Abstract
Introduction
Patients with end-stage kidney disease (ESKD) on dialysis have a special profile, including constant uremic status and frequent comorbidities, such as diabetes mellitus, arterial hypertension and coronary artery disease, as well as complications related to dialysis. All listed factors can influence or be the cause of sexual dysfunction in both men and women. There is a high incidence (70%) and prevalence (82%) of erectile dysfunction in men with CKD.
Purpose
In this meta-analysis, we aimed to evaluate the impact of renal transplantation in patients with end-stage chronic kidney disease and erectile dysfunction, using the same study population before and after transplantation.
Data sources: we searched MEDLINE (PubMed), Embase, Scopus and Cochrane Library (Inception to August 2022) and clinicaltrials.gov (Inception to August 2022) without language restrictions.
Study selection: eligible studies evaluated the same patients with end-stage kidney disease before and after renal transplantation using IEEF questionnaire.
Data extraction: reviewers working independently and in duplicate extracted data and assessed the risk of bias.
Data synthesis: the final analysis included 28 cohort studies, comprising 2252 participants.
Results
Our results showed improvement in erectile function after renal transplantation. Our study shows a 13% improvement in erectile dysfunction after renal transplantation.
Conclusions
The results of this meta-analysis would suggest improvement in erectile dysfunction after renal transplantation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Patients with end-stage kidney disease (ESKD) on dialysis have a special profile, including constant uremic status, frequent comorbidities, such as type 2 diabetes mellitus (T2DM), arterial hypertension, dyslipidaemia and coronary artery disease. Additionally, complications related to dialysis may occur, such as peritonitis in patients on continuous ambulatory peritoneal dialysis, access-related or hemodynamic in patients on haemodialysis. In addition, patients on dialysis have constant contact with the healthcare system, a lower quality of life, which can cause a range of neuropsychiatric disorders, such as depression, anxiety and distress. All these listed factors and the added comorbidities may influence or be the cause of sexual dysfunction in both men and women.
Erectile dysfunction (ED) is known to have a negative impact on the quality of life. The first epidemiological survey of sexual dysfunction in patients with chronic kidney disease (CKD) was conducted in 1972 [1] and since then several studies confirmed that the prevalence of sexual dysfunction in haemodialysis patients is high [2].
Erectile and kidney dysfunction share common risk factors associated with conditions that involve endothelial impairment such as coronary artery disease, dyslipidaemia, diabetes mellitus, hypertension, smoking and obesity [3, 4]. Increasing evidence suggests that CKD is frequently associated with psychosocial factors, such as anxiety, depression, and health-related poor quality of life, all of which can result in sexual dysfunction [5]. There’s a high incidence (70%) and prevalence (82%) of erectile dysfunction in men with CKD [2, 6].
Kidney transplant (KT) is recognized to be the best treatment for end-stage renal disease (ESRD), and the number of kidney transplants is increasing worldwide, with restoration of kidney function. Data regarding the state of erectile dysfunction after kidney transplantation is controversial: some studies show that erectile function improves after renal transplant (RT) [7,8,9,10,11,12,13] while other authors suggest that sexual parameters are not affected by renal transplantation [14,15,16,17]. Additionally, some studies have indicated that erectile dysfunction is worsened after kidney transplantation surgery [18,19,20,21].
In the twenty-first century, graft survival and survival of transplant recipients increased due to latest transplantation technology, as well as better evaluation of renal parameters and new immunosuppressive strategies that prevent graft rejection. In this new era of medicine, erectile function in the context of a better quality of life became an important concern for patients and doctors.
Aims
This review aims to evaluate the impact of renal transplantation on erectile dysfunction in men with end-stage chronic kidney disease.
Materials and methods
The updated Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were applied to standardize data search, collection, synthesis, and reporting [22]. For our meta-analysis, we used a protocol registered at OSF Registries (Registration https://doi.org/10.17605/OSF.IO/JV2MQ).
