Abstract
The epidermal growth factor (EGF) plays a crucial role in the control of uterine cell proliferation, growth and differentiation. This study was designed to investigate the spatiotemporal expression pattern and localization of the EGF receptor/ligand system during the process of uterine involution using immunohistochemistry. Our results indicated that the expression of the ErbB/HER receptors and their ligands varied with structural changes in the uterus at different days of involution. Supranuclear punctate ErbB1 immunostaining was observed in the luminal and glandular epithelial cells and endometrial fibroblasts. Moderate ErbB2/HER2 immunoreactivity was observed in the lateral membrane and cytoplasm of the epithelial cells on the 1st, 3rd and 5th days and was decreased on the other days of involution. The amount of nuclear and cytoplasmic ErbB3/HER3 and ErbB4/HER4 immunostaining remained constant throughout the postpartum period. The EGF immunoreaction was weak in the luminal and glandular epithelium throughout the involution period. Although the cytoplasmic AREG immunoreactivity in the glandular epithelium was stronger on the 1st and 3rd days compared with the other days of involution, NRG1 immunostaining was weak on the 1st and 3rd days and was moderate in the apical cytoplasm on the 10th and 15th days of involution. The macrophages displayed strong cytoplasmic immunoreactivity for ErbB3/HER3, ErbB4/HER4, EGF, AREG and NRG. Strong, moderate and weak immunostaining for ErbB2/HER2, ErbB4/HER4 and other proteins (ErbB1, ErbB3, AREG and NRG), respectively, was present in the myometrial smooth muscle cells. These findings support the hypothesis that the EGFsystem plays a role in the development of various physiological changes associated with uterine involution.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The postparturient period, which is also termed also puerperium or postpartum, is characterized by uterine involution and the restoration of ovarian functions. Uterine involution in mammalian species is necessary for the establishment of the next pregnancy (Esslemont and Kossaibati 2000). Uterine involution is the process by which the uterus returns to its pre-pregnant state by retrogressive processes including substantial tissue destruction and subsequent tissue repair and remodelling. A reduction of in uterine size, morphological and histological changes, uterine contraction, autolysis of myometrial cells, epithelial regeneration and proliferation occurs during this process (Blackburn 2007). Tissue repair is a strategic step in uterine involution and therefore uterine involution has features in common with events that occur during the repair of other tissues (Salamonsen 2003). The tissue repair and remodelling in the uterus are regulated by several mediators such as cytokines, matrix-degrading enzymes and growth factors (Salamonsen 2003). Growth factors activate cell proliferation and differentiation by binding to their attendant tyrosine kinase receptors that are expressed in the plasma membrane. These factors exert their effects on cells through endocrine, paracrine, autocrine, or intracrine mechanisms. The epidermal growth factor (EGF) family is one group of growth factor that plays a role in normal development, differentiation, migration, proliferation, embryogenesis, wound healing and apoptosis, which are essential for the viability of multicellular organisms (Bazley and Gullick 2005). The epidermal growth factor (EGF) system is a type I growth factor family consisting of four receptors: human EGF receptor 1 (HER1) (also called EGF-receptor/EGFR/ErbB1), HER2 (also called ErbB2/Neu), HER3 (also called ErbB3) and HER4 (also called ErbB4). These four receptors are widely expressed in epithelial, mesenchymal, and neuronal tissues. They share a common structural feature, but differ in their ligand specificities and kinase activities. The EGF receptors are transmembrane glycoproteins with an extracellular ligand-binding domain, a transmembrane region, a protein tyrosine kinase domain, and a C-terminal autophosphorylation domain. The intracellular domains of ErbB1/HER1, ErbB2/HER2 and ErbB4/HER4 display tyrosine kinase activity. Like other growth factor receptors, the molecules of the ErbB family form dimers when stimulated by a ligand, and they phosphorylate other molecules to activate certain signalling pathways. ErbB1 and ErbB4 form either homo- or heterodimers, whereas ErbB2 functions as a cofactor for the other receptors, and ErbB3 requires heterodimerization because of its lack of tyrosine kinase activity (Niikura et al. 1996; Ejskjaer et al. 2005).
Many ligands, or EGF-related peptide growth factors, trigger an intracellular signalling cascade upon binding to their receptors, causing changes within the target cells. Currently, seven ligands for EGFR have been identified: epidermal growth factor (EGF), transforming growth factor-α (TGF-α), heparin-binding EGF-like growth factor (HB-EGF), amphiregulin (AREG), betacellulin (BTC), epiregulin (EREG), and epigen. In mammals, these ligands and four receptors comprise the EGFR/ligand system. EGF, TGFα, AREG and epigen bind to EGFR. HB-EGF, EREG and BTC bind equally to EGFR and ErbB4. ErbB2 does not have a known ligand, but recent structural studies suggest that ErbB2 is most likely regulated by some ligand (Schneider and Wolf 2008). ErbB3 and ErbB4 are also targets of a group of structurally related cell-cell signalling proteins known as neuregulins (NRG) [Neu differentiation factor (NDF) or heregulins]. NRG-1 and NRG-2 bind to ErbB3 and ErbB4, and NRG-3 and NRG-4 bind to ErbB4 but not ErbB3 (Falls 2003).
Multiple research papers have demonstrated that EGFRs/ErbB/HER and their ligands play a crucial role in the control of uterine cell growth and differentiation during the menstrual or sexual cycle, pregnancy and implantation (Mukku and Stancel 1985; DiAugustine et al. 1988; Smith et al. 1991; Zhang et al. 1992; Das et al. 1995; Boomsma et al. 1997; Lennard et al. 1998; Tamada et al. 2000; Yue et al. 2000; Klonisch et al. 2001; Wollenhaupt et al. 2004; Brown et al. 2004; Sağsöz and Ketani 2010; Kida et al. 2010). The EGF family of ligands and their receptors are expressed in the uterus and the embryo in a temporal and cell type-specific fashion (Lim et al. 1998). The rat uterus contains specific, high-affinity EGF receptors. These receptors are present in the epithelial, stromal and myometrial cells of the uterus (Stancel et al. 1987). The EGF receptors localize in both the plasma membrane and in the cytoplasm of all cell types, and EGFRs may stimulate the growth of epithelial cells (Onagbesan et al. 1994). The uterine epithelial cell proliferation directed by EGF-like ligands or steroid hormones (oestrogen) is mediated either indirectly via EGFR in the uterine stromal cells in a paracrine manner or via other members of the ErbB family in uterine epithelial cells (Lim et al. 1997). Ligands, such as EGF, TGF-α, AREG, HB-EGF, EREG, BCL and NRG/heregulin are produced by both uterine epithelial and stromal cells (Gharib-Hamrouche et al. 1995; Kim et al. 1995; Das et al. 1997; Tsark et al. 1997; Reese et al. 1998) and secreted into the uterine lumen (Nelson et al. 1992; Kim et al. 1995).
The binding of EGF to the EGFR induces the proliferation of uterine epithelial cells in an autocrine manner, but stromal cell count was not affected by oestradiol or EGF in some mammals. EGF expression changes with the oestrous cycle in the adult uterus (Huet-Hudson et al. 1990); oestrogen may therefore be required for EGF synthesis in the adult uterus, and changes in uterine EGF expression in adult female mice are thought to be caused by cyclic changes in blood oestrogen levels (DiAugustine et al. 1988). Gardner et al. (Gardner et al. 1987) reported that EGF stimulated contractions in uterine tissues removed from immature and adult rats. EGF and TGF-α are known to be important for early embryonic growth and differentiation (Werb 1990).
AREG is a member of the epidermal growth factor family and is known to be expressed in the luminal epithelium of the mouse uterus. It appears that amphiregulin may participate in cellular infiltration in the process of implantation (Lee et al. 2006). AREG is known to be regulated by the progesterone induced by oestrogen. However, it has been shown that AREG mRNA is expressed throughout the oestrous cycle in the mouse uterus (Lee et al. 2005).
Of the neuregulins, the NRG-1 isoforms (Neu differentiation factor, NDF; sensory and motor neuron-derived factor, SMDF) are implantation-specific genes that are generated at the stage when the embryo attaches to the uterus and are required for the implantation of the blastocyst (Brown et al. 2004). The expression patterns of EGF, TGF-α, AREG and HB-EGF in the uterus during the peri-implantation period and their responsiveness to sex steroid hormones have been examined (Huet-Hudson et al. 1990; Das et al. 1995; Tamada et al. 2002). Ligand-receptor signalling through the EGF family of growth factors in the uterus and embryo is thought to be important for implantation, but there is currently no knowledge about its activity or that of the EGF receptors and their ligands during uterine involution. Furthermore, the mechanisms that regulate uterine involution are not completely understood. The uterus is a heterogeneous tissue consisting of different cell types. The uterus is lined with a thick mucosa, the endometrium, which is surrounded by a thick wall of smooth muscle, the myometrium. Both the endometrium and myometrium are characterized by ongoing proliferation and differentiation throughout almost half of the lifespan of a female, and it is tempting to hypothesize that the EGFR/ligand system plays a pivotal role in controlling these reactions during tissue repair and remodelling of the postpartum uterus. To elucidate the reason for this, we initiated studies using a rat model to examine the expression patterns of the ErbB receptors and ligands in the uterus during postpartum involution (days 1–15 of the postpartum period).
