Abstract
Human T-cell lymphotropic virus type 1 (HTLV-1) is linked to two debilitating diseases, adult T-cell leukemia/lymphoma (ATLL) and HTLV-1 associated myelopathy tropical spastic paraparesis (HAM/TSP), which are prevalent in various parts of the world, including the Alborz province in Iran. Understanding the prevalence and evolutionary relationships of HTLV-1 infections in these endemic areas is of utmost importance. In the realm of phylogenetic studies, long terminal repeat (LTR) region of HTLV-1 stands out as highly conserved, yet more variable compared to other gene segments. Consequently, it is the primary focus for phylogenetic analyses. Additionally, trans-activator of transcription (Tax), an oncoprotein, holds a pivotal role in the regulation of gene expression. This cross-sectional study delved into the phylogenetic analysis of HTLV-1 among individuals in Alborz province of Iran. To confirm infection, we amplified partial sequence LTR (PLTR) and HTLV-1 bZIP factor (PHBZ). For phylogenetic analysis, we sequenced the full sequence LTR (FLTR) and full Tax sequence (FTax). The FLTR and FTax sequences underwent analysis using BioEdit, and phylogenetic trees were constructed using MEGA-X software. Out of the roughly 15,000 annual blood donors in Alborz, 19 samples tested positive for HTLV-1, indicating a 0.13% HTLV-1 positivity rate among blood donors. Furthermore, the HTLV-1 virus prevalent in the Alborz province belongs to subtype A (cosmopolitan) subgroup A. The findings revealed that while mutations were observed in both the LTR and Tax genes, they were not significant enough to bring about fundamental alterations. Despite positive selection detected in three Alborz isolates, it has not led to mutations affecting Tax function and virulence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Human T-lymphotropic virus (HTLV) is a family of retroviruses that primarily affect T cells, a type of white blood cell essential for the immune system. There are two main types of HTLV which are HTLV-1 and HTLV-2. These viruses share some similarities but also exhibit distinct characteristics and clinical disorders [1]. Human T-cell lymphotropic virus type 1 (HTLV-1) belongs to the Retroviridae family, specifically categorized within the Deltaretrovirus genus. The genome of this virus is a positive, single-stranded RNA and spreads through cell to cell transmission within the body [2,3,4].
HTLV-1 is notably linked to two debilitating conditions: adult T-cell leukemia/lymphoma (ATLL) and HTLV-1 associated myelopathy tropical spastic paraparesis (HAM/TSP). While majority of HTLV-1 infected individuals remain as asymptomatic carriers (ACs), about 1–5% of them undergo clonal expansion of infected CD4+ T-cells and develop ATLL after a long latency period. Detection of oligoclonal and monoclonal expansion of infected cells via analysis of proviral integration sites and/or profiling of T cells receptor repertoire is documented as a risk factor for ATLL onset and development [5,6,7,8,9]. HAM/TSP, on the other hand, denotes a persistent inflammation affecting both the white and gray matter of the spinal cord [10] impacting approximately 0.25–3% of individuals infected with HTLV-1. This progressive condition manifests with symptoms akin to urinary dysfunction and those resembling multiple sclerosis (MS). During the course of this ailment, CD8+ cells respond to the virus by targeting Tax, leading to the production of inflammatory cytokines that contribute to demyelination and axonal damage [11, 12].
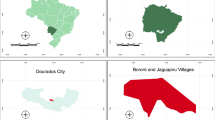
Current estimates suggest that 10–20 million individuals worldwide are infected with HTLV-1. Notable endemic regions include southern Japan, parts of southern and western Africa, South America, Romania, the Solomon Islands in Australia, and certain areas in the Middle East [13]. HTLV-1 has been found in nearly every province in Iran, but not all are classified as endemic due to inconsistent screening. The virus was first discovered in Africa in 1980, and by 1990, HTLV-1 infection was identified in Jews from Mashhad, Iran [14, 15]. In a survey conducted by Farid et al. in 1993, a study revealed that the prevalence of HTLV-1 in Mashhad was 2.3%, with the virus classified within the cosmopolitan molecular group [16].
