Abstract
Purpose
Currently, there is a lack of research comparing tadalafil treatment protocols recommended during low-intensity shock wave therapy (LI-SWT) for patients with erectile dysfunction (ED) who are unresponsive to phosphodiesterase type 5 inhibitors (PDE5i). The objective of this study is to compare the efficacy of only LI-SWT versus LI-SWT plus 5 mg tadalafil daily versus LI-SWT plus 20 mg tadalafil alternate-day in PDE5i -resistant ED.
Materıals and methods
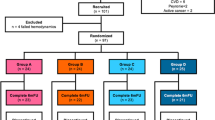
In this study, a cohort of 105 patients with PDE5i-resistant ED was recruited and divided into three groups labeled as A (only LI-SWT), B (LI-SWT plus 5 mg tadalafil daily), and C (LI-SWT plus 20 mg tadalafil alternate-day), comprising 27, 42, and 36 patients, respectively. The patients' International Index of Erectile Function-5 (IIEF-5) scores and the Erection Hardness Score (EHS) were evaluated at the baseline, three months and six months following the treatment.
Results
After three months post-treatment, the IIEF-5 scores in group A, B, and C increased by 4.1 ± 0.6, 7.3 ± 0.6, and 8.2 ± 0.6, respectively. These improvements were maintained at six months with IIEF-5 scores increasing by 3.7 ± 0.6, 7.3 ± 0.6, and 8.5 ± 0.7 in groups A, B, and C, respectively. At 3 and 6 months post-treatment, groups B and C showed significant improvement in IIEF-5 scores and EHS values compared to group A (p < 0.001). The rate of patients with EHS ≥ 3 and IIEF-5 ≥ 17 was significantly higher in groups B and C compared to group A, while there was no significantly different between groups B and C.
Conclusıon
In patients with PDE5i-resistant ED, PDE5i combined with LI-SWT is superior to LI-SWT monotherapy. The statistical analysis failed to demonstrate any difference between two distinct tadalafil regimens when administered with LI-SWT treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Phosphodiesterase-5 inhibitors (PDE5is) are commonly used drugs for the treatment of erectile dysfunction (ED), however, 30% of patients may not respond to these drugs and develop resistant ED [1]. Resistant ED refers to the failure of PDE5is to produce an adequate response in these patients, leading to a persistent inability to achieve or maintain an erection. The underlying causes of resistant ED can be complex and multifactorial, including psychological factors, comorbid conditions, and drug interactions. Management of resistant ED may involve a combination of interventions, including alternative ED treatments, and further evaluation for underlying medical conditions [2].
ED can lead to decreased self-esteem, decreased sexual desire, and relationship difficulties [3]. Identifying an effective treatment for PDE5is-resistant ED is crucial as it can significantly impact a person's quality of life and relationship satisfaction. Therefore, for individuals who do not respond to traditional PDE5is, the search for an effective treatment becomes even more critical. Effective treatment of ED can help to restore sexual function, improve psychological well-being, and enhance the overall quality of life [4]. Furthermore, early identification and management of resistant ED can prevent the development of more severe forms of ED and associated complications, such as decreased libido, sexual dissatisfaction, and relationship stress [5].
Low-intensity shockwave therapy (LI-SWT) can be a promising alternative for treating PDE5is-resistant ED [6, 7]. The effectiveness of LI-SWT alone and in combination with tadalafil, a PDE5i, has been evaluated in several studies [8]. Despite this, information about the optimal dose of tadalafil in combination with LI-SWT is limited. Therefore, further research is necessary to fully understand the optimal combination of LI-SWT and tadalafil for treating ED. For this purpose, we compared the efficacy of three different treatment options in patients with PDE5is-resistant ED.
