Abstract
Purpose
Obesity may negatively impact the clinical outcomes of patients undergoing peritoneal dialysis (PD). However, the impact of obesity on PD-related outcomes remains unclear. We herein examined the association of high body mass index (BMI) with complete hemodialysis (HD) transfer, transition to HD and PD/HD hybrid therapy, peritonitis, catheter exit-site and tunnel infection (ESI/TI), and heart failure-related hospitalization.
Methods
This retrospective cohort study included 120 patients who underwent PD-catheter insertion between January 2008 and June 2018. BMI ≥ 25 kg/m2 at the time of PD-catheter insertion was defined as high BMI, and its association with outcomes was analyzed using the log-rank test and Cox proportional hazards models.
Results
The follow-up duration was 46.2 (23.3–75.3) months. The time until transfer to HD and hybrid therapy was significantly shorter in the high BMI group than that in the low BMI group, whereas the time until HD transfer was not significantly different between the two groups (P < 0.001 and 0.18, respectively). Peritonitis-free and ESI/TI-free survivals were significantly shorter in the high BMI group than those in the low BMI group (P = 0.006 and 0.03, respectively). After adjusting for age, sex, diabetes mellitus, and estimated glomerular filtration rate, high BMI remained a significant risk factor for transferring to HD and hybrid therapy, peritonitis, and ESI/TI (hazard ratio [HR] 2.60, P < 0.001; HR 2.08, P = 0.01; HR 2.64, P = 0.02, respectively).
Conclusion
BMI ≥ 25 kg/m2 is a risk factor for transition to HD and hybrid therapy, peritonitis, and ESI/TI, but not for complete HD transfer in Japanese patients with PD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hemodialysis (HD) and peritoneal dialysis (PD) are the two main modalities of renal replacement therapy. Despite the potential advantages of PD compared to HD in terms of residual renal function (RRF), quality of life, and associated patient satisfaction, only 3% on patients who require dialysis use PD [1]. Technique failure leading to cessation of PD may play an important role in the reduced prevalence of PD use, as it was reported that approximately 20% of PD patients completely transferred to HD within 1–2 years after starting PD because of heart failure (HF) due to overhydration, catheter dysfunction, PD-associated peritonitis, or catheter exit-site and tunnel infection (ESI/TI) [2,3,4]. Clarifying pre-dialysis clinical factors associated with technique failure may help identify patients who may benefit more from PD treatment and those who may require careful management to prevent technique failure.
Although obesity has been known to result in a higher risk of peritonitis and HD transfer, data have been inconsistent [5,6,7,8,9,10,11,12]. In general, dialysis clearance is often not adequate in obese patients due to difficulties in achieving efficient solute removal and water removal [13]. A previous study conducted in the United States (US) showed that a body mass index (BMI) ≥ 30 kg/m2 was associated with shorter time to transfer to HD and more frequent peritonitis-related hospitalizations [12]. Furthermore, obesity for Japanese patients was defined by the Japanese Society for the Study of Obesity as a BMI of ≥ 25 kg/m2 [14], which is only equivalent to “overweight” as per the criteria set by the World Health Organization. Currently, no consensus has been established on whether obesity, defined as BMI ≥ 25 kg/m2, is associated with adverse outcomes among Japanese patients with PD.
PD/HD hybrid therapy, wherein patients usually undergo PD 5–6 days a week along with once-weekly HD, is a unique type of renal replacement therapy available in Japan and is an effective way to not only correct inadequate solute removal but also control fluid status [15]. Patients who develop solute retention or fluid overload with PD alone may first choose to transfer to PD/HD hybrid therapy instead of directly transferring to HD alone. The number of patients on PD/HD hybrid therapy in Japan has been increasing annually, since it was first approved by the Japanese National Health Insurance in 2010, with as many as 26.3% of patients with PD switching to hybrid therapy by the end of 2020 [1].
Therefore, this retrospective cohort study was conducted to evaluate the impact of obesity on the outcomes of patients with PD in terms of transition to HD alone or PD/HD hybrid therapy, peritonitis, ESI/TI, and HF-related hospitalization.