HTLV-1 infection has also been documented in Alborz province, with a reported seroprevalence of 0.057% among blood donors [17]. The origin of HTLV-1 introduction into Iran is uncertain, with three proposed hypotheses: transmission through Silk Road trade routes, introduction via enslaved Africans, and potential spread during the Mongol invasion or via pilgrims to holy shrine [18]. Among various modes of transmission, it is crucial to highlight that breastfeeding from an infected mother to her infant and the transfusion of infected blood samples are particularly significant in facilitating the virus’s spread within society. Studying the phylogeny of HTLV-1 is crucial for understanding the virus’s origin, evolution, and how it spreads [19]. Unlike other retroviruses such as HIV, HTLV-1 genome is very stable. Because HTLV-1 mainly expands in vivo via clonal proliferation of infected cells, not infectious transmission of viral particles mediated by reverse transcription. However, it has been reported that the genome of infected host cells accumulates somatic mutations and copy number alterations which eventually result in transformation of HTLV-1 infected cells and ATLL development [20,21,22]. LTR is preferred for phylogenetic analysis for several reasons: it contains variable information, is less affected by the environment, and has a wealth of existing research data [23]. Based on phylogenetic analysis of LTR sequences, researchers have classified HTLV-1 strains into seven subtypes (a–g) to date. While must subtypes are within A–D, a limited number of strains from Central Africa fall into other atypical subtypes (E, F, G) [13]. Tax, which is HTLV-1 oncoprotein leads to dysregulation of gene expression in HTLV-1 infected cells. Studying the variations and strains of Tax can provide valuable insights not only into phylogenetic research but also into the virulence of HTLV-1.
Despite the limited data on HTLV-1 phylogeny and prevalence in Alborz province, it is recognized as an endemic region for HTLV-1. This study aims to assess HTLV-1 prevalence among blood donors and elucidate the phylogeny, LTR, and Tax evolutions of HTLV-1 in the region. Following the confirmation of viral infection, two specific regions of Tax and LTR were chosen for phylogenetic analysis. The aim of this study is to investigate HTLV-1 prevalence among blood donors and explore the phylogeny variations of HTLV-1 in Alborz province.
Materials and methods
Study population
Each month around 1500 individuals refer to Blood Transfusion Organization of Alborz (BTOA) and other laboratory centers for blood donation that means approximately 15,000 individuals per year. In our cross sectional study (2020–2021), among the blood donor population of Alborz province from 15 thousand samples, 19 were confirmed to be HTLV positive. Infection screening was conducted in BTOA by Enzyme Immuno Assay (EIA).
In Table 1, we provide the frequency distribution and mean age of the studied population. The population is categorized into two groups based on gender. Among the participants, there were 5 females, constituting 26.3% of the population, with a mean age of 48 years. In contrast, the male participants numbered 14, making up 73.7% of the population, and had a slightly higher mean age of 50.86 years. These statistics provide an overview of the gender distribution and average age within the study group. This study was confirmed by Ethical committee of Alborz University of Medical Sciences (IR.ABZUMS.REC.1398.082).
DNA extraction and PCR
Purified DNA was collected from isolated white blood cells (WBCs) of EDTA-treated blood samples utilizing ROJE kit (DNsol, ROJE, Iran) according to manufactures guidelines. Four pairs of primers were designed, Partial LTR (PLTR) and Partial HBZ (PHBZ) for infection confirmation, Full LTR (FLTR) and Full Tax (FTax) for sequencing. The primers’ sequences for each mentioned genes are illustrated in Table 2. PCR and subsequent 1% Agarose gel electrophoresis was performed for PLTR and PHBZ and HTLV infection was confirmed for all 19 samples. PCR was also conducted for FLTR and FTax fallowing by 1% Agarose gel electrophoresis. The first step of PCR consists of initial denaturation, which was performed at 94 °C for 4 min. The denaturation step was held at 95 °C for 40 s and then annealing was done for each gene. The annealing temperature was 62 °C for pLTR, 60 °C for pHBZ, 62 °C for FLTR and 58 °C for FTax. All these annealing temperatures were done in 40 s. Subsequently, extension was done at 72 °C for 5 min for all genes. The PCR thermocycles are shown in Table 3.
