Abstract
Pain is a common clinical symptom that seriously affects the quality of life in a variety of patient populations. In recent years, research on the role of adenosine signaling in pain modulation has made great progress. Adenosine is a purine nucleoside and a neuromodulator, and regulates multiple physiological and pathophysiological functions through the activation of four G protein–coupled receptors, which are classified as A1, A2A, A2B, and A3 adenosine receptors (ARs). Adenosine and its receptors that are widespread in the central nervous system (CNS) play an important role in the processing of nociceptive sensory signals in different pain models. A1Rs have the highest affinity to adenosine, and the role in analgesia has been well investigated. The roles of A2ARs and A2BRs in the modulation of pain are controversial because they have both analgesic and pronociceptive effects. The analgesic effects of A3Rs are primarily manifested in neuropathic pain. In this article, we have reviewed the recent studies on ARs in the modulation of neuropathic pain, inflammatory pain, postoperative pain, and visceral pain in the CNS. Furthermore, we have outlined the pathways through which ARs contribute to pain regulation, thereby shedding light on how this mechanism can be targeted to provide effective pain relief.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pain is a distressing experience caused by tissue or nerve injury under different disease conditions, and it impacts human health globally. The latest research decision of the International Association for the Study of Pain (IASP) defines pain as “An unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage” [1]. Peripheral neurons, spinal cord, and brain mechanisms contributed to the modulation of pain. Sensory neurons in the periphery are activated and project into the spinal cord dorsal horn, and projection neurons send information to the brainstem and thalamus, and then to several brain regions involved in sensory discrimination and emotional sensory perception [2, 3]. Loss of synaptic inhibition in the spinal dorsal horn is a major process underlying the development of several pain conditions [3]. The cortical and subcortical regions related to pain perception are the primary and secondary somatosensory cortices, insula, anterior cingulate, thalamus, and prefrontal cortex [4]. Hyperactivity of sensory neurons and activation of astrocytes and microglia are also major contributors of chronic central nervous pain [5].
At present, the research on pain has made substantial progress; however, there are still many painful conditions that cannot be alleviated. The mechanisms of action associated with pain are not fully understood. As a neurotransmitter, adenosine regulates pain by activating four G protein–coupled receptors, namely, adenosine A1 receptors (A1Rs), adenosine A2A receptors (A2ARs), adenosine A2B receptors (A2BRs), and adenosine A3 receptors (A3Rs) [6]. There are significant differences in the affinities of adenosine to these receptors; adenosine has the highest affinity for A1Rs, followed by A3Rs, A2ARs, and A2BRs subtypes (A1Rs > A3Rs > A2ARs > A2BRs) [7, 8]. Adenosine triphosphate (ATP) is the main source of adenosine, which is sequentially dephosphorylated inside the cell to form adenosine diphosphate (ADP), adenosine monophosphate (AMP), and adenosine. Outside the cell, ectonucleosidase triphosphate diphosphohydrolase (CD39) and ecto-5′-nucleotidase (CD73) promote adenosine formation. Adenosine acts on its cognate receptors (A1Rs, A2ARs, A2BRs, and A3Rs) to regulate a variety of pain conditions [9,10,11] (Fig. 1). Accordingly, adenosine signaling has been identified as a potential target for the regulation of pain. Although the role of ARs in pain regulation has been studied in both central and peripheral nervous system, the role of CNS is more widely studied [12, 13].
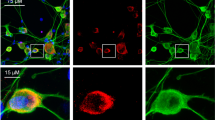
A schematic view of adenosine metabolism and ARs participating in pain. The dephosphorylation of ATP, ADP, and AMP is the main mechanism for the extracellular production of adenosine. A1R activation in CNS exerts analgesic effects in various types of pain such as inflammatory, neuropathic, postoperative, and visceral pain. The activation of A2ARs can play an analgesic role in neuropathic pain. On the other hand, the blockage of A2ARs exerts antinociceptive effects in postoperative pain. Both agonists and antagonists of A2ARs have been shown to relieve inflammatory pain. The stimulation of the A2BRs has an antinociceptive effect on chronic pain, while the blocking of A2BRs is helpful in the treatment of inflammatory pain. Besides, neuropathic pain can be relieved by agonists and antagonists of A2BRs. Finally, A3R activation gives analgesic effects in neuropathic pain
Since the 1970s, research on adenosine analgesia have mainly focused on the A1Rs [14]. With the intensive research on adenosine and its receptors, many investigators have found that other receptors (A2ARs, A2BRs, and A3Rs) also regulate pain. As per our present knowledge, adenosine signaling in the spinal cord involved in the analgesic process can be summarized in a relatively accurate manner as follows: (1) presynaptic inhibition of excitatory neurotransmitter release and inhibits the release of certain neurotransmitters in cerebrospinal fluid (CSF) and (2) postsynaptic inhibition of the effects of excitatory neurotransmitters [15]. However, owing to the scarcity of studies on the brain, the specific and in-depth analgesic mechanism is yet to be elucidated.
Here, we reviewed the distribution of AR subtypes in pain pathways and the role of each subtype in pain regulation of CNS, then highlight the regulatory roles and molecular mechanisms of several receptors in different pain models.
Location of adenosine receptors in the pain circuitry
ARs are present in various parts of the human body and mediate a myriad of physiological processes. Moreover, ARs affect the functioning of numerous systems in the body, including the CNS, cardiovascular system, gastrointestinal system, respiratory system, immune system, renal system, and metabolic system as well as different organs and tissues such as the kidney, bones, joints, eyes, and skin [9]. A1Rs are expressed in both central and peripheral nervous systems. In brain regions, A1Rs are found in the hippocampus, cerebral cortex, cerebellum, caudate-putamen, globus pallidus, thalamic nucleus, brain stem nucleus, periaqueductal gray (PAG), and basal ganglia, mainly in the excitatory synapses [6, 9, 16]. In the spinal cord dorsal horn, they are located in the inner lamina II postsynaptic neuronal cell bodies and processes [17]. Besides, the expression of A1Rs is found in the peripheral sensory nerve endings [6].
A2ARs are mainly located in the CNS and peripheral immune cells. Specifically, A2ARs are widely expressed in both the pre- and postsynaptic neurons, which are found in the caudate nucleus, nucleus accumbens, olfactory tubercle, and putamen of the brain. Experimental studies have illustrated the distribution of A2ARs in the lumbar spinal cord, the substantia gelatinosa, and in the lamina II neurons [18]. Immunochemical studies have revealed that A2ARs are expressed in the dorsal horn neurons of the thoracic spinal cord [19]. A2BRs are present on the presynaptic and postsynaptic neurons as well as on mature and precursor oligodendrocytes. They are widely expressed, but mostly in low abundance [10, 20, 21]. In the periphery, A2BRs are found on immune cells and inflammatory cells [22].