Data sources and search strategy
Potentially relevant studies were searched in the following databases, from the inception until August 2022: MELDINE (PubMed), SCOPUS, Embase and Cochrane library. No language filters were applied in the search process. In addition to aforementioned sources, ClinicalTrials.gov database was also screened for additional citations. References from representative studies were also searched to retrieve further studies for eligibility assessment. Hand search for relevant articles was also performed from textbooks. We used different combinations of keywords and controlled vocabulary to create a comprehensive search strategy: “renal transplant and erectile dysfunction”, “CKD and erectile dysfunction”, “erectile dysfunction after kidney transplant”, “erectile dysfunction”.
Study selection
We conducted a systematic review and meta-analysis including observational cohort studies and randomized controlled trials (RCTs) in men with ESRD that evaluated the role of renal transplant on the impact of erectile dysfunction in men. In this analysis, only ESRD who had undergone renal transplantation were included and the IIEF questionnaire was used. The same group of patients were analyzed using the same questionnaire after surgery. We considered studies that explored the prevalence and predictors of any form of sexual dysfunction in patients with CKD. Studies were eligible if they compared the same group of population before and after renal transplantation. Studies with a population of patients without CKD were excluded, as were studies that compared groups of patients on dialysis with different groups of patients with renal transplant.
Data extraction and synthesis
Data extracted included identifying information, aim of the study, details of the study protocol and demographic data. We extracted characteristics of each study including baseline IIEF score (IIEF—5), IIEF domain (IIEF – 15) (erectile function, intercourse satisfaction, orgasmic function, sexual desire, overall satisfaction), baseline clinical characteristics of the study population, known comorbidities, type of donor, type of anastomosis used during renal transplantation, type of study design, and total duration of follow-up.
Risk of bias
Two reviewers (AM and IN) evaluated the quality of the selected studies independently without blinding to authorship or journal according to recommendations from the Cochrane Collaboration. For the observational studies, the quality was assessed using the Newcastle–Ottawa scale (NOS) [23] The scale used three categories to evaluate: selection of the study groups, the comparability of the groups and the assessment of outcome. Stars awarded for each quality item serve as a quick visual assessment. Stars are awarded such that the highest quality studies are awarded up to nine stars. Disagreements were resolved by consensus. Publication bias was assessed using the funnel plot technique[24].
Main outcomes and measures
The primary outcome of this analysis was to measure the impact of renal transplantation on sexual function using the International Index of Erectile Function (IEEF) score, sexual domains and also other questionaries. Secondary outcomes included: 1. establishing if mean IIEF-15 or IIEF-5 change from baseline in KTs, 2. Number of patients with improvement or worsening of ED on postoperative evaluation.
The International Index of Erectile Function (IIEF) is a widely used, multi-dimensional self-report instrument for the evaluation of male sexual function [25]. It has been recommended as a primary endpoint for clinical trials of ED and for diagnostic evaluation of ED severity [26], and it is now considered gold-standard for measurement of sexual function [27]. This questionnaire includes all aspects of male sexual functions (erection, orgasmic function, libido, and overall satisfaction) and can evaluate as objectively as possible sexual function in male patients [28].
Statistical analysis
We used a random-effects model for meta-analysis and expressed treatment effects as a risk ratio (RR) with 95% confidence intervals (CI). We used the I2 statistic to assess for inconsistency across individual studies. An I2 > 50% indicated large inconsistency across studies (heterogeneity) not explained by chance. We considered a p-value below 0.10 to indicate significant heterogeneity All statistical analyses were performed using Review Manager Version 5.2 (The Cochrane Collaboration 2012).
We conducted sensitivity analyses to explore the influence of the following factors on effect size: repeating the analysis excluding unpublished studies; repeating the analysis taking account of risk of bias; repeating the analysis excluding any very long or large studies to establish how much they dominate the results; repeating the analysis excluding studies using the following filters: diagnostic criteria, language of publication, and country. A funnel plot was visually inspected. For all the analyses, a two-tailed p-value < 0.05 indicated statistical significance. We conducted the analyses in Review Manager (RevMan) Version 5.2. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2012.