DNA sequencing
From whole PCR product, the amplified segments of the LTR and Tax genes were sent to the Codon Company for sequencing. The Sanger method was used to determine the LTR and Tax gene segments. The resulting sequences were analyzed using BLAST and their accuracy was assessed in NCBI. The confirmed sequences were then documented in Gene Bank. BioEdit was used to analyze the sequences. Firstly, low-quality nucleotides at the beginning and end of the chromatograms were removed, and the entire sequences were corrected. Then, both sequences were assembled and mismatches were detected. Finally, the corrected sequences were saved as FASTA files.
Phylogeny tree designing
Resource sequences representing various virus subtypes were sourced from the NCBI database. These sequences were subjected to multiple alignments using BioEdit software and then saved in FASTA format. For the construction of phylogenetic trees, MEGA-X software was employed, utilizing the Maximum Likelihood, and Kimura Two-Parameter models. To ensure the reliability of these phylogenetic trees, Bootstrap analysis with 1000 replicates was conducted.
Results
Study population
During a 1-year period, approximately 15,000 blood donors were screened. Out of this sample, 19 individuals were identified as HTLV-1 positive. After conducting confirmatory tests. This left us with 19 confirmed cases of HTLV-1 infection, all of whom were subjected to confirmation through PLTR, PHBZ (Fig. 1). Consequently, the prevalence of HTLV-1 infection within the Alborz blood donor population was determined to be 0.13%. It is noteworthy that a substantial majority, 73.7%, of the infected individuals were male, suggesting that HTLV-1 infection is more prevalent among men. However, it is important to consider that various factors may have influenced this finding, such as differences in blood donation patterns between genders. Furthermore no cases of HTLV-2 infection were detected within the blood donor population in this study.
Gel electrophoresis image regarding PLTR, PHBZ, FTax and FLTR: In this gel electrophoresis image, we present the outcomes of our investigation into the presence of HTLV-1 and the amplification of particular genomic regions. The DNA fragments were separated through electrophoresis and subsequently visualized. First band is for HBZ and band two is the leader. PLTR and PHBZ were used for diagnosis and FLTR, Tax for phylogeny
DNA sequencing and mutational analysis
The sequences FTax gene of 19 confirmed HTLV-1 infected patients were analyzed and the results demonstrated that, although some mutations have occurred in these regions of genome but they have not resulted in a significant modification in LTR and Tax genes. The results of the mutational analysis of the nucleotide and amino acid sequences of Tax show that, although, positive selection has occurred in 3 isolations and negative selection in 16 isolations of Alborz blood donors and the virus has the tendency to modify its Tax gene segment, these mutations are not efficient for a fundamental change in Tax activity and function. And the Tax sequences are about 99% similar with the reference gene and the most similarity is between 240 and 310 amino acid sequences (Fig. 2).
Comparative sequences mutations according to Reference sequence. Analysis of the FTax gene sequences from 19 HTLV-1 infected patients revealed mutations, but these didn’t significantly alter the Tax genes. Mutational analysis of Tax sequences in Alborz blood donors indicated positive selection in 3 cases and negative selection in 16 cases
Phylogeny tree
The phylogeny results of our study on the LTR region of HTLV virus showed infection by type 1 and subtype (cosmopolitan), which was very similar to studies conducted in Japan, Canada, Germany, and also studies from Africa [24]. The results of this gene are shown in Fig. 3.
Tax phylogeny results also showed relatively similar results to LTR and the phylogeny analysis of this gene showed the closeness of the subtype involved in Alborz province with studies in the mentioned countries along with a study from America. The results of the Tax survey are also shown in Fig. 4.
Discussion
HTLV-1 infection prevalence in this study is reported to be 0.13% which is more than the previous report from the blood donors’ population of Alborz province where the prevalence was reported to be 0.057% [17]. This result may has stemmed from the high rate of migration to Alborz province during the last few years, where Alborz population was 2,712,400 in 2015 year and by 2020 this number has grown to 3,700,000. No significant sequence mutation differences were seen compared to our previous researches [24, 25].