The A3R subtypes are widely expressed in different kinds of primary cells, tissues, and cell lines. In the CNS, they are distributed in the thalamus, hypothalamus, cortex, and hippocampus. A3Rs are also present in the lumbar spinal cord and in the supraspinal region, including the rostral ventromedial medulla (RVM) [23]. In the periphery, A3Rs are present in various cells such as immune cells and inflammatory cells [24]. All four ARs are found in the microglia and astrocytes [9, 20, 25].
Adenosine signaling and neuropathic pain
Neuropathic pain is pain caused by a lesion or disease of the somatosensory nervous system [1]. Mechanisms underlying the generation of neuralgia are associated with peripheral and central sensitization, including alterations in ion channels (sodium, calcium, and potassium), activation of immune cells such as neutrophils, mast cells, and macrophages, excessive activation of glial cells such as astrocytes and microglia, and epigenetic modulation [26, 27]. The alleviation of neuropathic pain by A1Rs has been confirmed by many studies [28,29,30,31]. A1Rs are present in pre- and postsynaptic membranes. Presynaptic A1Rs can inhibit the release of neurotransmitters and the transmission of pain signals, while postsynaptic A1Rs can induce neuronal membrane hyperpolarization. Research has demonstrated that A1Rs can activate Ca2+ channels, cause intracellular K+ outflow, promote neuronal hyperpolarization, and inhibit the excitability of postsynaptic neurons [32]. Mice lacking A1Rs exhibited a high degree of neuropathic pain-like behavior. In mice with partial sciatic nerve injury, A1R−/− mice displayed a significantly increased neuropathic pain-like behavioral response to heat or cold stimulation. Intrathecal administration of A1R agonist effectively reduces this pain [33]. This analgesic effect was also demonstrated in another study involving mice with partial sciatic nerve ligation. Paeoniflorin significantly improved the mechanical threshold and extended the thermal latent period, while A1R antagonist eliminated the analgesic effect of paeoniflorin. Their finding suggests that paeoniflorin exerts its analgesic and hypnotic effects by activating A1Rs to inhibit the neuronal hyperactivity in the anterior cingulate cortex and ventrolateral PAG [34]. Hyperalgesia and mechanical static allodynia in a rat model of vincristine induced peripheral neuropathy effectively alleviated by intrathecal injection of the A1R agonist R-PIA. Intrathecal administration of R-PIA significantly reversed the increase of tumor necrosis factor-α (TNF-α) level and myeloperoxidase activity in a dose-dependent manner. This suggests that intrathecal injection of R-PIA appears to exert analgesic effects through its anti-inflammatory effects, particularly inhibition of TNF-α level and myeloperoxidase activity [35]. Furthermore, in a mice model of diabetes induced by streptozotocin, intrathecal injection of adenosine and A1R agonist significantly improved the mechanical threshold [36]. On the other hand, in naive rats, it only reduced thermal hypersensitivity and had no effect on the threshold of mechanical stimulation. Electrophysiological studies have shown that CPA suppresses C fibers, but not the baseline of A fibers. The sensory nerve C fiber mediates hyperalgesia caused by nociceptive thermal stimulation, while the sensory nerve A fiber is mainly involved in hypersensitivity to pain caused by mechanical stimulation. Therefore, the authors hypothesize that A1Rs may be expressed more in the nerve endings of C fiber than in A fiber [37]. Mitogen-activated protein kinase (MAPK) family, which consists of three independent signaling pathways, ERK, p38, and c-Jun N-terminal kinase, plays a key role in regulating nociceptive signaling. In different animal models, inhibition of all three MAPK pathways has been shown to reduce inflammatory and neuropathic pain [38]. Cobra neurotoxin (CNT), a short-chain peptide isolated from the venom of Naja naja atra, showed both a central antinociceptive effect and a hyperalgesic reaction in mice models. In the hot plate assay and spinal cord injury (SCI) model, a small dose (25 µg/kg) of CNT produced central analgesic effects by inhibiting the phosphorylation of ERK1 (p44 MAPK) and ERK2 (p42 MAPK) via activation of A1R in the spinal cord [39]. The above research have demonstrated that A1Rs could alleviate neuropathic pain. However, in a recent study, Metzner et al. found that although A1Rs are expressed in dorsal root ganglion (DRG) neurons and dorsal horn neurons involved in pain processing, administration of the A1R agonist capadenoson at established doses in vivo (0.03–1.0 mg/kg) did not alter mechanical hypersensitivity in mice models of spared nerve injury and paclitaxel-induced neuropathic pain. This suggests a partial A1R agonist failed to relieve neuropathic pain in mice [40].
In the CNS, the A2ARs have been shown to be potential targets for alleviating neuropathic pain [41, 42]. Mice lacking A2ARs (A2ARs−/−) display hypoalgesia [43]. Loram et al. found that a single intrathecal injection of A2AR agonist can relieve neuropathic pain constantly. In chronicconstrictive injury (CCI) rat models, a single intrathecal injection of an A2AR agonist (ATL313) or CGS21680 produced a prolonged reversal of mechanical hyperalgesia and hyperthermia for at least 4 weeks. The combined intrathecal administration of A2AR antagonist and ATL313 eliminated the effect of ATL313 on neuropathic pain in rats. ATL313 was able to effectively attenuate the CCI-induced upregulation of microglia and astrocyte activation marks in spinal cord segments L4–L6 at 1 and 4 weeks after a single intrathecal injection of ATL313. The effect of ATL313 on neuropathic pain was temporarily abolished by the intrathecal administration of neutralizing interleukin (IL)-10 antibodies. In addition, IL-10 mRNA was significantly elevated in the CSF cells collected from the lumbar region. Therefore, A2ARs may alleviate neuropathic pain by enhancing IL-10 in the immune-active cells of the CNS [44]. The researchers further explored the potential mechanism of the long-term effect of A2AR agonists. Intrathecal injection of ATL313 reverses neuropathic pain by significantly attenuating TNF-α production in microglia and astrocytes via PKA/protein kinase C (PKC) signaling. Therefore, intrathecal injection of adenosine A2AR agonist can reverse neuropathic hyperalgesia through PKA/PKC signal transduction [42]. This effect has also been demonstrated in another study. A single intrathecal injection of CGS21680 reversed SCI-induced tenderness for at least 6 weeks. To some extent, this reversal may be mediated by interleukin IL-10 [41]. Besides, many studies have shown that A2ARs mediate analgesia by altering the transduction of signals in the relevant neurotransmitter system. The activation of N-methyl d-aspartate (NMDA) receptors can induce hyperalgesia; patch-clamp recordings showed that NMDA currents were inhibited during the application of selective A2AR agonists. These results allude that A2ARs play a pivotal role in the regulation of NMDA receptors activity through a postsynaptic mechanism [18].
