Abstract
Purpose
The COVID-19 pandemic has highlighted the difficulties healthcare systems face to care for patients with chronic diseases. In the state of Victoria, Australia, the government implemented a state-wide lockdown and restricted the delivery of healthcare to limit the spread of the virus. This study investigated the impact of the pandemic on healthcare access, mental and physical health for patients with chronic kidney disease (CKD).
Methods
Patients with stage 4 or 5 CKD were recruited from the nephrology unit of a metropolitan hospital in Victoria. Participants completed a quantitative and qualitative questionnaire that assessed the impact of the pandemic on their access to healthcare and mental and physical health. The quantitative data were analysed by a series of one-way between-groups analysis of variance (ANOVAs) comparing impact between different time periods since the beginning of the pandemic.
Results
Participants (n = 75) completed the questionnaire from 30 March 2020 to 29 September 2021. Participants reported significant disruptions to accessing healthcare in the initial 6 months of the pandemic. There were no significant differences in the quantitative assessments of physical and mental health of participants across the 18 months of this study. The participants’ qualitative comments about disrupted normal activities, feeling vulnerable to COVID-19, transitioning to telehealth, feeling isolated and vaccination protection provided further insight into the cumulative negative mental health impact of the extended lockdown.
Conclusion
Our findings highlight the importance of optimising telehealth to improve communication between CKD patients and their treating teams and continuing to monitor the impacts of pandemic restrictions on patients’ mental and physical health.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Across the world, many governments implemented restrictions and lockdowns to limit the spread of the COVID-19 virus and directed healthcare resources towards caring for COVID-19 patients. Evidence is now emerging with reference to how the pandemic impacted the ongoing care of patients with chronic illnesses unrelated to COVID-19. Recent reviews have highlighted that patients with chronic diseases that require ongoing management, including chronic kidney disease (CKD), may be particularly affected by changes to healthcare access, and experience adverse physical and mental health outcomes due to the pandemic restrictions [1].
During the pandemic, healthcare settings were deemed ‘high-risk’ for COVID-19 transmission [2] and transition to telehealth services occurred globally to minimise physical contact with patients [3]. A systematic review demonstrated that telehealth is useful for providing continuous care to patients during the pandemic [3], however, the transition to telehealth in CKD patients has unique challenges. As the population of patients with CKD usually comprises older adults, telehealth usage can be limited by the increased prevalence of poorer cognition, vision and hearing impairment, and lack of required technology and/or technological know-how [4]. In Victoria, Australia, community transmission of COVID-19 remained relatively low throughout 2020, yet transmission within hospitals was concerning [5]. Despite the Victorian Government’s stay-at-home orders, CKD patients were allowed to visit high-risk hospital settings for essential treatment [6].
In addition to healthcare access, the pandemic also impacted mental health globally. People managing chronic health conditions or those with a history of psychiatric problems were more likely to suffer from poor mental health outcomes during the pandemic, unrelated to contracting the COVID-19 virus [7, 8]. CKD is often associated with psychological comorbidities such as anxiety [9] and depression [10], yet evidence regarding how the pandemic impacted the mental health of patients with CKD is lacking.
The pandemic restrictions also limited usual practices to maintain physical health, which have had a negative impact on physical activity levels and adherence to healthy diets, particularly for people with chronic diseases [11]. CKD management guidelines highlight the importance of lifestyle strategies such as physical exercise, weight loss, healthy diet, and reduction in alcohol and smoking [12]. The impact of the 154 days spent in lockdown [13] and a one-hour daily exercise limit on the physical health of patients with CKD remains to be determined.
Evidence from other countries indicates potential concern for the impact of the pandemic on CKD patients in relation to access to healthcare, mental health and physical health. Accordingly, it is important to investigate these impacts specifically in Victoria, Australia, where prolonged strict Government mandates were implemented. The current study aimed to determine the impact of the COVID-19 pandemic on patients with CKD, specifically in relation to access to healthcare and impact on both mental health and physical health. It was hypothesised that there would be minimal impact on access to healthcare due to the rapid transition to telehealth and the continued delivery of essential in-person healthcare, but that the extended lockdown and restrictions would have significant negative impacts on the mental health and physical health of people with CKD.