Since the identification of HTLV-1, numerous studies have investigated its prevalence across diverse groups. These investigations have spanned demographics like blood donors, pregnant women, and vulnerable populations such as individuals with conditions like thalassemia, and those undergoing hemodialysis. These groups are crucial due to their reliance on blood products, offering crucial insights into HTLV-1 prevalence in the general population. Following the report of HTLV-1 infection in Mashhad, individuals referred for blood donation in seven Iranian provinces (Alborz, Ardabil, Gilan, North Khorasan, Razavi Khorasan, South Khorasan, West Azerbaijan) are now routinely screened for HTLV-1 infection [26].
HTLV-1 infection prevalence in blood donors are evaluated in several studies in different provinces of Iran. The prevalence of 0.13% for HTLV-1 infection in Alborz blood donors is lower than (Mashhad, 2002, 0.77%), (Chaharmaha-Bakhtiari, 2005–2006, 0.62%), (West Azerbaijan, 2005–2006, 0.34%), (Ilam, 2006–2007, 0.21%), (Mashhad, 2011–2013, 0.18%), (Hormozgan, 2007–2008, 0.18%), and (Sabzevar, 2009–2012, 0.14%). However, this infection prevalence has increased from 2009 that the HTLV-1 infection prevalence in Alborz blood donors was 0.11% and it is about ten times greater than the prevalence in Bushehr in 2002–2003, 0.013% [27].
In a study over general population of Mashhad in 2011, it was demonstrated that HTLV-1 infection prevalence was 2.12% with no significant difference between males and females. The HTLV-1 virus in this study reported to be from the cosmopolitan subtype-a and HTLV-2 seropositivity was 0.12% [28]. Compared to the current study, HTLV-1 infection showed a more balanced distribution between males and females. HTLV-2 infection was present among Alborz blood donors but not in this particular study. The prevalence of infection in Alborz was notably higher than the 0.13% prevalence reported in this study, likely due to the higher prevalence in Mashhad compared to Alborz. Those who donate blood often have more awareness of high-risk activities for blood-borne and sexually transmitted diseases, potentially reducing their exposure to HTLV-1 infection. Moreover, HTLV-1 strains in Mashhad exhibit over 99% similarity to strains found in South India, suggesting a potential common ancestor of infection [27]. However, the strains from Alborz blood donors in this study were highly similar with the strains from Japan, China, and Canada.
HTLV-1 infection prevalence in Golestan province, was assessed among blood donors and the result demonstrated a 0.09% infection prevalence and the sequences of isolates was related to the subtype a (cosmopolitan) subgroup A and had a common source with the Khorasan’ isolates [29]. This study shows similarity with our research which may be an explain for their common origin. The overall prevalence of HTLV-I infection was 1.66 in Sabzevar and the Phylogenetic analysis revealed that the HTLV-I subtypes circulating in this city belonged to the cosmopolitan subtype, suggesting that the origin of the virus is the same as in Mashhad [18]. The overall HTLV-1 infection prevalence in Torbat-e-Heydarieh was reported 2.15% and no significant difference was observed in HTLV-1 sero-reactivity between males and females that is in contrast with our study. Phylogenetic analysis demonstrated that the LTR sequence from Torbat-e Heydarieh belongs to the group A (cosmopolitan) [24]. Compared to our study, we have also seen the cosmopolitan subtype which shows similarity to sabzevar study. In a study by Rafatpanah et al., sero-prevalence of HTLV-1 was observed in 2% of the participants (8 out of 400), while the actual prevalence among those with HTLV-1 provirus in their lymphocytes was 1.25%. The presence of HTLV-1 infection showed significant associations with factors like age, marital status, and a history of blood transfusion (P < 0.05). Regarding the phylogenetic analysis, it indicated that the predominant HTLV-1 sequence type in Torbat-e Heydarieh belongs to the cosmopolitan subtype A. Notably, the HTLV-1 prevalence in Torbat-e Heydarieh (1.25%) is notably lower in comparison to Mashhad (2–3%) and Neishabour (3.5–5%), both located within the Khorasan province. This disparity suggests that factors like travel, population mixing through activities such as marriage, bureaucratic engagements, occupation, and economic interactions may play a pivotal role in the potential spread of HTLV-1 within this isolated city [24].