Materials and methods
Animals and tissue preparation
The female Rattus norvegicus (Wistar) rats (250–300 g, 6–8 weeks) used in the study were obtained from a holding that performs regular production, and did not have any problems related to flock health (Experimental Animals Center, University of Erciyes, Kayseri). The animals were housed under controlled temperature (20 ± 2 °C) and photoperiod (12:12 h L:D) conditions. The midpoint of the light period was 12.00 h. Rats were given food and water ad libitum. Vaginal smears were taken daily from the rats in the morning (09.00–10.00 h) to identify their oestrus cycles. Male rats housed in similar conditions were allowed to mate with female rats at oestrus. The day on which sperm was first observed in a vaginal smear was counted as day 1 of pregnancy. The day of delivery of pups was designated as day 1 postpartum. For the determination of postpartum changes in the EGF receptor and ligands, uteri were collected on days 1, 3, 5, 10, and 15 postpartum (five rats per group) under deep anaesthesia (urethane 1.5 g/kg i.p). Adherent fat and blood vessels were trimmed from the uteri. The uteri were fixed in a 10 % formol-alcohol solution for 18 h, dehydrated, cleared, and embedded in Paraplast. This study was approved by the Department of Experimental Animals Ethic Committee, University of Erciyes (approval number 08/23).
Histology and Immunohistochemistry
Twelve slides were prepared from each sample, and each slide contained a minimum of three sections cut to be 5 μm thick. The tissue sections were mounted on glass slides coated with 3-aminopropyl-ethoxy-silane (APES) (Sigma-Aldrich Chemicals, St. Louis, MO, USA) and dried at 37 °C. To examine the general structure of the uterus during the involution period, the first slide was stained with Crosman’s triple stain (Crossman 1937). The second slide was stained with Dominici’s stain for the determination of mast cells (Aker 1954). The following adjacent slides were immunostained for macrophage markers (CD68, Macrophage Marker Ab-3, 1:50 dilution, Cat No: MS-397, Thermo Scientific and CD163 antibody (ED2), 1:50 dilution, sc-58965, Santa Cruz Biotechnology), vimentin (Leica Biosystems, Novacastra, Kat no: NCL-L-VIM-V9, 1:200 dilution), and EGF receptors [EGFR (1005, Santa Cruz Biotechnology, USA, sc-03, 1:50 dilution), ErbB2 (Neu) (F-11, Santa Cruz Biotechnology, sc-7301, USA, 1:300 dilution), ErbB3 (C-17, Santa Cruz Biotechnology, sc-285, USA, 1:50), ErbB4 (C-18, Santa Cruz Biotechnology, USA, sc-283, 1:100)] and ligands [(EGF (Z-12, Santa Cruz Biotechnology, USA, sc-275, 1:50), NRG-1 (H-210, Santa Cruz Biotechnology, USA, sc-28916, 1:50) or AREG (H-155, Santa Cruz Biotechnology, USA, sc-25436, 1:50)].
Immunohistochemistry was performed using a streptavidin–biotin–peroxidase detection system (Thermo Fisher Scientific Lab Vision Corporation, Fremont, CA, USA). Briefly, sections were de-paraffinized in xylene, rehydrated through a graded series of ethanol, and then rinsed several times with phosphate-buffered saline (PBS; pH 7,4). Endogenous peroxidase activity was blocked by incubating the slides in 3 % H2O2 in methanol for 15 min at room temperature, and the slides were then washed with PBS two times. Antigen retrieval was performed by boiling in 0.01 M citrate buffer (pH 6.0) for 30 min at 80 °C using a water bath, and the samples were cooled for 20 min prior to immunostaining (Liman et al. 2013). Sections were then washed in PBS and incubated in a blocking serum (Ultra V Block, Thermo Fisher Scientific Lab Vision Corporation, Fremont, CA, USA; TA-125UB) for 5 min at room temperature to block non-specific binding. The blocking solution was removed by tapping the slides, which were then incubated with primary antibodies overnight at 4 °C. This was followed by incubation with biotinylated goat anti-rabbit IgG (for EGFR, ErbB3, ErbB4, EGF, NRG and AREG) or biotinylated rabbit anti-mouse IgG (for CD68, CD163, Vimentin and ErbB2) for 20 min, followed by incubation with the avidin-biotin-peroxidase complex for 20 min. Between each step, sections were washed four times in PBS. The reaction was visualized using 3, 3′-diaminobenzidine tetra hydrochloride (DAB; Thermo Fisher Scientific Lab Vision Corporation, Fremont, CA, USA). After counterstaining with Gill’s hematoxylin the slides were dehydrated through an alcohol series, cleared with xylene, and mounted with coverslips using a permanent mounting medium (entellan).
The EGF receptor and ligand antibodies were obtained from Santa Cruz Biotechnology, Inc. (Santa Cruz, CA), which guarantees that the antibodies are specific for rat tissues. The specificity of immunohistochemical procedures was also verified by using negative and positive control sections. As positive controls, sections of breast carcinoma and rat mammary gland were incubated with primary antibodies because EGFRs and their ligands have been localized in the epithelial cells lining the secretory alveoli and ducts (Sağsöz and Ketani 2010). Negative control staining was performed by omitting the primary antibody and using normal rabbit IgG (Santa cruz sc-2027) instead of anti–EGFR, anti–ErbB3, anti–ErbB4, anti–EGF, anti–NRG and anti–AREG antibodies or normal mouse IgG (Santa cruz sc-2025) instead of anti–ErbB2, anti–CD68, anti–CD163, and anti–Vimentin antibodies. Non-specific staining was not detected in tissue samples from different days of the involution period. Examination was conducted using a conventional light microscope (BX51; Olympus, Tokyo, Japan).
Quantitative analysis
Immunohistochemical staining was performed in duplicate to verify results. The immunostaining was evaluated semi-quantitatively using an intensity score (IS). (Brown and Lamartiniere 2000; Alan and Liman 2012). The intensity score reflected the intensity of positive staining in the cell membranes, cytoplasm and nucleus. In this method, the intensity score (IS) was evaluated in the following manner: −, negative; +, weak staining; ++, moderate staining; and +++, strong staining.
The intensity score of the immunostaining reactions in the cells was determined by two independent researchers (E.A., N.L.), and the mean score of the two observers was calculated. The expression of the ErbB/HER receptors and their ligands (EGF, NRG, AREG) in the uterus was examined microscopically at 40×, 100×, 200× and 400× magnification. Five different cell groups were evaluated: the luminal epithelium, glandular epithelium cells, stromal cells, myometrial smooth muscle cells and blood vessels.
Results
The structural changes of the uterus during the postpartum involution period
On postpartum day 1, a thickened endometrium and myometrium were observed. The large lumen of the uterus was surrounded with mucosal folds, and the crypts were deep and irregular. The luminal epithelium, including different cell types together with intraepithelial capillary vessels, showed properties of a pseudostratified columnar epithelium. Many of the luminal epithelial cells were undergoing supranuclear vacuolation, as exhibited by small, pyknotic nuclei. The lamina propria or endometrial stroma consisted of expanded hypocellular oedematous loose connective tissue with little discernible extracellular matrix (ECM) and contained a few enlarged endometrial glands. On postpartum day 3, the intraepithelial vessels disappeared, the depth crypt decreased, and the cell density within the lamina propria increased. The endometrial thickness decreased as a result of reduction in extracellular space between the stromal fibroblasts and the distance between the endometrial glands. A marked increase in ECM staining was observed in the lamina propria. Myometrial thickness also decreased. On postpartum day 5, the lumen became narrow and shaped like the letter T. The luminal lining epithelial cells were columnar, and the vacuolization in the epithelium disappeared. A few crypts existed. The glands appeared smaller and the height of the glandular epithelium was increased compared with postpartum days 1 and 3. The thickness of the collagen fibres around the gland groups increased. On postpartum days 10 and 15, the uterus was structurally similar to that of non-pregnant females. The thickness of the endometrium and myometrium reached a minimum. The crypts disappeared completely, and the luminal epithelium consisted of columnar epithelial cells. The density of endometrial fibroblasts in the lamina propria increased and the fibroblasts showed two different locations in the endometrial stroma: subepithelial and deep stromal. The amount of fibroblasts in the subepithelial stroma was higher than in the deep stroma (Fig. 1).
In the present study, the endometrial stromal cells were typed based on their morphology and localization, using histochemical and immunohistochemical techniques. In the stroma, the vimentin-positive cells (Koumas et al. 2001), endometrial fibroblasts, and CD68- and CD163-positive cells localized particularly to the subepithelial and periglandular stroma were identified as macrophages (Fig. 2), whereas the cells that stained with Dominici’s stain and were localized to the periphery of the stromal vasculature and the blood vessels in the stratum vasculare of the myometrium were identified as mast cells. The amount of endometrial macrophages increased with the advance of postpartum days.
The immunohistochemical localization of receptors and their ligands
ErbB1 immunoreactivity was detected as punctate staining in the supranuclear region of the endometrial luminal, glandular epithelium and endometrial fibroblasts in the lamina propria during the postpartum period. During days 1 and 3 of the postpartum involution process, staining of the luminal epithelium was observed in some regions; on day 5 no such staining was observed in the prismatic epithelium, and on days 10 and 15 the entire luminal epithelium produced positive staining. As the number of endometrial fibroblasts in the oedematous mucosa on the first day of involution was lower compared with the other phases, the number of ErbB1-positive cells was also low, whereas on the other days of the postpartum involution period, an increased number of ErbB1-positive cells was detected owing to the increase in the number of endometrial fibroblasts that occurred with the structural changes. In blood vessels, the expression of ErbB1 was concentrated in the membrane of red blood cells in the lumen of the vessels but was not present in endothelial and smooth muscle cells of the vessels. In the myometrium, the smooth muscle cells showed a very weak ErbB1 expression during the postpartum period (Fig. 3, Table 1).