Methods
The data for this retrospective cohort study were obtained from medical records of patients who were treated for ED between January 1, 2018, and December 31, 2022. The study received approval from the Ankara University Ethics Board under protocol number [i06-397-23]. The study included male patients aged between 45 and 65 years, who were diagnosed with PDE5is-resistant ED. PDE5is-resistant ED had defined as a failure to achieve an erection sufficient for intercourse with at least 3 different PDE5is at maximal recommended doses for at least 6 months. These patients received one of the following treatments: either only LI-SWT, LI-SWT combined with 5 mg daily tadalafil, or LI-SWT combined with 20 mg tadalafil administered every alternate day. The inclusion criteria further required that the patient's medical records contained complete data on demographics, medical history, medications, and outcome measures. Additionally, it was essential for the patients in the tadalafil groups to have received regular PDE5i therapy for at least 6 months.
Patients were excluded from the study if they had a bleeding disorder, were receiving anticoagulant or antiplatelet therapy, had testosterone levels below 300 ng/dL despite receiving replacement therapy, had previously undergone prostate cancer therapy or pelvic surgery or had neurologic disease or had any type of penile deformity or skin disease.
Baseline questionnaire responses were obtained while patients were receiving PDE5i treatment before LI-SWT treatment. All patients without contraindications for the use of PDE5i were provided with the option of PDE5i treatment in combination with LI-SWT. The choice of PDE5i, either at a daily dose of 5 mg or at a dose of 20 mg every alternate day, was determined based on individual patient preference.
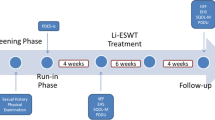
LI-ESWT was administered to all patients at six locations of the corpora at a frequency of two sessions per week for a period of three consecutive weeks. After selecting eligible patients, they were grouped according to the treatment they received: LI-SWT only (group A), LI-SWT plus daily 5 mg tadalafil (group B), or LI-SWT plus alternate-day 20 mg tadalafil (group C). The groups were compared for relevant demographic and clinical characteristics. The patients' International Index of Erectile Function-5 (IIEF-5) scores and the Erection Hardness Score (EHS) were assessed at baseline, 3 months post-treatment, and 6 months post-treatment. In addition, a comparison of the three groups was conducted based on their IIEF-5 scores, specifically the ratios of IIEF-5 scores greater than or equal to 17 and those below 17. The cutoff value of 17 was used to distinguish between mild-moderate and moderate ED. Similarly, the patient rates with EHS ≥ 3 and < 3 have been compared between the groups.
LI-ESWT procedure
A standard ultrasound gel was applied, after which penis was stretched manually to prepare for the treatment, and LI-ESWT was performed. Low-intensity extracorporeal shock wave (3,000 SWs, energy intensity of 0.25 mJ/mm2) was applied to six treatment points (500 SWs each) through an applicator: four along the penile shaft and two at the crural level. All of the studies included use the Duolith SD1 ultra (Storz Medical AG, Tägerwilen, Switzerland) for LI-ESWT. No local or systemic analgesia was required during the procedure.
Statistical analysis
Data were analyzed using SPSS 25.0.0.1 software (IBM Corp., Armonk, NY, USA) and considered statistically significant if p < 0.05. Descriptive statistics were calculated for all variables. The chi-square test was used to test for independence between categorical variables. One-way ANOVA and one-way repeated ANOVA were used to test for differences between groups and paired samples over multiple time points, respectively. Significant differences were identified using post hoc tests where applicable. The Kruskal–Wallis and Friedman tests were used for non-parametric data.
Results
In this study, a total of 105 patients were enrolled, with 27 patients in group A, 42 patients in group B, and 36 patients in group C. The mean age of the patients was 56.2 ± 7.4 years. It was determined that there were no statistically significant differences in demographic or characteristic features, baseline IIEF-5 scores, or EHS values between the groups. The summary of these variables is presented in Table 1.
At 3 months post-treatment, IIEF-5 scores increased by 4.1 ± 0.6, 7.3 ± 0.6, and 8.2 ± 0.6 in groups A, B, and C, respectively, and these increases were sustained at 6 months with scores increasing by 3.7 ± 0.6, 7.3 ± 0.6, and 8.5 ± 0.7 in groups A, B, and C, respectively. Statistical analysis revealed that the increase in IIEF-5 scores was comparable between groups B and C, while being significantly higher than that observed in group A at the 3-month and 6-month follow-ups (p = 0.001 and p < 0.001, respectively) (Table 2).
