Abstract
Objectives
The study was designed to investigate the effects of transcranial magnetic stimulation (TMS) over the dorsolateral prefrontal cortex (DLPFC) on emotional recognition among individuals differentiated on antisocial personality disorder (APD) symptoms.
Methods
Participants (N = 93) received continuous theta burst stimulation (cTBS) under four conditions: real or sham cTBS over the left and right DLPFC. After stimulation, participants performed a dynamic face recognition task depicting fearful, happy, sad, and painful expressions.
Results
Left and right DLPFC stimulation were followed by improved accuracy of happy and painful emotions compared to sham conditions. Participants receiving left stimulation were also better able to recognize sad expressions compared to the left sham condition. A three-way interaction between type of stimulation, emotion recognition, and APD groups suggested that the identified TMS effects on emotion recognition were only significant for individuals at elevated risk for APD symptoms.
Conclusions
Findings suggest that DLPFC stimulation can lead to benefits in emotion recognition among individuals high on APD symptoms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Prefrontal cortex (PFC) impairments have been associated with socio-emotional processing deficits (Adolphs 2002; Coccaro et al. 2011; Shamay-Tsoory et al. 2003). Evidence from neuropsychological research suggests that PFC structures interact with emotional neural circuits that underlie behavioral problems and affect the ability to recognize emotions by inhibiting or modulating their activation (Repple et al. 2017). The involvement of the dorsolateral prefrontal cortex (DLPFC) in cognitive processing of emotions has been evident in head injury and lesion studies, with findings documenting abnormal social-emotional functioning and impaired control of behavior (Fellows and Farah 2004; Butter et al. 1970). In congruence with these studies, noninvasive brain stimulation work demonstrated that modulation of PFC can induce changes on emotional perception and processing (Padberg et al. 2001; Winker et al. 2019). However, evidence for the potential of neuro-stimulation techniques for the treatment of disorders marked by deficits in emotional processing and frontal brain abnormalities (Blair 2013), such as antisocial personality disorder (APD), are lacking in the literature.
According to the DSM-5 (Diagnostic and Statistical Manual – 5th ed.; American Psychiatric Association [APA] 2013), a key feature of APD is a pervasive disregard and violation of the rights of others. There are seven main features of APD consisting of criminal behavior, deceitfulness, impulsivity, aggression and violence, reckless disregard for safety, irresponsibility, and lack of remorse. Individuals characterized by such antisocial behaviors frequently show deficits in emotional processing, recognizing facial expressions, and understanding the social cues of other people, which are essential for normal socialization (Dolan and Fullam 2006; Fanti 2018; Marsh and Blair 2008). Although individuals with antisocial behavior symptoms have deficits in processing both negative and positive facial expressions (Mitchell et al. 2006), it is the ability to understand distress-related cues, especially fearful and sad expressions, that has been shown to play an important role in appropriate interpersonal behaviors (Billeci et al. 2019; Dolan and Fullam 2006). Theoretical models attribute symptoms of antisocial behavior to core deficits in emotion processing that limit the capacity for empathic experience and prevent individuals from generating negative affect responses to aversive stimuli (Decety and Moriguchi 2007; Fanti 2018; Fairchild et al. 2009).
Empirical neuroimaging findings indicate that the emotion recognition deficits of individuals with APD are associated with structural and functional PFC deficits (Anderson and Kiehl 2012; Blair 2013; Raine et al. 1998; Yang and Raine 2009). A meta-analysis of 43 imaging studies linked recognition impairments of specific emotions, such as fear and sadness, among antisocial individuals with functional reductions in various PFC regions, with a stronger effect for the left than right DLPFC (Yang and Raine 2009). Additional work also provided evidence for the importance of the DLPFC during the processing of emotional stimuli, which is deficient among individuals with antisocial behavior symptoms, as well as attention mechanisms for monitoring and resolving conflict among thoughts and feelings (Ochsner and Gross 2005; Posner and Rothbart 2007). Neuro-stimulation might be a promising tool for better understanding the relationship between affect processing and antisociality by altering the function of accessible cortical regions, such as the DLPFC, and observe the effects on emotional tasks (Hartwigsen et al. 2015). Better understanding whether stimulating the PFC may enhance facial affect recognition would inform the limited literature on noninvasive stimulation and may possibly lead to effective interventions among antisocial individuals.
Transcranial magnetic stimulation (TMS) is a promising, non-invasive and low-risk tool to experimentally investigate the causal involvement of the PFC during emotional processing in both healthy individuals and individuals with psychological problems (De Wit et al. 2015; Salehinejad et al. 2017; van Honk et al. 2002). TMS involves administering noninvasive magnetic pulses that temporarily suppress or excite the function of a brain region based on the stimulation pattern, frequency, and intensity (Hallett 2007). As such, TMS is a promising tool for testing hypotheses about the role of PFC regions in cognitive and emotional processing (Schwarzkopf et al. 2011). By altering the function of a prefrontal cortical region, we can simultaneously test whether the target PFC region plays a role in the behavior under observation (Hartwigsen et al. 2015). Importantly, previous studies have used noninvasive brain stimulation over the DLPFC in healthy subjects and clinical populations (with a diagnosis of depression, violent offenders, or borderline personality disorder) and have reported significant beneficial effects on impulsivity, risk-taking, and self-reported aggressiveness (Choy et al. 2018; Molero-Chamizo et al. 2019; Teti-Mayer et al. 2019), which are symptoms of APD.
Studies that explored the effect of repetitive TMS over the DLPFC also showed modification or enhancements during emotion recognition paradigms after treatment. Both left and right DLPFC stimulation has been related to affective modulation and changes to empathic responses (Gamond and Cattaneo 2016; Wang et al. 2014). Results in nonclinical samples indicated that decreasing right DLPFC activation improves attention bias for threatening stimuli and alter emotion-related cognitive processes (Diefenbach et al. 2016). In addition, decreasing right PFC activation has been found to improve inhibitory control of emotion during decision making (Knoch et al. 2006). Other brain stimulation studies that used excitatory stimulation over the left DLPFC indicated a reduction in emotional discomfort while viewing images demonstrating human pain (Boggio et al. 2009; Rego et al. 2015). In summary, these results suggest that both left and right DLPFC stimulation might affect emotional processing although the differential role of DLPFC hemispheres is still unclear.