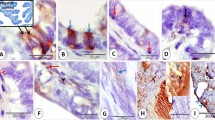
EGFR immunoreactivity in rat uterus of day 1 postpartum (PP1), day 3 postpartum (PP3), day 5 postpartum (PP5), day 10 postpartum (PP10) and day 15 postpartum (PP15) and negative control. L lumen, c crypt, Le luminal epithelium, g endometrial gland, v blood vessel, s stroma, arrow head: ErbB1 positive punctate staining in the supranuclear region of the stromal fibroblasts, arrows: ErbB1 positive punctate staining in the supranuclear region of the endometrial luminal and glandular epithelium
It was determined that the ErbB2 immunoreactivity on was localized to the cytoplasm and lateral membrane of the luminal and glandular epithelial cells. In the luminal epithelium, the cytoplasmic reactivity was of a moderate intensity on days 1, 3 and 5 of the postpartum period, and weak on postpartum days 10 and 15. The endometrial fibroblasts also showed moderate ErbB2 expression. The macrophages that were determined to be positive for CD68 and CD163, which are macrophage markers, produced a strong cytoplasmic reaction (Fig. 2). Furthermore, on all of the postpartum days investigated, the ErbB2 immunoreactivity in the myometrial myocytes, vascular endothelium and vascular smooth muscle cells was more strongly positive than that in the luminal and glandular epithelial cells (Fig. 4, Table 2).
ErbB2 immunoreactivity in rat uterus of day 1 postpartum (PP1), day 3 postpartum (PP3), day 5 postpartum (PP5), day 10 postpartum (PP10) and day 15 postpartum (PP15) and negative control. Le luminal epithelium, g endometrial gland, v blood vessel, s stroma, m myometrium, arrow: ErbB2 positive the endothelial cells, arrows head: ErbB2 positive the lateral memrane
Throughout the postpartum period, it was observed that the ErbB3 immunoreactivity was localized particularly to the apical and basal cytoplasm of the luminal and glandular epithelial cells, but some cell nuclei were also determined to be ErbB3-immunopositive. During the entire postpartum involution period, whereas the majority of the endometrial fibroblasts presented with a weak cytoplasmic and moderate nuclear staining, the macrophages produced a strong cytoplasmic staining. The mast cells found in the connective tissue surrounding the blood vessels in the endometrial stroma and the stratum vasculare of the myometrium displayed ErbB3-positive cytoplasmic staining. Blood vessels exhibited moderate ErbB3 expression in the endothelial cells. In the myometrium, the smooth muscle cells showed weak ErbB3 expression during the postpartum period (Fig. 5, Table 3).
ErbB3 immunoreactivity in rat uterus of day 1 postpartum (PP1), day 3 postpartum (PP3), day 5 postpartum (PP5), day 10 postpartum (PP10) and day 15 postpartum (PP15) and negative control. L lumen, c crypt, Le luminal epithelium, g endometrial gland, v blood vessel, s stroma, arrow: ErbB3 positive the macrophages
Throughout the postpartum period, ErbB4 was localized to the cytoplasm and membrane and was also found in the nucleus of some luminal and glandular epithelial cells, and the immunoreactivity did not vary during the postpartum period. The endometrial fibroblasts presented with moderate cytoplasmic ErbB4 immunoreactivity. The stromal macrophages produced a strong cytoplasmic reaction (Fig. 6, Table 4).
During the postpartum period, in general, the EGF immunoreactivity was weak in the luminal and glandular epithelial cells and endometrial fibroblasts. In the stroma, EGF expression was concentrated in macrophages, with the most intense expression throughout the postpartum involution period. There was no EGF expression in blood vessels or in myometrial smooth muscle cells (Fig. 7, Table 5).
EGF immunoreactivity in rat uterus of day 1 postpartum (PP1), day 3 postpartum (PP3), day 5 postpartum (PP5), day 10 postpartum (PP10) and day 15 postpartum (PP15) and negative control. L lumen, c crypt, Le luminal epithelium, g endometrial gland, v blood vessel, s stroma, m myometrium, arrows: EGF positive the macrophages
The AREG immunoreactivity was localized to the cytoplasm of the luminal and glandular epithelial cells, and the staining in the apical cytoplasm of the glands was stronger on postpartum days 1 and 3 compared with the other days. The AREG immunreactivity was also observed in the nuclei of most (but not all) luminal and glandular epithelial cells. Whereas endometrial fibroblasts presented with a nuclear reactivity (nuclear membrane), macrophages displayed an intense cytoplasmic reaction. In the myometrium, the AREG immunoreaction was very weakly positive in the nucleus and cytoplasm of the muscle cells. Blood vessels exhibited a moderate AREG expression in endothelial cells (Fig. 8, Table 6).
AREG immunoreactivity in rat uterus of day 1 postpartum (PP1), day 3 postpartum (PP3), day 5 postpartum (PP5), day 10 postpartum (PP10) and day 15 postpartum (PP15) and negative control. L lumen, c crypt, Le luminal epithelium, g endometrial gland, v blood vessel, s stroma, m myometrium, arrows: AREG positive the macrophages, arrow heads: AREG positive the nucleus
On postpartum days 1, 3, and 5 the luminal and glandular epithelial cells produced a weak cytoplasmic NRG1 immunoreaction, whereas on postpartum days 10 and 15, this immunoreaction intensified in the apical cytoplasm and reached a moderate intensity. Stromal macrophages exhibited strong NRG1 expression during the postpartum period, whereas blood vessels showed moderate NRG1 expression in the endothelial cells. In the myometrium, the NRG 1 immunoreaction was very weakly positive in the cytoplasm of the muscle cells (Fig. 9, Table 7).
NRG-1 immunoreactivity in rat uterus of day 1 postpartum (PP1), day 3 postpartum (PP3), day 5 postpartum (PP5), day 10 postpartum (PP10) and day 15 postpartum (PP15) and negative control. L lumen, Le luminal epithelium, g endometrial gland, v blood vessel, s stroma, m myometrium, arrows: NRG-1 positive the macrophages, arrows heads: hemosiderine-load macrophages
Discussion
Our data show for the first time the localization of the receptors of the EGF system, ErbB1/HER1, ErbB2/HER2, ErbB3/HER3 and ErbB4/HER4 and three ligands (AREG, NRG and EGF) in the uterus of rats on days 1, 3, 5, 10 and 15 of the postpartum involution period by immunohistochemistry. Moreover, the results, which showed that the organization and distribution of these molecules in the endometrial and myometrial components of the uterus varied with the morphological changes that occurred during the involution process, suggest that these molecules undergo ovarian hormonal control and likely participate in the preparation of the uterus that is necessary for the establishment of the next pregnancy as previously reported in the mammalian uterus during the menstrual or oestrous cycle (Smith et al. 1991; Wang et al. 1992; Imai et al. 1995; Wollenhaupt et al. 1997; Miturski et al. 1998; Srinivasan et al. 1999; Tamada et al. 2000; Ejskjaer et al. 2005; Kida et al. 2010; Sağsöz et al. 2012; Sağsöz et al. 2014).
Endometrial repair after parturition is a critical process of uterine involution. This process consists of the regeneration and proliferation of both the epithelium and endometrial stroma (Blackburn 2007). Warbrick (1955) stated that in the rat, at the time of parturition, the uterine mucosa is lined with epithelium everywhere except at the placental sites and that re-epithelialization of the placental sites is completed within 36 h. This author suggested that this rapid regeneration is likely related to the early post-partum oestrus; in the rat the first postpartum ovulation occurs at approximately 18 h. Furthermore, Warbrick (1955) reported that during involution, areas of the uterine epithelium show a vacuolation of the columnar cells that is particularly marked 36 h post-partum. In our study, a microscopic examination of the involuting uterine mucosa of rats showed that on postpartum day 1, the luminal epithelium including different cell types together with intraepithelial capillary vessels had properties of pseudostratified columnar epithelium. Many of the luminal epithelial cells were undergoing supranuclear vacuolation, as exhibited small, pyknotic nuclei. In the luminal epithelium, the intraepithelial vessels and vacuolization disappeared on postpartum days 3 and 5, respectively. On postpartum day 5, the luminal epithelial cells were columnar and on the 10th day postpartum, the crypts disappeared completely and the epithelium showed the features of a high columnar epithelium that was similar to that of non-pregnant females at the diestrus stage of oestrous cycle (Komárek 2000).
To date, the results of studies have shown that the expressions and localizations of epidermal growth factor receptors and ligands in the luminal and glandular epithelium of endometrium are different from each other and vary according to the mammalian species and the sexual cycle. In the rat uterus during the postpartum involution period, ErbB1 was localized to the luminal and glandular epithelia in the endometrium, confirming earlier observations in the human (Smith et al. 1991; Miturski et al. 1998; Ejskjaer et al. 2005), pig (Wollenhaupt et al. 1997), goat (Tamada et al. 2000), bitch (Kida et al. 2010; Sağsöz et al. 2014) and cow (Sağsöz et al. 2012). In contrast to the findings obtained in the present study, ErbB1 was reported not to be expressed in the uterine epithelial cells in the mouse by Das et al. (1994) and in the human uterine glands by Wang et al. (1992). In accordance with microscopic findings, our immunohistochemical results, showed ErbB1/HER1 immunoreactivity in only some regions of the luminal epithelium on days 1 and 3 of the postpartum involution period and the absence of the reaction in the prismatic epithelium on postpartum day 5. These results were similar to previous reports in humans (Imai et al. 1995) that reported that ErbB1/HER1 is expressed at low levels during the early follicular phase. Furthermore, in the rat uterus, the histological findings and the immunoreactivity of ErbB1/HER1 in the entire luminal epithelium on postpartum days 10 and 15 as reported in the luteal phase of sexual cycle of other mammals (Smith et al. 1991; Miturski et al. 1998; Ejskjaer et al. 2005; Wollenhaupt et al. 1997; Tamada et al. 2000; Kida et al. 2010; Sağsöz et al. 2014; Sağsöz et al. 2012) demonstrate that the repair and remodelling processes of the luminal epithelium were already completed by day 10 postpartum and that the expression of ErbB1/HER1 in the epithelium varies with morphological changes in the luminal epithelium during the postpartum period.