Materials and methods
Study population
This single-center retrospective cohort study and all protocols were approved by the ethics committee of the study hospital (approval number: 20211105). The study included patients aged ≥ 20 years who selected PD based on shared decision-making in renal replacement therapy selection, underwent PD-catheter insertion, and started PD at our hospital between January 1, 2008 and June 30, 2018, as well as provided consent for participation. Patients without BMI data at the time of PD-catheter insertion were excluded.
Data collection and patient evaluation
The following demographic data at the time of PD-catheter insertion were obtained from medical records: age, sex, PD modality (continuous ambulatory or automated), method of PD initiation (short-term PD induction and education or stepwise PD initiation using the Moncrief–Popovich technique), history of diabetes mellitus (DM), history of cerebrocardiovascular disease, blood pressure, and type of antihypertensive agents or diuretics used. The Charlson comorbidity index (CCI) was calculated from the records. BMI was calculated using the height (m) and body weight (kg) data at the time of PD-catheter insertion. The geriatric nutritional risk index (GNRI) was calculated using BMI and serum albumin levels [16].
Follow-up
The participants were divided into two groups according to their BMI (Japanese definition) (≥ 25 kg/m2, high BMI group and < 25 kg/m2, low BMI group) [15]. All participants were followed up until PD cessation (i.e., transfer to HD alone), death, kidney transplantation, or study completion (June 30, 2020). The primary outcomes were evaluated in two ways: the first was a complete transition to HD alone, either from PD/HD hybrid therapy or directly from PD, and the second was a transition to HD and PD/HD hybrid therapy, whichever came first (Fig. 1). Participants who either died or received kidney transplants were censored as recommended by the International Society for Peritoneal Dialysis [17]. Transition to HD alone was defined as a transition to thrice weekly HD (including the transition from PD/HD hybrid therapy), and transition to PD/HD hybrid therapy was defined as transferring to a combination of once-weekly HD and 5–6 days a week of PD therapy. In both the therapies, the day of the first HD session was considered the day of transition. Peritonitis, ESI/TI requiring surgical intervention, and HF-related hospitalization were recorded as secondary endpoints, because PD-related infection and HF are two leading causes of PD discontinuation in Japan [18].
Statistical analysis
Continuous variables were described as means ± standard deviation or median (25th–75th percentiles) based on normality assessed by the Shapiro–Wilk test, and binary variables were presented as percentages. Normally and non-normally distributed continuous variables were evaluated by unpaired Student’s t test and Mann–Whitney U test, respectively, and Chi-square test was used for binary variables to compare parameters between groups. Survival curves were plotted by the Kaplan–Meier method and compared by log-rank test. The Cox proportional hazards models were adopted to determine hazard ratios (HRs) with 95% confidence intervals for survival. In addition to the BMI categories, parameters that were previously shown to be associated with time until transfer to HD were included in the multivariate regression model. In adjusted model 1A, age, sex, DM, and estimated glomerular filtration rate (eGFR) were included as candidate independent variables [19,20,21,22]. Of the above variables, CCI replaced DM in adjusted model 1B; DM and CCI were separately analyzed, taking multicollinearity into consideration. Model 2 included the same variables as model 1A, but added the use of angiotensin-converting enzyme inhibitor/angiotensin II receptor blockers (ACEi/ARBs) and loop diuretics as independent variables. Model 3 included the same variables as model 2, but also included logarithmic brain natriuretic peptide (BNP) as one of the volume status markers as an independent variable. For simplicity, the same variables were also selected as potential covariates for multivariate analysis to assess their association with peritonitis-free survival, ESI/TI-free survival, and HF-related hospitalization-free survival, because PD-related infection and HF are two leading causes of PD discontinuation in Japan [18]. Indeed, obesity, older age, sex, DM, and lower RRF have been reported as possible risk factors for PD-related peritonitis [23], which were not far from candidate independent variables selected in this study. Additionally, as death and transplantation were competing risk events against each outcome, the cumulative incidence considering competing risks was compared using Gray’s test, and the Fine–Gray subdistribution hazards model was used in the multivariate model as a sensitivity analysis for each outcome together with the standard Cox regression model for cause-specific hazards [24]. All statistical analyses were performed using EZR (Saitama Medical Center, Jichi Medical University, Saitama, Japan), a graphical user interface for R (The R Foundation for Statistical Computing, Vienna, Austria) [25]. A two-tailed P value < 0.05 was considered significant.