Possible source of heterogeneity was explored based on the type of anastomosis (end-to-side to external iliac artery, end-to-end to internal iliac artery or end-to-side to common iliac artery), risk of bias, type of transplantation and year of publication.
Results
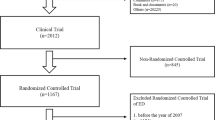
The literature search using the specified databases retrieved 1703 articles. After removing duplicates, 943 articles were screened by title and abstract and 43 articles were read in full-text. We then removed articles where the inclusion criteria were not met, articles that included meta-analyses and articles where the study population was not the same before and after renal transplantation. Finally, a total of 28 articles were included in the present meta-analysis, comprising a total of 2252 participants (Fig. 1).
The articles included in this meta-analysis were observational conducted worldwide. The follow-up period varied between three and 282 months. 17 studies reported the type of renal replacement therapy before renal transplantation. The majority of patients underwent haemodialysis, while out of the same 17 studies, a total of 35 patients were on peritoneal dialysis and 34 patients had a pre-emptive transplantation. Dialysis time before RT was between 6 months to 7 years. 11 studies reported the type of donor involved in the process of RT. The follow-up between studies varied between three months to 72 months. The majority of studies used the IIEF-5 questionnaire as the main method to assess sexual function, while 5 studies used questionnaires developed by the authors. The characteristics of all included studies are included in Table 1.
Regarding the baseline characteristics of all included participants, few studies reported life-style risk factors such as smoking and alcohol [14, 17,18,19, 29,30,31,32,33] or the weight of included participants [17, 18, 30, 33]. Four studies [10, 13, 29, 34] excluded patients with diabetes mellitus. 12 studies reported data on immunosuppressive therapy, while five studies reported other chronic medications. 10 studies also reported the hormone panel before and after renal transplantation. The complete baseline characteristics of all included participants are summarized in Table 2.
Presence or absence of erectile dysfunction after renal transplantation
28 studies included (2252 patients) compared the rate of sexual dysfunction before and after renal transplantation. In dichotomic analysis with a comparison before and after renal transplantation, we found an improvement of 13% regarding sexual dysfunction after renal transplantation. (RR 0.87) (95% CI 0.76–1.00) (Fig. 2).
Improvement versus worsening of erectile dysfunction
We evaluated the impact of renal transplantation on sexual function in an analysis that included 19 studies comprising a total of 1613 participants. Our results show that post-renal transplantation, there was an improvement in erectile dysfunction with 234% (RR 2.3) (95% CI 1.36, 4.01) (Fig. 3).
Impact of renal transplantation on IEEF score
Data reported in six studies show an improvement of mean IEEF score with 3.92 points after KT: (MD 3.92) (CI 95% 3.26 to 4.58) (Fig. 4).
Subdomain analysis was not performed due to insufficient data. Three studies reported other components, such as erectile function, orgasmic function, intercourse satisfaction and overall satisfaction. However, there was not enough data to perform an analysis on these components, but the results generally suggest an improvement in sexual function after renal transplantation.
Type of anastomosis and impact on erectile function
14 studies included the type of anastomosis used during renal transplantation. Gontero et al. reported worsening erectile function with end-to side external iliac artery anastomosis and five studies reported good results using end-to-end or end-to-side internal iliac artery anastomosis. However, there was not enough data to perform an analysis.
Type of immunosuppression used after renal transplantation
13 Studies reported the current regimen of immunosuppression and five studies reported concurrent medications for comorbidities, but there was insufficient data, so that we could not perform a formal analysis based on these components.
Second transplantation and erectile function
Few studies in our analysis reported the number of included patients that had a second transplant. A total of 49 patients underwent a second kidney transplant, but there was insufficient data to perform an analysis.
Risk of bias
We explored the publication bias and found an equal distribution of the included trials (Fig. 5).
The quality of the included studies was assessed using the Newcastle–Ottawa scale (NOS). Starts were awarded for each quality item investigated. Overall, the quality of studies was adequate, with only a few studies that had an average quality score under 7 points. The full assessment of the studies included and overall quality score of each study can be seen in Table 3.