ErbB1/HER1 has been reported tolocalize at the basal region of the luminal epithelial cells (Ejskjaer et al. 2005), the surface of the glandular epithelial cells in the human uterus (Smith et al. 1991), the apical and basal membranes of the luminal epithelium and only the apical membrane of the glandular epithelium in the bovine uterus (Sağsöz et al. 2012), whereas membrane, cytoplasmic and nuclear immunoreactivity has been determined in the bitch uterus (Sağsöz et al. 2014). In contrast to other mammalian species, the present study that in the rat, the uterine localization of ErbB1/HER1 was of a supranuclear punctate pattern in the endometrial luminal and glandular epithelial cells. ErbB1/HER1 is a prototypical receptor tyrosine kinase. The binding of ligands, such as EGF, to the extracellular portion of ErbB1/HER1 on the cell surface induces ErbB1/HER1 dimerization and tyrosine kinase activation. After receptor activation, ErbB1/HER1 is typically downregulated via an endocytic pathway that results in receptor degradation or recycling. Therefore, the endocytic pathway is the primary molecular mechanism that maintains the balance of EGFR (Haley and Gullick 2008). Activated ErbB1/HER1 is internalized into endosomes. Endosomal ErbB1/HER1 is translocated to the endoplasmic reticulum (ER) directly or indirectly via the Golgi. Subsequently, ErbB1 is retrotranslocated from the ER to the cytosol (Sorkin and Goh 2008). It has been reported that the Golgi apparatus is localized in the supranuclear region of the luminal and glandular epithelium in the rat uterus (Glasser et al. 1988). In view of these literature reports, although the subcellular localization of ErbB1/HER1 was not examined by electron microscopy in the present study, the observation of the ErbB1/HER1 immunoreactivity in a punctate pattern in the supranuclear region suggested that the Golgi body and the associated endosomal vesicles were ErbB1-positive. This finding supports the presence of endosomal ErbB1 signalling (Wang et al. 2002) in the rat endometrial epithelial cells. Because EGFR signalling affects various cellular processes such as proliferation, differentiation, survival, growth, and migration and because endosomal EGFR signalling promotes the activation of major signalling pathway such as ERK1/2 and Akt, leading to cell proliferation and cell survival (Wang et al. 2002), we propose that ErbB1 may act in an autocrine and/or paracrine manner to regulate the proliferation, differentiation and viability of endometrial epithelial cells during uterine involution.
The ErbB2 (HER2/Neu proto-oncogene) plays an important role in normal cell growth and differentiation in the uterus several mammals and ErbB2/HER2 expression in different uterine components varies with the phases of the sexual cycle (Wang et al. 1992; Miturski et al. 1998; Lim et al. 1997; Idris et al. 2001; Klonisch et al. 2001; Sağsöz et al. 2012; Sağsöz et al. 2014). In agreement with the reports available for the mouse (Lim et al. 1997), rabbit (Klonisch et al. 2001), human (Miturski et al. 1998; Ejskjaer et al. 2005), cat (Mısırlıoglu et al. 2006), cow (Sağsöz et al. 2012) and dog (Sağsöz et al. 2014), in the present study, it was ascertained that throughout the postpartum period, a moderate reactivity was observed in the cytoplasm and membrane of the luminal and glandular epithelial cells. The cytoplasmic reactivity in the luminal epithelium was observed to be weaker on postpartum days 10 and 15 compared with the other days. Lim et al. (1997) reported that ErbB2 may be a potential candidate receptor subtype for interaction with the EGF-related ligands in epithelial cell proliferation/differentiation during the preimplantation period (Lim et al. 1997). Based on this information and our immunohistochemical findings, we suggest that the ErbB2/HER2 receptor participates in the regulation of proliferation and differentiation of the endometrial epithelium in the rat uterus throughout the postpartum involution period.
The ErbB3/HER3 receptor is mainly expressed by normal tissues. The major difference between other ErbB receptors and the ErbB3 receptor, is that the latter possesses either very little or no tyrosine kinase activity. For this reason, homodimers of ErbB3 are inactive (Srinivasan et al. 1999). Studies in the uterus (Srinivasan et al. 1999; Ejskjær et al. 2005; Sağsöz et al. 2012; Sağsöz et al. 2014) showed that ErbB3/HER3 expression in the luminal and glandular epithelium did not vary with the different phases of the menstrual or oestrous cycle (Srinivasan et al. 1999; Ejskjær et al. 2005; Sağsöz et al. 2012; Sağsöz et al. 2014). Our immunohistochemical data showed that ErbB3/HER3 immunoreactivity was localized particularly in the apical and basal cytoplasm of the luminal and glandular epithelial cells, and in the nucleus in some cells, and this staining did not vary during the uterine involution period.
The ErbB4 protein is a member of the receptor tyrosine kinase family and weighs 180 kDa. Previous studies have discovered that the expression of ErbB4/HER4 in the cellular components of the uterus is different in several mammalian species including, human (Imai et al. 1995; Niikura et al. 1996; Srinivasan et al. 1999; Srinivasan et al. 1998; Möller et al. 2001; Ejskjaer et al. 2005), cow (Sağsöz et al. 2012) and bitch (Sağsöz et al. 2014), and shows cyclic variations depending upon the species. Although Ejskjaer et al. (2005) stated that ErbB4/HER4 is localized to the cytoplasm of luminal and glandular epithelial cells, Srinivasan et al. (1998) observed positive staining for erbB4/HER4 on the apical, lateral and basal membranes of epithelia. In the present study, it was observed that throughout the postpartum involution period, the luminal and glandular epithelia displayed a strong cytoplasmic, membranous and nuclear (nuclear membrane) distribution pattern for ErbB4/HER4, and this ErbB4/HER4 immunoreaction did not vary during the postpartum involution period. Recent studies showed that membranous ErbB1, ErbB2, ErbB3, and ErbB4 proteins can translocate to the nucleus in a variety of cancer cells (Lin et al. 2001; Offterdinger et al. 2002; Koumakpayi et al. 2006) and that the nuclear localization of ErbB acts as a transcriptional regulator, transmits signals, and is involved in multiple biological functions, including cell proliferation, tumour progression, DNA repair and replication, and chemo- and radio-resistance (Wang and Hung 2012). The ErbB3/HER3 and ErbB4/HER4 nuclear reactivity observed in the endometrial epithelial cells in the rat uterus during the postpartum involution period supports the opinion that this expression may be associated with the downstream signalling activities that regulate the proliferation, mobility and differentiation of cells during the involution process (Wang and Hung 2012).
EGF, a ligand that bind to the EGF receptor (ErbB1/HER1), is a mitogenic polypeptide growth hormone that is known to regulate the proliferation and differentiation of a variety of cells including uterine epithelial cells by paracrine and/or autocrine action (Shiraga et al. 2000). Several studies in the uterus of multiple mammals, including humans (Chegini et al. 1992; Imai et al. 1995; Möller et al. 2001), rats (Gardner et al. 1989), mice (Das et al. 1994), rhesus monkeys (Yue et al. 2000), baboons (Slowey et al. 1994), dogs (Kida et al. 2010; Sağsöz et al. 2014) and pigs (Wollenhaupt et al. 1997), have demonstrated that the localization and expression of EGF in the cellular component of the uterus are different among species and among the stages of the menstrual or sexual cycle. Previous studies in the uterus of many mammals including human (Imai et al. 1995; Chegini et al. 1992; Möller et al. 2001), baboon (Slowey et al. 1994), goat (Tamada et al. 2000), and bitch (Kida et al. 2010; Sağsöz et al. (2014), demonstrated that the luminal and glandular epithelial cells express EGF. However, the present study indicates that EGF immunoreactivity was weak in the cytoplasm of the luminal and glandular epithelium.
AREG is a heparin-binding molecule that binds ErbB1/HER1 and is expressed in various tissues but mainly in the reproductive and urinary systems (mammary glands, uterus/ovary, placenta, testis and prostate) (Stern 2003). In the reproductive system, AREG participates in a wide range of physiological processes, including blastocyst attachment and preparing the uterus for embryo implantation (Das et al. 1995; Lee et al. 2006). Investigations conducted in the uterus of the mouse, monkey, and pig and in humans (Das et al. 1995; Yue et al. 2000; Kim et al. 2003; Ejskjaer et al. 2005; Gui et al. 2008; Aghajanova et al. 2008) have shown that the expression of AREG in the uterus varies between species. Furthermore, the presence of AREG in the human endometrium is controversial: one group observed weak immunostaining in the cytoplasm and nuclei of luminal and glandular epithelial cells and low mRNA levels of AREG (Aghajanova et al. 2008); however, other researchers determined that AREG was located in the cytoplasm of the glandular epithelial cells (Gui et al. 2008). It has been reported that in the rhesus monkey (Yue et al. 2000) and bitch (Sağsöz et al. 2014), AREG is localized in the luminal and glandular epithelium. Similar to the reports for humans (Gui et al. 2008; Aghajanova et al. 2008) and the rhesus monkey (Yue et al. 2000) and bitch (Sağsöz et al. 2014), in the present study, it was observed that AREG was localized to the cytoplasm and nuclei of luminal and glandular epithelium. In agreement with the report from Aghajanova et al. (2008) for the human endometrium, AREG immunoreactivity was also observed on the apical surface of the luminal and glandular epithelial cells of the rat uterus.