In Tehran where is in high contact with Alborz province the prevalence of HTLV-1 infection was reported to be 0.42% in 1996 and 0.5% in Karaj in the blood donors. Alborz is located in close proximity of Tehran and people commute to work from Alborz to Tehran and vice versa (Karaj is the capital city of Alborz province) [30]. These two cities are the destination for many immigrants from other provinces because of the higher job opportunity and this will result in the growth in the population and the increase in the infection prevalence of many blood-born or sexually transmitted disease.
Studies in other countries have also been conducted on the prevalence of HTLV 1, 2 especially in countries where this virus is endemic.
Salvador in Brazil has one of the highest prevalence rates of HTLV-1 among cities. The reported prevalence of the virus in this region is reported 1.48%. Among the infected population, the majority are women. Interestingly, children under 17 years old have the lowest prevalence rate of the virus [31]. A study conducted in Australia examined gag, pol, env, Tax, and LTR of HTLV-1 among individuals infected with HTLV. The researchers identified subtype 1c of the virus. The proviral strains showed a very high level of genetic diversity, particularly in the northern and southern regions of Australia. It appears that the virus evolved into two clades of HTLV 1c in these two geographical areas [32]. Another study conducted in Brazil investigated the infected population of immigrants from Japan to this country and found that 6.8% of samples were positive. Among 14 patients whose samples were sequenced, all exhibited the Cosmopolitan subtype. Half belonged to subgroup A (transcontinental), and the other half to subgroup B (Japanese). The research emphasized age, particularly above 45, as a significant risk factor for contracting the virus [33]. Compared to our research, we have only found subgroup A and there is no trace of subgroup B. The absence of subgroup B of HTLV-1 in Alborz, while being found in Brazil, likely stems from diverse geographical distributions, population genetics, and transmission dynamics.
Epidemiological investigations and sequencing analyses are crucial in understanding the disease status, identifying the subtypes present in different regions, conducting genetic studies, and ultimately controlling viral infections in society. Although our study was statistically acceptable, we suggest conducting more extensive research to gain a more accurate understanding of the disease’s epidemiological situation. Our study’s limitation is that it shows the incidence only within the year of study (2020–2021), and the prevalence of HTLV-1 can change within the years.
Conclusion
Based on this study, we can assume that Alborz province is an endemic area for HTLV-1 infection with the high prevalence of 0.13% among Alborz’s blood donors and the screening for this infection should still be done in this province. The phylogenic analyses according to the LTR region demonstrated the HTLV-1 virus circulating in Alborz province belongs to the subtype a (cosmopolitan), subgroup A. The sequences had a considerable similarity with the strains from Japan and China. In this study mutations in LTR and Tax genes were detected but they were not sufficient for a fundamental modification in these two genes and however, 3 positive and 16 negative selections were reported in the Tax gene, no functional mutation is detectable in the Tax protein and its virulence.
Data Availability
The information used in this paper can be available upon request.
