glycohydrolase, CD38) in ADP ribose (ADPR) and then by CD203a into AMP, which is metabolized in ADO by CD73. The CD26 protein (dipeptidyl peptidase-4, DPP4) complexes with adenosine deaminase (ADA) to control ADO concentration in the extracellular space [17, 19, 28]. The dynamic equilibrium between ATP and ADO, which is accomplished by the presence and regulatory activity of ectonucleotidases, is one of the many factors associated with the pro-carcinogenic or anti-tumoral fate [29]. Extracellular ATP has been described as a “find me” signal that promotes innate and adaptive immune response by attracting immune cells; ADO, on the other hand, acts as an immunosuppressive molecule redirecting the phenotype of infiltrated immune to disrupt the antitumor attack [30, 31]. In the present study, we used mRNA data to explore the clinical significance of ectonucleotidases genes expression in silico and ectonucleotidases protein expression ex vivo, in order to explore possible prognostic biomarkers for patients with childhood B-ALL.
In the current study, NT5E gene expression was associated with worse progression-free survival in bone marrow samples from childhood B-ALL patients. Among the four genes involved in purinergic signaling, DPP4, CD38, ENTPD1, and NT5E, only NT5E showed a robust association between high expression at diagnosis and worse progression-free survival (PFS) in bone marrow samples in childhood B-ALL patients. There is evidence from a number of articles suggesting that NT5E expression may be important in enhancing the invasive and metastatic properties of some cancer cells [32]. It has been observed, in The Cancer Genome Atlas (TCGA) dataset analysis, that there is an association between high NT5E expression and worse 5-year overall survival. In addition, high NT5E expression and higher regulatory T cell (Treg) signature have been correlated in patients with renal cell carcinoma (RCC) [33]. In patients with papillary thyroid carcinoma (PTC), high expression of NT5E mRNA was associated with unfavorable clinicopathologic characteristics, the abundance of Tregs and dendritic cells, depletion of natural killer (NK) cells, high expression of immune checkpoint genes, and epithelial-to-mesenchymal transition-related genes in TCGA dataset [34]. Although evidence from a series of articles correlates NT5E expression and prognosis, this is the first study to suggest that NT5E expression in bone marrow samples has a significant prognostic impact in childhood B-ALL patients. It is noteworthy that genes may show differences in expression between bone marrow and peripheral blood and, according to Sakhinia et al., this difference in expression may be due to the particular involvement of these genes in the pathobiology of leukemia [35].
It has been postulated that alterations in gene expression may be associated with the presence of MRD, having a significant prognostic impact [36]. Our study analyzed the expression of the NT5E gene in childhood B-ALL patients (TARGET cohort) classified as MRD < 0.1% and MRD > 0.1%, with MRD > 0.1% being a higher risk classification compared to MRD < 0.1%. Notably, greater levels of MRD were associated with high expression of NT5E on day 8 and, consequently, associated with a worse response to treatment. Therefore, we suggest the NT5E gene as a possible prognostic biomarker, particularly regarding progression-free survival, in childhood B-ALL.
In the second part of this study, we focused our efforts on the ex vivo analysis of ectonucleotidases protein expression on peripheral blood from childhood B-ALL patients. Noteworthy, we have analyzed CD38, CD39, and CD73 expression in the same sample, equipment, software, and quality control from the clinical analysis routine. In diagnosed childhood B-ALL patients, we observed that WBC cells (excluding blasts) had similar CD73 expression than healthy donors. Moreover, the expression of this protein was not different in any subset of cells even considering MRD analysis. In fact, in a prospective and larger study, it was observed that the long-term event-free survival was not dependent of CD73 expression in children with ALL [37]. On the other hand, CD73 protein expression, in MRD-positive leukemic B cells, has been reported to be six times greater than in MRD-negative patients’ leukemic B-cells, leading CD73 to be recommended as an optional MRD marker for B-ALL patients using flow cytometry [38]. It is important to note that Wieten et al. measured CD73 in mononuclear cells from bone marrow of children with ALL ageing 1–18 years, while Wang et al. analyzed the CD73 expression on leukemic B cells of patients averaging 46 years. Factors such cell population, type of sample (PB or BM), and age of the cohort may explain these predictive differences. In our conditions, at the protein level, CD73 was not considered an independent prognostic biomarker.