Neuregulin 1 (NRG1) is one of four proteins in the neuregulin family that act on the EGFR family of receptors. NRG1 binds to the ErbB3 and ErbB4 receptors and mediates cell-cell interactions, and its multiple isoforms perform diverse functions such as inducing growth and differentiation of epithelial, glial, neuronal, and skeletal muscle cells (reviewed in Burden and Yarden 1997). The expression of NRG1 in the uterus has been investigated during the menstrual cycle in humans (Srinivasan et al. 1999) and during the oestrous cycle in the bitch (Sağsöz et al. 2014). The study by Srinivasan et al. (1999) confirmed that NRG1 is expressed by glandular epithelial cells at a higher level during the secretory stage, whereas Sağsöz et al. (2014) demonstrated that NRG1 expression is strong in luminal and glandular epithelium throughout the oestrus cycle. In contrast to humans (Srinivasan et al. 1999) and the bitch (Sağsöz et al. (2014), the results of our study reveal that cytoplasmic NRG1 immunoreactivity was weak in luminal and glandular epithelium throughout the postpartum involution period of the rat uterus. This finding support the information in the literature (Brown et al. 2004) that NRG-1 is implantation-specific gene and is required for the implantation of the blastocyst.
The rat uterus undergoes a rapid roughly 10-fold increase in wet weight during pregnancy over a period of 21 days and an even more rapid involution within 5–6 days post-partum (Afting and Elce 1978). A feature of particular interest in involution is the re-organization of the connective tissue framework of the endometrial stroma, which is a major component of the endometrium, with 83 % of its collagen resorbed in the first 3 days following parturition (Ryan and Woessner 1972). During postpartum uterine involution fibroblasts, along with smooth muscle cells and macrophages, work in concert with extracellular degradation and ingest enormous amounts of collagen over a brief period of time (Ryvnyak et al. 1999; Parakkal 1972).
Our microscopic findings demonstrated that on postpartum day 1, the endometrial stroma consisted of expanded hypocellular oedematous loose connective tissue with little discernible extracellular matrix (ECM), and following day 3 after birth, the endometrial fibroblast density within the lamina propria increased with the advancement of the postpartum involution process. Furthermore, we observed that on postpartum days 10 and 15, the endometrial fibroblasts showed two different locations in the endometrial stroma: subepithelial and deep stromal, and the amount of fibroblasts in the subepithelial stroma was more than in the deep stroma. These findings support the hypothesis that the fibroblast in the superficial stroma may play a role in the preparation of desidualization and that the fibroblasts in the deep stroma may be is associated with reconstruction of the endometrium in the post-partum period (Salgado et al. 2011).
It has been reported that in the rat and hamster, primary (solitary) ciliated fibroblasts are present in the endometrial stroma, and in these cells, the Golgi body is conspicuous in the periphery of the basal body situated adjacent to the nucleus (Tachi et al. 1969; Clark and Brinsfield 1973). More than 300 primary cilia have been identified using electron microscopy in a variety of embryonic and mature connective tissue cells (Poole et al. 1985). The function of primary cilia, such as those found in endometrial stromal cells of the uterus is unknown. However, Poole et al. (1985) proposed that the primary cilia in connective tissue cells could act as multifunctional, cellular cybernetic probes, thus receiving, transducing, and conducting a variety of extrinsic stimuli to the intracellular organelles responsible for inducing the appropriate homeostatic feedback response to changes in the extracellular microenvironment. Recently, Christensen et al. (2008) suggested that the primary cilium coordinates signalling pathways during cell cycle control and migration during development and tissue repair. As the present study was based on the use of light microscopy, the presence of ciliated fibroblasts was not able to be observed. However, endometrial stromal cells were identified as fibroblasts on the basis of their morphology, localization and vimentin-positive reactivity (data not shown) (Koumas et al. 2001).
Previous studies have shown that the expression and localization of EGFRs and ligands in the stromal cells of the endometrium are different from each other and vary according to the mammalian species and the sexual cycle. Our immunohistochemical results concerning the localization of the EGFRs and their ligands indicate that the localization and expression of these proteins in fibroblasts are different from each other. Furthermore, it was determined that although the number of immunopositive fibroblasts for each receptor and ligand increased with the advance of postpartum days and reached a maximum on postpartum days 10 and 15, the immunostaining intensity remained relatively stable throughout the postpartum period.
We found that the immunoreactivity of ErbB1/HER1 was located in the fibroblasts within the endometrial stroma in the form of a large granule in the supranuclear region. The presence of ErbB1/HER1 in the endometrial fibroblasts in the rat uterus is in agreement with previous reports in several mammalian species (Wang et al. 1992; Miturski et al. 1998; Möller et al. 2001; Ejskjaer et al. 2005), but the localization is different from these reports (Wang et al. 1992; Miturski et al. 1998; Möller et al. 2001; Ejskjaer et al. 2005), which observed the stromal cells displayed cytoplasmic ErbB1/HER1 imunoreactivity. In view of the literature reports cited above and on the basis of the knowledge that ErbB1 receptor activation induces proliferation and motility in fibroblasts (Yarden and Sliwkowski 2001), we hypothesized that the ErbB1/HER1 immunoreactivity observed in the endometrial fibroblasts could be localized to the Golgi body and that ErbB1/HER1 could be associated with the proliferation and motility of endometrial fibroblasts. However, to prove this hypothesis, detailed immnunoelectron microscopic research is required.
Research conducted in the uterus showed that the expression and localization of the ErbB1 ligands EGF and AREG in the stromal cells vary between species. In humans, Chegini et al. (1992) and Möller et al. (2001) showed that the endometrial stromal cells are the site of EGF expression. In the baboon uterus, Slowey et al. (1994) stated that EGF is only expressed in stromal cells surrounding the glands (periglandular stroma) during the follicular stage, whereas during the luteal stage, glandular epithelial and stromal cells produced positive immunoreactions for EGF. However, in mares, EGF was absent (Gerstenberg et al. 1999), and in goats (Tamada et al. 2000), expression was either weak or absent in stromal cells. In the bitch uterus, Sağsöz et al. (2014) demonstrated that EGF was localized in the endometrial stromal cells throughout the oestrus cycle. Furthermore, the presence of AREG in the human endometrium is controversial: one group found a few stromal cells in the endometrial stroma and leukocytes in the blood expressing AREG protein and mRNA, which decreased from the early proliferative to the early secretory phase (Ejskjaer et al. 2005), whereas a second group observed weak AREG immunostaining in the cytoplasm and nuclei of stromal cells and low mRNA levels of AREG, without cyclic variations (Aghajanova et al. 2008). In addition, it has been reported that in the bitch, AREG immunoreactivity is localized to the stromal cells and does not vary during the oestrous cycle (Sağsöz et al. 2014). Our immunohistochemical findings show that the expression and localization of the ErbB1 ligands EGF and AREG are different from that of ErbB1, although EGF is weakly expressed in the cytoplasm of fibroblasts, whereas AREG is localized at the nuclear membrane of endometrial fibroblasts. It is known that fibroblasts play a significant role in epithelial-mesenchymal interactions, secreting various growth factors and cytokines that have a direct effect on epithelial proliferation and differentiation and on the formation of extracellular matrix (Wong et al. 2007). AREG has been shown to induce fibroblast proliferation (Shoyab et al. 1988). Altogether, these data led us to hypothesize that the expression of AREG in the nuclear membrane of endometrial fibroblasts may stimulate stromal cell proliferation, differentiation and migration, supporting assumptions that AREG plays a key role in stromal restoration during uterus involution. Furthermore, although the absence of ErbB2/HER2 immunoreactivity was reported by Mısırlıoglu et al. (2006) in the stromal cells in the cat and by Wang et al. (1992) in the stromal cells of humans, the findings of this study demonstrate that during the postpartum involution period in the rat uterus, endometrial fibroblasts displayed positive cytoplasmic ErbB2/HER2 immunoreactivity. Taken together with the histological and histochemical findings that showed that the number of immunopositive fibroblasts increased with the advance of postpartum days and reached a maximum on postpartum days 10 and 15, this finding may indicate that ErbB2 is a potential candidate receptor subtype for fibroblast proliferation and preparation for decidualization during the postpartum involution period as reported during the implantation period (Lim et al. 1997). Previous investigations in humans (Srinivasan et al. 1999) and the cow (Sağsöz et al. 2012) and bitch (Sağsöz et al. 2014) showed that the stromal cells in the endometrium are positive for ErbB3. Our immunohistochemical data indicate that the staining pattern of ErbB3 in endometrial fibroblast was predominantly nuclear and cytoplasmic. In addition to its cytoplasmic and membrane localization, ErbB3 protein has been reported in cell nuclei and the nuclear localization of HER3, like that of EGFR, is suggested to function as a transcription factor in chromatin remodelling as well as DNA repair (Jiang et al. 2012). Based on this information, we suggest that the nuclear localization of ErbB3/HER3 in the endometrial fibroblasts may be associated with downstream signalling activities regulating the proliferation, mobility and differentiation of these cells during the involution process (Wang and Hung 2012).
Work by Srinivasan et al. (1999) reported that Erb4/HER4 is expressed at high levels on the membrane of stromal cells during the secretory stage of the menstrual cycle of human, whereas work by Chobotova et al. (2005) showed Erb4/HER4 localized mainly to the stroma during the proliferative phase and to the epithelium and stroma during the secretory phase. Although previous research in cows (Sağsöz et al. 2012) reported that the staining intensity of erbB4/HER4 in the stromal cells was weak, another study in the bitch (Sağsöz et al. 2014) stated that the stromal cells were more weakly stained in anestrus than proestrus, oestrus or diestrus. In the present study, throughout the postpartum involution period, the endometrial fibroblasts displayed moderate cytoplasmic ErbB4/HER4 immunoreactivity.
Investigations conducted in the uterus of humans (Srinivasan et al. 1999) and the bitch (Sağsöz et al. 2014) showed that the expression of the ErbB3 and ErbB4 ligand NRG1 in the stromal cells is weak compared with the epithelial component of the uterus. Similar to these reports our findings indicate that cytoplasmic NRG1 immunoreactivity, like that of ErbB3 and ErbB4, was weak in endometrial fibroblasts.