A2BR involvement has also been investigated in relation to neuropathic pain. Nevertheless, both agonists and antagonists have been shown to relieve neuralgia in different experiments. Studies supporting the pronociceptive effect of A2BRs suggest that these receptors may be involved in pain. Electrophysiological studies have shown that the continuous increase in A2BRs signaling enhances the excitability of primary sensory neurons, leading to chronic pain in the Ada−/− mice [7]. The prolonged accumulation of circulating adenosine may cause pain in three animal models of chronic pain, including Ada−/−, sickle cell disease, and CFA-injected mice. Persistent elevation of plasma adenosine mediates the activation of A2BRs in myeloid cells and induces TRPV1 gene expression in the DRG neurons through gp130-dependent IL-6/sIL-6R signal transduction, thereby promoting chronic pain [45]. On the contrary, studies supporting the analgesic effect of A2BRs suggest that they may alleviate neuropathic pain. In the CCI experiment, the long-term reversal of neuropathic hyperalgesia extended to A2BRs, while A1Rs only produced a short-term reversal of mechanical hyperalgesia, which lasted < 3 days. [42].
The role of A3Rs in the CNS is mainly reflected in the reversal of neuropathic pain. Many studies have shown that glial cells can release nitroxidative species and pro-inflammatory cytokines to sensitize the dorsal horn neurons and cause pain, whereas A3Rs can attenuate nociception by modulating the glial cells [23]. The systemic administration of A3R agonist (IB MECA) can reverse neuropathic pain after peripheral tibial nerve injury by inhibiting the activation of microglia and phosphorylation of p38 MAPK nerve in the spinal dorsal horn [46]. In rat models of oxaliplatin [47]- and paclitaxel [48]-induced peripheral neuropathy, intraperitoneal injection of the agonist IB-MECA effectively blocked the development of neuropathic pain by suppressing the redox-sensitive transcription factor (NFκB) and mitogen-activated protein kinases (ERK and p38), reducing the astrocyte overactivation, inhibiting the generation of pro-inflammatory and neuroexcitatory cytokines (TNF, IL-1β), and increasing the levels of the anti-inflammatory/neuroprotective cytokines (IL-10, IL-4). Furthermore, A3Rs can also achieve analgesic effect by regulating the MAPK/ERK pathway. In a rat model of neuropathic pain induced by spinal nerve ligation (SNL), amitriptyline inhibits MAPK/ERK and cyclic AMP response element-binding protein pathways and proinflammatory cytokines, including TNF-α, intercellular adhesion molecule 1 (ICAM-1), macrophage inflammatory protein 2 (MIP-2), and monocyte chemoattractant protein 1 (MCP-1), by activating A3Rs to exert antinociceptive effects [49]. In a CCI-induced neuropathic pain model in mice, intraperitoneal injection of the highly selective A3R agonist MRS5980, which releases IL-10 by activating A3Rs expressed on CD4 + T cells, reduces the excitability of neuronal DRG and thereby reverses established hypersensitivity [50]. In addition, the regulation of neurotransmitter imbalance is one major pathway by which A3Rs mediate antinociception. Electrophysiological studies have shown that voltage-dependent Ca2+ channels (VDCCs) play a key role in neuropathic pain. These channels are activated at the presynaptic level and induce the release of neurotransmitters through the sensory neurons of the central and peripheral nervous systems, including the DRG. Selective A3R activation inhibits N-type VDCC opening, which curtails the neurotransmitter release and decreases the action potential firing in isolated rat DRG neurons [51]. Little et al. demonstrated that augmenting the endogenous adenosine level through selective adenosine kinase inhibition can produce strong analgesic effects in models of neuropathic pain through the A3R signaling pathway. Similar results were achieved by spinal or RVM injection of the A3R agonist IB-MECA. The antinociceptive functions of A3R agonists are independent of endogenous opioid or endocannabinoid pathways. These agonists reverse allodynia by activating the 5-HT and norepinephrine circuits and reducing the excitability of a wide and dynamic range of spinal neurons. This finding suggests that the activation of A3Rs by adenosine is an endogenous antinociceptive pathway [52]. Restoration of the GABAergic inhibition system contributes to the reversal of neuropathic pain after A3R activation. The activated A3Rs can act on the neurons and promote the release of GABAergic, thereby inhibiting nerve excitability and reducing nociceptive signals and producing an analgesic effect [23]. Intrathecal administration of the A3R agonist MRS5698 dose-dependently reversed CCI-induced mechanical allodynia, and spinal administration of the A3R antagonist MRS1523 blocked the analgesia produced by MRS5698. Their study suggests MRS5698 contributed to restore K+–Cl− cotransporter 2 (KCC2)–dependent Cl− transport in CNS neurons, which underlies the increased capacity for GABAergic neurotransmission [53]. In addition, A3R agonists can reduce the activation of astrocytes and restore the normal function of the GABAergic inhibitory system by lowering the brain-derived neurotrophic factor (BDNF) signaling [23, 46]. A single dose of IB-MECA was more effective in analgesia in the neuralgia model than in inflammatory pain, and IB-MECA reversed the neuralgia model–induced increase in brainstem BDNF levels to attenuate pain [54].
To summarize, among the four subtypes of ARs, A1Rs, A2ARs, and A3Rs are mainly involved in neuropathic pain, while there are relatively few studies on A2BRs. A1Rs exert their effects by inhibiting TNF-α expression through the MAPK/ERK pathway. A2ARs alleviate neuropathic pain by inhibiting microglia, astrocytes, and TNF-α through the PKA/PKC signaling pathway, and enhancing IL-10. In neuropathic pain, A3Rs play an analgesic role by inhibiting TNF, IL-1β, and BDNF, increasing IL-10 and IL-4 level signals, and restoring the normal function of the GABAergic inhibitory system by regulating the MAPK/ERK pathway.