Results
Patients’ clinical characteristics
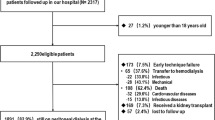
Among 122 eligible patients, two were excluded because of missing values for BMI; therefore, the study cohort included 120 patients (Fig. S1). Table 1 summarizes the clinical characteristics of the study population and the two groups categorized according to BMI. The high BMI group (n = 44) exhibited significantly lower age, higher prevalence of DM, higher frequency of use of ACEi/ARB and loop diuretics, and naturally higher BMI and GNRI values compared with the low BMI group (n = 76) (P = 0.003, 0.02, 0.02, 0.022, < 0.001, and < 0.001, respectively); the remaining characteristics were not significantly different between the groups.
In the study cohort, the median follow-up period was 46.2 (23.3–75.3) months; 35 (29%) patients were directly transferred from PD to HD and 39 (33%) patients were transferred first to PD/HD hybrid therapy and then either remained on PD/HD hybrid therapy (n = 26) or transitioned completely to HD (n = 13) by the end of the study. Consequently, 48 (40%) patients discontinued PD and were transferred to HD alone, and 74 (62%) patients transferred to HD and/or PD/HD hybrid therapy (Fig. 1). In addition, 55 (46%) patients developed peritonitis, 27 (23%) patients developed ESI/TI, and 53 (44%) patients were hospitalized due to HF during the study period. Furthermore, 8 (7%) patients underwent kidney transplantation, and 25 (21%) patients died without transitioning to HD alone. There was no loss to follow up.
Association between high BMI and transfer to HD alone or PD/HD hybrid therapy
A total of 19 (43%) patients in the high BMI group and 29 (38%) patients in the low BMI group transitioned to HD alone, and a total of 20 (45%) patients in the high BMI group and 19 (25%) patients in the low BMI group transitioned to PD/HD hybrid therapy. Furthermore, five (4%) of these patients in the high BMI group and eight (7%) of these patients in the low BMI group subsequently transitioned to HD therapy alone.
In the high BMI group, transition to HD occurred due to peritonitis (n = 12), difficulty in controlling volume overload (n = 2), uremic solute retention (n = 1), major abdominal surgery (n = 3), and tunnel infection (n = 1). In the low BMI group, transition to HD occurred due to peritonitis (n = 13), difficulty in controlling volume overload (n = 4), uremic solute retention (n = 3), difficulties in performing PD due to decreased activities of daily living (n = 5), cerebrovascular disease leading to physical disability (n = 1), catheter malfunction (n = 1), eosinophilia (n = 1), and pleuroperitoneal communication (n = 1).
Meanwhile, PD/HD hybrid therapy was initiated due to difficulty in controlling volume overload and uremic solute retention in both the high (n = 18 and n = 2, respectively) and low (n = 16 and n = 3, respectively) BMI groups.
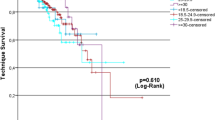
Regarding the median time until complete transition to HD, there was no significant difference between the high and low BMI groups (70.0 vs. 95.4 months, respectively; P = 0.18) (Fig. 2A); however, it is notable that the time until transition to HD and PD/HD hybrid therapy was significantly shorter in the high BMI group than in the low BMI group (38.1 vs. 72.8 months, respectively; P < 0.001) (Fig. 2B). In addition, there was no significant difference in the cumulative incidence of HD transfer between both groups (P = 0.33 by Gray’s test; Fig. 3A), whereas that of the transition to HD and PD/HD hybrid therapy was significantly higher in the high BMI group than in the low BMI group (P < 0.001 by Gray’s test; Fig. 3B).
For multivariate analysis, we separately used the standard Cox regression model and the subdistribution hazard regression model in models 1A, 1B, 2, and 3. High BMI was not associated with HD transfer in any models (Table 2).
On the contrary, Cox regression in models 1A, 1B, 2, and 3 revealed that a high BMI was independently associated with a higher rate of transfer to HD and PD/HD hybrid therapy (HR 2.60, P < 0.001; HR 2.67, P < 0.001; HR 2.74, P < 0.001; and HR 2.40, P = 0.02; respectively) (Table 2). The subdistribution hazard regression models revealed a similar result (HR 1.99, P = 0.009; HR 2.03, P = 0.008; HR 2.01, P = 0.01; and HR 2.02, P = 0.01; respectively) (Table 2).