It has long been appreciated that endometrial macrophages (in the rat, rabbit, and mouse) play a role in the reduction of stromal volume. These phagocytes appear in the stroma during the early postpartum period and phagocytose the solubilized denatured collagen fragments degraded by extracellular proteases (Padycula1976). Additionally, recent studies demonstrated that macrophages express ErbB2, ErbB3 and ErbB4 and neuregulin-1 and that these receptors and ligands enhance macrophage motility (Calvo et al. 2010). Lamb et al. (Lamb et al. 2004) found that EGF mediates monocyte chemotaxis and macrophage proliferation. Based on this information in the literature and our data showing the presence of ErbB2, ErbB3, ErbB4, EGF, AREG and NRG1 in macrophages, we suggest that EGFR signalling may play a role in the migration of macrophages during uterine involution. Uterine involution results from a decrease in myometrial smooth muscle cell size, but the number of myometrial cells does not decrease. This decrease in size is the result of ischemia, autolysis, and phagocytosis (Afting and Elce 1978; Simpson and Creehan 2008). Our data are limited to a histological study; as a result, we could not determine the degree of ischemia, autolysis and phagocytosis of myometrial cells during the involution of the uterus. However, we observed that following day 3 after birth, myometrial thickness decreased with the advance of postpartum days and reached a minimum on postpartum days 10 and 15.
The ErbB family of receptors and ligands has been demonstrated to play an important role in growth regulation and intracellular signalling in a wide variety of cell types including myometrial smooth muscle cells. These studies revealed that the expression of ErbB family of receptors and ligands differed among species and stages of the menstrual or sexual cycle. ErbB1/HER1/EGFR mRNA expression has been identified in the smooth muscle cells of the normal myometrium (Yeh et al. 1991). In humans, no significant difference in the concentrations of ErbB1/HER1/EGFR in the myometrium during the menstrual cycle was reported (Konopka et al. 1998). Tamada et al. (2005) reported that in the bitch, the ErbB1/HER1 immunoreactivity was weak in the myometrium, whereas Sağsöz et al. (2014) reported that at proestrus and diestrus, the expression of ErbB1 was strong. ErbB1/HER1 immunoreactivity was reported to be weak in 50-day-old rats that had recently reached puberty (Brown and Lamartiniere 2000). The findings obtained in the present study demonstrated that ErbB1 immunoreactivity was weak in the myometrium of the rat uterus throughout the postpartum involution period, and similar to the human uterus during the menstrual cycle (Konopka et al. 1998), no significant alterations were observed during the involution period. Previous studies in the cow (Sağsöz et al. 2012) and the bitch (Sağsöz et al. 2014) have shown ErbB2/HER2-positive reactivity in myometrial smooth muscle cells, whereas feline uterine myometrial cells did not produce any immunoreaction (Mısırlıoglu et al. 2006). Furthermore, in the bitch, it has been reported that the immunoreactivity for ErbB2 in the myometrial smooth muscle cells during oestrus is significantly different than that during diestrus and anestrus (Sağsöz et al. 2014). A primary function of ErbB2/HER2 is suppressing apoptosis to enhance cell survival, giving rise to uncontrolled proliferation and tumour growth. Maintenance of ErbB2/HER2 expression is also required for ErbB2/HER2-mediated suppression of apoptosis (Carpenter and Lo 2013), and ErbB2 is required for muscle spindle and myoblast cell survival (Andrechek et al. 2002). It is known that postpartum uterine involution is characterized by the expression of genes associated with apoptosis, wound repair, and tissue regeneration. This allows the uterus to resume its normal, nonpregnant receptive conditions (Petraglia et al. 2007). Shynlova et al. (2006) reported that the major antiapoptotic protein Bcl-2 localized in the cytoplasm of rat myometrial cells, and that Bcl-2 protein expression was abundant in the nonpregnant and early pregnant myometrium (up to gestational day 12), then decreased dramatically during late gestation (17-fold decrease at gestational days 21 and 22) and returned to a high nonpregnant level by postpartum day 4. Bcl-2 protein has been shown to prevent the activation of the caspase cascade (Monney et al. 1996), and recently, in the myometrium, it has been stated that under normal circumstances, caspase cascade activation does not occur at term (Shynlova et al. 2006). Furthermore, ErbB2/HER2 gene amplification has also been reported to correlate with the expression of the apoptosis-suppressing genes Bcl-2 and Bcl-xL in breast cancer (Siziopikou and Khan 2005). The ErbB2 receptor also has important roles in mitogenesis and the differentiation of smooth muscle cells (Yamanaka et al. 2001).
The precise roles of ErbB2 in myometrial smooth muscle physiology have not been previously elucidated. However, collectively, the information in the literature combined with our own results showing the strong cytoplasmic expression of ErbB2/HER2 in the myometrial cells of uterus during postpartum involution period led us to hypothesize that erbB2/HER2 may play a role similar to that of Bcl-2 by preventing the development of true apoptosis in myometrial tissues and thus, ErbB2/HER2 may regulate mitogenesis and the differentiation of myometrial smooth muscle cells (Yamanaka et al. 2001).
It has been reported that in the bitch (Sağsöz et al. 2014), ErbB3/HER3 immunoreactivity in the myometrial smooth muscle cells was of a moderate intensity at anoestrus and weak during the other phases of the oestrous cycle, whereas the ErbB4/HER4 and NRG immunoreactivity was weak, and the AREG and EGF immunoreactivity was moderate throughout the sexual cycle. In the mouse, it has been reported that there was little detectable apoptosis in the myometrial smooth muscle cells of wild-type 24–48 h postpartum uteri and ErbB4 expression was observed throughout the smooth muscle cells of the myometrium, suggesting that ErbB4 may play an important role in the regulation of physiological tissue remodelling (Yu et al. 2002). Furthermore, Tamada et al. (2000) reported that in the goat uterus, the myometrial smooth muscle cells produced a weak EGF reaction, whereas Brown and Lamartiniere (2000) reported to have observed moderate EGF reactivity in the rat uterus. Harrison-Woolrych et al. (1994) stated that in the myometrium of the human uterus, the levels of EGF mRNA did not differ between the proliferative and secretory phase of the cycle.
The results of the present study demonstrated that in the myometrium, the immunoreactivity of ErbB3/HER3, EGF, AREG and NRG1 was weak and was not altered during the involution period. Furthermore, as reported for the postpartum mouse uterus (Yu et al. 2002), it was ascertained that in the postpartum rat uterus, the ErbB4 immunoreactivity in the myometrial smooth muscle cells was of a moderate intensity. This finding supports the hypothesis that the ErbB4/HER4 receptor may be significantly involved in the remodelling of the myometrium during the involution period (Yu et al. 2002).
Conclusion
In conclusion, the current study demonstrate the presence of ErbB/HER receptors and their ligands (EGF, NRG and AREG) in the uterine luminal and glandular epithelium, stromal cells, and myometrial compartments during postpartum uterine involution in the rat and showed that the expression levels of these proteins are different among tissue compartments of the uterus. However, although the changes in the expression levels of epidermal growth system members are generally not as dramatic, our results indicate that the expression of ErbB receptors and their ligands varied with structural changes in the uterus on different days of involution. Our data were limited to a semi-quantitative immunohistochemical analysis; therefore, we could not determine the exact function of the EGF system in the uterine involution process. However, we suggest that the ErbB/HER receptors and their ligands play a major role in the development of various physiologic changes associated with uterine involution.