Adenosine signaling and inflammatory pain
Inflammatory pain is caused by thermal, chemical, or mechanical damage to nociceptors of the nervous system, as well as increased mechanical and thermal sensitivity due to inflammation-related changes [55]. The central underlying mechanisms of inflammatory pain remain unclear. The antinociceptive effect of adenosine signaling has been primarily attributed to the activation of A1Rs. In an inflammatory model of thermal hyperalgesia, agents that act directly or indirectly on adenosine, when administered through the spinal cord, were found to produce antinociception via activation of the spinal A1Rs [56]. Inhibitory glycinergic neurotransmission is an important target for adenosine regulation. Activation of A1Rs may increase the inhibitory postsynaptic currents mediated by glycine receptors in the spinal cord sections of rats injected with complete Freund’s adjuvant (CFA) through the Gαi/PKAα3 and Gβγ/α1ins pathways. Thus, nociceptive information is transmitted by inhibiting the excitability of neurons and weakening the spinal cord neural circuits. This enhanced spinal cord inhibition may be an important pathway by which A1Rs reduce hyperalgesia [57]. The α1ins phosphorylation at Ser380 by ERK has been proven to lower the glycinergic synaptic currents and contribute to spinal disinhibition. CFA-induced peripheral inflammation increased the phosphorylation of Ser380 in the spinal dorsal horn of mice and was inhibited by the activation of specific A1Rs. This finding further supports the above analgesic mechanism of A1Rs [58]. In addition, T35 (Zusanli) at 10.6-μM laser irradiation exerts analgesic effects by upregulating spinal A1Rs to inhibit nociceptive sensation and NMDA receptor 1 phosphorylation in the monosodium iodoacetate–induced knee osteoarthritis model [59]. Moreover, the anti-inflammatory and analgesic effects of some drugs are also mediated through A1Rs in the spinal cord, such as tramadol and Norisoboldine [60, 61]. We also compared the analgesic effects of A1Rs with morphine. To the best of our knowledge, the intrathecal administration of both A1R agonist and morphine can alleviate formalin-induced pain behaviors. However, while morphine acts on the presynaptic and postsynaptic mechanisms of the CSF glutamate release system, the analgesic mechanism of A1Rs may be related to the reduction of postsynaptic excitability by inhibiting the glutamate terminal [62].
The role of adenosine in the regulation of inflammatory pain is also dependent on the A2ARs [42, 44]. The relationship between A2ARs and pain has long been controversial; both A2AR antagonists and agonists exhibit analgesic effects. Studies supporting the analgesic effect of A2ARs indicate that the central application of A2AR agonists can produce an analgesic effect. The intrathecal injection of neuropeptide S (NPS) can alleviate the nociception caused by formalin. The function of adenosine in the regulation of inflammatory pain is mainly dependent on the A2ARs. Intrathecal injection of the A2AR antagonist ZM241385 blocked the antinociceptive effect of NPS throughout the experiment. In addition, the A1R antagonist DPCPX blocked the effects of NPS during the first 5 min of the experiment. This observation demonstrates the involvement of adenosine in NPS analgesia, especially A2AR, plays a more lasting role [63]. Such effects have also been observed in the brain. Intracerebroventricular injection of Adonis, an agonist-like monoclonal antibody with high specificity for the A2ARs, resulted in a significant dose-dependent increase in hot-plate and tail-flick latencies in mice, and this effect was prevented by A2AR antagonist [64]. These trials establish that A2ARs have antinociceptive effects on the CNS. However, studies supporting the pronociceptive effect of A2ARs have suggested that the central administration of A2AR antagonist can produce an analgesic effect. Intrathecal injection of A2AR antagonist SCH58261 produced antinociception in formalin test, suggesting that A2ARs are involved in the antinociceptive effect of the spinal cord [65]. The A2AR antagonist ZM241385 blocked bladder hyperactivity and hyperalgesia from cyclophosphamide-induced cystitis. A2ARs and transient receptor potential vanilloid 1 (TRPV1) are co-expressed in DRG neurons. Inhibition of A2ARs decreased the sensitivity of TRPV1 in DRG neurons. This result illustrates that the inhibition of adenosine A2ARs alleviate bladder hyperalgesia in cyclophosphamide induced cystitis by inhibiting sensitization of TRPV1 [66].
The regulatory role of A2BRs in inflammatory pain has also been studied. In a formalin experiment, intrathecal injection of adenosine A2BR antagonist could reverse the antinociceptive effect of adenosine, alluding the antinociceptive role for spinal A2BRs [15]. In another formalin experiment, Bilkei-Gorzo et al. found that the A2BR antagonist PSB-1115 has a dose-dependent effect on the alleviation of inflammatory pain, which reached the maximum effect at a low dose of 3 mg/kg, while being nociceptive over a broad dose range [67]. These results suggest that A2BRs may have a pronociceptive effect.
Overall, the abovementioned data showed that A1Rs and A2ARs are mainly involved in inflammatory pain in the CNS. A1Rs alleviate inflammatory pain by inhibiting excitatory amino acids through the Gαi/PKAα3 and Gβγ/α1ins pathways. A2ARs have both pronociceptive and antinociceptive effects, the pronociceptive effect of A2ARs may be related to TRPV1. A2BRs may play a promoting role in inflammatory pain; however, there are few studies on A2BRs and A3Rs, so the mechanisms need more research to prove.
Adenosine signaling and postoperative and visceral pain
A1Rs also seem to be involved in postoperative pain. Intrathecal injection of the A1R agonist R-PIA can reduce postoperative mechanical hyperalgesia and improve the pain threshold in incisions. Zahn et al. assessed the different K+ channels for A1R-mediated antinociception in the surgical incision of rats. The results illustrated that the analgesic effect of R-PIA was alleviated by the intrathecal administration of a KATP channel blocker, while Ca2+-activated K+ channels or Kv1.3 or Kv1.6 channel blockers failed to decrease R-PIA-induced hypoalgesia. This result implies that the opening of the KATP channel is conducive for the analgesic effects of A1R agonist [68]. Another report suggests that intrathecal adenosine may be an effective treatment for neuropathic pain but not for postoperative pain. Yamaoka et al. compared the effects of intrathecal injection of adenosine on three types of pain signals: two neuropathic pains (spinal cord compression and chronic constriction of the sciatic nerve) and one postoperative pain (plantar incision). Following the intrathecal injection of Cl-adenosine 24 h after the surgery, the pain levels of the three models were significantly improved. Intrathecal administration of adenosine at 72 h after the surgery suppressed hyperalgesia in a neuropathic pain model, but it had no effect on the postoperative pain model. When compared with the other two models, the expressions of A1R messenger RNA (mRNA) and protein were significantly decreased in the plantar incision. This observation signifies that the decrease in A1Rs may be the main reason for the ineffective analgesia of adenosine [69]. Moreover, A2ARs are involved in the regulation of postoperative pain perception in the median preoptic nucleus (MnPO). When compared with ad libitum sleep, complete sleep deprivation (the hypothalamus pituitary adrenal axis was not activated) 6 h before the surgical incision significantly enhanced the postoperative mechanical hypersensitivity of the affected paw and prolonged the recovery time. Microinjection of the adenosine A2AR antagonist ZM241385 into the MnPO not only effectively blocked the surgical pain in the rats but also eliminated the thermal hyperalgesia caused by sleep deprivation in a group of non-surgical rats [70].