Discussion
Sexual dysfunction is prevalent among individuals with chronic kidney disease. A meta-analysis of 50 studies comprising 8343 participants with CKD, both males and females, reported a high summary estimate of erectile dysfunction in men with CKD—70% [6]. The cause of erectile dysfunction in CKD could be related to the underlying disease (diabetes, arterial hypertension), but it can also be related to the uremic effects on the nervous system and the changes in the hormone panel, such as diminished testosterone production [35].
Our meta-analysis shows that renal transplantation improves erectile function in participants with end-stage renal disease. The majority of the participants included in our study were on renal replacement therapy (especially haemodialysis) before renal transplantation and only 34 had a pre-emptive transplant. Compared to pre-transplant evaluation, our study shows a 13% improvement in erectile dysfunction after renal transplantation. This improvement is also reflected in an analysis of six studies that shows a mean rise of 3.92 points in the IIEF score post-transplant.
Payne et al. [36] conducted a literature review regarding the prevalence and treatment of erectile dysfunction in male solid organ transplant recipients and indicated that the prevalence of erectile dysfunction in male renal transplant recipients was between 54 and 66%. However, it did not evaluate the population pre-transplantation.
Our findings are in line with other meta-analyses that researched sexual function after renal transplantation in CKD patients or patients on renal replacement therapy. One meta-analysis published in 2020 by Kang et al. [37] that included 9 observational studies indicated that renal transplantation may improve erectile function in patients with end-stage kidney disease. They also showed improvement in the mean IIEF 5 and IIEF-15 scores. Compared to our meta-analysis, Kang et al. did not include the same study population before and after renal transplantation and the overall sample size was significantly smaller compared to our analysis. Another meta-analysis conducted by Pyrgidis et al. [38] included a total of 10,320 males with end-stage kidney disease and showed a high prevalence of erectile dysfunction in patients with chronic kidney disease: 79% in patients on haemodialysis, 71% in patients with peritoneal dialysis, 82% in patients starting dialysis. The lowest prevalence of erectile dysfunction was 59% in participants with renal transplantation. However, although Pyrgidis et al. showed that in renal transplantation there is a lower prevalence of erectile dysfunction, they did not evaluate the effect of renal transplantation on erectile function.
Our meta-analysis has a few strong points. First, it has a large population of males (2252 participants) with end-stage kidney disease that underwent renal transplantation. Another advantage is that we only included studies using the same study population before and after renal transplantation. This way, we could evaluate directly the impact of renal transplantation on erectile function. Additionally, the majority of the studies in our meta-analysis used the standardized IIEF to assess sexual function.
However, our study has some limitations, one of which being the observational nature of the studies included and the lack of RCTs conducted on this subject. Another limitation is that we cannot completely rule out overlapping study populations. For example, two of the articles included: El-Bahnasawy et al. A and El-Bahnasawy et al. B had an overlap of 50 patients. Other limitations include the inability to perform analyses regarding the effect of the type of anastomosis used and the effect on erectile function. We could not perform analyses on other factors that could affect erectile function, such as concurrent immunosuppressive regimens used after renal transplantation.
Abnormalities in the serum levels of testosterone, LH, FSH and prolactin have been reported in patients with ESKD. Specifically, testosterone levels tend to be suboptimal in patients on haemodialysis. Some of the studies included in this meta-analysis reported the hormone levels before and after renal transplantation. For example, Akbari et al. and Teng et al. showed that the level of testosterone increased after renal transplantation, while levels of LH, FSH and prolactin decrease. Increase in testosterone levels seem to be consistent among the studies that reported hormone levels, but an analysis could not be performed on these components due to insufficient data.
The underlying pathological mechanisms involving ED and CKD are not completely understood, but various treatments are available, including phosphodiesterase type 5 inhibitors or testosterone therapy in patients with low levels of testosterone. It is important to study the effect of renal transplantation on erectile dysfunction, since erectile dysfunction further affects quality of life and could accentuate certain neuropsychiatric disorders, such as depression and anxiety.
