Abstract
The emergence of drug-resistant tuberculosis is a major global public health threat. Thailand is one of the top 14 countries with high tuberculosis and multi-drug resistant tuberculosis rates. Immediate detection of drug-resistant tuberculosis is necessary to reduce mortality and morbidity by effectively providing treatment to ameliorate the formation of resistant strains. Limited data exist of mutation profiles in Northeastern Thailand. Here, 65 drug-resistant Mycobacterium tuberculosis isolates were used to detect mutations by polymerase chain reaction (PCR) and DNA sequencing. In the katG gene, mutations were occurred in 47 (79.7%) among 59 isoniazid resistant samples. For rpoB gene, 31 (96.9%) were observed as mutations in 32 rifampicin resistant isolates. Of 47 katG mutation samples, 45 (95.7%) had mutations in katG315 codon and 2 (4.3%) showed novel mutations at katG365 with amino acid substitution of CCG-CGG (Pro-Arg). Moreover, out of 31 rpoB mutation isolates, the codon positions rpoB516, rpoB526, rpoB531 and rpoB533 were 3 (9.7%), 8 (25.8%), 11 (35.5%) and 1 (3.2%), respectively. Seven isolates of double point mutation were found [rpoB516, 526; 1 (3.2%) and rpoB516, 531; 6 (19.4%)]. In addition, 1 (3.2%) sample had triple point mutation at codon positions rpoB516, 526 and 531. Common and novel mutation codons of the rpoB and katG genes were generated. Although DNA sequencing showed high accuracy, conventional PCR could be applied as an initial marker for screening drug-resistant Mycobacterium tuberculosis isolates in limit resources region. Mutations reported here should be considered when developing new molecular diagnostic methods for implementation in Northeastern Thailand.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tuberculosis (TB) caused by Mycobacterium tuberculosis (MTB) bacteria is a serious global infectious disease even though diagnosis and treatment are available. About one fourth of population (10 million people) in the world is suffering from this disease, with death rates of 1.4 million people in 2019 (World Health Organization 2020). The emergence of multi-drug resistant TB (MDR TB), described as resistant to at least rifampicin and isoniazid, as the two most commonly applied powerful first-line anti-TB drugs, is also a major public health threat worldwide (Lange et al. 2019; Jang and Chung 2020). Globally in 2019, an estimated 465,000 incident cases were reported as MDR and rifampicin resistant (RR) TB, while 3.3% and 13% of new cases and 18% and 17.4% of previously treated cases were diagnosed with MDR/RR TB and isoniazid (INH) resistant TB, respectively (World Health Organization 2020). Thailand is one of the top 14 countries with high TB, TB/HIV and MDR-TB rates and had 150 TB cases per 100,000 population in 2019 (World Health Organization 2020; Anukool et al. 2020). Immediate detection and accurate identification of MDR-TB is necessary to reduce mortality and morbidity by effectively providing treatment, to ameliorate the formation and spread of resistant strains (Jaksuwan et al. 2017; Nimri et al. 2011; Prammananan et al. 2008). The phenotypic DST method is the gold standard for detection of drug resistant but this takes 2–3 months to yield results and also increases the risk of bacterial contamination and cross infection by non-tuberculous mycobacterial infection. To shorten the turnaround time, two rapid molecular diagnostic methods, polymerase chain reaction (PCR) and DNA sequencing were selected in this study (Genestet et al. 2020; Li et al. 2020; Jang and Chung 2020). The distribution of drug-resistant genes varies according to geographical locations and identifying the mutation patterns of MDR-TB is important to optimize the treatment protocol (Jaksuwan et al. 2017; Seifert et al. 2015). However, limited data exist of mutation profiles in Northeastern Thailand.
A better understanding of drug-resistant mechanisms and the most commonly found mutation codons of rifampicin (RIF) and isoniazid (INH) are required. RIF is one of the most effective anti-TB drugs. Its mode of action involves binding to the β-subunit of RNA polymerase, thereby inhibiting the elongation of messenger RNA (Palomino and Martin 2014). The mechanism of RIF resistance in MTB is associated with mutation of the rpoB gene (Isakova et al. 2018). Some 96% of the mutation codons of RIF resistant MTB isolates mostly occur in 81 bp spanning codons (507–533), called the rifampicin resistance determining region (RRDR). Among these codons, rpoB516, 526 and 531 provided the highest level of resistance with percentage of 70–95% (Palomino and Martin 2014; Tajbakhsh et al. 2018). Another powerful drug for MTB is isoniazid and mutations in several genes such as katG, inhA, oxyR, kasA, ahpC and ndh are responsible for INH drug resistance. Most INH resistance is caused by mutation in the katG gene that codes for the catalase-peroxidase enzyme, a key factor in mycolic acid biosynthesis. The most common mutation in INH-resistant strains occurs at the codon position 315 of katG gene (katG315) reported that on average 50–95% (Gupta et al. 2013; Pandey et al. 2017; Ravibalan et al. 2015).
Here, we examined the mutations of drug-resistant MTB strains emphasizing on the rpoB and katG genes in Northeastern Thailand populations by the used of PCR and DNA sequencing methods.