The potential role of A1Rs in postoperative pain was also investigated. Intracisternal injection of CPA increased the threshold of abdominal withdrawal reflex induced by colon dilation in rats. In addition, the administration of DPCPX, an A1R antagonist, completely blocked the brain orexin-induced antinociceptive action against colonic distension [71]. Subsequently, Okumura et al. confirmed the antinociceptive effects of CPA in visceral pain. In their study, intracisternal injection of 5-HT1A or 5-HT2A receptor antagonist was given, and subcutaneous injection of dopamine D1 receptor antagonist, cannabinoid 1 (CB1) receptor antagonist, or naloxone blocked the CPA-induced visceral antinociception. However, intracisternal injection of 5-HT1B and subcutaneous injections of dopamine D2 receptor and CB2 receptor antagonists failed to block the CPA-induced antinociception. It could therefore be inferred that the visceral antinociception of A1Rs is caused by the activation of 5-HT2A, 5-HT1A, and dopamine D1 or CB1 receptors [72].
As far as current studies are concerned, in CNS, the regulation of postoperative and visceral pain is mainly mediated by A1Rs. A1Rs relieve postoperative pain through the KATP pathway, and A1Rs relieve visceral pain through 5-HT2A, 5-HT1A, and dopamine D1 or CB1 receptors. A2ARs have also been implicated in regulating postoperative pain; however, relatively few studies have been conducted on A2ARs, A2BRs, and A3Rs, and the related mechanisms need to be further explored (Table 1).
Conclusion and perspectives
Purinergic signaling induces potent modulation in different pain models. Most studies have shown that activation of A1Rs contributes to relieve a variety of pain, but recent studies have also demonstrated that some agonists are ineffective in relieving neuralgia in mice, which needs to be confirmed by further studies. The role of A2ARs in pain regulation is related to different pain models. Activation of A2ARs can relieve neuralgia, while A2ARs have both pronociceptive and antinociceptive effects in inflammatory pain. A2BR regulation of pain in the CNS is relatively poorly studied, and specific mechanisms need further exploration. The activation of A3Rs contributes to the relief of neuropathic pain, and its regulation of inflammatory pain has been relatively poorly reported in the CNS.
Even though great achievements have been made for the past decades in regulation of pain mediated by adenosine signaling, there still exist a lot of challenges for further investigations: (1) Compared with other receptors, A2BRs have been less studied in the CNS. It is still not clear how A2BRs regulate pain. And the specific pathways and downstream molecular mechanisms that regulate pain need to be further studied. (2) Adenosine degrades rapidly in vivo, making it difficult to detect adenosine signals in time. It might be most helpful to introduce new detection tools to elucidate the regulatory role of adenosine signaling in pathological conditions. In summary, adenosine signaling exerts a significant role at pain regulation in the CNS, and as research continues, adenosine signaling pathway may become effective target of drugs for the treatment of pain in the near future.
Data availability
This article does not contain unpublished data, and all data discussed in this article are available in cited publications.
References
(2020) International Association For The Study Of Pain
Peirs C, Seal RP (2016) Neural circuits for pain: recent advances and current views. Science, 354(6312), 578–584. https://doi.org/10.1126/science.aaf8933
Zeilhofer HU (2008) Loss of glycinergic and GABAergic inhibition in chronic pain--contributions of inflammation and microglia. Int Immunopharmacol, 8(2), 182–187. https://doi.org/10.1016/j.intimp.2007.07.009
Apkarian AV, Bushnell MC, Treede RD, Zubieta JK (2005) Human brain mechanisms of pain perception and regulation in health and disease. Eur J Pain, 9(4), 463–484. https://doi.org/10.1016/j.ejpain.2004.11.001
Gwak YS, Hulsebosch CE, Leem JW (2017) Neuronal-glial interactions maintain chronic neuropathic pain after spinal cord injury. Neural Plast, 20172480689. https://doi.org/10.1155/2017/2480689
Sawynok J (2016) Adenosine receptor targets for pain. Neuroscience, 3381–18. https://doi.org/10.1016/j.neuroscience.2015.10.031
Adebiyi MG, Manalo J, Kellems RE, Xia Y (2019) Differential role of adenosine signaling cascade in acute and chronic pain. Neurosci Lett, 712134483. https://doi.org/10.1016/j.neulet.2019.134483
Fredholm BB, AP IJ, Jacobson KA, Linden J, Muller CE (2011) International Union of Basic and Clinical Pharmacology. LXXXI. Nomenclature and classification of adenosine receptors--an update. Pharmacol Rev, 63(1), 1–34. https://doi.org/10.1124/pr.110.003285
Borea PA, Gessi S, Merighi S, Vincenzi F, Varani K (2018) Pharmacology of adenosine receptors: the state of the art. Physiol Rev, 98(3), 1591–1625. https://doi.org/10.1152/physrev.00049.2017
Chen JF, Eltzschig HK, Fredholm BB (2013) Adenosine receptors as drug targets--what are the challenges? Nat Rev Drug Discov, 12(4), 265–286. https://doi.org/10.1038/nrd3955
Shaw S, Uniyal A, Gadepalli A, Tiwari V, Belinskaia DA, Shestakova NN, Venugopala KN, Deb PK, Tiwari V (2020) Adenosine receptor signalling: probing the potential pathways for the ministration of neuropathic pain. Eur J Pharmacol, 889173619. https://doi.org/10.1016/j.ejphar.2020.173619
Choudhury H, Chellappan DK, Sengupta P, Pandey M, Gorain B (2019) Adenosine receptors in modulation of central nervous system disorders. Curr Pharm Des, 25(26), 2808–2827. https://doi.org/10.2174/1381612825666190712181955
Liu YJ, Chen J, Li X, Zhou X, Hu YM, Chu SF, Peng Y, Chen NH (2019) Research progress on adenosine in central nervous system diseases. CNS Neurosci Ther, 25(9), 899–910. https://doi.org/10.1111/cns.13190
Vapaatalo H, Onken D, Neuvonen PJ, Westermann E (1975) Stereospecificity in some central and circulatory effects of phenylisopropyl-adenosine (PIA). Arzneimittelforschung, 25(3), 407–410.