The reports regarding CD38 expression and the association with progression of ALL are scarce, and even more in childhood B-ALL. Firstly, we observed greater CD38 expression on non-malignant cells of B-ALL patients in relation to healthy donors. Furthermore, we identified that this higher expression was significant only in patients who presented a poorer outcome (MRD > 0.1). It has been reported in other studies that increased CD38 expression in blasts is associated with favorable prognosis in adult acute lymphoblastic leukemia (ALL) and acute myeloid leukemia (AML) [25]. On the other hand, in childhood ALL, the expression of CD38 on B cells or T cells does not add prognostic significance to either survival or event-free survival [39, 40]. In multiple myeloma, CD38 expression has been described as an adverse prognostic factor, showing high and uniform expression on malignant plasma cells and relatively low expression on lymphoid and myeloid cells [41]. In our findings, the high expression of CD38 in non-malignant cells of MRD > 0.1 patients might be related to the enzymatic activity, producing metabolites of the non-classical adenosinergic pathway (NAD > ADPr > AMP > ADO). Adenosine is a strong immunosuppressive molecule involved in immune escape and canonical and non-canonical adenosinergic enzymes have been associated with worse prognosis in several types of cancer [42, 43].
Despite increasing knowledge about the functions of CD38, there has still been considerable controversy regarding the clinical significance of its expression in hematopoietic malignancies in the blasts’ population and even fewer reports regarding WBC cells. It is also worth mentioning that CD38 expression is a temporal characteristic of the activation state and/or stage of cells’ maturation, and it can be expressed in normal and neoplastic cells [44]. Differently from T-ALL blasts [45], in the conditions of the current work, cells from blasts’ region present lower CD38 expression, considering MRD > 0.1 patients, when compared to non-malignant cells and, therefore, a possible antiCD38-mAb repurposing therapy would have to be carefully evaluated in childhood B-ALL. Therefore, the high protein expression of CD38 on non-malignant cells at diagnosis is related to increased cellularity in MRD and, with worse prognosis. Noteworthy, these patients (MRD > 0.1) had higher CD38 expression in non-malignant cells than blasts. Thus, CD38 is still an open research field as a potential prognostic marker and needs deep evaluation as a potential targeted therapy in childhood B-ALL.
Further progress in the treatments of childhood B-ALL will require optimization of risk allocation to avoid excessive or insufficient treatment of patients, as well as the development of new anti-leukemic agents [46, 47]. The association between the NT5E gene expression and prognosis clearly deserves further investigation; we can also suggest that measurements of NT5E expression in bone marrow samples may assist, in the future, to identify patients with worse prognosis and who are more prone to disease progression. Our study presents CD38 protein expression as a useful independent biomarker that allows prediction of disease outcome, highlighting its relevance not only in blasts but also mainly in immune cells. Future experimental investigations could attempt to understand the mechanisms underlying why higher levels of CD38 in peripheral blood immune cells in childhood B-ALL can be an indicative of worse prognosis. Finally, it is necessary to recognize the limitations of this study such as sample size and reduced number of markers applied ex vivo. Therefore, we suggest that more advanced studies are needed to provide valuable information about the purinergic characteristics in childhood B-ALL patients to allow the pursuit robust prognostic biomarkers and treatment strategies.
Conclusions
In conclusion, of the genes analyzed in this study, only NT5E showed a robust association between high expression at diagnosis and worse progression-free survival in bone marrow samples. In addition, we found that high expression of NT5E was associated with a worse response to treatment in childhood B-ALL patients. However, at protein level, only high expression of CD38 on non-malignant cells at diagnosis was related to a worse prognosis. Further studies are necessary to provide information about the purinergic characteristics in childhood B-ALL patients in order to optimize risk allocation of patients, as well as the development of new anti-leukemic agents.
Data Availability
All data are available upon reasonable request.