Materials and methods
Sample sources and processing
A total of 357 MTB isolates were randomly selected from the TB laboratory at the Office of Disease Prevention and Control Center (DPC) 7th, 8th, 9th and 10th (Khon Kaen Province, Udon Thani Province, Nakhon Ratchasima Province and Ubon Ratchathani Province, respectively) between 2013 and 2016 in Northeastern Thailand. Among these samples, 92 isolates were found with drug resistance (rifampicin and isoniazid) by testing with the standard proportion method in all DPC centers (Rueangsak et al. 2020). In this study, 65 drug-resistant MTB isolates were used for detection of mutation patterns in Northeastern Thailand. All isolates were confirmed as MTB by observing culture positive on Lowenstein-Jensen medium and using immunochromatographic assay (ICA) kit (SD Bioline TB Ag MPT64 rapid test) to detect and amplify real-time PCR.
DNA extraction
Genomic DNA of the 65 drug-resistant isolates of Mycobacterium tuberculosis (26 resistant to both RIF and INH, 33 mono-resistant to isoniazid and 6 mono- resistant to rifampin) were extracted using the CTAB (cetyl trimethylammonium bromide) method (Van Embden et al. 1993). In two microcentrifuge tubes, each 400 μL of bacterial cell suspension was transferred. After that, both tubes were put on heat block with the temperature at 80 °C for 20 min. After adding all chemical reagents, the DNA pellets were re-dissolved in 50 μL of TE buffer and stored at -20 °C and -70 °C until required for further use. The estimation of DNA concentration was done by using a spectrophotometer (NanoDrop 2000c, USA) with the absorbance at a wavelength of 260 nm.
PCR amplification
Conventional polymerase chain reaction was used to determine mutations in 4 regions for the rpoB gene codons 516, 526, 531 and 533 and 1 region for the katG gene codon 315 using specific primers (Table 1) (Nurpermatasari et al. 2018; Ahmed et al. 2013). For each condition, the preparation of master mix concentration and cycling temperature was modified from the methods of (Allegui et al. 2012; Tajbakhsh et al. 2018; Farnia et al. 2010).
Amplification reactions for the rpoB516 and katG315 codons were performed in a final volume of 50 µL containing 0.5 µL of 2.5 mM dNTPs, 5 µL of 10X Buffer, 0.25 µL of 5 U/ µL Taq polymerase, 1.66 µL of 50 mM MgCl2, 40.59 µL sterile DI water, 0.5 µL of each forward and reverse 10 µM primers and 1 µL of 20 ng genomic DNA. Similar concentrations of all reagents were also used for amplifying the rpoB531 and rpoB526 codons with a final volume of 25 µL composed of 0.25 µL of dNTPs, 2.5 µL of Buffer, 0.2 µL of Taq polymerase, 0.5 µL (for 531 codon) and 1 µL (for 526 codon) of MgCl2, 18.55 µL and 18.05 µL of sterile DI water for 531 and 526 codons, respectively. After 1 µL of each primer and 1 µL of DNA. For the rpoB533 amplification, the PCR reaction was performed in a final volume of 25 µL containing the same concentrations of the above reagents accompanied by dNTPs (2 µL), Buffer (2.5 µL), Taq (0.25 µL), MgCl2 (2.75 µL), DI water (13 µL), forward primer (0.5 µL), reverse primer (2 µL) and DNA (2 µL).
The DNA amplifications were performed in a thermal cycler, FlexCycler2, (Analytik Jena AG, Germany). Cycling temperatures for the rpoB516 and katG315 codons were initial denaturing at 96 °C for 3 min; 23 cycles of 95 °C for 50 s, 68 °C for 40 s, and 72 °C for 1 min; and final elongation at 72 °C for 7 min. For rpoB531 and 526 codons, the following cycling temperatures were used: initial denaturing at 95 °C for 5 min, 40 cycles of 94 °C for 1 min, 58 °C (for 531 codon) and 55 °C (for 526 codon) for 1 min, 72 °C for 1 min, and a final extension at 72 °C for 10 min. Furthermore, initial denaturing at 95 °C for 5 min; 40 cycles of 95 °C for 30 s, 68 °C for 30 s, and 72 °C for 30 s; and final elongation at 72 °C for 7 min were used as cycling temperatures for amplifying the rpoB533 primer. All PCR fragments were analyzed by agarose gel electrophoresis using 1.5% agarose gel. The gels were exposed to UV light with photos taken by a GeneFlash gel documentation system (Syngene, USA).