Impact of high BMI on peritonitis, ESI/TI, and HF-related hospitalization
Peritonitis was observed in 26 (59%) and 29 (38%) patients in the high and low BMI groups, respectively. The peritonitis-free survival time was significantly shorter in the high BMI group than in the low BMI group (35.6 vs. 82.8 months, respectively; P = 0.006) (Fig. 4A). In addition, the cumulative incidence of peritonitis was significantly higher in the high BMI group than in the low BMI group (P = 0.004 by Gray’s test; Fig. 4B). In the multivariate analysis, a higher BMI was independently associated with the development of peritonitis according to Cox regression analysis in models 1A, 1B, 2, and 3 (HR 2.08, P = 0.01; HR 2.10, P = 0.01; HR 2.06, P = 0.02; and HR 2.08, P = 0.01; respectively) (Table 3). The subdistribution hazards in models 1A, 1B, 2, and 3 revealed a similar result regarding high BMI (HR 2.19, P = 0.005; HR 2.18, P = 0.003; HR 2.17, P = 0.008; and HR 2.20, P = 0.006; respectively) (Table 3).
The incidence rate of ESI/TI was 14 (32%) and 13 (17%) in the high and low BMI groups, respectively. The ESI/TI-free survival time was significantly shorter in the high BMI group than in the low BMI group (P = 0.03) (Fig. 5A). The cumulative incidence of ESI/TI was significantly higher in the high BMI group than in the low BMI group (P = 0.03 by Gray’s test; Fig. 5B). In the multivariate analysis, standard Cox regression analysis revealed that a higher BMI was independently associated with the development of ESI/TI in models 1A and 1B (HR 2.64, P = 0.02 and HR 2.68, P = 0.02, respectively), whereas models 2 and 3 exhibited a borderline significant association with a higher risk of ESI/TI (HR 2.20, P = 0.06 and HR 2.20, P = 0.06, respectively) (Table 3). The subdistribution hazards in all models (1A, 1B, 2, and 3) revealed a significant association between a higher BMI and ESI/TI (HR 2.67, P = 0.02; HR 2.74, P = 0.002; HR 2.20, P < 0.05; and HR 2.25, P = 0.04; respectively) (Table 3).
The incidence rates of HF-related hospitalization were 22 (50%) and 31 (41%) in the high and low BMI groups, respectively. The HF-related hospitalization-free survival time did not show a significant difference between the high and low BMI groups (45.2 vs. 72.9 months, respectively; P = 0.09) (Figs. S2A and S2B). In the multivariate analysis, a high BMI was not independently associated with HF-related hospitalization in any models (Table S1).
Discussion
Although the study showed a significant reduction in the time until transition to HD or PD/HD hybrid therapy in obese (Japanese definition) patients [15], it did not show a reduction in the time until transition to HD in such patients. The risk of peritonitis and ESI/TI was also higher in obese patients. These results held true after adjustment for known predictors of PD discontinuation such as age, sex, eGFR, CCI, and DM.
It has been previously reported that older age, sex, DM, CCI, lower RRF, hypoalbuminemia, anemia, and lower exercise capacity were independently associated with a higher technique failure rate [4, 19,20,21,22, 24, 26,27,28,29,30]. In a previous study from Japan, a BMI ≥ 25 kg/m2 in PD patients was reported to be associated with composite outcomes of technique failure and all-cause mortality within 2 years after PD [31]. Additionally, data from a large US dialysis organization indicated that a BMI ≥ 30 kg/m2 in PD patients was associated with shorter time to transition to HD therapy and more frequent peritonitis-related hospitalizations [12]. However, some reports have shown no association between obesity and technique failure or PD-related infection [10, 11]. Thus, no consensus has been reached.