Based on the data obtained, it was observed that the mean EHS value after a period of three and six months post-treatment was considerably higher in groups B and C in comparison to group A. This difference was found to be statistically significant (Table 2). However, upon analyzing the change in EHS scores at 3 months and 6 months post-treatment, no statistically significant difference was observed between the groups (Table 2).
Before treatment, only 17 (16.2%) patients had an EHS of ≥ 3. However, at 3 months and 6 months post-treatment, the number of patients with an EHS score of ≥ 3 significantly increased to 86 (81.9%) and 85 (81%), respectively. The rate of patients with EHS ≥ 3 at both the 3rd and 6th months after treatment was found to be superior in group B and group C compared to group A (p = 0.012 and p = 0.004, respectively) (Table 3). Remarkably, in groups B and C, the number of patients with an EHS score of ≥ 3 remained constant at 3 months and 6 months post-treatment. Similirly, before treatment, only 2 patients (1.9%) had an IIEF-5 score of ≥ 17. However, at 3 months and 6 months post-treatment, the number of patients with an IIEF-5 score of ≥ 17 significantly increased to 52 (49.5%). Notably, there were no patients in group A with an IIEF-5 score of ≥ 17 at 6 months post-treatment (Table 3). At 3 months, the number of patients with an IIEF-5 score of ≥ 17 in group B and group C was 24 (57.1%) and 26 (72.2%), respectively, and at 6 months, it was 25 (59.5%) and 27 (75%), respectively, with no significant difference observed between the two groups (p = 0.166 and p = 0.148, respectively). No significant side effects were reported in the three groups.
Discussion
Tadalafil and LI-SWT are two different treatment options for ED that work through different mechanisms. Tadalafil acts by inhibiting the enzyme phosphodiesterase type 5 (PDE5), which increases the levels of cyclic guanosine monophosphate and enhances smooth muscle relaxation, leading to improved blood flow and erectile function (EF). LI-SWT is a non-invasive treatment that uses low-intensity sound waves to improve blood flow and stimulate the growth of new blood vessels in the penis. It can be postulated as a hypothesis that combining LI-SWT with PDE5i may lead to an improvement in EF among patients with PDE5i-resistant ED. This hypothesis is grounded in the potential of LI-SWT to enhance the production of nitric oxide, promote neovascularization and improve nerve function, which may complement the effects of PDE5i by enhancing their absorption and efficacy [9].
There are two main tadalafil regimens that are used in the treatment of ED. "Daily tadalafil regimen" involves taking a low dose of tadalafil (5 mg) every day, regardless of sexual activity. This approach provides a continuous effect of the medication and allows for spontaneity in sexual activity. “On-demand tadalafil regimen” involves taking a higher dose of tadalafil (10 mg or 20 mg) shortly before sexual activity. This approach provides a more immediate effect, but requires planning and timing of sexual activity. In general, both the daily and on-demand regimens have been shown to be effective in improving EF and achieving successful sexual intercourse [10]. In a meta-analysis of 21 randomized controlled trials (RCTs) involving over 4000 men with ED, it was concluded that tadalafil was effective in improving EF for most clinical populations. In addition, both daily and on-demand regimens showed efficacy in treating ED without one dose regimen being superior to the other [11]. The choice of regimen may depend on individual patient factors, such as sexual frequency and personal preference. While there are studies comparing different tadalafil regimens such as the studies mentioned, none of these studies were conducted with the specific aim of exploring the optimal dosage of tadalafil in relation to the administration of LI-SWT.
Alternate-day tadalafil treatment is not a commonly recommended regimen for the treatment of ED. However, some studies have shown that alternate-day dosing may be effective with less advers events for some patients, particularly those who experience adverse effects with on-demand dosing [12]. In a recent study, the safety and effectiveness of using 20 mg of tadalafil every three days to treat ED in diabetic men were examined. The results emphasized the promising and safety nature of this treatment regimen. The study found that 20 mg of tadalafil every three days significantly improved the IIEF-5 score, with a mean change of 7.1 points. The study also emphasized that tadalafil was well-tolerated, with a partially low incidence of adverse events [13].