Conclusions
In conclusion, the findings from our meta-analysis show improvement in erectile dysfunction after renal transplantation when compared to pre-transplant evaluation. Additionally, there is also improvement in mean IIEF score. However, further studies with a larger number of patients are needed to investigate the impact of renal transplantation on erectile dysfunction. Moreover, studies are needed to determine whether the type of anastomosis used has an effect on post-transplant sexual function.
Data availability
Data analyzed in this study were a re-analysis of existing data, which are openly available at locations cited in the reference section.
References
Levy NB (1973) Sexual adjustment to maintenance hemodialysis and renal transplantation: national survey by questionnaire: preliminary report. Trans Am Soc Artif Intern Org 19:138–143
Rosas SE et al (2001) Prevalence and determinants of erectile dysfunction in hemodialysis patients. Kidney Int 59(6):2259–2266
Stewart-Bentley M, Gans D, Horton R (1974) Regulation of gonadal function in uremia. Metabolism 23(11):1065–1072
Cerqueira J, Moraes M, Glina S (2002) Erectile dysfunction: prevalence and associated variables in patients with chronic renal failure. Int J Impot Res 14(2):65–71
McKercher C, Sanderson K, Jose MD (2013) Psychosocial factors in people with chronic kidney disease prior to renal replacement therapy. Nephrology (Carlton) 18(9):585–591
Navaneethan, S., et al., Prevalence and predictors of sexual dysfunction in chronic kidney disease: A systematic review and meta-analysis of observational studies. NDT Plus, 2010. 3: p. iii87.
Nassir A (2009) Sexual function in male patients undergoing treatment for renal failure: A prospective view. J Sex Med 6(12):3407–3414
Mehrsai A et al (2006) Improvement of erectile dysfunction after kidney transplantation: the role of the associated factors. Urol J 3(4):240–244
Salvatierra O, Fortmann JL, Belzer FO (1975) Sexual function in males before and after renal transplantation. Urology 5(1):64–66
Burgos FJ et al (1997) Effect of kidney transplantation and cyclosporine treatment on male sexual performance and hormonal profile: a prospective study. Transplant Proc 29(1–2):227–228
Pourmand G et al (2007) Does renal transplantation improve erectile dysfunction in hemodialysed patients? What is the role of associated factors? Transpl Proc 39(4):1029–1032
Ahmad M et al (2009) Impact of renal transplantation on erectile dysfunction due to chronic renal failure in male patients. J Ayub Med Coll Abbottabad 21(1):69–71
Teng LC, Wang CX, Chen L (2011) Improved erectile function and sex hormone profiles in male Chinese recipients of kidney transplantation. Clin Transplant 25(2):265–269
Gontero P et al (2012) Does kidney transplantation onto the external iliac artery affect the haemodynamic parameters of the cavernosal arteries? Asian J Androl 14(4):621–625
Tsujimura A et al (2002) Effect of renal transplantation on sexual function. Arch Androl 48(6):467–474
Jürgensen JS et al (2008) Sexual dysfunction after simultaneous pancreas-kidney transplantation. Transpl Proc 40(4):927–930
Mota RL et al (2019) Sexual dysfunction and satisfaction in kidney transplant patients. Journal of Sexual Medicine 16(7):1018–1028
Mirone V et al (2009) Renal transplantation does not improve erectile function in hemodialysed patients. Eur Urol 56(6):1047–1054
El-Bahnasawy MS et al (2004) Effect of the use of internal iliac artery for renal transplantation on penile vascularity and erectile function: A prospective study. J Urol 172(6 I):2335–2339
Peşkircioǧlu L et al (1998) Evaluation of erectile function in renal transplant recipients. Transpl Proc 30(3):747–749
Musone D et al (2003) Erectile dysfunction in kidney transplanted patients. Minerva Urol Nefrol 55(3):193–197
Page MJ et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71
Stang A (2010) Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 25(9):603–605
JPT, H., Cochrane Handbook for Systematic Reviews of Interventions ed. G. S. Vol. Version 5.1.0. 2011, The Cochrane Collaboration.