References
Martinez MP, Al-Saleem J, Green PL (2019) Comparative virology of HTLV-1 and HTLV-2. Retrovirology 16(1):1–12
Ohtsuki Y, Akagi T, Takahashi K, Miyoshi I (1982) Ultrastructural study on type C virus particles in a human cord T-cell line established by co-cultivation with adult T-cell leukemia cells. Adv Virol 73(1):69–73
Nejmeddine M, Bangham CR (2010) The HTLV-1 virological synapse. Viruses 2(7):1427–1447
Yamaguchi K, Watanabe T (2002) Human T lymphotropic virus type-I and adult T-cell leukemia in Japan. Int J Hematol 76(Suppl 2):240–245
Firouzi S, López Y, Suzuki Y, Nakai K, Sugano S, Yamochi T, Watanabe T (2014) Development and validation of a new high-throughput method to investigate the clonality of HTLV-1-infected cells based on provirus integration sites. Genome Med 6(6):1–15
Firouzi S, Farmanbar A, Nakai K, Iwanaga M, Uchimaru K, Utsunomiya A et al (2017) Clonality of HTLV-1–infected T cells as a risk indicator for development and progression of adult T-cell leukemia. Blood Adv 1(15):1195–1205
Farmanbar A, Firouzi S, Makałowski W, Iwanaga M, Uchimaru K, Utsunomiya A et al (2017) Inferring clonal structure in HTLV-1-infected individuals: towards bridging the gap between analysis and visualization. Hum Genomics 11(1):1–13
Farmanbar A, Firouzi S, Park S-J, Nakai K, Uchimaru K, Watanabe T (2017) Multidisciplinary insight into clonal expansion of HTLV-1-infected cells in adult T-cell leukemia via modeling by deterministic finite automata coupled with high-throughput sequencing. BMC Med Genomics 10:1–12
Farmanbar A, Kneller R, Firouzi S (2019) RNA sequencing identifies clonal structure of T-cell repertoires in patients with adult T-cell leukemia/lymphoma. NPJ Genom Med 4(1):10
Verdonck K, Gonzalez E, Van Dooren S, Vandamme AM, Vanham G, Gotuzzo E (2007) Human T-lymphotropic virus 1: recent knowledge about an ancient infection. Lancet Infect Dis 7(4):266–281
Gessain A, Barin F, Vernant JC, Gout O, Maurs L, Calender A, de Thé G (1985) Antibodies to human T-lymphotropic virus type-I in patients with tropical spastic paraparesis. The Lancet (London, England) 2(8452):407–410
Osame M (2002) Pathological mechanisms of human T-cell lymphotropic virus type I-associated myelopathy (HAM/TSP). J Neurovirol 8(5):359–364
Gessain A, Cassar O (2012) Epidemiological aspects and world distribution of HTLV-1 infection. Front Microbiol 3:388
Poiesz BJ, Ruscetti FW, Gazdar AF, Bunn PA, Minna JD, Gallo RC (1980) Detection and isolation of type C retrovirus particles from fresh and cultured lymphocytes of a patient with cutaneous T-cell lymphoma. Proc Natl Acad Sci USA 77(12):7415–7419
Sidi Y, Meytes D, Shohat B, Fenig E, Weisbort Y, Lee H et al (1990) Adult T-cell lymphoma in Israeli patients of Iranian origin. Cancer 65(3):590–593
Farid R, Etemadi M, Baradaran H, Nikbin B (1993) Seroepidemiology and virology of HTLV-1 in the city of Mashhad, northeastern Iran. Serodiagn Immunother Infect Dis 5(4):251–252
Karimi G, Zadsar M, Pourfathollah AA (2017) Seroprevalence and geographical distribution of human T-lymphotropic virus type 1 among volunteer blood donors in endemic areas of Iran. Virol J. https://doi.org/10.1186/s12985-017-0693-9
Azarpazhooh MR, Hasanpour K, Ghanbari M, Rezaee SAR, Mashkani B, Hedayati-Moghaddam MR et al (2012) Human T-lymphotropic virus type 1 prevalence in Northeastern Iran, Sabzevar: an epidemiologic-based study and phylogenetic analysis. AIDS Res Hum Retrovir 28(9):895–901
Pashabayg CR, Momenifar N, Malekpour SA, Sadeghi M, Foroushani AR, Rafatpanah H et al (2020) Phylogenetic and phylodynamic study of human T-cell lymphotropic virus type 1 (HTLV-1) in Iran. Infect Genet Evol 85:104426
Kataoka K, Nagata Y, Kitanaka A, Shiraishi Y, Shimamura T, Yasunaga J-I et al (2015) Integrated molecular analysis of adult T cell leukemia/lymphoma. Nat Genet 47(11):1304–1315