References
Carroll W, Loh M, Biondi A, Willman C (2011) Childhood leukemia. 29–62. https://doi.org/10.1007/978-3-642-13781-5
Moorman AV (2016) New and emerging prognostic and predictive genetic biomarkers in B-cell precursor acute lymphoblastic leukemia. Haematologica 101:407–416. https://doi.org/10.3324/haematol.2015.141101
Roberts KG, Mullighan CG (2015) Genomics in acute lymphoblastic leukaemia: insights and treatment implications. Nat Rev Clin Oncol 12:344–357. https://doi.org/10.1038/nrclinonc.2015.38
Zhang X, Rastogi P, Shah B, Zhang L (2017) B lymphoblastic leukemia/lymphoma: new insights into genetics, molecular aberrations, subclassification and targeted therapy. Oncotarget 8:66728–66741. https://doi.org/10.18632/oncotarget.19271
Hann I, Vora A, Richards S et al (2000) Benefit of intensified treatment for all children with acute lymphoblastic leukaemia: results from MRC UKALL XI and MRC ALL97 randomised trials. Leukemia 14:356–363. https://doi.org/10.1038/sj.leu.2401704
Schultz KR, Pullen DJ, Sather HN et al (2007) Risk- and response-based classification of childhood B-precursor acute lymphoblastic leukemia: a combined analysis of prognostic markers from the Pediatric Oncology Group (POG) and Children’s Cancer Group (CCG). Blood 109:926–935. https://doi.org/10.1182/blood-2006-01-024729
Carroll WL, Raetz EA (2012) Clinical and laboratory biology of childhood acute lymphoblastic leukemia. J Pediatr 160:10–18. https://doi.org/10.1016/j.jpeds.2011.08.006
Bartram J, Patel B, Fielding AK (2020) Monitoring MRD in ALL: methodologies, technical aspects and optimal time points for measurement. Semin Hematol 57:142–148. https://doi.org/10.1053/j.seminhematol.2020.06.003
Schuurhuis GJ, Heuser M, Freeman S et al (2018) Minimal/measurable residual disease in AML: a consensus document from the European LeukemiaNet MRD Working Party. Blood 131:1275–1291. https://doi.org/10.1182/blood-2017-09-801498
Garza-Veloz I, Martinez-Fierro ML, Jaime-Perez JC et al (2015) Identification of differentially expressed genes associated with prognosis of B acute lymphoblastic leukemia. Dis Markers 2015:1–11. https://doi.org/10.1155/2015/828145
Bungaro S, Dell’Orto MC, Zangrando A et al (2009) Integration of genomic and gene expression data of childhood ALL without known aberrations identifies subgroups with specific genetic hallmarks. Genes Chromosom Cancer 48:22–38. https://doi.org/10.1002/gcc.20616
Dawson AJ, Yanofsky R, Vallente R et al (2011) Array comparative genomic hybridization and cytogenetic analysis in pediatric acute leukemias. Curr Oncol 18:e210. https://doi.org/10.3747/co.v18i5.770
Yeoh E, Ross ME, Shurtleff SA et al (2002) Classification, subtype discovery, and prediction of outcome in pediatric acute lymphoblastic leukemia by gene expression profiling. Cancer Cell 1:133–143. https://doi.org/10.1016/S1535-6108(02)00032-6
Burnstock G (2007) Purine and pyrimidine receptors. Cell Mol Life Sci 64:1471–1483. https://doi.org/10.1007/s00018-007-6497-0
Careta O, Cuevas E, Muñoz-Esquerre M et al (2019) Imbalance in the expression of genes associated with purinergic signalling in the lung and systemic arteries of COPD patients. Sci Rep 9:1–9. https://doi.org/10.1038/s41598-019-39233-y
Chang CC, Liu CZ, Cleveland RP (2003) Relative importance of CD38 expression over myeloid-associated markers expression in predicting the clinical course of B-CLL patients. Leuk Lymphoma 44:977–982. https://doi.org/10.1080/1042819031000076990
Zimmermann H (1996) Biochemistry, localization and functional roles of ecto-nucleotidases in the nervous system. Prog Neurobiol 49:589–618. https://doi.org/10.1016/0301-0082(96)00026-3
Yegutkin GG, Henttinen T, Samburski SS et al (2002) The evidence for two opposite, ATP-generating and ATP-consuming, extracellular pathways on endothelial and lymphoid cells. Biochem J 367:121–128. https://doi.org/10.1042/BJ20020439