References
Afting E-G, Elce JS (1978) DNA in the rat uterus myometrium during pregnancy and postpartum involution: Measurement of DNA in small pieces of mammalian tissue. Anal Biochem 86:90–99
Aghajanova L, Bjuresten K, Altmae S, Landgren BM, Stavreus-Evers A (2008) HB-EGF but not amphiregulin or their receptors HER1 and HER4 is altered in endometrium of women with unexplained infertility. Reprod Sci 15:484–492
Aker ON (1954) Laboratuvar El Kitabı, Hususi Boyama Teknikleri. Örnek Matbaası, Ankara. S:138–139
Alan E, Liman N (2012) Immunohistochemical localization of beta defensins in the endometrium of rat uterus during the postpartum involution period. Vet Res Commun 36:173–185
Andrechek ER, Hardy WR, Girgis-Gabardo AA et al (2002) ErbB2 is required for muscle spindle and myoblast cell survival. Mol Cell Biol 22:4714–4722
Bazley LA, Gullick WJ (2005) The epidermal growth factor receptor family. Endocr Relat Cancer 12:17–27
Blackburn ST (2007) Maternal, fetal, and neonatal physiology: a clinical perspective. Saunders Elseiver, St. Louis Missouri, p 153
Boomsma RA, Mavrogianis PA, Verhage HG (1997) Immunohistochemical localization of TGF-α, EGF and EGFR in the cat endometrium and placenta. Histochem J 29:495–504
Brown NM, Lamartiniere CA (2000) Genistein regulation of transforming growth factor-a, epidermal growth factor (EGF), and EGF Receptor expression in the rat uterus and vagina. Cell Growth Differ 11:255–260
Brown N, Deb K, Paria BC, Das SK, Reese J (2004) Embryo-uterine interactions via the neuregulin family of growth factors during implantation in the mouse. Biol Reprod 71:2003–2011
Burden S, Yarden Y (1997) Neuregulins and their receptors: a versatile signaling module in organogenesis and oncogenesis. Neuron 18:847–855
Calvo M, Zhu N, Tsantoulas C, Ma Z, Grist J, Loeb JA, Bennett DL (2010) Neuregulin–erbB signaling promotes microglial proliferation and chemotaxis contributing to microgliosis and pain after peripheral nerve injury. J Neurosci 30:5437–5450
Carpenter RL, Lo H-W (2013) Regulaton of apoptosis by HER2 in breast cancer. J Carcinog Mutagen S7:003
Chegini N, Rossi M, Masterson B (1992) Platelet-derived growth factor (PDGF), epidermal growth factor (EGF), and EGF and PDGF beta-receptors in human endometrial tissue: localization and in vitroaction. Endocrinology 130:2373–2385
Chobotova K, Karpovich N, Carver J et al (2005) Heparin-binding epidermal growth factor and its receptors mediate decidualization and potentiate survival of human endometrial stromal cells. J Clin Endocrinol Metab 90:913–919
Christensen ST, Pedersen SF, Satir P, Veland IR, Scneider L (2008) The primary cilium coordinates signaling pathways in cell cycle control and migration during development and tissue repair. Curr Top Dev Biol 85:261–301
Clark MV, Brinsfield TH (1973) Ciliated stromal cells in the hamster uterus. Biol Reprod 8:100–102
Crossman G (1937) A modification of Mallory’s connective tissue stain with a discussion of the principles involved. Anat Rec 69:33–38
Das SK, Tsukamura H, Paria BC, Andrews GK, Dey SK (1994) Differantial expression of epidermal growth factor receptor (EGF-R) gene and regulation of EGF-R bioactivity by progestrone and estrogen in the adult mouse uterus. Endocrinology 134:971–981
Das SK, Chakraborty I, Paria BC, Wang XN, Plowman G, Dey SK (1995) Amphiregulin is an implantation-specific and progesterone-regulated gene in the mouse uterus. Mol Endocrinol 9:691–705
Das SK, Das N, Wang J et al (1997) Expression of betacellulin and epiregulin genes in the mouse uterus temporally by the blastocyst solely at the site of its apposition is coincident with the “window” of implantation. Dev Biol 190:178–190
DiAugustine RP, Petrusz P, Bell GL et al (1988) Influence of estrogens on mouse uterine epidermal growth factor precursor protein and messenger ribonucleic acid. Endocrinology 122:2355–2363
Ejskjaer K, Sorensen BS, Poulsen SS, Mogensen O, Forman A, Nexo E (2005) Expression of the epidermal growth factor system in human endometrium during the menstrual cycle. Mol Hum Reprod 11:543–551
Esslemont RJ, Kossaibati MA (2000) The use of databases to manage fertility. Anim Reprod Sci 60–61:725–741
Falls DL (2003) Neuregulins: functions, forms, and signaling strategies. Exp Cell Res 284:14–30
Gardner RM, Lingham RB, Stancel GM (1987) Contractions of the isolated uterus stimulated by epidermal growth factor. FASEB J 1:224–228
Gardner RM, Verner G, Kirkland JL, Stancel GM (1989) Regulation of uterine epidermal growth factor (EGF) receptors by estrogen inthe mature rat and during the estrous cycle. J Steroid Biochem 32:339–343
Gerstenberg C, Allen W, Stewart F (1999) Factors controlling epidermal growth factor (EGF) gene expression in the endometrium of the mare. Mol Reprod Dev 53:255–265
Gharib-Hamrouche N, Chene N, Martal J (1995) Comparative expression of TGF-α and EGF genes in the ovine conceptus and uterine endometrium in the peri-implantation period. Reprod Nutr Dev 35:291–303
Glasser SR, Julian J, Decker GL, Tang J-P, Carson DD (1988) Development of morphological and functional polarity in primary cultures of immature rat uterine epithelial cells. J Cell Biol 107:2409–2423
Gui Y, Zhang J, Liang W, Cai Z (2008) Expression of amphiregulin in human endometrium during the menstrual cycle. Beijing Da Xue Xue Bao 40:241–244
Haley JD, Gullick WJ (2008) EGFR Signaling Networks in Cancer Therapy. Humana Press, Springer Science + Business Media, LLC, New York, p 193
Harrison-Woolrych ML, Charnock-Jones DS, Smith SK (1994) Quantification of messenger ribonucleic acid for epidermal growth factor in human myometrium and leiomyomata using reverse transcriptase polymerase chain reaction. J Clin Endocrinol Metab 78:1179–1184
Huet-Hudson YM, Chakraborty C, De SK, Suzuki Y, Anderws GK, Dey SK (1990) Estrogen regulates the synthesis of epidermal growth factor in Mouse uterine epithelial cells. Mol Endocrinol 4:510–523
Idris N, Carothers Carraway CA, Carraway KL (2001) Differential localization of erbB2 in different tissues of the rat female reproductive tract: implications for the use of specific antibodies for erbB2 analysis. J Cell Physiol 189:162–170
Imai T, Kurachi H, Adachi K et al (1995) Changes in epidermal growth factor receptor and the levels of its ligands during menstrual cycle in human endometrium. Biol Reprod 52:928–938
Jiang N, Saba NF, Chen ZG (2012) Advances in targeting HER3 as an anticancer therapy. Chemother Res Pract 2012:817304
Kida K, Maezono Y, Kawate N, Inaba T, Hatoya S, Tamada H (2010) Epidermal growth factor, transforming growth factor-α, and epidermal growth factor receptor expression and localization in the canine endometrium during the estrous cycle and in bitches with pyometra. Theriogenology 73:36–47
Kim GY, Besner GE, Steffen CL et al (1995) Purification of heparin-binding EGF-like growth factor from pig uterine luminal flushings, and its production by endometrial tissues. Biol Reprod 52:561–571
Kim JG, Vallet JL, Christenson RK (2003) Molecular cloning and endometrial expression of porcine amphiregulin. Mol Reprod Dev 65:366–372
Klonisch T, Wolf P, Hombach-Klonisch S et al (2001) Epidermal growth factor-like ligands and erbB genes in the peri-implantation rabbit uterus and blastocyst. Biol Reprod 64:1835–1844
Komárek V (2000) Snopsis of the organ anatomy. In: Krinke GJ (ed) The laboratory rat. Academic, San Diego, p 315
Konopka B, Skasko E, Kluska A et al (1998) Changes in the concentrations of receptors of insulin-like growth factor-I, epithelial growth factor, oestrogens and progestagens in adenomyosis foci, endometrium and myometrium of women during menstrual cycle. Eur J Gynaecol Oncol 19:93–97
Koumakpayi IH, Diallo JS, Le Page C et al (2006) Expression and nuclear localization of ErbB3 in prostate cancer. Clin Cancer Res 12:2730–2737
Koumas L, King AE, Critchley HOD, Kelly RW, Phipps RP (2001) Fibroblast heterogeneity: existence of functionally distinct Thy 1+ and Thy 1− human female reproductive tract fibroblasts. Am J Pathol 159:925–935
Lamb DJ, Modjtahedi H, Plant NJ, Ferns G (2004) EGF mediates monocyte chemotaxis and macrophage proliferation and EGF receptor is expressed in atherosclerotic plaques. Atherosclerosis 176:21–26
Lee DS, Ueta YY, Xuan X et al (2005) Expression patterns of the implantation-associated genes in the uterus during the estrous cycle in mice. J Reprod Dev 51:787–798
Lee D-S, Yanagimoto Ueta Y, Suzuki H (2006) Expression of amphiregulin during the pre- and post-implantation period in the mouse reproduction tract. J Reprod Dev 52:781–787
Lennard SN, Gerstenberg C, Allen WR, Stewart E (1998) Expression of epidermal growth factor and its receptor in equine placental tissues. J Reprod Fertil 112:49–57
Lim H, Dey SK, Das SK (1997) Differential expression of the erbB2 gene in the periimplantation mouse uterus: potential mediator of signaling by epidermal growth factor-like growth factors. Endocrinology 138:1328–1337
Lim H, Das N, Dey SK (1998) ErbB genes in the mouse uterus: cell-specific signaling by epidermal growth factor (EGF) family of growth factors during implantation. Dev Biol 204:97–110
Liman N, Alan E, Küçük Bayram G, Gürbulak K (2013) Expression of survivin, Bcl-2 and bax proteins in the domestic Cat (Felis catus) endometrium during the oestrus cycle. Reprod Domest Anim 48:33–45
Lin SY, Makino K, Xia W et al (2001) Nuclear localization of EGF receptor and its potential new role as a transcription factor. Nat Cell Biol 3:802–808
Mısırlıoglu D, Nak D, Sevimli A et al (2006) Steroid receptor expression and HER-2/neu (c-erbB-2) oncoprotein in the uterus of cats with cystic endometrial hyperplasia–pyometra complex. J Vet Med A 53:225–229
Miturski R, Semczuk A, Jacowicki JA (1998) C-erbB-2 expression in human proliferative and hyperplastic endometrium. Int J Gynecol Obstet 61:73–74