LI-SWT has been shown to improve both EHS and IIEF-5 scores in the treatment of ED, according to several meta-analyses. A meta-analysis published in 2020 included 15 studies with a total of 987 non-responder to PDEi5 patients and found that LI-SWT significantly improved both EHS and IIEF-5 scores [14]. Similarly, our study revealed a statistically significant increase in the IIEF-5 score and EHS among patients with PDE5i-resistant ED who were treated with LI-SWT alone. However, the clinical significance of this increase in erectile capacity is questionable, as there were no patients who achieved an IIEF-5 score of ≥ 17, despite the EHS ≥ 3 rate increasing to 59.3% in the LI-SWT-only group (which was close to 90% in the tadalafil groups) after 6 months of follow-up. Furthermore, it appears imperative to conduct additional research on combination therapies to be utilized in combination with LI-SWT to enhance the efficacy of LI-SWT and attain maximal erectile capacity.
In recent years, researchers have suggested that combining different therapies with LI-SWT can improve LI-SWT effectiveness. For instance, a study showed that the combination of Li-ESWT with stem cell therapy resulted in enhanced formation of new blood vessels [15]. Another study reported that the use of platelet-rich plasma plus LI-ESWT was more effective than using LI-ESWT alone [16]. Nevertheless, in order to obtain decisive evidence, it may be imperative to validate the outcomes of these studies by conducting further investigations utilizing analogous methodologies in a more extensive patient population. In addition, one of the most commonly used approaches in combination therapy with LI-SWT is LI-SWT along with tadalafil.
Several studies have reported positive results with LI-SWT plus PDE5i in patients with ED who are non-responsive to PDE5i therapy. A double-blind RCT involving 58 patients found that those who received LI-SWT plus PDE5i had a significant improvement in their IIEF-5 score compared to the sham group. The mean increase in IIEF-5 score was 5 points in the LI-SWT group compared to 0 points in the sham group. In the LI-SWT group, 54.1% of patients achieved an erection hard enough for vaginal penetration [17]. In contrast to our study, this study did not include a patient group receiving LI-SWT alone. Instead, the study incorporated a sham treatment combined with the PDE5i group. Bechara et al. [18] investigated the long-term effectiveness and safety of LI-SWT in 50 patients with ED who did not respond to PDE5i treatment. The results showed that 60% of patients had a positive response to LI-SWT, and the response was maintained for 12 months in %91.7 of responder-patients. Although the patients in this study were administered PDE5i treatment at either the maximum recommended dose or a daily dose consistent with the established protocol, the impact of this variable on treatment outcomes was not specifically examined. Verze et al. [19] reported that in patients with Type 2 Diabetes Mellitus and ED, the combined approach of administering tadalafil 5 mg once daily along with a protocol involving 2400 shockwaves of LI-SWT resulted in significant advantages in terms of improvement in IIEF-5 score, as compared to administering tadalafil 5 mg alone per day.
In a another investigation involving PDE5i non-responders, patients underwent assessment during a follow-up visit after one month of LI-SWT treatment. Subsequently, an active PDE5i medication was administered until the final follow-up assessment. IIEF-5 scores were reported for the pre-treatment phase, the phase after LI-SWT, and the phase after the administration of a PDE5i. The scores were 8.8, 12.3, and 18.8, respectively, and improvement in IIEF-5 scores with PDE5i treatment was remarkable. Each patient was provided with a PDE5i medication regime consisting of four tablets, which was selected based on their individual preferences, but no information was provided as to which of the selected regimens was more beneficial [20]. In another study comprising ED patients who were unresponsive to PDE5is, a dose of 2.5 mg tadalafil was recommended as the only option PDE5i regimen at four weeks following LI-SWT. The average EHS demonstrated a noteworthy improvement in 35% of patients one month after LI-SWT, and in 50% of patients at two and six months after the procedure. The addition of a daily dose of 2.5 mg tadalafil to the treatment notably elevated the EHS scores of PDE5i-unresponsive ED patients [21].