DNA sequencing
Two primers: rpoB-F (5´-TACGGTCGGCGAGCTGATCC-3´) and rpoB-R (5´-TACGGCGTTTCGATGAACC-3´) were used to amplify a 411 bp fragment (1119 – 1532 bp) of the rpoB gene, containing 81 bp (RRDR region). The region of the 435 bp (669–1103 bp) katG gene was amplified with a set of primers sequences: Forward-(5´-GCAGATGGGGCTGATCTACG-3´) and Reverse-(5´-AACGGGTCCGGGATGGTG-3´). Before sequencing, PCR amplification reactions were modified following (Farnia et al. 2010) and (Jaiswal et al. 2017). Final volumes of 50 µL were used for the rpoB and katG genes. For the rpoB gene, sterile DI water 32.9 µL, 10X buffer 5 µL, 5 U/µL Taq Polymerase 0.5 µL, 2.5 mM dNTPs 4 µL, 50 mM MgCl2 1 µL, 10 µM Forward and Reverse Primers 0.8 µL each and 4 µL of 20 ng DNA were used, while sterile DI water (25.75 µL), 10X buffer (6.25 µL), 5 U/ µL Taq Polymerase (0.5 µL), 2.5 mM dNTPs (4 µL), 50 mM MgCl2 (2 µL), 10 µM forward and reverse primers (3.75µL for each) and 4 µL of 20 ng DNA were used to amplify the katG gene.
PCR conditions were as follows: initial denaturation at 95 °C for 5 min (rpoB gene) and 95 °C for 3 min (katG gene), followed by 40 cycles of 95 °C for 30 s, annealing at 69 °C for 30 s, extension of 72 °C for 30 s and final extension of 72 °C for 7 min for the rpoB gene followed by 35 cycles of 95 °C for 45 s, annealing at 64 °C for 45 s, extension of 72 °C for 1 min and final extension of 72 °C for 5 min for the katG gene. The PCR products were analyzed by electrophoresis on 2% agarose gel under ultraviolet light. After amplification, the PCR products containing specific genes and specific portions were sent to a sequencing company (Ward Medic), including the gel purification step.
Sequence analysis
The sequencing data obtained from the company were aligned with the wild type H37Rv sequences of rpoB and katG genes (GenBank accession NC_000962.3) by using the BioEdit bioinformatic tool. Then, mutation codons and types of mutation in the samples were examined. For the rpoB gene, the nucleotide numbering system was based on E. coli.
Two isolates with novel mutation in the katG365 codon can be accessed (GenBank Accession No. MZ093466, MZ093467).
Results
Out of 357 MTB isolates, 92 samples (25.8%) were found with drug resistance, as already described by (Rueangsak et al. 2020). Of the 92 drug-resistant samples, 38 (41.3%) were multi-drug resistant, while 46 (50%) and 8 (8.7%) were mono-resistant to isoniazid and mono-resistant to rifampicin, respectively. Sixty-five drug-resistant samples (26 multi-drug resistant, 33 mono-resistant to isoniazid and 6 mono-resistant to rifampicin) were used to find mutations in the hot spot regions of the rpoB and katG genes.
PCR amplification results
To detect mutations in the rpoB516, 526, 531, 533 and katG315 genes codons, each reaction for amplifying target size was optimized by using the H37Rv reference strain as the DNA template. Fifty-nine mono-resistant isoniazid isolates were detected by using the katG315 primer to determine the mutation codons. Among the 56 isoniazid resistant samples, 45 (80.4%) were identified as mutation in the katG315 codon. The remaining 3 samples were not differentiated by PCR.
Consequently, 32 mono-resistant rifampicin isolates were tested to observe mutations by using all rpoB primers individually. Of 32 RIF resistant samples, the rpoB516 gene mutation codon was found in 10 (31.2%), rpoB526 mutation codon was observed in 5 (15.6%) and 11 (34.4%) were identified as mutation in the rpoB531 gene codon. There were no mutation isolates with the rpoB533 primer. Therefore, the rpoB531 gene mutation codon had the highest percentage followed by rpoB516 and rpoB526.
Twenty-six MDR isolates were detected to observe combined mutation codons of both genes by using rpoB516, 526, 531, 533 and katG315 primers. A total of 13 out of 26 (50%) MDR cases showed mutations in both genes, while 4 isolates harbored no mutation in MDR samples. Mutation codon in the katG gene alone was found in 8 samples, whereas 1 sample was found to have mutation codon in the rpoB gene alone in MDR isolates. Six samples showed no mutation codon in mono resistant to INH and 3 samples of mono resistant to INH were not differentiated by PCR. Three samples were found as no mutation codon in mono resistant to RIF samples. Hence, 15 samples for the rpoB gene and 14 samples for the katG gene were selected for DNA sequencing to detect mutation sites that were not detected by PCR.
DNA sequencing results
PCR amplifications for DNA sequencing of the rpoB and katG genes were optimized by using the H37Rv reference strain as the DNA template. Fifteen isolates that exhibited the rpoB gene with no mutation and 14 isolates that showed no mutation at katG315 codon by PCR were sequenced. Our analysis detected 5 mutated positions distributed among 4 codons within RRDR of the rpoB gene. Of the 15 isolates, 7 had mutation at codon 531 with amino acid changes at the position of TCG-TTG (Ser-Leu), while mutation at rpoB526 of CAC-CGC (His-Arg) occurred in 3 isolates and changes of CAC-TAC (His-Tyr) occurred in 2 isolates. Moreover, 1 mutation at rpoB516 GAC-GTC (Asp-Val) was identified, while a mutation at rpoB533 displayed CTG-CCG (Leu-Pro) amino acid change. No mutation was detected in 1 isolate.