Rosen RC et al (1997) The international index of erectile function (IIEF): a multidimensional scale for assessment of erectile dysfunction. Urology 49(6):822–830
Rosen RC et al (2007) Development and validation of four-item version of Male Sexual Health Questionnaire to assess ejaculatory dysfunction. Urology 69(5):805–809
Cappelleri JC et al (1999) Diagnostic evaluation of the erectile function domain of the International Index of Erectile Function. Urology 54(2):346–351
Rosen RC et al (2011) Minimal clinically important differences in the erectile function domain of the International Index of Erectile Function scale. Eur Urol 60(5):1010–1016
El-Bahnasawy MS et al (2004) Critical evaluation of the factors influencing erectile function after renal transplantation. Int J Impot Res 16(6):521–526
Guo P et al (2010) Erectile dysfunction in living donor kidney transplant recipients associated with chronic hepatitis b infection. Transpl Proc 42(7):2556–2559
Qiao Q et al (2009) Prevalence and prognostic factors for erectile dysfunction in end-stage renal disease patients before and after renal transplantation. Eur Urol Suppl 8(4):141
Shamsa A, Motavalli SM, Aghdam B (2005) Erectile function in end-stage renal disease before and after renal transplantation. Transpl Proc 37(7):3087–3089
Spirito L et al (2020) Impact of kidney transplantation on male sexual function: results from a ten-year retrospective study. Journal of Sexual Medicine 17(11):2191–2197
Akbari F et al (2003) Effect of renal transplantation on sperm quality and sex hormone levels. BJU Int 92(3):281–283
Lundy SD, Vij SC (2019) Male infertility in renal failure and transplantation. Translational Andrology and Urology 8(2):173–181
Payne K et al (2021) The prevalence and treatment of erectile dysfunction in male solid organ transplant recipients. Sexual Medicine Reviews 9(2):331–339
Kang J et al (2020) Erectile function after kidney transplantation: a meta-analysis. Translational Andrology and Urology 9(5):1967–1979
Pyrgidis N et al (2021) Prevalence of erectile dysfunction in patients with end-stage renal disease: a systematic review and meta-analysis. J Sex Med 18(1):113–120
Nghiem DD et al (1983) Factors influencing male sexual impotence after renal transplantation. Urology 21(1):49–52
Tian XH et al (2007) Impacts of kidney transplantation on erectile function and its contributing factors evaluation. Zhonghua nan ke xue = Natl J Androl 13(5):431–434
Peng T et al (2007) Erectile function in male kidney transplant recipients and effects of different methods of renal arterial anastomosis. Zhonghua nan ke xue = Natl J Androl 13(5):396–399
Raggi MC et al (2012) Sexual and relationship functioning before and after renal transplantation: a descriptive study with patients and partners. Scand J Urol Nephrol 46(6):431–436
Jabali SS et al (2020) Erectile dysfunction pre and post kidney transplant recipients in Duhok city; cross sectional study. Ann Med Surg 55:107–110
Soliman A, Khashab S (2017) Impact of hemodialysis and renal transplantation on erectile function in chronic HCV patients with ESRD. Transpl Int 30:340
Nanjappa B et al (2012) Impact of renal transplant on vasculogenic and neurogenic determinants of erectile dysfunction in patients with chronic renal failure. J Urol 187(4):e861
Bujdak P, V.P., Lackova F, Grajtovska B, Breza J (2003) Study of prevalence and severity of erectile dysfunction in patients treated by hemodialysis and kidney transplantation. Eur Urol Suppl 2(1)
Ji ZG et al (2010) Influence of the interruption of arteria iliaca interna distal end on penile vascularity and erectile function in male renal transplant recipients. Zhonghua nan ke xue = Natl J Androl 16(4):341–344
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Miron, A., Stefan, AE., Nistor, I. et al. The impact of renal transplantation on sexual function in males with end-stage kidney disease: a systematic review and meta-analysis. Int Urol Nephrol 55, 563–577 (2023). https://doi.org/10.1007/s11255-022-03442-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-022-03442-8