Horenstein AL, Chillemi A, Zaccarello G, et al (2013) A CD38/CD203a/CD73 ectoenzymatic pathway independent of CD39 drives a novel adenosinergic loop in human T lymphocytes. Oncoimmunology 2https://doi.org/10.4161/ONCI.26246
Di Virgilio F, Boeynaems J-M, Robson SC (2009) Extracellular nucleotides as negative modulators of immunity. Curr Opin Pharmacol 9:507–513. https://doi.org/10.1016/j.coph.2009.06.021
Abousamra NK, Salah El-Din M, Hamza Elzahaf E, Esmael ME (2015) Ectonucleoside triphosphate diphosphohydrolase-1 (E-NTPDase1/CD39) as a new prognostic marker in chronic lymphocytic leukemia. Leuk Lymphoma 56:113–119. https://doi.org/10.3109/10428194.2014.907893
Lu X, Chen Y, Feng B et al (2013) Expression and clinical significance of CD73 and hypoxia-inducible factor-1α in gastric carcinoma. World J Gastroenterol 19:1912. https://doi.org/10.3748/WJG.V19.I12.1912
Zhang B, Song B, Wang X et al (2015) The expression and clinical significance of CD73 molecule in human rectal adenocarcinoma. Tumor Biol 36:5459–5466. https://doi.org/10.1007/s13277-015-3212-x
Liang P, Yeh B, Li W et al (2017) DPP4/CD26 overexpression in urothelial carcinoma confers an independent prognostic impact and correlates with intrinsic biological aggressiveness. Oncotarget 8:2995–3008. https://doi.org/10.18632/oncotarget.13820
Keyhani A, Huh YOO, Jendiroba D et al (2000) Increased CD38 expression is associated with favorable prognosis in adult acute leukemia. Leuk Res 24:153–159. https://doi.org/10.1016/S0145-2126(99)00147-2
Kalina T, Flores-Montero J, Van Der Velden VHJ et al (2012) EuroFlow standardization of flow cytometer instrument settings and immunophenotyping protocols. Leukemia 26:1986–2010. https://doi.org/10.1038/leu.2012.122
Therneau TM, Lumley T (2020) Survival analysis; [R package “survival” version 3.1–12]. In: Compr. R Arch. Netw. https://cran.r-project.org/package=survival. Accessed 28 Jul 2020
Iqbal J, Zaidi M (2006) Extracellular NAD+ metabolism modulates osteoclastogenesis. Biochem Biophys Res Commun 349:533–539. https://doi.org/10.1016/j.bbrc.2006.08.108
Campos-Contreras ADR, Díaz-Muñoz M, Vázquez-Cuevas FG (2020) Purinergic signaling in the hallmarks of cancer. Cells 9:1612. https://doi.org/10.3390/cells9071612
Allard B, Beavis PA, Darcy PK, Stagg J (2016) Immunosuppressive activities of adenosine in cancer. Curr Opin Pharmacol 29:7–16. https://doi.org/10.1016/j.coph.2016.04.001
de Andrade MP, Coutinho-Silva R, Savio LEB (2017) Multifaceted effects of extracellular adenosine triphosphate and adenosine in the tumor–host interaction and therapeutic perspectives. Front Immunol 8:1526. https://doi.org/10.3389/fimmu.2017.01526
Jiang T, Xu X, Qiao M et al (2018) (2018) Comprehensive evaluation of NT5E/CD73 expression and its prognostic significance in distinct types of cancers. BMC Cancer 181(18):1–10. https://doi.org/10.1186/S12885-018-4073-7
Tripathi A, Lin E, Xie W, et al (2020) Prognostic significance and immune correlates of CD73 expression in renal cell carcinoma. J Immunother Cancer 8https://doi.org/10.1136/jitc-2020-001467
Jeong YM, Cho H, Kim T-M et al (2020) CD73 Overexpression promotes progression and recurrence of papillary thyroid carcinoma. Cancers (Basel) 12:3042. https://doi.org/10.3390/cancers12103042
Sakhinia E, Farahangpour M, Tholouli E et al (2006) Comparison of gene-expression profiles in parallel bone marrow and peripheral blood samples in acute myeloid leukaemia by real-time polymerase chain reaction. J Clin Pathol 59:1059–1065. https://doi.org/10.1136/jcp.2005.031161
Flotho C, Coustan-Smith E, Pei D et al (2006) Genes contributing to minimal residual disease in childhood acute lymphoblastic leukemia: prognostic significance of CASP8AP2. Blood 108:1050–1057. https://doi.org/10.1182/blood-2006-01-0322