A promising and newer patterned form of TMS is theta-burst stimulation (TBS), which applies 50-Hz stimulation repeated with a rate in the theta range of five times per second (Huang et al. 2005). TBS is a novel stimulation pattern shown to induce significant and long-lasting neuronal conditioning responses in motor cortical studies, while electro-physiological effects in the PFC have also been observed (Grossheinrich et al. 2009). Intermittent train of TBS (iTBS) induces cortical facilitation, whereas continuous train of TBS (cTBS) decreases cortical excitability (Huang et al. 2005). Given the current evidence base, this novel pattern of stimulation, which received its FDA approval in 2018 for the treatment of depression (Blumberger et al. 2018), allows a treatment session to last less than 15 min compared to standard treatment sessions that last for about 40–50 min (Chung et al. 2015). In depression, evidence for the effectiveness of excitatory TBS and non-inferiority to conventional TMS protocols exists but remain weak in other mental disorders (Chen et al. 2019). Nevertheless, TBS remains a promising instrument to target maladaptive brain networks because it is a more convenient intervention for patients and it is certainly a technique more affordable to treat a larger number of people. The clinical relevance of TBS has been less systematically tested especially on PFC regions such as the DLPFC, which is a main aim of the current study.
Although limited, studies that used specifically theta burst protocols over the DLPFC also provided evidence supporting that inhibitory cTBS may enhance emotional processing (e.g., Engelen et al. 2018). Recently, the impact of cTBS that reduces neuronal excitability in the DLPFC was examined using electroencephalography during emotional face processing (Cao et al. 2018). Findings indicated that inhibitory cTBS does affect emotional processing, and this effect was observed in changes in electric patterns in the brain and specifically on alpha band oscillations (Cao et al. 2018). In this study, the authors showed that cTBS delivered over the right DLPFC decreased alpha power oscillations, pointing to increased activity at the cortical level during the presentation of happy facial emotional stimuli (also see Coan and Allen 2004). In another recent study that applied cTBS over the DLPFC during affective processing, right inhibition enhanced occipito-parietal brain activity for both subliminal and supraliminal negative images compared to neutral (Keuper et al. 2018). Adding to these findings, inhibitory TMS has also been found to modulate early affective processing and reaction times for fearful faces in a facial expression identification task (Zwanzger et al. 2014). Thus, inhibitory TMS or cTBS may be promising stimulation techniques to boost processing and attention to emotional stimuli. However, it is still unknown whether these techniques could be used to enhance emotional processing among individuals with antisocial behavior, an aim of the current study.
Current study
In the current study, we used an experimental design involving both active and sham TMS conditions to investigate differences in emotion recognition. Sham TMS mimics the sensory effects of active TMS without actual stimulation of the brain (Paulus 2005; Vallence et al. 2015). Participants were blinded to condition (real versus sham) and after stimulation completed a computerized face recognition task. By doing so, we aimed to shed light on the possible causal role of the left and right DLPFC in emotional processing. In addition, we investigated whether inhibitory cTBS over the right and left DLPFC had a differential impact on the emotion recognition of individuals at low or high risk for APD symptoms. This is of great importance because there are no previous studies comparing right and left DLPFC stimulation that simultaneously tests for the effects of antisocial behavior symptoms on emotional stimuli.
In addition to testing differences on the importance of right and left DLPFC for emotion recognition, we also investigated the effects of cTBS on both positive and negative emotions. The asymmetric inhibition model of hemispheric differences, proposed by Grimshaw and Carmel (2014), has suggested that dominance of the right-hemisphere activity is related with reduced responses to approach-related (positive) stimuli and dominance of the left-hemisphere activity with reduced responses to withdrawal (negative) stimuli. Based on this model, we hypothesized that cTBS inhibition over the right DLPFC might result in better accuracy of positive expressions, whereas cTBS inhibition over the left DLPFC might result in increased accuracy of negative emotional expressions. Furthermore, we hypothesized that active stimulation would improve emotion recognition among individuals with high levels of APD symptoms compared to those with low levels, since emotion recognition deficits are more pronounced among antisocial individuals (Dawel et al. 2012).
Finally, we aim to test whether anxiety, depression, and callous-unemotional traits might be important covariates in the effects of TMS. Although a single-session of TMS is usually not found to acutely affect mood in healthy volunteers (Baeken et al. 2006), it has been reported that mood and anxiety levels prior to stimulation (perhaps related to expectations concerning the TMS procedures) affects both cognitive-affective and cortisol responses to TMS (Baeken et al. 2011; Vanderhasselt et al. 2011). Thus, anxiety and depression might influence the effects of TMS on emotion recognition. In addition, callous-unemotional traits have been associated with emotional deficits among adolescents and young adults high on antisocial behavior (Kimonis et al. 2013; Kyranides et al. 2016), suggesting that these traits might explain the association of APD symptoms with emotion recognition deficits.
Methods
Participants
Ninety-three young adults (31 males, Mage = 22.10, SD = 1.54, Age range 18–26; 62 females, Mage = 20.61, SD = 1.34, age range 18–23) were recruited for the purpose of the current study. They were medication-free, right-handed and had normal vision (for computer tasks). All invited participants completed the cTBS session. Exclusion criteria included history of psychiatric/neurological disorders including epilepsy, head trauma and migraine. One female participant was excluded from the current sample because of the use of antidepressant medication. The study was approved by the Cyprus National Bioethics committee.
Procedure
This study used a double-blind, randomized, sham-controlled design, where participants were randomly assigned to one of four different stimulation conditions: left cTBS (N = 23), right cTBS (N = 23), left sham (N = 24), and right sham (N = 23). Participants that met preliminary inclusion criteria began with an overview of the study and completed a written informed consent. The procedure was driven by the experimenter so that a quarter of the participants were assigned to the “blue,” “green,” “yellow,” and “orange” group (unknown stimulation condition to the participant). Male and female participants were pseudo-randomly assigned to a color-group according to the order of arrival at the lab. Participants were told that they belong to the color-group indicated by the card they had chosen and that they will be presented with a face recognition task of different emotions after receiving a short TMS stimulation session (40 s). Prior to the experiment, all participants were asked to complete a battery of Self-Report measures. Self-report assessment was followed by cTBS and then the emotion recognition task. Immediately after stimulation, participants were comfortably seated in front of a 19′ computer screen (1024 × 768) at an approximate distance of 80 cm. Participants first completed a training phase (120 s) of the task, to allow themselves to familiarize with the overall procedure. Faces were presented in random order and the E-Prime 2.0 software (Psychology Software Tools, Pittsburg, PA) was used for stimulation presentation and data collection.
cTBS protocol—real and sham cTBS
Coil positioning was determined using standardized coordinates from the EEG (Steinmetz et al. 1989) International 10–20 system (with F4 corresponding to the right DLPFC stimulation target and F3 corresponding to the left DLPFC). The location and orientation of each participant’s coil placement was indicated on a nylon cap that participants wore throughout the single stimulation session. A figure-of-eight focal coil (70 mm diameter) was used. The coil was held in a fixed position by a mechanical arm and oriented so that the induced electric current flowed in a posterior–anterior direction. Stimulus intensities were set at 70% of active motor threshold (AMT). We chose to use 70% intensity to prevent intense facial muscle twitching during stimulation. In addition, previous experiments that used cTBS found significant inhibitory effects using as stimulation intensity 70% of the AMT (Goldsworthy et al. 2015; McAllister et al. 2009). Each stimulation session TBS burst consisted of 3 pulses at 50 Hz, with each train being repeated every 200 ms (5 Hz) for a duration of 40 s (600 pulses). It has been shown that this stimulation paradigm suppresses cortical excitability. The number of pulses per participant used in the present study is consistent with the prototype protocol (see Huang et al. 2005).