The aforementioned studies have reported that improved EF was achieved when all patients maintained tadalafil treatment on demand or daily while undergoing LI-SWT. However, it is noteworthy that there exists a dearth of information concerning the relative efficacy of different tadalafil regimens. As a significant aspect of our study, patients were stratified into two groups, which received different treatment regimens consisting of tadalafil, in addition to the LI-SWT alone treatment group. Our findings suggest that although the improvement in EF was somewhat more prominent in the group that received the maximum dose of tadalafil alternate day compared to the group that received daily treatment, this difference was not statistically significant. Therefore, it would be more appropriate to recommend any PDE5i regimen to be combined with LI-SWT rather than treating patients with LI-SWT alone. It is important to note that while we emphasize that there is currently no difference between the two PDE5i regimens, the outcomes of future prospective studies with a substantial patient cohort, comparing different PDE5i regimens for combination with LI-SWT, may alter these results.
Our current study may have several limitations. The non-randomise and retrospective nature of the study and the relatively limited sample size may represent potential limitations. Furthermore, it is imperative to acknowledge that our study also bears the limitations of a relatively short follow-up period and an unequal distribution of patients across the distinct groups.
Consequently, in patients with ED who are unresponsive to PDE5i monotherapy, combining PDE5i therapy with LI-SWT is more effective than LI-SWT treatment alone. Although no statistical difference was observed between two different tadalafil regimens combined with LI-SWT treatment, the group receiving 20 mg of tadalafil every other day exhibited a greater improvement in IIEF-5 score and EHS compared to the daily 5 mg tadalafil group. This finding suggests that the observed difference may become statistically significant with an increase in the number of patients enrolled in the study. Further investigations using different tadalafil regimens and larger patient populations are warranted to validate these results.
Data availability
The datasets generated during and/or analyzed during the current study are not publicly available but are available from the corresponding author on reasonable request.
References
Gong B, Ma M, Xie W et al (2017) Direct comparison of tadalafil with sildenafil for the treatment of erectile dysfunction: a systematic review and meta-analysis. Int Urol Nephrol 49:1731–1740
Salonia ABC, Capogrosso P, Carvalho J, Corona G, Hatzichristodoulou G, Jones TH, Kadioglu A, Martinez-Salamanca JI, Minhas S, Serefoglu EC, Verze P (2023) EAU guidelines on sexual and reproductive health [Available from: https://d56bochluxqnz.cloudfront.net/documents/full-guideline/EAU-Guidelines-on-Sexual-and-Reproductive-Health-2023.pdf.
McCabe MP, Matic H (2008) Erectile dysfunction and relationships: views of men with erectile dysfunction and their partners. Sex Relatsh Ther 23(1):51–60
Althof SE, O’Leary MP, Cappelleri JC et al (2006) Impact of erectile dysfunction on confidence, self-esteem and relationship satisfaction after 9 months of sildenafil citrate treatment. J Urol 176(5):2132–2137
Lee D, Nazroo J, Pendleton N (2015) Erectile dysfunction and phosphodiesterase type 5 inhibitor use: associations with sexual activities, function and satisfaction in a population sample of older men. Int J Impot Res 27(4):146–151
Vita R, Benvenga S, Giammusso B et al (2019) Determinants of early response to low-intensity extracorporeal shockwaves for the treatment of vasculogenic erectile dysfunction: an open-label, prospective study. J Clin Med 8(7):1017
Vinay J, Moreno D, Rajmil O et al (2021) Penile low intensity shock wave treatment for PDE5I refractory erectile dysfunction: a randomized double-blind sham-controlled clinical trial. World J Urol 39:2217–2222
Mykoniatis I, Pyrgidis N, Sokolakis I et al (2021) Assessment of combination therapies vs monotherapy for erectile dysfunction: a systematic review and meta-analysis. JAMA Netw Open 4(2):e2036337