Yoon MH, Bae HB, Choi JI, Kim SJ, Chung ST, Kim CM (2006) Roles of adenosine receptor subtypes in the antinociceptive effect of intrathecal adenosine in a rat formalin test. Pharmacology, 78(1), 21–26. https://doi.org/10.1159/000094762
Rivkees SA, Price SL, Zhou FC (1995) Immunohistochemical detection of A1 adenosine receptors in rat brain with emphasis on localization in the hippocampal formation, cerebral cortex, cerebellum, and basal ganglia. Brain Res, 677(2), 193–203. https://doi.org/10.1016/0006-8993(95)00062-u
Schulte G, Robertson B, Fredholm BB, DeLander GE, Shortland P, Molander C (2003) Distribution of antinociceptive adenosine a1 receptors in the spinal cord dorsal horn, and relationship to primary afferents and neuronal subpopulations. Neuroscience 121(4):907–916. https://doi.org/10.1016/s0306-4522(03)00480-9
Guntz E, Dumont H, Pastijn E, d'Exaerde Ade K, Azdad K, Sosnowski M, Schiffmann SN, Gall D (2008) Expression of adenosine A 2A receptors in the rat lumbar spinal cord and implications in the modulation of N-methyl-d-aspartate receptor currents. Anesth Analg, 106(6), 1882–1889. https://doi.org/10.1213/ane.0b013e318173251f
Brooke RE, Deuchars J, Deuchars SA (2004) Input-specific modulation of neurotransmitter release in the lateral horn of the spinal cord via adenosine receptors. J Neurosci, 24(1), 127–137. https://doi.org/10.1523/JNEUROSCI.4591-03.2004
Merighi S, Borea PA, Stefanelli A, Bencivenni S, Castillo CA, Varani K, Gessi S (2015) A2a and a2b adenosine receptors affect HIF-1alpha signaling in activated primary microglial cells. Glia, 63(11), 1933–1952. https://doi.org/10.1002/glia.22861
Pedata F, Dettori I, Coppi E, Melani A, Fusco I, Corradetti R, Pugliese AM (2016) Purinergic signalling in brain ischemia. Neuropharmacology, 104105–130. https://doi.org/10.1016/j.neuropharm.2015.11.007
Hasko G, Csoka B, Nemeth ZH, Vizi ES, Pacher P (2009) A(2B) adenosine receptors in immunity and inflammation. Trends Immunol, 30(6), 263–270. https://doi.org/10.1016/j.it.2009.04.001
Janes K, Symons-Liguori AM, Jacobson KA, Salvemini D (2016) Identification of A3 adenosine receptor agonists as novel non-narcotic analgesics. Br J Pharmacol, 173(8), 1253–1267. https://doi.org/10.1111/bph.13446
Vincenzi F, Pasquini S, Borea PA, Varani K (2020) Targeting adenosine receptors: a potential pharmacological avenue for acute and chronic pain. Int J Mol Sci, 21(22). https://doi.org/10.3390/ijms21228710
Boison D, Chen JF, Fredholm BB (2010) Adenosine signaling and function in glial cells. Cell Death Differ, 17(7), 1071–1082. https://doi.org/10.1038/cdd.2009.131
Finnerup NB, Kuner R, Jensen TS (2021) Neuropathic pain: from mechanisms to treatment. Physiol Rev, 101(1), 259–301. https://doi.org/10.1152/physrev.00045.2019
Meacham K, Shepherd A, Mohapatra DP, Haroutounian S (2017) Neuropathic pain: central vs. peripheral mechanisms. Curr Pain Headache Rep, 21(6), 28. https://doi.org/10.1007/s11916-017-0629-5
Dai QX, Huang LP, Mo YC, Yu LN, Du WW, Zhang AQ, Geng WJ, Wang JL, Yan M (2020) Role of spinal adenosine A1 receptors in the analgesic effect of electroacupuncture in a rat model of neuropathic pain. J Int Med Res, 48(4), 300060519883748. https://doi.org/10.1177/0300060519883748
Zhang M, Dai Q, Liang D, Li D, Chen S, Chen S, Han K, Huang L, Wang J (2018) Involvement of adenosine A1 receptor in electroacupuncture-mediated inhibition of astrocyte activation during neuropathic pain. Arq Neuropsiquiatr, 76(11), 736–742. https://doi.org/10.1590/0004-282X20180128
Jacobson KA, Giancotti LA, Lauro F, Mufti F, Salvemini D (2020) Treatment of chronic neuropathic pain: purine receptor modulation. Pain, 161(7), 1425–1441. https://doi.org/10.1097/j.pain.0000000000001857
Hansen Wang, Hui Xu, Long-Jun Wu, Susan S Kim, Tao Chen, Kohei Koga GD, Bo Gong, Kunjumon I Vadakkan, Xuehan Zhang, Bong-Kiun Kaang MZ (2011) Identification of an adenylyl cyclase inhibitor for treating neuropathic and inflammatory pain. Sci Transl Med. https://doi.org/10.1126/scitranslmed.3001269
Salter MW, De Koninck Y, Henry JL (1993) Physiological roles for adenosine and ATP in synaptic transmission in the spinal dorsal horn. Prog Neurobiol, 41(2), 125–156. https://doi.org/10.1016/0301-0082(93)90006-e
Wu WP, Hao JX, Halldner L, Lovdahl C, DeLander GE, Wiesenfeld-Hallin Z, Fredholm BB, Xu XJ (2005) Increased nociceptive response in mice lacking the adenosine A1 receptor. Pain, 113(3), 395–404. https://doi.org/10.1016/j.pain.2004.11.020
Yin D, Liu YY, Wang TX, Hu ZZ, Qu WM, Chen JF, Cheng NN, Huang ZL (2016) Paeoniflorin exerts analgesic and hypnotic effects via adenosine A1 receptors in a mouse neuropathic pain model. Psychopharmacology (Berl), 233(2), 281–293. https://doi.org/10.1007/s00213-015-4108-6
Kim K, Jeong W, Jun IG, Park JY (2020) Antiallodynic and anti-inflammatory effects of intrathecal R-PIA in a rat model of vincristine-induced peripheral neuropathy. Korean J Anesthesiol, 73(5), 434–444. https://doi.org/10.4097/kja.19481
Katz NK, Ryals JM, Wright DE (2015) Central or peripheral delivery of an adenosine A1 receptor agonist improves mechanical allodynia in a mouse model of painful diabetic neuropathy. Neuroscience, 285312–323. https://doi.org/10.1016/j.neuroscience.2014.10.065
Gong QJ, Li YY, Xin WJ, Wei XH, Cui Y, Wang J, Liu Y, Liu CC, Li YY, Liu XG (2010) Differential effects of adenosine A1 receptor on pain-related behavior in normal and nerve-injured rats. Brain Res, 136123–30. https://doi.org/10.1016/j.brainres.2010.09.034