Sham stimulation was delivered using an identical with the real Magstim figure-of-eight focal sham coil (70 mm diameter) that also produced identical stimulation noise. Sham Magstim figure-of-eight coil have been found to induce nearly zero electric-field under the coil’s center (Chistyakov et al. 2015; Smith and Peterchev 2018), which make it a credible placebo procedure. The coil was held in a fixed position by a mechanical arm and oriented so that the induced electric current flowed in a posterior–anterior direction. Stimulus intensities were the same with the real stimulation condition and the same positioning procedure was followed using the 10–20 system for all participants.
Experimental task
Face recognition task
A dynamic version of an emotion recognition task was created using standardized stimuli of dynamic, prototypical facial expressions from the Montréal Pain and Affective Face Clips (MPAFC) database (see Simon et al. 2008). Participants viewed a series of 96 1-s dynamic visual stimuli depicting a man or a woman (48 of each sex), whose facial expression morphed from neutral to one of four basic expressions: fear, happiness, sadness, and pain (24 facial expressions were shown for each emotion). Eight clips were presented in random order for each emotion. Individuals viewed facial expressions on a computer screen and were instructed to label each emotion on a keyboard. After a practice phase consisting of each of the four expressions, participants were presented with the test stimuli in random order. Participants were scored according to whether or not they correctly identified the facial expression depicted (Bentler 1990), and the final outcome variable used in the analysis was the number of accuracy errors that could range from 0 to 24 for each emotion.
Self-report measures
The Adult Self-Report Inventory-4 (ASRI-4; Gadow et al. 2004) was used to assess APD, generalized anxiety, and depression symptoms as defined in the DSM-5 (APA 2013). Symptoms on the ASRI-4 are rated on a 4-point Likert-type scale ranging from 0 (never) to 3 (very often). The items were summed to create overall APD (α = 0.78; 7 items; e.g., “I do things that I could get arrested for;” “I start fights”), anxiety (α = 0.86; 6 items; e.g., “I have trouble getting myself to stop worrying”), and depression (α = 0.81; 9 items; e.g., “I feel unhappy or sad”) symptom scores for the purposes of the current study. Research with clinical, college, and community samples has demonstrated that scores on the ASRI-4 show convergent and discriminant validity (Gadow et al. 2007; Kyranides et al. 2019; Kyranides et al. 2017). Young adult APD symptoms assessed with ASRI-4 have been associated with conduct disorder symptoms during adolescence, pointing to continuity over time (Kyranides et al. 2019). Even though behavioral symptoms of specific disorders are included in the ASRI-4, it does not provide additional diagnostic criteria; therefore, the responses do not indicate a clinical diagnosis but a continuity in symptom severity.
The Inventory of Callous–Unemotional Traits (ICU; Frick 2004), which is designed to assess self-reported callous–unemotional (CU) traits, was also administered. The ICU comprises of 24 items (α = 0.80; e.g., “The feelings of others are important to you” reverse coded) that are rated on a 4-point Likert scale ranging from 0 (not at all true) to 3 (definitely true). CU traits, measured with the ICU, have been associated with aggression, delinquency, psychosocial and psychophysiological impairment (Fanti 2013; Fanti et al. 2017). Previous research has provided evidence for the validity of ICU scores in community and college samples of young adults (Fanti et al. 2016; Kimonis et al. 2015).
Plan of analysis
Similar to prior work (e.g., Coid and Ullrich 2010), median split of the data was conducted in IBM SPSS 20.0 on the basis of participants ASRI-4 pre-stimulation scores, in order to recode the continuous APD variable into a categorical one. Independent sample t-tests were used to compare the identified groups on APD symptoms, co-occurring psychopathologies and callous unemotional traits. To address our main aim, we conducted repeated measures ANOVA in IBM SPSS 20.0 with type of stimulation and APD groups as the between-group independent variables and accuracy errors as the within-subjects factor. Before proceeding with the main analysis, we tested if anxiety, depression and callous-unemotional traits were significant covariates. For all analyses, significant interactions and repeated effects are depicted in graphs.
Results
APD groups
Individuals above the median on APD symptoms (N = 38; M = 3.06; SD = 1.35), labeled “High APD,” greatly differed in severity of symptoms compared to those below the median (N = 55; M = 0.34; SD = 0.48, t(91) = 13.73, p < .001), labeled “Low APD.” In addition, low and high APD groups differed on internalizing psychopathologies, including depression and anxiety, and callous-unemotional (CU) traits. t Test results provided evidence that there were significant differences between high APD and low APD groups on depression, t(91) = 3.72, p < .001, anxiety, t(91) = 3.68, p < .001, and CU traits, t(91) = 3.34, p < .001 (mean scores are reported in Table 1). Because the identified groups differed in these measures, these variables were tested as potential covariates in further analysis.
TMS stimulation results
Repeated measures ANOVA was conducted in IBM SPSS 20.0 with type of stimulation and APD groups as the between-group independent variables and accuracy errors as the within-subjects factor. Before proceeding with the analysis, we tested for potential covariates as well as main and interactive effects of gender. Neither anxiety, F(1, 82) = 0.05, p = .82, nor depression, F(1, 82) = 0.46, p = .50, nor CU traits, F(1, 82) = 0.60, p = .44, were significant covariates. Thus, although the high APD group differed from the low APD group on anxiety, depression, and CU traits, these variables did not explain potential associations in the repeated measures ANOVA. In addition, no main, F(1, 77) = 0.05, p = .83, or interactive effects of gender (F ranged from 0.62 to 1.76) were identified. As a result, these variables were excluded from further analysis.