Methods
Research design and setting
Patients from the nephrology unit of St Vincent’s Hospital, a large metropolitan hospital in Melbourne, Australia, were recruited prior to the COVID-19 pandemic for a separate, larger study [14]. We received approval from the St Vincent’s Hospital Human Research Ethics Committee (HREC-A 019/14) to collect additional COVID-19 pandemic data from the participants of that study. Written informed consent was obtained from all participants.
Participants
Participants were recruited from the nephrology department through out-patient clinic attendance or clinician referral. Eligible participants met the following inclusion criteria: (1) Stage 4 or 5 CKD, evidenced by an eGFR of < 30 ml/min; (2) 18 years or older; (3) English speaking; and (4) absence of cognitive deficits that would preclude informed consent. Full eligibility criteria are described elsewhere [15].
Impact of COVID-19
The impact of COVID-19 on mental health, physical health and changes to access in healthcare (Appendix) were reported by participants for 18 months following the declaration of a human biosecurity emergency on 18 March 2020 [16]. Participants were also asked to comment on any other impact the COVID-19 pandemic had on their mental or physical health.
Statistical analyses
Data analyses were performed using SPSS Version 27. Means and standard deviations were calculated for continuous variables, and frequencies were measured for categorical variables. To ensure generalisability of the results, key participant characteristics were compared between the sample that had completed the COVID-19 questionnaire and the larger sample of participants with CKD who participated in the randomised controlled trial. Assessments of the impact of COVID-19 were grouped into three time points:
-
i.
Initial 6 months (18/3/2020 – 29/9/2020);
-
ii.
6–12 months (30/9/2020 – 29/3/2021);
-
iii.
12–18 months (30/3/2021–29/9/2021).
Differences between time points since the beginning of the pandemic on the impact of COVID-19 were assessed by a series of Analysis of Variance (ANOVA) tests.
Results
The assessment of the impact of COVID-19 questionnaire was completed by 75 participants; see Table 1 for participant characteristics.
There were no significant differences between the current sample and the larger trial sample age, gender, or ethnicity. However, the current sample included a significantly greater proportion of individuals who were not on dialysis (72%) and a significantly lower proportion of individuals who were on peritoneal dialysis (11%) compared to all trial participants, respectively (52%, 22%; χ2(2, N = 226) = 8.80, p = 0.012).
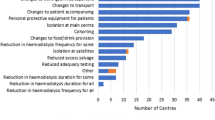
Across the three 6-month time periods following the beginning of the COVID-19 pandemic, there was a significant difference in reported access to healthcare reported (Table 2). Participants reported significantly greater impact on their access to healthcare related to the COVID-19 pandemic in the 6 months immediately following the beginning of the pandemic, compared to the 6–12-month follow-up period. There were no significant differences across the three time periods on the quantitative assessment of impact of COVID-19 on physical or mental health (Table 2).
Participants (n = 48) also provided qualitative comments on the impact of the COVID-19 pandemic on their mental or physical health which were thematically grouped (Table 3).
Discussion
The current study aimed to assess the impact of the COVID-19 pandemic on CKD patients in relation to access to healthcare, and impact on both mental health and physical health. The hypothesis that there would be no significant impact on access to healthcare was not supported. The hypothesis that there would be significant impacts on the mental and physical health of CKD patients due to the pandemic was partially supported, given the qualitative feedback from participants indicated some impact on functioning.
Access to healthcare
Participants in this study self-reported significantly greater difficulty accessing healthcare during the initial 6 months of the pandemic, compared to 12 months and 18 months. Participants commented on increased difficulty accessing routine face-to-face healthcare during the earlier months of the pandemic, and challenges with the transition and adjustment to telehealth. Beyond 6 months, there was no significant increased difficulty accessing healthcare, likely due to patients adjusting to utilising telehealth. Other studies have also found that telehealth has maintained convenient access to healthcare during the pandemic, but restricted non-verbal communication with the clinician and required adjustment to the technology [17, 18]. A meta-analysis of the pandemic and access to healthcare for CKD patients found increased telehealth use to maintain patient care, but reduced access to dialysis [19], highlighting the need for increased focus on improving the utility of telehealth for CKD patients and their treatment teams.