Ji RR, Gereau RWt, Malcangio M, Strichartz GR (2009) MAP kinase and pain. Brain Res Rev, 60(1), 135–148. https://doi.org/10.1016/j.brainresrev.2008.12.011
Zhao C, Zhao J, Yang Q, Ye Y (2017) Cobra neurotoxin produces central analgesic and hyperalgesic actions via adenosine A1 and A2A receptors. Mol Pain, 131744806917720336. https://doi.org/10.1177/1744806917720336
Metzner K, Gross T, Balzulat A, Wack G, Lu R, Schmidtko A (2021) Lack of efficacy of a partial adenosine A1 receptor agonist in neuropathic pain models in mice. Purinergic Signal. https://doi.org/10.1007/s11302-021-09806-6
Kwilasz AJ, Ellis A, Wieseler J, Loram L, Favret J, McFadden A, Springer K, Falci S, Rieger J, Maier SF, Watkins LR (2018) Sustained reversal of central neuropathic pain induced by a single intrathecal injection of adenosine A2A receptor agonists. Brain Behav Immun, 69470–479. https://doi.org/10.1016/j.bbi.2018.01.005
Loram LC, Taylor FR, Strand KA, Harrison JA, Rzasalynn R, Sholar P, Rieger J, Maier SF, Watkins LR (2013) Intrathecal injection of adenosine 2A receptor agonists reversed neuropathic allodynia through protein kinase (PK)A/PKC signaling. Brain Behav Immun, 33112–122. https://doi.org/10.1016/j.bbi.2013.06.004
Bailey A, Weber D, Zimmer A, Zimmer AM, Hourani SM, Kitchen I (2004) Quantitative autoradiography of adenosine receptors and NBTI-sensitive adenosine transporters in the brains of mice deficient in the preproenkephalin gene. Brain Res, 1025(1–2), 1–9. https://doi.org/10.1016/j.brainres.2004.06.088
Loram LC, Harrison JA, Sloane EM, Hutchinson MR, Sholar P, Taylor FR, Berkelhammer D, Coats BD, Poole S, Milligan ED, Maier SF, Rieger J, Watkins LR (2009) Enduring reversal of neuropathic pain by a single intrathecal injection of adenosine 2A receptor agonists: a novel therapy for neuropathic pain. J Neurosci, 29(44), 14015–14025. https://doi.org/10.1523/JNEUROSCI.3447-09.2009
Hu X, Adebiyi MG, Luo J, Sun K, Le TT, Zhang Y, Wu H, Zhao S, Karmouty-Quintana H, Liu H, Huang A, Wen YE, Zaika OL, Mamenko M, Pochynyuk OM, Kellems RE, Eltzschig HK, Blackburn MR, Walters ET, Huang D, Hu H, Xia Y (2016) Sustained elevated adenosine via ADORA2B promotes chronic pain through neuro-immune interaction. Cell Rep, 16(1), 106–119. https://doi.org/10.1016/j.celrep.2016.05.080
Terayama R, Tabata M, Maruhama K, Iida S (2018) A3 adenosine receptor agonist attenuates neuropathic pain by suppressing activation of microglia and convergence of nociceptive inputs in the spinal dorsal horn. Exp Brain Res, 236(12), 3203–3213. https://doi.org/10.1007/s00221-018-5377-1
Janes K, Wahlman C, Little JW, Doyle T, Tosh DK, Jacobson KA, Salvemini D (2015) Spinal neuroimmune activation is independent of T-cell infiltration and attenuated by A3 adenosine receptor agonists in a model of oxaliplatin-induced peripheral neuropathy. Brain Behav Immun, 4491–99. https://doi.org/10.1016/j.bbi.2014.08.010
Janes K, Esposito E, Doyle T, Cuzzocrea S, Tosh DK, Jacobson KA, Salvemini D (2014) A3 adenosine receptor agonist prevents the development of paclitaxel-induced neuropathic pain by modulating spinal glial-restricted redox-dependent signaling pathways. Pain, 155(12), 2560–2567. https://doi.org/10.1016/j.pain.2014.09.016
Kim Y, Kwon SY, Jung HS, Park YJ, Kim YS, In JH, Choi JW, Kim JA, Joo JD (2019) Amitriptyline inhibits the MAPK/ERK and CREB pathways and proinflammatory cytokines through A3AR activation in rat neuropathic pain models. Korean J Anesthesiol, 72(1), 60–67. https://doi.org/10.4097/kja.d.18.00022
Durante M, Squillace S, Lauro F, Giancotti LA, Coppi E, Cherchi F, Di Cesare Mannelli L, Ghelardini C, Kolar G, Wahlman C, Opejin A, Xiao C, Reitman ML, Tosh DK, Hawiger D, Jacobson KA, Salvemini D (2021) Adenosine A3 agonists reverse neuropathic pain via T cell-mediated production of IL-10. J Clin Invest, 131(7). https://doi.org/10.1172/JCI139299
Coppi E, Cherchi F, Fusco I, Failli P, Vona A, Dettori I, Gaviano L, Lucarini E, Jacobson KA, Tosh DK, Salvemini D, Ghelardini C, Pedata F, Di Cesare Mannelli L, Pugliese AM (2019) Adenosine A3 receptor activation inhibits pronociceptive N-type Ca2+ currents and cell excitability in dorsal root ganglion neurons. Pain, 160(5), 1103–1118. https://doi.org/10.1097/j.pain.0000000000001488
Little JW, Ford A, Symons-Liguori AM, Chen Z, Janes K, Doyle T, Xie J, Luongo L, Tosh DK, Maione S, Bannister K, Dickenson AH, Vanderah TW, Porreca F, Jacobson KA, Salvemini D (2015) Endogenous adenosine A3 receptor activation selectively alleviates persistent pain states. Brain, 138(Pt 1), 28–35. https://doi.org/10.1093/brain/awu330
Ford A, Castonguay A, Cottet M, Little JW, Chen Z, Symons-Liguori AM, Doyle T, Egan TM, Vanderah TW, De Koninck Y, Tosh DK, Jacobson KA, Salvemini D (2015) Engagement of the GABA to KCC2 signaling pathway contributes to the analgesic effects of A3AR agonists in neuropathic pain. J Neurosci, 35(15), 6057–6067. https://doi.org/10.1523/JNEUROSCI.4495-14.2015
Cioato SG, Medeiros LF, Lopes BC, de Souza A, Medeiros HR, Assumpcao JAF, Caumo W, Roesler R, Torres ILS (2020) Antinociceptive and neurochemical effects of a single dose of IB-MECA in chronic pain rat models. Purinergic Signal, 16(4), 573–584. https://doi.org/10.1007/s11302-020-09751-w
Pedersen JL (2000) Inflammatory pain in experimental burns in man. Dan Med Bull, 47(3), 168–195