Although there was no significant difference in the time to complete HD transfer between the higher and lower BMI groups in this study, the time to transition to HD and PD/HD hybrid therapy was shorter in the obese group. In most countries, where hybrid therapy is uncommon, patients undergoing PD usually transfer to HD alone on developing fluid overload or insufficient solute removal; however, in Japan, where hybrid therapy is prevalent, patients often shift to PD/HD hybrid therapy first, which allows them to continue PD further and receive PD benefits such as longer and better quality of life. In a previous study, PD/HD hybrid therapy was associated with lower all-cause mortality, cardiovascular mortality, and congestive HF-related mortality compared to PD alone [32]. Another study reported that extracellular water normalized to a patient’s height was the highest in pre-HD sessions followed by PD, PD/HD hybrid therapy, and post-HD patients; thus, PD/HD hybrid therapy is better than PD regarding volume control and is as acceptable as HD even with decreased RRF [33]. Given that obese patients consistently achieve a lower total Kt/V over time despite a greater increase in dialysis Kt/V because of higher total body fluid volume [12], the aggressive use of PD/HD hybrid therapy may offset the disadvantages of PD in obese patients, especially in those with decreased RRF with a high risk of fluid overload and insufficient solute removal [34]. Namely, in Japan, given that PD/HD hybrid therapy is often chosen as an alternative to the transition to HD, obese patients have more opportunities to continue PD as PD/HD hybrid therapy.
In terms of PD-related infections, obesity was shown to be a risk factor for both peritonitis and ESI/TI. Obesity, older age, sex, DM, lower RRF, and depression have been reported as possible risk factors for PD-related peritonitis [23, 35,36,37], and thus, we have adjusted for these factors in the multivariate analysis. High BMI was still significantly associated with PD-related peritonitis and ESI/TI. Especially, considering that the rate of DM was significantly higher in the higher BMI group than that in the lower BMI group, high BMI exerted a negative impact on PD cessation and PD-related infections independent of DM. This result is one of the strengths of our study, considering that not many studies have elucidated the association between obesity and ESI/TI. Potential reasons for the high incidence of infection in obese patients include protracted wound healing, greater difficulties in daily care, and increased susceptibility to skin and soft-tissue infections [38, 39]. Additionally, a high BMI was determined to be a significant predictor of antibiotic prescription failure [39]. Excess body fat may increase the volume of distribution and clearance of antibacterial medications, resulting in less-than-optimal drug concentrations in the blood and tissues [40]. Although knowing the precise association between excess body fat and high BMI was not possible, because we did not systematically assess body composition using bioelectrical impedance analysis or dual-energy X-ray absorptiometry due to the retrospective nature of this study, in general, BMI and percentage of fat are often proportional [41, 42].
The present study has several limitations. First, this was an observational cohort study that did not completely exclude the impact of other potential confounders, although we minimized the effects of covariates by performing multivariate analysis using all known risk factors of technique failure reported in previous studies. Additionally, the study was performed at a single center with a small sample size, which limits generalizability. Second, we used BMI as a measure of obesity similar to other epidemiological studies; however, BMI does not distinguish between muscle mass, fat, and fluids. Hence, PD patients may have fluid overload early during treatment, and changes in fluid volume may have a role in weight changes. To minimize any of these effects, we regarded BNP as one of the measures of the fluid status and added it as an independent variable in the multivariate analysis as model 3, which yielded similar results to those of models 1 and 2. Finally, race and socioeconomic status were not investigated nor analyzed; however, all participants were Japanese and had health insurance through the Japanese insurance system, which made the patient backgrounds similar.
In conclusion, we found that a BMI ≥ 25 kg/m2 was an independent risk factor for transition to HD and PD/HD hybrid therapy, peritonitis, and ESI/TI in Japan, whereas the time for HD transfer was not associated with obesity. In particular, in Japan, where hybrid therapy is prevalent and is often chosen as an alternative to complete HD transfer, obese patients have more options to avoid an early transition to HD alone, similar to non-obese patients. These results indicate that PD induction should not necessarily be avoided in obese patients. PD/HD hybrid therapy may be a useful option for obese patients to forego early complete HD transfer, but further studies will be necessary and warranted to confirm whether successful weight reduction enhances the survival advantage of obese patients undergoing PD while reducing PD-related infections.