Among the 14 isolates that showed no mutation at katG315 codon, 2 isolates had mutation at codon 365 CCG-CGG (Pro-Arg). These were recognized as novel mutations and no mutations were observed in 12 samples. The above 3 samples that were not differentiated by PCR revealed no mutation with the sequencing method.
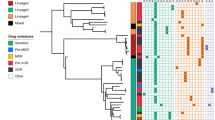
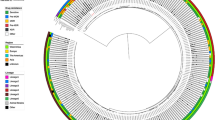
Distribution of mutation profiles based on PCR and DNA sequencing methods
All of mutation isolates detected by PCR and DNA sequencing were analyzed in percentage frequency showed by pie chart with individual gene codon (katG or rpoB) and multidrug resistant isolates. The katG gene mutations occurred in 47 (79.7%) of the 59 INH resistant samples. For the rpoB gene, 31 (96.9%) were observed as mutations in 32 RIF resistant isolates (Fig. 1). Finally, the number of those isolates were mapped to indicate the presence of geographical distribution of the rpoB and katG gene mutation samples in each province of Northeastern Thailand (Fig. 2).
The mutation of assigned codon position in katG and rpoB genes were detected from clinical isolates of Mycobacterium tuberculosis by PCR and DNA sequencing methods. Mutation frequency percentage in the katG gene among 47 INH resistant isolates. Predominate mutation of katG gene found in codon position 315 (a). The rpoB gene mutation occurred among 31 RIF resistant isolates, including 23, 7 and 1 isolates were detected as single, double, and triple points mutation, respectively (b). Of 26 MDR isolates, 22 isolates were detected as katG and rpoB gene mutation by these 2 methods (c)
Discussion
This is the first study determining the distribution of Mycobacterium tuberculosis mutation genes codons in Northeastern Thailand. We found 41.3% as MDR, 50% as resistant to INH and 8.7% as resistant to RIF among 92 drug-resistant isolates. RIF resistance is caused by mutation in the rpoB gene, encoding the β-subunit of the DNA-dependent RNA polymerase (Jureen et al. 2006; Chaves et al. 2000). More than 95% of rpoB mutation codons in RIF-resistant clinical isolates have been found within the rifampicin resistant determining region (RRDR) (González et al. 1999). Our findings revealed that 96.9% of rpoB gene mutation codons were observed within the RRDR region. Our result was similar to a report in Bangladesh that also showed 96.43% of rpoB gene point mutation in the RRDR (Mistri et al. 2016). Other studies have documented the presence of common and novel rpoB mutations outside the RRDR (Mani et al. 2001; Aparna Lingala et al. 2010). According to our size of product, we only determined the most prevalent mutation codons between the positions 454–591 including the RRDR region. Inside the 81-bp RRDR, mutations at codons 516, 526 and 531 are responsible for up to 90% of RIF-resistant strains and recognized as the most frequent codons (Pang et al. 2013; Williams et al. 1994). Out of the rpoB codon mutation isolates in our study, 58.1% were detected at rpoB531 codon, 35.5% at rpoB516 codon and 32.3% at rpoB526 codon. Therefore, the most prevalent mutation codon was rpoB531, consistent with other findings in the Kyrgyz Republic (64.8%) (Isakova et al. 2018), Shanghai (53.8%) (Fan et al. 2003) and North India (66.7%) (Makadia et al. 2012). Most studies in China (Yue et al. 2003), Vietnam (Caws et al. 2006) and Singapore (Lee et al. 2005) exhibited the rpoB526 codon as the second highest mutation frequency that is different from our results. Moreover, only 1 (3.2%) sample was found to have mutation in rpoB533 (Leu-Pro). This codon 533 was also detected in a study in Ratchaburi Province, Thailand as a novel mutation; however, different amino acids indicated rpoB533 (Leu-Arg) (Jintaridh et al. 2014). In accordance with our study, reports from Thailand by (Prammananan et al. 2008) and Taiwan by (Qian et al. 2002) displayed rpoB533 (Leu-Pro) mutation with the percentages of 2.1 and 3, respectively. Furthermore, double point mutation was determined in 7 samples and triple point mutation was identified in 1 sample in our study. In our research, rpoB531 codon that expressed highest mutation percentages, could be applied as an indicator to investigate rifampicin resistant Mycobacterium tuberculosis isolates in this area.