Wieten E, van der Linden-Schrever MBE, Sonneveld E et al (2011) CD73 (5′-nucleotidase) expression has no prognostic value in children with acute lymphoblastic leukemia. Leukemia. https://doi.org/10.1038/leu.2011.174
Wang W, Gao L, Li Y et al (2016) The application of CD73 in minimal residual disease monitoring using flow cytometry in B-cell acute lymphoblastic leukemia. Leuk Lymphoma 57:1174–1181. https://doi.org/10.3109/10428194.2015.1070153
Koehler M, Behm F, Hancock M, Pui CH (1993) Expression of activation antigens CD38 and CD71 is not clinically important in childhood acute lymphoblastic leukemia. Leukemia 7(1):41–5 (PMID: 8418378)
C L, DY S, XJ X, et al (2020) High CD38 expression in childhood T-cell acute lymphoblastic leukemia is not associated with prognosis. Cancer Biomark 27:277–284https://doi.org/10.3233/CBM-190946
Morandi F, Horenstein AL, Costa F et al (2018) CD38: a target for immunotherapeutic approaches in multiple myeloma. Front Immunol 0:2722. https://doi.org/10.3389/FIMMU.2018.02722
Sek K, Mølck C, Stewart G et al (2018) Targeting adenosine receptor signaling in cancer immunotherapy. Int J Mol Sci 19:3837. https://doi.org/10.3390/ijms19123837
Hammami A, Allard D, Allard B, Stagg J (2019) Targeting the adenosine pathway for cancer immunotherapy. Semin Immunol 42:101304. https://doi.org/10.1016/J.SMIM.2019.101304
Malavasi F, Deaglio S, Funaro A et al (2008) Evolution and function of the ADP ribosyl cyclase/CD38 gene family in physiology and pathology. Physiol Rev 88:841–886. https://doi.org/10.1152/physrev.00035.2007
Tembhare R, Sriram H, Khanka T et al (2020) Flow cytometric evaluation of CD38 expression levels in the newly diagnosed T-cell acute lymphoblastic leukemia and the effect of chemotherapy on its expression in measurable residual disease, refractory disease and relapsed disease: an implication for anti-CD38 immunotherapy. J Immunother Cancer 8:630. https://doi.org/10.1136/jitc-2020-000630
Silverman LB, Sallan SE (2003) Newly diagnosed childhood acute lymphoblastic leukemia: update on prognostic factors and treatment. Curr Opin Hematol 10:290–296. https://doi.org/10.1097/00062752-200307000-00007
Pui C-H, Campana D, Evans WE (2001) Childhood acute lymphoblastic leukaemia – current status and future perspectives. Lancet Oncol 2:597–607. https://doi.org/10.1016/S1470-2045(01)00516-2
Funding
This study was supported by CNPq (PQ no. 302879/2017–0, AMO Battastini grant), FAPERGS (FAPERGS/PQG grant no. 19/2551–0001783-9; ARD grant no. 19/2551–0001269-1 and PRONEX no. 16–2551-0000467–6), and INCT/CNPq/CAPES/ FAPERGS grant no. 465671/2014–4. Fundo de Incentivo a Pesquisa do Hospital de Clínicas de Porto Alegre (project no.: 2018–0401; CAAE no.: 93973218110015327). This study was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior-Brasil (CAPES)—Finance Code 001.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Vitória Brum da Silva Nunes, Camila Kehl Dias, Marco Antônio De Bastiani, and Fabrício Figueiró. The first draft of the manuscript was written by Vitória Brum da Silva Nunes and all authors commented on later versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
The study was conducted in accordance with the 1964 Helsinki Declaration, and the protocol was approved by the Ethics Committee of the Hospital de Clínicas de Porto Alegre (Project number: 2018–0401; CAAE number: 93973218110015327). All guardians of the children provided informed consent.
Conflicts of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
da Silva Nunes, V.B., Dias, C.K., De Bastiani, M.A. et al. NT5E gene and CD38 protein as potential prognostic biomarkers for childhood B-acute lymphoblastic leukemia. Purinergic Signalling 18, 211–222 (2022). https://doi.org/10.1007/s11302-022-09841-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11302-022-09841-x