A Poon JS (1998) Antinociception by adenosine analogs and inhibitors of adenosine metabolism in an inflammatory thermal hyperalgesia model in the rat. Pain, 235–245. https://doi.org/10.1016/S0304-3959(97)00186-3
Bai HH, Liu JP, Yang L, Zhao JY, Suo ZW, Yang X, Hu XD (2017) Adenosine A1 receptor potentiated glycinergic transmission in spinal cord dorsal horn of rats after peripheral inflammation. Neuropharmacology, 126158–167. https://doi.org/10.1016/j.neuropharm.2017.09.001
Diao XT, Yao L, Ma JJ, Zhang TY, Bai HH, Suo ZW, Yang X, Hu XD (2020) Analgesic action of adenosine A1 receptor involves the dephosphorylation of glycine receptor alpha1(ins) subunit in spinal dorsal horn of mice. Neuropharmacology, 176108219. https://doi.org/10.1016/j.neuropharm.2020.108219
Li Y, Wu F, Lao LX, Shen XY (2020) Laser irradiation activates spinal adenosine A1 receptor to alleviate osteoarthritis pain in monosodium iodoacetate injected rats. J Integr Neurosci, 19(2), 295–302. https://doi.org/10.31083/j.jin.2020.02.33
Gao X, Lu Q, Chou G, Wang Z, Pan R, Xia Y, Hu H, Dai Y (2014) Norisoboldine attenuates inflammatory pain via the adenosine A1 receptor. Eur J Pain, 18(7), 939–948. https://doi.org/10.1002/j.1532-2149.2013.00439.x
Sawynok J, Reid AR, Liu J (2013) Spinal and peripheral adenosine A(1) receptors contribute to antinociception by tramadol in the formalin test in mice. Eur J Pharmacol, 714(1–3), 373–378. https://doi.org/10.1016/j.ejphar.2013.07.012
Yamamoto S, Nakanishi O, Matsui T, Shinohara N, Kinoshita H, Lambert C, Ishikawa T (2003) Intrathecal adenosine A1 receptor agonist attenuates hyperalgesia without inhibiting spinal glutamate release in the rat. Cell Mol Neurobiol, 23(2), 175–185. https://doi.org/10.1023/a:1022997805525
Holanda AD, Asth L, Santos AR, Guerrini R, de PS-RV, Calo G, Andre E, Gavioli EC (2015) Central adenosine A1 and A2A receptors mediate the antinociceptive effects of neuropeptide S in the mouse formalin test. Life Sci, 1208–12. https://doi.org/10.1016/j.lfs.2014.10.021
By Y, Condo J, Durand-Gorde JM, Lejeune PJ, Mallet B, Guieu R, Ruf J (2011) Intracerebroventricular injection of an agonist-like monoclonal antibody to adenosine A(2A) receptor has antinociceptive effects in mice. J Neuroimmunol, 230(1–2), 178–182. https://doi.org/10.1016/j.jneuroim.2010.07.025
Sawynok J, Reid AR (2012) Caffeine inhibits antinociception by acetaminophen in the formalin test by inhibiting spinal adenosine A(1) receptors. Eur J Pharmacol, 674(2–3), 248–254. https://doi.org/10.1016/j.ejphar.2011.10.036
Yang Y, Zhang H, Lu Q, Liu X, Fan Y, Zhu J, Sun B, Zhao J, Dong X, Li L (2021) Suppression of adenosine A2a receptors alleviates bladder overactivity and hyperalgesia in cyclophosphamide-induced cystitis by inhibiting TRPV1. Biochem Pharmacol, 183114340. https://doi.org/10.1016/j.bcp.2020.114340
Bilkei-Gorzo A, Abo-Salem OM, Hayallah AM, Michel K, Muller CE, Zimmer A (2008) Adenosine receptor subtype-selective antagonists in inflammation and hyperalgesia. Naunyn Schmiedebergs Arch Pharmacol, 377(1), 65–76. https://doi.org/10.1007/s00210-007-0252-9
Zahn PK, Straub H, Wenk M, Pogatzki-Zahn EM (2007) Adenosine A1 but not A2a receptor agonist reduces hyperalgesia caused by a surgical incision in rats: a pertussis toxin-sensitive G protein-dependent process. Anesthesiology, 107(5), 797–806. https://doi.org/10.1097/01.anes.0000286982.36342.3f
Yamaoka G, Horiuchi H, Morino T, Miura H, Ogata T (2013) Different analgesic effects of adenosine between postoperative and neuropathic pain. J Orthop Sci, 18(1), 130–136. https://doi.org/10.1007/s00776-012-0302-0
Hambrecht-Wiedbusch VS, Gabel M, Liu LJ, Imperial JP, Colmenero AV, Vanini G (2017) Preemptive caffeine administration blocks the increase in postoperative pain caused by previous sleep loss in the rat: a potential role for preoptic adenosine A2A receptors in sleep-pain interactions. Sleep, 40(9). https://doi.org/10.1093/sleep/zsx116
Okumura T, Nozu T, Kumei S, Takakusaki K, Miyagishi S, Ohhira M (2016) Adenosine A1 receptors mediate the intracisternal injection of orexin-induced antinociceptive action against colonic distension in conscious rats. J Neurol Sci, 362106–110. https://doi.org/10.1016/j.jns.2016.01.031
Okumura T, Nozu T, Ishioh M, Igarashi S, Kumei S, Ohhira M (2020) Adenosine A1 receptor agonist induces visceral antinociception via 5-HT1A, 5-HT2A, dopamine D1 or cannabinoid CB1 receptors, and the opioid system in the central nervous system. Physiol Behav, 220112881. https://doi.org/10.1016/j.physbeh.2020.112881
Zhang XH, Feng CC, Pei LJ, Zhang YN, Chen L, Wei XQ, Zhou J, Yong Y, Wang K (2021) Electroacupuncture attenuates neuropathic pain and comorbid negative behavior: the involvement of the dopamine system in the amygdala. Front Neurosci, 15657507. https://doi.org/10.3389/fnins.2021.657507
Funding
This study was financially supported by the National Natural Science Foundation of China (NSFC) No. 81973944 and 81503636, the National Natural Science Foundation of Tianjin No.20JCYBJC00200, and the Youth Talent Promotion Project of the Tianjin Association for Science and Technology No. TJSQNTJ-2020–15.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
All authors declare no competing interests.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhou, M., Wu, J., Chang, H. et al. Adenosine signaling mediate pain transmission in the central nervous system. Purinergic Signalling 19, 245–254 (2023). https://doi.org/10.1007/s11302-021-09826-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11302-021-09826-2