Nearly all rifampicin-resistant strains are further resistant to other drugs, especially to isoniazid. Thus, rifampicin resistance is recognized as a surrogate marker for MDR-TB (Traore et al. 2000). Detection of resistance for another drug in this study was isoniazid that inhibits the synthesis of mycolic acids and acts as a prodrug that is activated by the catalase-peroxidase enzyme, katG (Jena et al. 2014; Timmins and Deretic 2006). According to our report, the percentage of 79.7% for the katG gene mutation was consistent with earlier studies in Thailand (Boonaiam et al. 2010; Suthum et al. 2020) and other Southeast Asian Countries (Ismail et al. 2016; Caws et al. 2006; Valvatne et al. 2009; Liu et al. 2018; Cheng et al. 2021). The prevalence of katG315 mutation codon varied according to the geographical region: Southeast Asia (78.4%) (Seifert et al. 2015), Vietnam (85.3%) (Hang et al. 2019), China (59.4%) (Wu et al. 2006), the Netherlands (53%) (Van Soolingen et al. 2000), Japan (22%) (Ando et al. 2010) and Singapore (26%) (Lee et al. 1999). Furthermore, our results revealed that higher percentage of katG315 mutation codon in resistant to INH isolates than in MDR strains (53.3% and 46.7%, respectively). Two isolates of novel mutation at katG365 (GenBank accession no. MZ093466, MZ093467) with the amino acid substitution of CCG-CGG (Pro-Arg) were exhibited in our report. As previously mentioned, the katG315 mutation codon provided higher percentages, and therefore, this mutation codon could be utilized as an indicator for the detection of isoniazid resistance Mycobacterium tuberculosis isolates in this region.
After PCR amplification, 15 samples of resistant to RIF that did not show any mutation with primers of the PCR method were selected for rpoB gene sequencing to discover more mutation codons. These 15 isolates showed single point mutation within RRDR of the rpoB gene in 14 and no mutation in 1 sample. katG sequencing was performed in the 14 isolates (5 MDR samples, 6 samples were resistant to INH and 3 samples were not detected by PCR) that showed no mutation at katG315 codon. Mutation patterns performed by DNA sequencing in this study showed missense mutation in all isolates.
According to Fig. 2, mutation samples of the rpoB and katG genes in each province were widely distributed. The katG315 gene mutation samples were fully distributed throughout Northeastern Thailand and detected in every provinces except Bueng Kan that also showed no mutation samples. Moreover, rpoB531 gene mutation samples were also widespread and found in many provinces except for Bueng Kan, Chaiyaphum, Nakhon Ratchasima, Yasothon and Maha Sarakham. Higher distribution of mutation codons was found in provinces located near the Laos border. In Sakon Nakhon and Amnat Charoen Provinces, 2 isolates (one in each province) showing novel mutation were detected, while 1 isolate of rpoB533 gene mutation was found in Mukdahan Province.
When comparing PCR and DNA sequencing methods, discordant results were found for detection of the rpoB gene but not for the katG gene. PCR did not identify 7, 5, 1 and 1 isolates of rpoB531, rpoB526, rpoB516 and rpoB533 mutation codons, respectively. These observed possibly because the isolates contained heterogeneous populations of bacteria with mutated and wild type rpoB alleles, leading to amplification of the wild type PCR product (Ullah et al. 2019). No mutations were detected in 1 isolate of resistant to RIF and 12 isolates of resistant to INH by both PCR and DNA sequencing. This could be having mutations outside of the rpoB and katG genes that were not considered in this study. The DNA sequencing method showed greater sensitivity and specificity than PCR but the latter is more appropriate for use as a screening method to obtain faster results in low resource countries. Our results showed similar percentages of mutation codons reported in Thailand and Southeast Asian Countries except for katG315 mutation codon percentage and having novel mutation of katG365 codon.
Study limitations were as follows. Gene mutation of katG, ahpC, inhA and kasA can cause isoniazid resistance (Zhang et al. 1992); however, we only detected katG gene mutation that provided high-level resistance. Even though we identified the katG gene mutation, the amino acid change pattern of this gene mutation could not be performed by sequencing, especially in katG315 codon. Furthermore, a larger sample size would further validate our findings. We were unable to identify the entire genes of rpoB and katG because we focused on the most prevalent mutation sites for sequencing. Therefore, further studies should sequence the entire rpoB and katG genes to obtain more accurate results.
Conclusions
Even though DNA sequencing has great accuracy, conventional PCR method could be applied as an initial marker for the screening of rifampicin and isoniazid resistant Mycobacterium tuberculosis in Northeastern Thailand. Our results showed that rpoB531 codon and katG315 codon expressed highest mutation percentages and could be utilized as indicators to investigate rifampicin and isoniazid resistant Mycobacterium tuberculosis isolates in this area. Two isolates with novel mutation at katG365, with amino acid substitution CCG-CGG (Pro-Arg) were exhibited in our report. The mutations reported here should be considered in the development of new molecular diagnostic methods for implementation in Northeastern Thailand. These novel techniques could reduce mortality and morbidity and provide effective treatment to ameliorate the formation of further resistant strains and spread of disease in Northeastern Thailand.
Data availability
Not applicable.
Code availability
Not applicable.