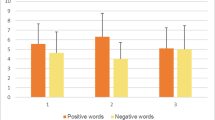
Findings from the repeated measures ANOVA suggested a significant within-groups effect for accuracy errors, F(3, 255) = 58.23, p < .001, η2 = 0.41, indicating that participants showed lower accuracy errors during happy (M = 0.68, SE = 0.11) compared to fear (M = 6.10, SE = 0.41; p < .001), pain (M = 5.39, SE = 0.44; p < .001), and sad (M = 5.34, SE = 0.35; p < .001) facial expressions. Between-group differences for type of stimulation were also identified, F(3, 85) = 3.66, p < .05, η2 = 0.13. On average, participants receiving left stimulation showed lower overall accuracy errors (see Fig. 1: average) compared to both sham conditions. Importantly, an interaction between accuracy errors and type of stimulation was identified, F(9, 255) = 2.19, p < .05, η2 = 0.07. As shown in Fig. 1, those receiving stimulation (both left and right) scored lower on accuracy errors for happy emotions compared to the sham left group, and lower on accuracy errors for pain emotions compared to the sham right group. Finally, participants receiving left stimulation scored lower on accuracy errors in response to sad facial expressions compared to the left sham group.
Effects of APD groups
Participants high on APD symptoms in general made more errors (M = 4.96, SE = 0.34) compared to those low on APD (M = 3.80, SE = 0.27; d = 0.60; p < .05), F(1,85) = 6.73, p < .05, η2 = 0.08. However, according to a two-way interaction between APD groups and type of stimulation (Fig. 2), F(3,85) = 3.38, p < .05, η2 = 0.12, this difference was only significant for the sham condition, but not for the stimulation conditions. These findings indicate that TMS stimulation decreased the difference in accuracy between APD groups. Additionally, we identified a three-way interaction between accuracy errors, type of stimulation and APD groups, F(9, 255) = 2.04, p < 0.05, η2 = 0.08. Figure 3 shows the differences in accuracy errors by type of stimulation for low (see Fig. 3a) and high (see Fig. 3b) APD groups. Findings suggested that none of the identified differences reported in Fig. 1 were significant among participants in the low APD group (Fig. 3a); however, these differences remained significant for the high APD group (see Fig. 3b). One of the reasons, as evident in Fig. 3, might be that in general participants in the low APD group scored low on accuracy errors irrespective of stimulation or sham condition (scores for happy emotions ranged from 0.24 to 0.48 and for negative emotions from 4 to 5.93); however, this was not the case for the high APD group. As depicted in Fig. 3, the majority of the differences among stimulation groups for happy, pain, and sad emotions identified for the overall sample were specific to the high APD group. The main difference was that only participants high on APD receiving left stimulation differed from those in the right sham condition in response to pain emotions. Interestingly, individuals receiving left stimulation scored lower on accuracy errors in response to fear expressions compared to other stimulation groups, although these differences only approached significance (p < .10).
Discussion
The present study investigated the impact of inhibitory cTBS over the right and left DLPFC on facial emotion processing during the presentation of fearful, sad, happy, and painful facial expressions. Our results showed that both left and right DLPFC stimulation was followed by better emotion recognition performance as demonstrated by lower accuracy errors for happy emotions compared to the sham left group, and lower accuracy errors for painful emotions compared to the sham right group. In addition, participants receiving left stimulation showed higher accuracy rates in response to sad facial expressions compared to the left sham group. Importantly, findings suggested that differences in accuracy rates remained significant only for the high APD group. Specifically, individuals in the high, but not the low, APD group showed better emotion recognition performance when receiving real compared to sham stimulation over the left DLPFC for happy, painful and sad emotions. High APD individuals also showed higher accuracy rates when receiving right DLPFC stimulation to happy expressions compared to sham conditions. Findings also indicated that on average TMS stimulation decreased the differences in accuracy ratings identified among individuals with low versus elevated APD symptoms.
The lateral division of the human brain into the left and right hemispheres underlies asymmetries in both structure and function across a broad range of cognitive and emotional processes. Our results partially agree with the asymmetric inhibition model (Grimshaw and Carmel 2014), since cTBS inhibition over the left, but not the right, DLPFC resulted in increased accuracy of negative expressions. However, it should be pointed out that besides the asymmetric inhibition model, a number of other theories have been proposed. One model used to explain the brain hemispheres role on emotion, which has been supported by several studies, is the right hemisphere hypothesis for emotion lateralization (Borod et al. 1998; Alves et al. 2008). Numerous clinical studies assessing patients with unilateral brain damage have found that right hemisphere damage is more likely to cause emotion-processing deficits than left hemisphere damage (e.g., Abbott et al. 2014; Harciarek et al. 2006). In contrast, the valence hypothesis proposes that the right hemisphere controls negative emotions, whereas the left hemisphere controls positive emotions (see Demaree et al. 2005; Tamietto et al. 2006). Further, the approach-withdrawal model proposed that the left hemisphere controls approach-related behaviors, and the right hemisphere avoidance-related behaviors (see Rutherford and Lindell 2011). Overall, it seems that the specific nature of the lateral division of emotion control remains controversial.
An important contribution of the current study, which is in accordance with the majority of the above-mentioned models, is the finding that both left and right DLPFC regions are involved in emotion processing. A possible explanation for this effect can be derived from recent findings, which suggested that inhibitory repetitive TMS of the DLPFC can modulate selective attention to emotional stimuli (Zwanzger et al. 2014). Apart from the present study, DLPFC inhibition has been associated with enhanced responses to angry compared to neutral stimuli (Engelen et al. 2018) and enhance brain activity in response to happy emotional faces (Cao et al. 2018). Using inhibitory TMS, van Honk et al. (2002) found that the left and right PFC were involved in reducing the vigilant emotional response to unmasked versions of emotional faces, suggesting an important role in emotional processing. However, these studies did not include facial expressions depicting different emotions, and differed from the present study with respect to the experimental task employed to asses facial recognition processes. Our results provided an important contribution to the experimental TMS research by evidencing the involvement of the left and right PFC for recognition processes of distinct emotional expressions. Left DLPFC stimulation contributed to improved recognition accuracy of pain and sadness and both left and right stimulation improved recognition accuracy to happiness.
Furthermore, our findings suggest that modulating the left DLPFC with cTBS may play a role in increasing emotion recognition of different facial expressions among individuals with antisocial symptoms. The significant interaction between groups (high versus low APD) and emotion recognition, suggested that only the high APD group receiving active left cTBS showed better performance compared to sham conditions during painful, sad, and happy facial expression stimuli. Compared to the low risk group, those in the high APD group also showed less accuracy errors in response to happy faces after right DLPFC inhibition. Antisocial symptoms in general have been associated with hypo-sensitivity to others’ distress and empathy-eliciting information (Fanti 2018). Further, individuals with behavioral problems demonstrate deficits in processing facial expressions associated with both negative and positive emotions (Mitchell et al. 2006). Recent studies also suggested that high levels of antisocial traits are related with impairments on processing the salient aspects of emotional facial stimuli (i.e., eyes) and especially emotions associated with sadness and fear (Fanti et al. 2016; Kimonis et al. 2015; Kyranides et al. 2019). It is possible that by modulating the atypical pattern of neural activity of individuals with APD while viewing others emotional expressions may result in positive emotional and behavioral changes. However, this is only a hypothesis that should be explored in future studies, especially since we are not aware of any previous work that applied TMS or cTBS as an intervention for emotional processing deficits among individuals with APD or antisocial behavior.