Sun N, Yau SS-T (2022) In-depth investigation of the point mutation pattern of HIV-1. Front Cell Infect Microbiol 12:1033481
Farmanbar A, Firouzi S, Makałowski W, Kneller R, Iwanaga M, Utsunomiya A et al (2018) Mutational intratumor heterogeneity is a complex and early event in the development of adult T-cell leukemia/lymphoma. Neoplasia 20(9):883–893
Miura T, Fukunaga T, Igarashi T, Yamashita M, Ido E, Funahashi S et al (1994) Phylogenetic subtypes of human T-lymphotropic virus type I and their relations to the anthropological background. Proc Natl Acad Sci USA 91(3):1124–1127
Rafatpanah H, Torkamani M, Valizadeh N, Vakili R, Meshkani B, Khademi H et al (2016) Prevalence and phylogenetic analysis of HTLV-1 in a segregated population in Iran. J Med Virol 88(7):1247–1253
Abedi F, Mozhgani S-H, Rahimzadegan M, Gudarzi H, Valizadeh N, Rezaee SA (2017) Prevalence and phylogenic study of human T-lymphotropic virus 1 in patients with thalassemia in the northeast of Iran. Future Virol 12(5):253–258
Karimi G, Zadsar M, Pourfathollah AA (2017) Seroprevalence and geographical distribution of human T-lymphotropic virus type 1 among volunteer blood donors in endemic areas of Iran. Virol J 14:1–9
Pirayeshfard L, Sharifi Z, Amini-Kafiabad S, Haghnazari SN (2018) Phylogenetic analysis of HTLV-1 in Iranian blood donors, HIV-1 positive patients and patients with beta thalassemia. J Med Virol 90(8):1398–1405
Rafatpanah H, Hedayati-Moghaddam MR, Fathimoghadam F, Bidkhori HR, Shamsian SK, Ahmadi S et al (2011) High prevalence of HTLV-I infection in Mashhad, Northeast Iran: a population-based seroepidemiology survey. J Clin Virol 52(3):172–176
Mehrabi Habibabadi H, Parsania M, Pourfathollah AA, Bahrami A, Sharifi Z (2021) Prevalence and phylogenetic analysis of HTLV-1 in blood donors in Golestan Province, in the Northeast of Iran. J Virol Methods 290:114073. https://doi.org/10.1016/j.jviromet.2021.114073
Rezvan H, Farhadi M, Ahmadi J, Tarvian SJBJ (1995) Preliminary survey of frequency of HTLV-I/II among blood donors in Iran. Blood J (Sci J Iran Blood Transfus Org) 2(1):23–28
Nunes D, Boa-Sorte N, Grassi MFR, Taylor GP, Teixeira MG, Barreto ML et al (2017) HTLV-1 is predominantly sexually transmitted in Salvador, the city with the highest HTLV-1 prevalence in Brazil. PLoS ONE 12(2):e0171303
Cassar O, Einsiedel L, Afonso PV, Gessain A (2013) Human T-cell lymphotropic virus type 1 subtype C molecular variants among indigenous Australians: new insights into the molecular epidemiology of HTLV-1 in Australo-Melanesia. PLoS Negl Trop Dis 7(9):e2418
Bandeira LM, Uehara SN, Asato MA, Aguena GS, Maedo CM, Benites NH et al (2015) High prevalence of HTLV-1 infection among Japanese immigrants in non-endemic area of Brazil. PLoS Negl Trop Dis 9(4):e0003691
Acknowledgements
We would like to express our heartfelt appreciation to the dedicated participation of Blood Transfusion Organization of Alborz staff.
Funding
The study was supported by Alborz University of Medical Sciences (1397-03-01-2071).
Author information
Authors and Affiliations
Contributions
MS, FH-S, AL, SS: methodology, writing original draft, validation, investigation. SY, MM, KK, MSH: validation, investigation. S-HM: conceptualization, supervision, validation, review and editing.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
Ethical approval was obtained from Alborz University of Medical Sciences (IR.ABZUMS.REC.1398.082).
Additional information
Edited by Simon Scott.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Safavi, M., Habibian-Sezavar, F., Letafati, A. et al. Determination of molecular epidemiologic pattern of human T-lymphotropic virus type 1 (HTLV-1) in Alborz province, Iran. Virus Genes 60, 117–125 (2024). https://doi.org/10.1007/s11262-024-02051-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11262-024-02051-0