Jeon SH, Shrestha KR, Kim RY et al (2016) Combination therapy using human adipose-derived stem cells on the cavernous nerve and low-energy shockwaves on the corpus cavernosum in a rat model of post-prostatectomy erectile dysfunction. Urology 88(226):e1–e9
Brock GB, McMahon CG, Chen K et al (2002) Efficacy and safety of tadalafil for the treatment of erectile dysfunction: results of integrated analyses. J Urol 168(4):1332–1336
Brock G, Ni X, Oelke M et al (2016) Efficacy of continuous dosing of tadalafil once daily vs tadalafil on demand in clinical subgroups of men with erectile dysfunction: a descriptive comparison using the integrated tadalafil databases. J Sex Med 13(5):860–875
Mirone V, Costa P, Damber J-E et al (2005) An evaluation of an alternative dosing regimen with tadalafil, 3 times/week, for men with erectile dysfunction: SURE study in 14 European countries. Eur Urol 47(6):846–854
Nguyen Q, Van Do H (2022) Assessment of the results of treatment erectile dysfunction in diabetic patients by tadalafil 20mg once every there days. J Sex Med 19(5):S188
Grandez-Urbina JA, Rodríguez RP, Torres-Román JS et al (2020) Low-intensity extracorporeal shock wave treatment improves erectile function in non-responder PDEi5 patients: a systematic review. Rev Int de Androl 19(4):272–280
Zhu GQ, Jeon SH, Bae WJ et al (2018) Efficient promotion of autophagy and angiogenesis using mesenchymal stem cell therapy enhanced by the low-energy shock waves in the treatment of erectile dysfunction. Stem Cells Int 2018:14
Ruffo A, Stanojevic N, Romeo G et al (2020) PS-5-3 management of erectile dysfunction using a combination treatment of low-intensity shock waves (LISW) and platelet rich plasma (PRP) intracavernosal injections. J Sex Med 17(6):S133–S134
Kitrey ND, Gruenwald I, Appel B et al (2016) Penile low intensity shock wave treatment is able to shift PDE5i nonresponders to responders: a double-blind, sham controlled study. J Urol 195(5):1550–1555
Bechara A, Casabé A, De Bonis W et al (2016) Twelve-month efficacy and safety of low-intensity shockwave therapy for erectile dysfunction in patients who do not respond to phosphodiesterase type 5 inhibitors. Sex Med 4(4):e225–e232
Verze P, Capece M, Creta M et al (2020) Efficacy and safety of low-intensity shockwave therapy plus tadalafil 5 mg once daily in men with type 2 diabetes mellitus and erectile dysfunction: a matched-pair comparison study. Asian J Androl 22(4):379
Gruenwald I, Appel B, Vardi Y (2012) Low-intensity extracorporeal shock wave therapy—a novel effective treatment for erectile dysfunction in severe ED patients who respond poorly to PDE5 inhibitor therapy. J Sex Med 9(1):259–264
Vena W, Vaccalluzzo L, Morenghi E et al (2021) Low-intensity shockwave treatment (liswt) improves penile rigidity in eugonadal subjects with erectile dysfunction: a pilot study. Minerva Endocrinol 48(1):4–11
Funding
The authors declare that they have no relevant financial.
Author information
Authors and Affiliations
Contributions
MAI & FO performed the research, CA & ZT analyzed the data and wrote the paper, and OY designed the research study and wrote the paper. All authors approve the final version of the text.
Corresponding author
Ethics declarations
Conflict of interest
No conflict of interest was declared by the authors.
Ethical approval
The study was approved by the Ankara University Faculty of Medicine Ethics Committee (protocol number [i06-397–23]).
Informed consent
This is a retrospective analysis based on electronic medical record data. According to the requirements of ethics committee of Ankara University, informed consent can be exempted after anonymization of medical record data.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
İbis, M.A., Ozkaya, F., Tokatli, Z. et al. Efficacy of low-intensity shockwave therapy with different tadalafil regimens in patients with PDE5 inhibitor-resistant erectile dysfunction: a retrospective cohort study. Int Urol Nephrol 56, 407–413 (2024). https://doi.org/10.1007/s11255-023-03769-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-023-03769-w