Nevertheless, our results supported the view that cTBS could play an important role in tackling some of the problems observed among individuals with antisocial symptoms related to emotional processing. In terms of clinical implications, these results suggest that TMS may be a potential clinical tool to facilitate emotional processing to happy but also sad and painful emotions. In the context of a single session, we could observe a cTBS related effect on improving accuracy errors for facial expressions. Regarding the participation of the left and the right DLPFC hemispheres in emotional processing, current results indicate that both regions were involved in emotional processing with an effect of the right DLPFC in response to happy faces and an effect of the left DLPFC in response to happy, painful and sad expressions. The results may also allow for a speculation regarding the mechanisms by which cTBS contributes to improved emotional accuracy, which is via inhibitory effects on DLPFC. Agreeing with this suggestion, previous studies of reappraisal of negative emotional stimuli have found activations in a number of prefrontal cortical areas, reductions of amygdala activity, and changes in evaluations of the value of emotional stimuli or situations (Baeken et al. 2010; Etkin et al. 2011; Wager et al. 2008). At this point, this suggestion remains a speculation that will need to be further investigated in future studies with designs that allow such hypothesis testing.
Limitations, strengths, future directions, and conclusions
Potential limitations of our study also need to be discussed. A critical issue concerns the interpretation of our results with respect to the lack of baseline testing on the emotional recognition task. We measured facial recognition accuracy responses only after stimulation. Replicating the identified differences between groups receiving real and sham stimulation, with comparisons before and after stimulation will provide additional evidence about the cTBS effects on emotion recognition. Moreover, considering that the female participants in our sample outnumbered male participants and that participants were healthy individuals without an APD diagnosis, generalization of the present findings is limited. Therefore, this study is in need of replication in a sample with more male subjects, clinically diagnosed with APD. However, the identified APD groups in our study greatly differed in severity of symptoms. In addition, we compared the identified groups on co-occurring psychopathologies and callous-unemotional traits, finding that the groups scoring high on APD symptoms were at greater risk for both internalizing problems and psychopathic traits. These findings agree with prior work that APD increases the risk of anxiety and depression, which leads to societal maladjustment, substance use, and suicidal ideation (Goodwin and Hamilton 2003). Further, prior work using similar samples verified the strong association between callous-unemotional traits and the diagnosis of APD, suggesting that APD relates to low empathy and lower sympathy for others (Kimonis et al. 2013; Kyranides et al. 2019). Finding that the high APD group in the current study is characterized by co-occurring internalizing problems and CU traits suggest that these individuals might be at greatest need for intervention. Nevertheless, none of these variables were significant covariates, indicating that the identified effects were due to cTBS.
Another limitation is the lack of neuroimaging data to demonstrate the effects of cTBS in other brain areas beside the DLPFC. In addition, conducting multi-session cTBS at both left and right DLPFC would help to elucidate the impact of this type of stimulation and understand its long-term effects in modulating emotion processing more fully. Future pilot studies that combine multi-session designs, neuroimaging, and neuromodulation methods are essential for informing effective interventions. Despite the limitations, the current study is among the first to consider left and right DLPFC stimulation and sham conditions, with a larger sample size compared to the majority of prior TMS work.
It is also important to consider the possibility that TMS could be used to strengthen the effects of existing behavioral or cognitive interventions as well. One example for future investigations is attention modification therapy (AMT) towards emotional stimuli combined with TMS since our findings indicate that cTBS may boost emotion recognition. AMT is a novel treatment approach based on cognitive neuroscience research (Bar-Haim 2010) and can be delivered cheaply and safely to large numbers of children and adults. Combining TMS with AMT may be an interesting intervention opportunity for altering attention bias towards emotional stimuli through which noninvasive brain stimulation could have the potential to become an enhancing tool. Furthermore, we investigated the effects of cTBS over both PFC hemispheres and identified that both left and right stimulation was followed by better emotion recognition. Importantly, the identification of such clinical effects of different protocols, in this case cTBS, can be used to minimize the adverse effects of pharmacology interventions. In fact, TMS is used for patients with resistant depression that do not respond to drug treatment (Perera et al. 2016). Moreover, so far only standard inhibitory and excitatory stimulation have been used in clinical practice, without customizing the choice of different and more novel protocols such as TBS according to a patient’s specific clinical profile or imaging-based estimates of dysregulation. Getting to know better the effects of novel protocols will give the chance to clinicians in collaboration with TMS technicians to choose among a variety of stimulation protocols that are most appropriate to the needs of each patient.
This study takes a step towards advancing knowledge about neural mechanisms that regulate emotional processing. Furthermore, our findings help in clarifying that treatment programs for antisocial behaviors may benefit by considering noninvasive brain stimulation techniques. Among other etiological mechanisms, the role of neural impairments on the development of antisocial behavior has been increasingly acknowledged (Fanti et al. 2019; Raine et al. 1998; Van Goozen and Fairchild 2008). Our findings further suggested that left stimulation affected emotion recognition of others’ pain, sadness, and happiness, whereas right stimulation affected emotion recognition of others’ happiness. These findings may have clinical implications for the application of TMS. In addition, current findings may advance our understanding of the networks involved in the emotional processing of facial stimuli, which possibly relate to differences in cognitive and affective empathy. Although additional evidence is needed, our novel findings suggest that the modulation of the right and left DLPFC can affect emotion recognition and may help on targeting atypical neural responses in antisocial populations.
References
Abbott, J. D., Wijeratne, T., Hughes, A., Perre, D., & Lindell, A. K. (2014). The influence of left and right hemisphere brain damage on configural and featural processing of affective faces. Laterality: Asymmetries of Body, Brain and Cognition, 19(4), 455–472.
Adolphs, R. (2002). Neural systems for recognizing emotion. Current Opinion in Neurobiology, 12, 169–177.
Alves, N. T., Fukusima, S. S., & Aznar-Casanova, J. A. (2008). Models of brain asymmetry in emotional processing. Psychology & Neuroscience, 1(1), 63.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders: DSM-5.
Anderson, N. E., & Kiehl, K. A. (2012). The psychopath magnetized: Insights from brain imaging. Trends in Cognitive Sciences, 16, 52–60.
Baeken, C., Leyman, L., De Raedt, R., Vanderhasselt, M. A., & Dhaenen, H. (2006). Lack of impact of repetitive high frequency transcranial magnetic stimulation on mood in healthy female subjects. Journal of Affective Disorders, 90(1), 63–66.