References
Ahmed M, Ahmed AR, Mohammed S (2013) First experience with using simple polymerase chain reaction-based methods as an alternative to phenotypic drug susceptibility testing for Myobacterium tuberculosis in Iraq. Int J Appl Basic Med Res 3:98–105. https://doi.org/10.4103/2229-516x.117069
Allegui Z, Ghariani A, Draoui H et al (2012) Detection of isoniazid and rifampin resistance of Mycobacterium tuberculosis by a multiplex allele-specific polymerase chain reaction (PCR) assay. Int J Mycobacteriol 1:34–39. https://doi.org/10.1016/j.ijmyco.2012.01.006
Ando H, Kondo Y, Suetake T et al (2010) Identification of katG mutations associated with high-level isoniazid resistance in Mycobacterium tuberculosis. Antimicrob Agents Chemother 54:1793–1799. https://doi.org/10.1128/AAC.01691-09
Anukool U, Phunpae P, Tharinjaroen CS et al (2020) Genotypic distribution and a potential diagnostic assay of multidrug-resistant tuberculosis in northern thailand. Infect Drug Resist 13:3375–3382. https://doi.org/10.2147/IDR.S263082
Aparna Lingala ML, Srikantam A, Jain S et al (2010) Clinical and geographical profiles of rpoB gene mutations in Mycobacterium tuberculosis isolates from Hyderabad and Koraput in India. J Microbiol Antimicrob 2:13–18
Boonaiam S, Chaiprasert A, Prammananan T, Leechawengwongs M (2010) Genotypic analysis of genes associated with isoniazid and ethionamide resistance in MDR-TB isolates from Thailand. Clin Microbiol Infect 16:396–399. https://doi.org/10.1111/j.1469-0691.2009.02838
Caws M, Minh Duy P, Quang Tho D et al (2006) Mutations prevalent among Rifampin- and isoniazid-resistant Mycobacterium tuberculosis isolates from a hospital in Vietnam. J Clin Microbiol 44:2333–2337. https://doi.org/10.1128/JCM.00330-06
Chaves F, Alonso-Sanz M, Rebollo MJ et al (2000) rpoB mutations as an epidemiologic marker in rifampin-resistant Mycobacterium tuberculosis. Int J Tuberc Lung Dis 4(8):765–770
Cheng S, Hide M, Pheng SH et al (2021) Resistance to second-line anti-TB drugs in Cambodia: a phenotypic and genetic study. Infect Drug Resist 14:1089–1104. https://doi.org/10.2147/idr.s289907
Fan XY, Hu ZY, Xu FH et al (2003) Rapid detection of rpoB gene mutations in rifampin-resistant Mycobacterium tuberculosis isolates in Shanghai by using the amplification refractory mutation system. J Clin Microbiol 41:993–997. https://doi.org/10.1128/JCM.41.3.993-997.2003
Farnia P, Taghavi K, Sh S, et al (2010) Susceptibility testing multiplex - PCR, PCR SSCP and PCR ELISA Mycobacteriology Research Center (MRC), 2168099; Tehran: National Research Institute of Tuberculosis and Lung Diseases, 978–600. https://doi.org/10.13140/RG.2.2.14291.07200
Genestet C, Hodille E, Berland JL et al (2020) Whole-genome sequencing in drug susceptibility testing of Mycobacterium tuberculosis in routine practice in Lyon. France Int J Antimicrob Agents 55:105912. https://doi.org/10.1016/j.ijantimicag.2020.105912
González N, Torres MJ, Aznar J, Palomares JC (1999) Molecular analysis of rifampin and isoniazid resistance of Mycobacterium tuberculosis clinical isolates in Seville, Spain. Tuber Lung Dis 79:187–190. https://doi.org/10.1054/tuld.1998.0195
Gupta A, Prakash P, Singh SK, Anupurba S (2013) Rapid Genotypic Detection of rpoB and katG Gene Mutations in Mycobacterium tuberculosis Clinical Isolates from Northern India as Determined by MAS-PCR. J Clin Lab Anal 27:31–37. https://doi.org/10.1002/jcla.21558
Hang NTL, Hijikata M, Maeda S et al (2019) Whole genome sequencing, analyses of drug resistance-conferring mutations, and correlation with transmission of Mycobacterium tuberculosis carrying katG-S315T in Hanoi, Vietnam. Sci Rep 9:15354. https://doi.org/10.1038/s41598-019-51812-7
Isakova J, Sovkhozova N, Vinnikov D et al (2018) Mutations of rpoB, katG, inhA and ahp genes in rifampicin and isoniazid-resistant Mycobacterium tuberculosis in Kyrgyz Republic. BMC Microbiol 18:1–8. https://doi.org/10.1186/s12866-018-1168-x
Ismail N-A, Fazli Ismail M, Suraiya S et al (2016) Genotypic detection of rpoB and katG gene mutations associated with rifampicin and isoniazid resistance in Mycobacterium tuberculosis isolates: a local scenario (Kelantan). Malays J Med Sci 23(1):22–26
Jaiswal I, Jain A, Singh P et al (2017) Mutations in katG and inhA genes of isoniazid-resistant and -sensitive clinical isolates of Mycobacterium tuberculosis from cases of pulmonary tuberculosis and their association with minimum inhibitory concentration of isoniazid. Clin Epidemiol Glob Heal 5:143–147. https://doi.org/10.1016/j.cegh.2016.08.008