Möller B, Rasmussen C, Lindblom B, Olovsson M (2001) Expression ofthe angiogenic growth factors VEGF, FGF-2, EGF and their receptors in normal human endometrium during the menstrual cycle. Mol Hum Reprod 7:65–72
Monney L, Otter I, Olivier R et al (1996) Bcl-2 overexpression blocks activation of the death protease CPP32/Yama/apopain. Biochem Biophys Res Commun 221:340–345
Mukku VR, Stancel GM (1985) Receptors for epidermal growth factor in the rat uterus. Endocrinology 117:149–154
Nelson KG, Takahashi T, Lee DC et al (1992) Transforming growth factor-α is a potential mediator of estrogen actionin the mouse uterus. Endocrinology 131:1657–1664
Niikura H, Sasano H, Kaga K, Sato S, Yajima A (1996) Expression of epidermal growth factor family proteins and epidermal growth factor receptor in human endometrium. Hum Pathol 27:282–289
Offterdinger M, Schofer C, Weipoltshammer K, Grunt TW (2002) c-erbB-3: a nuclear protein in mammary epithelial cells. J Cell Biol 157:929–939
Onagbesan OM, Gullick W, Woolveridge I, Peddie MJ (1994) Immunohistochemical localization of epidermal growth factor receptors, epidermal-growth-factor-like and transforming-growth-factor-alpha-like peptides in chicken ovarian follicles. J Reprod Fertil 102:147–153
Padycula HA (1976) Cellular mechanisms involved in cyclic stromal renewal of the uterus. III. Cells of the immune response. Anat Rec 184:49–72
Parakkal PF (1972) Macrophages: the time course and sequence of their distribution in the postpartum uterus. J Ultrastruct Res 40:284–291
Petraglia F, Strauss JF, Weiss G, Gabbe SG (2007) Preterm birth: mechanisms, mediators, prediction, prevention & interventions, 1st edn. Informa Healthcare, UK, pp 16–17
Poole CA, Flint MH, Beaumont BW (1985) Analysis of the morphology and function of primary cilia in connective tissues: a cellular cybernetic probe? Cell Motil 5:175–193
Reese J, Brown N, Das SK, Dey SK (1998) Expression of neu differantation factor during the periimplantation period in the mouse uterus. Biol Reprod 58:719–727
Ryan JN, Woessner JF (1972) Oestradiol inhibits collagen breakdown in the involuting rat uterus. Biochem J 127:705–713
Ryvnyak VV, Gudumak VS, Rybakova MA, Grumeza OF, Pelin AV (1999) Extra-and intracellular collagen resorption by smooth muscle cells in postpartum uterine involution. Bull Exp Biol Med 127:96–98
Sağsöz H, Ketani MA (2010) The role of estrogen receptors, erbB receptors, vascular endothelial growth factor and its receptors, and vascular endothelial growth inhibitor in the development of the rat mammary gland. Growth Factors 28:379–393
Sağsöz H, Ketani MA, Saruhan BG (2012) Expression of the erbB/HER receptor family in the bovine uterus during the sexual cycle and the relation of this family to serum sex steroids. Biotech Histochem 87:105–116
Sağsöz H, Liman N, Güney Saruhan B, Küçükaslan I (2014) The expression of epidermal growth factor receptors and their ligands (epidermal growth factor, neuregulin, amphiregulin) in the bitch uterus during the estrus cyle. Anim Reprod Sci 147:161–179. doi:10.1016/j.anireprosci/2014.04.005
Salamonsen LA (2003) Tissue injury and repair in the female human reproductive tract. Reproduction 125:301–311
Salgado RM, Favaro RR, Zorn TMT (2011) Modulation of small leucine-rich proteoglycans (SLRPs) expression in the mouse uterus by estradiol and progesterone. Reprod Biol Endocrinol 9:22
Schneider MR, Wolf E (2008) The epidermal growth factor receptor and its ligands in female reproduction: insights from rodent models. Cytokine Growth Factor Rev 19:173–181
Shiraga M, Komatsu N, Teshigawara K et al (2000) Epidermal growth factor stimulates proliferation of mouse uterine epithelial cells in primary culture. Zool Sci 17:661–666
Shoyab M, McDonald VL, Bradley JG, Todaro GJ (1988) Amphiregulin: a bifunctional growth-modulating glycoprotein produced by the phorbol 12-myristate 13-acetate-treated human breast adenocarcinoma cell line MCF-7. Proc Natl Acad Sci U S A 85:6528–6532
Shynlova O, Oldenhof A, Dorogin A et al (2006) Myometrial apoptosis: activation of the caspase cascade in the pregnant rat myometrium at midgestation. Biol Reprod 74:839–849
Simpson KR, Creehan PA (2008) Perinatal nursing. Lippincott Williams & Wilkins, Philadelphia, p 485
Siziopikou KP, Khan S (2005) Correlation of HER2 gene amplification with expression of the apoptosis-suppressing genes bcl-2 and bcl-x-L in ductal carcinoma in situ of the breast. Appl Immunohistochem Mol Morphol 13:14–18
Slowey MJ, Verhage HG, Fazleabas AT (1994) Epidermal growth factor, transforming growth factor-α, and epidermal growth factor receptor localization in the baboon (Papio anubis) uterus during the menstrual cycle and early pregnancy. J Soc Gynecol Investig 1:277–284
Smith K, Lejeune S, Harris AH, Rees MCP (1991) Epidermal growth factor receptor in human uterine tissues. Hum Reprod 6:619–622
Sorkin A, Goh LK (2008) Endocytosis and intracellular trafficking of ErbBs. Exp Cell Res 314:3093–3106
Srinivasan R, Poulsom R, Hurst HC, Gullick WJ (1998) Expression of the c-erbB-4/HER4 protein and mRNA in normal human fetal and adult tissues and in a survey of nine solid tumour types. J Pathol 185:236–245
Srinivasan R, Benton E, McCormick F, Thomas H, Gullick WJ (1999) Expresssion of the c-erbB3/HER-3 and c-erbB4/HER-4 growth factor receptors and their ligands, neuregulin-1α, neuregulin-1β, and betacellulin, in normal endometrium and endometrial cancer. Clin Cancer Res 5:2877–2883
Stancel GM, Gardner RM, Kirkland JL et al (1987) Interactions between estrogen and EGF in uterine growth and function. Adv Exp Med Biol 230:99–118
Stern DF (2003) ErbBs in mammary development. Exp Cell Res 284:89–98
Tachi S, Tachi C, Linder HR (1969) Cilia-bearing stromal cells in the rat uterus. J Anat 104:295–308
Tamada H, Yoh C, Inaba T, Takano H, Kawate N, Sawada T (2000) Epidermal growth factor (EGF) in the goat uterus: immunohistochemical localization of EGF and EGF receptor and effectof EGF on uterine activity in vivo. Therigenology 54:159–169
Tamada H, Tsubutani D, Kawate N et al (2002) Detection of transforming growth factor-α and epidermal growth factor receptor mRNA and immunohistochemical localization of their proteins in the ovine uterus during the early implantation period. Histochem J 34:383–390
Tamada H, Tominaga M, Kida K et al (2005) Detection of transforming growth factor-a andepidermal growth factor receptor mRNA and immunohistochemical localization of the corresponding proteins in the canine uterus duringthe estrous cycle. Histol Histopathol 20:817–824
Tsark EC, Adamson ED, Withers GE, Wiley LM (1997) Expression and function of amphiregulin during murine preimplantation development. Mol Reprod Dev 47:271–283
Wang YN, Hung MC (2012) Nuclear functions and subcellular trafficking mechanisms of the epidermal growth factor receptor family. Cell Biosci 2:13
Wang D, Fujii S, Konishi I, Nanbu Y, Iwai T, Nonogaki H (1992) Expression of c-erbB2 protein and epidermal growth factor receptor in normal tissues of the female genital tract and in tha placenta. Virchows Arch A Pathol Anat Histopathol 420:385–393
Wang Y, Pennock S, Chen SX, Wang Z (2002) Endosomal signaling of epidermal growth factor receptor stimulates signal transduction pathways leading to cell survival. Mol Cell Biol 22:7279–7290
Warbrick JG (1955) Postpartum changes in the uterus of rat. J Embryol Exp Morphol 3:256–264
Werb Z (1990) Expression of EGF and TGF-α genes in early mammalian development. Mol Reprod Dev 27:10–15
Wollenhaupt K, Tiemann U, Einspanier R, Schneider F, Kanitz W, Brüssow K-P (1997) Characterization of the epidermal growth factor receptor in pig oviduct and endometrium. J Reprod Fertil 111:173–181
Wollenhaupt K, Welter H, Einspanier R, Manabe N, Brüssow K-P (2004) Expression of epidermal growth factor receptor (EGF-R), vascular endothelial growth factor receptor (VEGF-R) and fibroblast growth factor receptor (FGF-R) systems in porcine oviduct and endometrium during the time of implantation. J Reprod Dev 50:269–278
Wong T, McGrath JA, Navsaria H (2007) The role of fibroblasts in tissue engineering and regeneration. Br J Dermatol 156:1149–1155
Yamanaka Y, Hayashi K, Komurasaki T, Morimoto S, Ogihara T, Sobue K (2001) EGF family ligand-dependent phenotypic modulation of smooth muscle cells through EGF receptor. Biochem Biophys Res Commun 281:373–377
Yarden Y, Sliwkowski MX (2001) Untangling the ErbB signalling network. Nat Rev Mol Cell Biol 2:127–137
Yeh J, Rein M, Nowak R (1991) Presence of messenger ribonucleic acid for epidermal growth factor (EGF) and EGF receptor demonstrable in monolayer cell cultures of myometria and leiomyomata. Fertil Steril 56:997–1000
Yu W-H, Woessner JF, McNeish JD, Starnenkovic I (2002) CD44 anchors the assembly of matrilysin/MMP-7 with heparin-binding epidermal growth factor precursor and ErbB4 and regulates female reproductive organ remodeling. Genes Dev 16:307–323
Yue Z-P, Yang Z-M, Li S-J, Wang H-B, Haroer MJK (2000) Epidermal growth factor family in rhesus monkey uterus during the menstrual cycle and early pregnancy. Mol Reprod Dev 55:164–174
Zhang Z, Krause M, Davis DL (1992) Epidermal growth factor receptors in porcine endometrium: binding characteristics and the regulation of prostaglandin E and F2 alpha production. Biol Reprod 46:932–936
Acknowledgments
This study was financially supported by Scientific Research Council of Erciyes University (Project No: TSA-12-3865).
Conflict of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Alan, E., Liman, N. & Sağsöz, H. The profile of the epidermal growth factor system in rat endometrium during postpartum involution period. Vet Res Commun 39, 115–135 (2015). https://doi.org/10.1007/s11259-015-9633-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11259-015-9633-6