Baeken, C., De Raedt, R., Van Schuerbeek, P., Vanderhasselt, M. A., De Mey, J., Bossuyt, A., & Luypaert, R. (2010). Right prefrontal HF-rTMS attenuates right amygdala processing of negatively valenced emotional stimuli in healthy females. Behavioural Brain Research, 214, 450–455.
Baeken, C., Vanderhasselt, M. A., & De Raedt, R. (2011). Baseline ‘state anxiety’influences HPA-axis sensitivity to one sham-controlled HF-rTMS session applied to the right dorsolateral prefrontal cortex. Psychoneuroendocrinology, 36(1), 60–67.
Bar-Haim, Y. (2010). Research review: Attention bias modification (ABM): A novel treatment for anxiety disorders. Journal of Child Psychology and Psychiatry, 51(8), 859–870.
Bentler, P. M. (1990). Comparative fit indexes in structural models. Psychological Bulletin, 107, 238–246.
Billeci, L., Muratori, P., Calderoni, S., Chericoni, N., Levantini, V., Milone, A., et al. (2019). Emotional processing deficits in Italian children with disruptive behavior disorder: The role of callous unemotional traits. Behaviour Research and Therapy, 113, 32–38.
Blair, R. J. R. (2013). The neurobiology of psychopathic traits in youths. Nature Reviews Neuroscience, 14(11), 786–799.
Blumberger, D. M., Vila-Rodriguez, F., Thorpe, K. E., Feffer, K., Noda, Y., Giacobbe, P., et al. (2018). Effectiveness of theta burst versus high-frequency repetitive transcranial magnetic stimulation in patients with depression (THREE-D): A randomised non-inferiority trial. The Lancet, 391(10131), 1683–1692.
Boggio, P. S., Zaghi, S., & Fregni, F. (2009). Modulation of emotions associated with images of human pain using anodal transcranial direct current stimulation (tDCS). Neuropsychologia, 47, 212–217.
Borod, J. C., Cicero, B. A., Obler, L. K., Welkowitz, J., Erhan, H. M., Santschi, C., et al. (1998). Right hemisphere emotional perception: Evidence across multiple channels. Neuropsychology, 12(3), 446.
Butter, C. M., Snyder, D. R., & McDonald, J. A. (1970). Effects of orbital frontal lesions on aversive and aggressive behaviors in rhesus monkeys. Journal of Comparative and Physiological Psychology, 72, 132.
Cao, D., Li, Y., Niznikiewicz, M. A., Tang, Y., & Wang, J. (2018). The theta burst transcranial magnetic stimulation over the right PFC affects electroencephalogram oscillation during emotional processing. Progress in Neuro-Psychopharmacology and Biological Psychiatry, 82, 21–30.
Chen, X., Ji, G. J., Zhu, C., Bai, X., Wang, L., He, K., et al. (2019). Neural correlates of auditory verbal hallucinations in schizophrenia and the therapeutic response to theta-burst transcranial magnetic stimulation. Schizophrenia Bulletin, 45(2), 474–483.
Chistyakov, A. V., Kreinin, B., Marmor, S., Kaplan, B., Khatib, A., Darawsheh, N., et al. (2015). Preliminary assessment of the therapeutic efficacy of continuous theta-burst magnetic stimulation (cTBS) in major depression: A double-blind sham-controlled study. Journal of Affective Disorders, 170, 225–229.
Choy, O., Raine, A., & Hamilton, R. H. (2018). Stimulation of the prefrontal cortex reduces intentions to commit aggression: a randomized, double-blind, placebo-controlled, stratified, parallel-group trial. Journal of Neuroscience, 38, 6505–6512.
Chung, S. W., Hoy, K. E., & Fitzgerald, P. B. (2015). Theta-burst stimulation: A new form of TMS treatment for depression? Depression and Anxiety, 32(3), 182–192.
Coan, J. A., & Allen, J. J. (2004). Frontal EEG asymmetry as a moderator and mediator of emotion. Biological Psychology, 67(1–2), 7–50.
Coccaro, E. F., Sripada, C. S., Yanowitch, R. N., & Phan, K. L. (2011). Corticolimbic function in impulsive aggressive behavior. Biological Psychiatry, 69, 1153–1159.
Coid, J., & Ullrich, S. (2010). Antisocial personality disorder is on a continuum with psychopathy. Comprehensive Psychiatry, 51(4), 426–433.
Dawel, A., O’Kearney, R., McKone, E., & Palermo, R. (2012). Not just fear and sadness: Meta-analytic evidence of pervasive emotion recognition deficits for facial and vocal expressions in psychopathy. Neuroscience & Biobehavioral Reviews, 36(10), 2288–2304.
De Wit, S. J., Van der Werf, Y. D., Mataix-Cols, D., Trujillo, J. P., Van Oppen, P., Veltman, D. J., & van den Heuvel, O. A. (2015). Emotion regulation before and after transcranial magnetic stimulation in obsessive compulsive disorder. Psychological Medicine, 45, 3059–3073.
Decety, J., & Moriguchi, Y. (2007). The empathic brain and its dysfunction in psychiatric populations: Implications for intervention across different clinical conditions. BioPsychoSocial medicine, 1, 22.
Demaree, H. A., Everhart, D. E., Youngstrom, E. A., & Harrison, D. W. (2005). Brain lateralization of emotional processing: Historical roots and a future incorporating “dominance”. Behavioral and Cognitive Neuroscience Reviews, 4(1), 3–20.
Diefenbach, G. J., Assaf, M., Goethe, J. W., Gueorguieva, R., & Tolin, D. F. (2016). Improvements in emotion regulation following repetitive transcranial magnetic stimulation for generalized anxiety disorder. Journal of Anxiety Disorders, 43, 1–7.
Dolan, M., & Fullam, R. (2006). Face affect recognition deficits in personality-disordered offenders: Association with psychopathy. Psychological Medicine, 36(11), 1563–1569.
Engelen, T., Zhan, M., Sack, A. T., & de Gelder, B. (2018). Dynamic interactions between emotion perception and action preparation for reacting to social threat: A combined cTBS-fMRI study. eNeuro, 5(3).
Etkin, A., Egner, T., & Kalisch, R. (2011). Emotional processing in anterior cingulate and medial prefrontal cortex. Trends in Cognitive Sciences, 15, 85–93.
Fairchild, G., Van Goozen, S. H., Calder, A. J., Stollery, S. J., & Goodyer, I. M. (2009). Deficits in facial expression recognition in male adolescents with early-onset or adolescence-onset conduct disorder. Journal of Child Psychology and Psychiatry, 50, 627–636.
Fanti, K. A. (2013). Individual, social, and behavioral factors associated with co-occurring conduct problems and callous-unemotional traits. Journal of Abnormal Child Psychology, 41, 811–824.