Physical and mental health
This study found no significant impact of pandemic restrictions on participants’ quantitative self-reported physical health. However, respondents provided qualitative feedback detailing disruptions to their usual exercise activities, which created a gap in their healthcare plans. Globally, the impact of COVID-19 pandemic restrictions on physical health has been varied. A mixed-methods study conducted in Portugal found that patients with CKD had difficulties maintaining physical activity levels and adhering to dietary restrictions during lockdown [20]. However, an observational longitudinal study conducted in France and Switzerland found that walking and moderate physical activity increased during the pandemic compared to pre-pandemic levels, albeit sedentary behaviour also increased [21]. In Australia, increased alcohol-use associated with social isolation and pandemic lockdowns has been reported, but these studies have focused on the general population rather than CKD patients [22, 23]. Further research should focus on how the pandemic has impacted specific areas of CKD patients’ physical health, and how patients can adapt their lifestyle strategies to suit the evolving pandemic context.
While participants did not report any differences in the quantitative assessment of impact of the pandemic on mental health, qualitative feedback demonstrated increased psychological distress and isolation in some participants. The comments are consistent with studies which found significant increases in clinical depression and anxiety in the general Victorian population during the prolonged restrictions [8, 23], likely due to the cumulative impacts of lockdown on population mental health. Similarly, adults with type 2 diabetes mellitus in Victoria have also self-reported negative impacts of the pandemic restrictions on emotional wellbeing and leisure activities, despite the study finding no increased anxiety or depressive symptoms compared to pre-COVID-19 levels [24]. In our study, some participants reported concerns about their vulnerability to COVID-19 infection due to CKD and feeling unsafe to leave home, while others expressed increased feelings of confidence and protection after receiving a COVID-19 vaccination. The lack of significant change in the quantitative assessment of impact on mental health in the current study is similarly reported in another retrospective study, which did not find any significant increase in psychological distress, depression or anxiety scores in the general population of Victoria, Australia, compared to pre-pandemic levels [25]. The authors of that study hypothesised that the pandemic resulted in an increase in the number of people experiencing mild or moderate mental health symptoms, which was reflected as an increase in the demand for digital mental health services, but there was no increase in the average severity of the symptoms [25].
Despite this, the qualitative comments in the current study suggest that there was a degree of negative impact of ongoing pandemic restrictions on mental wellbeing.
Conclusion
This study found that CKD patients in Victoria experienced disruptions to accessing healthcare in the initial 6 months of the COVID-19 pandemic, as face-to-face appointments rapidly transitioned to telehealth. Further research is required to assess how telehealth can be optimised to improve communication between CKD patients and their treating teams. Qualitative comments demonstrated concerns about disruption to physical activity and feelings of isolation in CKD patients during the 18 months following the introduction of the COVID-19 pandemic in Melbourne, Australia, which likely correspond with the cumulative negative impact of extended restrictions on mental health in the general Victorian population. As the pandemic context and restrictions (some self-imposed) continue to evolve, ongoing assessments on the physical and mental health of CKD patients will continue to be an important focus for future research.
References
Kendzerska T, Zhu DT, Gershon AS et al (2021) The effects of the health system response to the COVID-19 pandemic on chronic disease management: a narrative review. Risk Manag Healthcare Policy 14:575–584
Li J, Li S-X, Zhao L-F, Kong D-L, Guo Z-Y (2020) Management recommendations for patients with chronic kidney disease during the novel coronavirus disease 2019 (COVID-19) epidemic. Chronic DiS Transl Med 6(2):119–123
Monaghesh E, Hajizadeh A (2020) The role of telehealth during COVID-19 outbreak: a systematic review based on current evidence. BMC Public Health 20(1):1193
Novick TK, Rizzolo K, Cervantes L (2020) COVID-19 and kidney disease disparities in the United States. Adv Chronic Kidney Dis 27(5):427–433
Buising KL, Williamson D, Cowie BC et al (2021) A hospital-wide response to multiple outbreaks of COVID-19 in health care workers: lessons learned from the field. Med J Aust 214(3):101-104.e101