Jaksuwan R, Tharavichikul P, Patumanond J et al (2017) Genotypic distribution of multidrug-resistant and extensively drug-resistant tuberculosis in northern Thailand. Infect Drug Resist 10:167–174. https://doi.org/10.2147/IDR.S130203
Jang JG, Chung JH (2020) Diagnosis and treatment of multidrug-resistant tuberculosis. Yeungnam Univ J Med 37:277–285. https://doi.org/10.12701/yujm.2020.00626
Jena L, Waghmare P, Kashikar S et al (2014) Computational approach to understanding the mechanism of action of isoniazid, an anti-TB drug. Int J Mycobacteriol 3:276–282. https://doi.org/10.1016/j.ijmyco.2014.08.003
Jintaridh P, Ramasoota P, Pyar K et al (2014) Novel mutation detection in rpoB of Rifampicin-resistant Mycobacterium tuberculosis using pyrosequencing. Southeast Asian J Trop Med Public Health 45:843–852
Jureen P, Engstrand L, Eriksson S et al (2006) Rapid detection of rifampin resistance in Mycobacterium tuberculosis by pyrosequencing technology. J Clin Microbiol 44:1925–1929. https://doi.org/10.1128/JCM.02210-05
Lange C, Aarnoutse RE, Alffenaar JWC et al (2019) Management of patients with multidrug-resistant tuberculosis. Int J Tuberc Lung Dis 23:645–662. https://doi.org/10.5588/ijtld.18.0622
Lee ASG, Lim IHK, Tang LLH et al (1999) Contribution of kasA analysis to detection of isoniazid-resistant Mycobacterium tuberculosis in Singapore. Antimicrob Agents Chemother 43:2087–2089. https://doi.org/10.1128/aac.43.8.2087
Lee ASG, Lim IHK, Tang LLH, Sin YW (2005) High frequency of mutations in the rpoB gene in rifampin-resistant clinical isolates of Mycobacterium tuberculosis from Singapore. J Clin Microbiol 43:2026–2027
Li MC, Chen R, Lin SQ et al (2020) Detecting ethambutol resistance in Mycobacterium tuberculosis isolates in China: a comparison between phenotypic drug susceptibility testing methods and DNA sequencing of embAB. Front Microbiol 11:1–7. https://doi.org/10.3389/fmicb.2020.00781
Liu L, Jiang F, Chen L et al (2018) The impact of combined gene mutations in inhA and ahpC genes on high levels of isoniazid resistance amongst katG non-315 in multidrug-resistant tuberculosis isolates from China. Emerg Microbes Infect 7:183. https://doi.org/10.1038/s41426-018-0184-0
Makadia JS, Jain A, Patra SK et al (2012) Emerging trend of mutation profile of rpoB gene in MDR tuberculosis, North India. Indian J Clin Biochem 27:370–374. https://doi.org/10.1007/s12291-012-0228-5
Mani C, Selvakumar N, Narayanan S, Narayanan PR (2001) Mutations in the rpoB gene of multidrug-resistant Mycobacterium tuberculosis clinical isolates from India. J Clin Microbiol 39:2987–2990. https://doi.org/10.1128/JCM.39.8.2987-2990.2001
Mistri SK, Sultana M, Kamal SMM et al (2016) Evaluation of efficiency of nested multiplex allele-specific PCR assay for detection of multidrug resistant tuberculosis directly from sputum samples. Lett Appl Microbiol 62:411–418. https://doi.org/10.1111/lam.12564
Nimri L, Samara H, Batchoun R (2011) Detection of mutations associated with multidrug-resistant Mycobacterium tuberculosis clinical isolates. FEMS Immunol Med Microbiol 62:321–327. https://doi.org/10.1111/j.1574-695X.2011.00814.x
Nurpermatasari A, Harahap U, Siagian P (2018) Identification gene mutations rpoB cause of multidrug resistance tuberculosis in Haji Adam Malik hospital. Asian J Pharm Clin Res 11:155–158. https://doi.org/10.22159/ajpcr.2018.v11s1.26595
Palomino JC, Martin A (2014) Drug resistance mechanisms in Mycobacterium tuberculosis. Antibiotics 3:317–340
Pandey S, Lamichhane A, Byanjankar A et al (2017) Direct detection of rpoB and katG gene mutations of Mycobacterium tuberculosis in clinical samples. Asian Pac J Trop Biomed 7:698–701. https://doi.org/10.1016/j.apjtb.2017.07.018
Pang Y, Lu J, Wang Y et al (2013) Study of the rifampin monoresistance mechanism in Mycobacterium tuberculosis. Antimicrob Agents Chemother 57:893–900. https://doi.org/10.1128/AAC.01024-12
Prammananan T, Cheunoy W, Taechamahapun D et al (2008) Distribution of rpoB mutations among multidrug-resistant Mycobacterium tuberculosis (MDRTB) strains from Thailand and development of a rapid method for mutation detection. Clin Microbiol Infect 14:446–453. https://doi.org/10.1111/j.1469-0691.2008.01951
Qian L, Abe C, Lin TP et al (2002) rpoB genotypes of Mycobacterium tuberculosis Beijing family isolates from East Asian countries. J Clin Microbiol 40:1091–1094. https://doi.org/10.1128/JCM.40.3.1091-1094.2002
Ravibalan T, Samrot AV, Maruthai K et al (2015) Evaluation of multiplex polymerase chain reaction assay for the detection of katG (S315T) gene mutation in Mycobacterium tuberculosis isolates from Puducherry, South India. J Pure Appl Microbiol 9:2339–2345