Fanti, K. A. (2018). Understanding heterogeneity in conduct disorder: A review of psychophysiological studies. Neuroscience & Biobehavioral Reviews, 91, 4–20.
Fanti, K. A., Panayiotou, G., Lombardo, M. V., & Kyranides, M. N. (2016). Unemotional on all counts: Evidence of reduced affective responses in individuals with high callous-unemotional traits across emotion systems and valences. Social Neuroscience, 11, 72–87.
Fanti, K. A., Kyranides, M. N., Georgiou, G., Colins, O. F., Tuvblad, C., & Andershed, H. (2017). Callous-unemotional, impulsive-irresponsible, and grandiose-manipulative traits: Distinct associations with heart rate, skin conductance, and startle responses to violent and erotic scenes. Psychophysiology, 54(5), 663–672. https://doi.org/10.1111/psyp.12837.
Fanti, K. A., Konikkou, K., Cohn, M., Popma, A., & Brazil, I. A. (2019). Amygdala functioning during threat acquisition and extinction differentiates antisocial subtypes. Journal of neuropsychology.
Fellows, L. K., & Farah, M. J. (2004). Different underlying impairments in decision-making following ventromedial and dorsolateral frontal lobe damage in humans. Cerebral Cortex, 15, 58–63.
Frick, P. J. (2004). The inventory of callous-unemotional traits. Unpublished rating scale.
Gadow, K. D., Sprafkin, J., & Weiss, M. (2004). Adult self-report inventory-4 manual. Stony Brook, NY: Checkmate Plus.
Gadow, K. D., Sprafkin, J., Schneider, J., Nolan, E. E., Schwartz, J., & Weiss, M. D. (2007). ODD, ADHD, versus ODD+ ADHD in clinic and community adults. Journal of Attention Disorders, 11, 374–383.
Gamond, L., & Cattaneo, Z. (2016). The dorsomedial prefrontal cortex plays a causal role in mediating in-group advantage in emotion recognition: A TMS study. Neuropsychologia, 93, 312–317.
Goldsworthy, M. R., Müller-Dahlhaus, F., Ridding, M. C., & Ziemann, U. (2015). Resistant against de-depression: LTD-like plasticity in the human motor cortex induced by spaced cTBS. Cerebral Cortex, 25(7), 1724–1734.
Goodwin, R. D., & Hamilton, S. P. (2003). Lifetime comorbidity of antisocial personality disorder and anxiety disorders among adults in the community. Psychiatry Research, 117(2), 159–166.
Grimshaw, G. M., & Carmel, D. (2014). An asymmetric inhibition model of hemispheric differences in emotional processing. Frontiers in Psychology, 5, 489.
Grossheinrich, N., Rau, A., Pogarell, O., Hennig-Fast, K., Reinl, M., Karch, S., et al. (2009). Theta burst stimulation of the prefrontal cortex: Safety and impact on cognition, mood, and resting electroencephalogram. Biological Psychiatry, 65(9), 778–784.
Hallett, M. (2007). Transcranial magnetic stimulation: a primer. Neuron, 55, 187–199.
Harciarek, M., Heilman, K. M., & Jodzio, K. (2006). Defective comprehension of emotional faces and prosody as a result of right hemisphere stroke: Modality versus emotion-type specificity. Journal of the International Neuropsychological Society, 12(6), 774–781.
Hartwigsen, G., Bergmann, T. O., Herz, D. M., Angstmann, S., Karabanov, A., Raffin, E., et al. (2015). Modeling the effects of noninvasive transcranial brain stimulation at the biophysical, network, and cognitive level. Progress in Brain Research, 222, 261–287.
Huang, Y. Z., Edwards, M. J., Rounis, E., Bhatia, K. P., & Rothwell, J. C. (2005). Theta burst stimulation of the human motor cortex. Neuron, 45, 201–206.
Keuper, K., Terrighena, E. L., Chan, C. C., Junghoefer, M., & Lee, T. (2018). How the dorsolateral prefrontal cortex controls affective processing in absence of visual awareness–insights from a combined EEG-rTMS study. Frontiers in Human Neuroscience, 12, 412.
Kimonis, E. R., Branch, J., Hagman, B., Graham, N., & Miller, C. (2013). The psychometric properties of the inventory of callous–unemotional traits in an undergraduate sample. Psychological Assessment, 25(1), 84.
Kimonis, E. R., Fanti, K. A., Frick, P. J., Moffitt, T., Essau, C., Bijttebier, P., & Marsee, M. A. (2015). Using self-reported callous-unemotional traits to cross-nationally assess the DSM-5 “with limited prosocial emotions” specifier. Journal of Child Psychology and Psychiatry, 56, 1249–1261.
Knoch, D., Pascual-Leone, A., Meyer, K., Treyer, V., & Fehr, E. (2006). Diminishing reciprocal fairness by disrupting the right prefrontal cortex. Science, 314, 829–832.
Kyranides, M., Fanti, K. A., Sikki, M., & Patrick, C. (2017). Triarchic dimensions of psychopathy in young adulthood: Associations with clinical and physiological measures after accounting for adolescent psychopathic traits. Personality Disorders: Theory, Research, and Treatment, 8(2), 140–149.
Kyranides, M. N., Fanti, K. A., Petridou, M., & Kimonis, E. R. (2019). In the eyes of the beholder: Ιnvestigating the effect of visual probing on accuracy and gaze fixations when attending to facial expressions among primary and secondary callous-unemotional variants. European Child & Adolescent Psychiatry. https://doi.org/10.1007/s00787-019-01452-z.
Kyranides, M., Fanti, K. A., & Panayiotou, G. (2016). The disruptive adolescent as a grown-up: Predicting adult startle responses to violent and erotic films from adolescent conduct problems and callous-unemotional traits. Journal of Psychopathology and Behavioral Assessment, 38, 183–194.
Marsh, A. A., & Blair, R. J. R. (2008). Deficits in facial affect recognition among antisocial populations: A meta-analysis. Neuroscience & Biobehavioral Reviews, 32(3), 454–465.
McAllister, S. M., Rothwell, J. C., & Ridding, M. C. (2009). Selective modulation of intracortical inhibition by low-intensity theta burst stimulation. Clinical Neurophysiology, 120(4), 820–826.
Mitchell, D. G., Richell, R. A., Leonard, A., & Blair, R. J. R. (2006). Emotion at the expense of cognition: Psychopathic individuals outperform controls on an operant response task. Journal of Abnormal Psychology, 115, 559–564.
Molero-Chamizo, A., Riquel, R. M., Moriana, J. A., Nitsche, M. A., & Rivera-Urbina, G. N. (2019). Bilateral prefrontal cortex anodal tDCS effects on self-reported aggressiveness in imprisoned violent offenders. Neuroscience, 397, 31–40.