Media hub—coronavirus (COVID-19) [press release]. Melbourne: department of health and human services, 20 September 2021 2020
Flaherty GT, Hession P, Liew CH et al (2020) COVID-19 in adult patients with pre-existing chronic cardiac, respiratory and metabolic disease: a critical literature review with clinical recommendations. Trop Dis Travel Med Vaccin 6:16–16
Fisher J, Tran T, Hammarberg K et al (2021) Quantifying the mental health burden of the most severe covid-19 restrictions: a natural experiment. J Affect Disord 293:406–414
Webster AC, Nagler EV, Morton RL, Masson P (2017) Chronic kidney disease. Lancet 389(10075):1238–1252
Levenson JL, Glocheski S (1991) Psychological factors affecting end-stage renal disease. Psychosomatics 32(4):382–389
Jiménez-Pavón D, Carbonell-Baeza A, Lavie CJ (2020) Physical exercise as therapy to fight against the mental and physical consequences of COVID-19 quarantine: special focus in older people. Prog Cardiovasc Dis 63(3):386–388
Levin A, Hemmelgarn B, Culleton B et al (2008) Guidelines for the management of chronic kidney disease. CMAJ 179(11):1154–1162
Victorian COVID-19 data. Department of Health and Human Services. https://www.coronavirus.vic.gov.au/victorian-coronavirus-covid-19-data. Published 2021. Accessed 20 September 2021, 2021
Jenkins ZM, Tan EJ, O’Flaherty E et al (2021) A psychosocial intervention for individuals with advanced chronic kidney disease: a feasibility randomized controlled trial. Nephrology 26(5):442–453
Knowles SR, Ski CF, Langham R et al (2016) Design and protocol for the dialysis optimal health program (DOHP) randomised controlled trial. Trials 17(1):447
Biosecurity Declaration 2020. In: Health, ed. ACT: Federal Register of Legislation
Huuskes BM, Scholes-Robertson N, Guha C et al (2021) Kidney transplant recipient perspectives on telehealth during the COVID-19 pandemic. Transpl Int 34(8):1517–1529
Schulz T, Long K, Kanhutu K, Bayrak I, Johnson D, Fazio T (2020) Telehealth during the coronavirus disease 2019 pandemic: rapid expansion of telehealth outpatient use during a pandemic is possible if the programme is previously established. J Telemed Telecare 28:445
Deng D, Liang A, Chui JN, Wong G, Cooper TE (2021) The COVID-19 pandemic and access to health care in people with chronic kidney disease: a systematic review and meta-analysis. Nephrology 27:410
Sousa H, Ribeiro O, Costa E et al (2021) Being on hemodialysis during the COVID-19 outbreak: a mixed-methods’ study exploring the impacts on dialysis adequacy, analytical data, and patients’ experiences. Semin Dial 34(1):66–76
Cheval B, Sivaramakrishnan H, Maltagliati S et al (2021) Relationships between changes in self-reported physical activity, sedentary behaviour and health during the coronavirus (COVID-19) pandemic in France and Switzerland. J Sports Sci 39(6):699–704
Czeisler MÉ, Wiley JF, Facer-Childs ER et al (2021) Mental health, substance use, and suicidal ideation during a prolonged COVID-19-related lockdown in a region with low SARS-CoV-2 prevalence. J Psychiatr Res 140:533–544
Jiang J, Akhlaghi H, Haywood D, Morrissey B, Parnis S (2022) Mental health consequences of COVID-19 suppression strategies in Victoria, Australia: a narrative review. J Int Med Res 50(11):03000605221134466
Sacre JW, Holmes-Truscott E, Salim A et al (2021) Impact of the COVID-19 pandemic and lockdown restrictions on psychosocial and behavioural outcomes among Australian adults with type 2 diabetes: Findings from the PREDICT cohort study. Diabet Med 38(9):e14611–e14611
Staples L, Nielssen O, Kayrouz R, Cross S, Karin E, Ryan K et al (2021) Rapid report 3: mental health symptoms, characteristics, and regional variation, for users of an Australian digital mental health service during the first 8 months of COVID-19. Internet Interv 24:100378
Funding
This work was supported through the Australian Government’s Medical Research Future Fund Rapid Applied Research Translation and the Victorian Medical Research Acceleration Fund Grants. Department of Industry, Science, Energy and Resources, Australian Government, Rapid Applied Research Translation initiative, Zoe M Jenkins, Department of Jobs, Precincts and Regions, Victorian Medical Research Acceleration Fund, Zoe M Jenkins
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no competing interests to declare that are relevant to the content of this article. The authors would like to thank the participants involved in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix: COVID-19 related questions
Appendix: COVID-19 related questions

Rights and permissions
About this article
Cite this article
Jiang, J.J., Jenkins, Z.M., Crocker, K.M. et al. Impact of the COVID-19 pandemic on access to healthcare, physical and mental health among patients with chronic kidney disease in Victoria, Australia. Int Urol Nephrol 55, 1635–1640 (2023). https://doi.org/10.1007/s11255-023-03480-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-023-03480-w