Rueangsak K, Tanuchit S, Chumpol J et al (2020) 24-locus MIRU-VNTR and Spoligotyping analysis of drug-resistant Mycobacterium tuberculosis strains isolated from Northeastern Thailand. Infect Genet Evol 85:104449. https://doi.org/10.1016/j.meegid.2020.104449
Seifert M, Catanzaro D, Catanzaro A, Rodwell TC (2015) Genetic mutations associated with isoniazid resistance in Mycobacterium tuberculosis: a systematic review. PLoS ONE 10:1–13. https://doi.org/10.1371/journal.pone.0119628
Suthum K, Samosornsuk W, Samosornsuk S (2020) Characterization of katG, inhA, rpoB and pncA in Mycobacterium tuberculosis isolates from MDR-TB risk patients in Thailand. J Infect Dev Ctries 14:268–276. https://doi.org/10.3855/jidc.11974
Tajbakhsh A, Ghasemi F, Mirbagheri SZ et al (2018) Investigation of the rpoB mutations causing Rifampin resistance by rapid screening in Mycobacterium tuberculosis in North-East of Iran. Iran J Pathol 13(4):429–437
Timmins GS, Deretic V (2006) Mechanisms of action of isoniazid. Mol Microbiol 62:1220–1227
Traore H, Fissette K, Bastian I et al (2000) Detection of rifampicin resistance in Mycobacterium tuberculosis isolates from diverse countries by a commercial line probe assay as an initial indicator of multidrug resistance. Int J Tuberc Lung Dis 4(5):481–484
Ullah I, Ahmad W, Shah AA et al (2019) Detection of rifampicin resistance of Mycobacterium tuberculosis using multiplex allele specific polymerase chain reaction (MAS-PCR) in Pakistan. Infect Genet Evol 71:42–46. https://doi.org/10.1016/j.meegid.2019.03.007
Valvatne H, Syre H, Kross M et al (2009) Isoniazid and rifampicin resistance-associated mutations in Mycobacterium tuberculosis isolates from Yangon, Myanmar: implications for rapid molecular testing. J Antimicrob Chemother 64:694–701. https://doi.org/10.1093/jac/dkp292
Van Embden JDA, Cave MD, Crawford JT et al (1993) Strain Identification of Mycobacterium tuberculosis by DNA fingerprinting: recommendations for a standardized methodology. J Clin Microbiol 31:406–409
Van Soolingen D, De Haas PEW, Rogier Van Doorn H et al (2000) Mutations at amino acid position 315 of the katG gene are associated with high-level resistance to isoniazid, other drug resistance, and successful transmission of Mycobacterium tuberculosis in The Netherlands. J Infect Dis 182:1788–1790
Williams DL, Waguespack C, Eisenach K et al (1994) Characterization of Rifampin resistance in pathogenic mycobacteria. Antimicrob Agents Chemother 38:2380–2386
World Health Organizatin (2020) . Global tuberculosis report 2020. http://apps.who.int/bookorders. Accessed 11 Mar 2021.
Wu XQ, Lu Y, Zhang JX et al (2006) Detection of the mutations in katG315 and inhA-15 of Mycobacterium tuberculosis strains isolated from Chinese patients. Chin Med J (engl) 119:230–233. https://doi.org/10.1097/00029330-200602010-00011
Yue J, Shi W, Xie J et al (2003) Mutations in the rpoB gene of multidrug-resistant Mycobacterium tuberculosis isolates from China. J Clin Microbiol 41:2209–2212. https://doi.org/10.1128/JCM.41.5.2209-2212.2003
Zhang Y, Heym B, Allen B et al (1992) The catalase—peroxidase gene and isoniazid resistance of Mycobacterium tuberculosis. Nature 358:591–593. https://doi.org/10.1038/358591a0
Acknowledgements
This research project was supported by Khon Kaen University Research Grant (Project Numbers 590038 and 6100033) and Centre for Research and Development of Medical Diagnostic Laboratories, Khon Kaen University. We would like to thank the KKU Scholarship for ASEAN and GMS Countries’ Personnel of Academic Year 2019, Khon Kaen University for providing a scholarship for Ei Phoo Thwe. Special thanks also go to Miss Kulrattana Rueangsak for her technical assistance.
Funding
The present study was supported by Centre for Research and Development in Medical Diagnostic Laboratory, Faculty of Associated Medical Sciences, Khon Kaen University and the Graduate School, Khon Kaen University, Thailand.
Author information
Authors and Affiliations
Contributions
Not applicable.
Corresponding author
Ethics declarations
Conflict of interest
The author declares that they have no conflict of interest.
Ethical approval
This study was approved by Khon Kaen University Ethics Committee for Human Research (HE631314).
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Thwe, E.P., Namwat, W., Pinlaor, P. et al. Novel mutations detected from drug resistant Mycobacterium tuberculosis isolated from North East of Thailand. World J Microbiol Biotechnol 37, 194 (2021). https://doi.org/10.1007/s11274-021-03163-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11274-021-03163-7