Ochsner, K. N., & Gross, J. J. (2005). The cognitive control of emotion. Trends in Cognitive Sciences, 9, 242–249.
Padberg, F., Juckel, G., Präßl, A., Zwanzger, P., Mavrogiorgou, P., Hegerl, U., et al. (2001). Prefrontal cortex modulation of mood and emotionally induced facial expressions: A transcranial magnetic stimulation study. The Journal of Neuropsychiatry and Clinical Neurosciences, 13, 206–212.
Paulus, W. (2005). Toward establishing a therapeutic window for rTMS by theta burst stimulation. Neuron, 45, 181–183.
Perera, T., George, M. S., Grammer, G., Janicak, P. G., Pascual-Leone, A., & Wirecki, T. S. (2016). The clinical TMS society consensus review and treatment recommendations for TMS therapy for major depressive disorder. Brain Stimulation, 9(3), 336–346.
Posner, M. I., & Rothbart, M. K. (2007). Research on attention networks as a model for the integration of psychological science. Annual Review of Psychology., 58, 1–23.
Raine, A., Meloy, J. R., Bihrle, S., Stoddard, J., LaCasse, L., & Buchsbaum, M. S. (1998). Reduced prefrontal and increased subcortical brain functioning assessed using positron emission tomography in predatory and affective murderers. Behavioral Sciences & the Law, 16, 319–332.
Rego, G. G., Lapenta, O. M., Marques, L. M., Costa, T. L., Leite, J., Carvalho, S., et al. (2015). Hemispheric dorsolateral prefrontal cortex lateralization in the regulation of empathy for pain. Neuroscience Letters, 594, 12–16.
Repple, J., Pawliczek, C. M., Voss, B., Siegel, S., Schneider, F., Kohn, N., & Habel, U. (2017). From provocation to aggression: The neural network. BMC Neuroscience, 18, 73.
Rutherford, H. J., & Lindell, A. K. (2011). Thriving and surviving: Approach and avoidance motivation and lateralization. Emotion Review, 3(3), 333–343.
Salehinejad, M. A., Ghanavai, E., Rostami, R., & Nejati, V. (2017). Cognitive control dysfunction in emotion dysregulation and psychopathology of major depression (MD): Evidence from transcranial brain stimulation of the dorsolateral prefrontal cortex (DLPFC). Journal of Affective Disorders, 210, 241–248.
Schwarzkopf, D. S., Silvanto, J., & Rees, G. (2011). Stochastic resonance effects reveal the neural mechanisms of transcranial magnetic stimulation. Journal of Neuroscience, 31(9), 3143–3147.
Shamay-Tsoory, S. G., Tomer, R., Berger, B. D., & Aharon-Peretz, J. (2003). Characterization of empathy deficits following prefrontal brain damage: The role of the right ventromedial prefrontal cortex. Journal of Cognitive Neuroscience, 15, 324–337.
Simon, D., Craig, K. D., Gosselin, F., Belin, P., & Rainville, P. (2008). Recognition and discrimination of prototypical dynamic expressions of pain and emotions. PAIN, 55–64.
Smith, J. E., & Peterchev, A. V. (2018). Electric field measurement of two commercial active/sham coils for transcranial magnetic stimulation. Journal of Neural Engineering, 15(5), 054001.
Steinmetz, H., Fürst, G., & Meyer, B. U. (1989). Craniocerebral topography within the international 10–20 system. Electroencephalography and Clinical Neurophysiology, 72, 499–506.
Tamietto, M., Corazzini, L. L., de Gelder, B., & Geminiani, G. (2006). Functional asymmetry and interhemispheric cooperation in the perception of emotions from facial expressions. Experimental Brain Research, 171(3), 389–404.
Teti-Mayer, J., Nicolier, M., Tio, G., Mouchabac, S., Haffen, E., & Bennabi, D. (2019). Effects of high frequency repetitive transcranial magnetic stimulation (HF-rTMS) on delay discounting in major depressive disorder: An open-label uncontrolled pilot study. Brain Sciences, 9, 230–237.
Vallence, A. M., Goldsworthy, M. R., Hodyl, N. A., Semmler, J. G., Pitcher, J. B., & Ridding, M. C. (2015). Inter-and intra-subject variability of motor cortex plasticity following continuous theta-burst stimulation. Neuroscience, 304, 266–278.
Van Goozen, S. H., & Fairchild, G. (2008). How can the study of biological processes help design new interventions for children with severe antisocial behavior? Development and Psychopathology, 20, 941–973.
van Honk, J., Schutter, D. J., d’Alfonso, A. A., Kessels, R. P., & de Haan, E. H. (2002). 1 hz rTMS over the right prefrontal cortex reduces vigilant attention to unmasked but not to masked fearful faces. Biological Psychiatry, 52, 312–317.
Vanderhasselt, M. A., Baeken, C., Hendricks, M., & De Raedt, R. (2011). The effects of high frequency rTMS on negative attentional bias are influenced by baseline state anxiety. Neuropsychologia, 49(7), 1824–1830.
Wager, T. D., Davidson, M. L., Hughes, B. L., Lindquist, M. A., & Ochsner, K. N. (2008). Prefrontal-subcortical pathways mediating successful emotion regulation. Neuron, 59, 1037–1050.
Wang, J., Wang, Y., Hu, Z., & Li, X. (2014). Transcranial direct current stimulation of the dorsolateral prefrontal cortex increased pain empathy. Neuroscience, 281, 202–207.
Winker, C., Rehbein, M. A., Sabatinelli, D., Dohn, M., Maitzen, J., Wolters, C. H., et al. (2019). Noninvasive stimulation of the ventromedial prefrontal cortex indicates valence ambiguity in sad compared to happy and fearful face processing. Frontiers in Behavioral Neuroscience, 13, 83.
Yang, Y., & Raine, A. (2009). Prefrontal structural and functional brain imaging findings in antisocial, violent, and psychopathic individuals: A meta-analysis. Psychiatry Research: Neuroimaging, 174(2), 81–88.
Zwanzger, P., Steinberg, C., Rehbein, M. A., Bröckelmann, A. K., Dobel, C., Zavorotnyy, M., et al. (2014). Inhibitory repetitive transcranial magnetic stimulation (rTMS) of the dorsolateral prefrontal cortex modulates early affective processing. Neuroimage, 101, 193–203.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Konikkou, K., Kostantinou, N. & Fanti, K.A. Transcranial magnetic stimulation over the dorsolateral prefrontal cortex affects emotional processing: accounting for individual differences in antisocial behavior. J Exp Criminol 16, 349–366 (2020). https://doi.org/10.1007/s11292-020-09440-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11292-020-09440-z