References
Nitta K, Goto S, Masakane I et al (2020) Annual dialysis data report for 2018, JSDT renal data registry: survey methods, facility data, incidence, prevalence, and mortality. Ren Replace Ther. https://doi.org/10.1186/s41100-020-00286-9
Jaar BG, Plantinga LC, Crews DC et al (2009) Timing, causes, predictors and prognosis of switching from peritoneal dialysis to hemodialysis: a prospective study. BMC Nephrol 10:3. https://doi.org/10.1186/1471-2369-10-3
Guo A, Mujais S (2003) Patient and technique survival on peritoneal dialysis in the United States: evaluation in large incident cohorts. Kidney Int. https://doi.org/10.1046/j.1523-1755.2003.08801.x
Huisman RM, Nieuwenhuizen MG, de Charro Th, F, (2002) Patient-related and centre-related factors influencing technique survival of peritoneal dialysis in the Netherlands. Nephrol Dial Transplant 17:1655–1660. https://doi.org/10.1093/ndt/17.9.1655
Johnson DW, Herzig KA, Purdie DM et al (2000) Is obesity a favorable prognostic factor in peritoneal dialysis patients? Perit Dial Int 20:715–721. https://doi.org/10.1177/089686080002000623
Aslam N, Bernardini J, Fried L, Piraino B (2002) Large body mass index does not predict short-term survival in peritoneal dialysis patients. Perit Dial Int 22:191–196. https://doi.org/10.1177/089686080202200205
McDonald SP, Collins JF, Johnson DW (2003) Obesity is associated with worse peritoneal dialysis outcomes in the Australia and New Zealand patient populations. J Am Soc Nephrol 14:2894–2901. https://doi.org/10.1097/01.asn.0000091587.55159.5f
Snyder JJ, Foley RN, Gilbertson DT, Vonesh EF, Collins AJ (2003) Body size and outcomes on peritoneal dialysis in the United States. Kidney Int 64:1838–1844. https://doi.org/10.1046/j.1523-1755.2003.00287.x
Abbott KC, Glanton CW, Trespalacios FC et al (2004) Body mass index, dialysis modality, and survival: analysis of the United States renal data system dialysis morbidity and mortality wave II study. Kidney Int 65:597–605. https://doi.org/10.1111/j.1523-1755.2004.00385.x
Johansen KL, Young B, Kaysen GA, Chertow GM (2004) Association of body size with outcomes among patients beginning dialysis. Am J Clin Nutr 80:324–332. https://doi.org/10.1093/ajcn/80.2.324
de Mutsert R, Grootendorst DC, Boeschoten EW, Dekker FW, Krediet RT (2009) Is obesity associated with a survival advantage in patients starting peritoneal dialysis? Contrib Nephrol 163:124–131. https://doi.org/10.1159/000223790
Obi Y, Streja E, Mehrotra R, Rivara MB, Rhee CM, Soohoo M et al (2018) Impact of obesity on modality longevity, residual kidney function, peritonitis, and survival among incident peritoneal dialysis patients. Am J Kidney Dis 71:802–813. https://doi.org/10.1053/j.ajkd.2017.09.010
Shibagaki Y, Faber MD, Divine G, Shetty A (2002) Feasibility of adequate solute clearance in obese patients on peritoneal dialysis: a cross-sectional study. Am J Kidney Dis 40:1295–1300. https://doi.org/10.1053/ajkd.2002.36904
Yoshiike NWN, Matsushima S, Ito C et al (2000) Obese degree and diabetes, hypertension based on body mass index, epidemiological examination - by associated - multicenter study with the risk factor of hyperlipidemia. J Japan Soc Study Obes 6:4–17
Kawanishi H, Marshall MR, Zhao J et al (2021) Mortality, hospitalization and transfer to haemodialysis and hybrid therapy, in Japanese peritoneal dialysis patients. Perit Dial Int. https://doi.org/10.1177/08968608211016127
Kang SH, Cho KH, Park JW, Yoon KW, Do JY (2013) Geriatric nutritional risk index as a prognostic factor in peritoneal dialysis patients. Perit Dial Int 33:405–410. https://doi.org/10.3747/pdi.2012.00018
Figueiredo A, Goh BL, Jenkins S et al (2010) Clinical practice guidelines for peritoneal access. Perit Dial Int 30:424–429. https://doi.org/10.3747/pdi.2010.00087
Nakayama M, Miyazaki M, Honda K et al (2014) Encapsulating peritoneal sclerosis in the era of a multi-disciplinary approach based on biocompatible solutions: the NEXT-PD study. Perit Dial Int 34:766–774. https://doi.org/10.3747/pdi.2013.00074
Kolesnyk I, Dekker FW, Boeschoten EW, Krediet RT (2010) Time-dependent reasons for peritoneal dialysis technique failure and mortality. Perit Dial Int 30:170–177. https://doi.org/10.3747/pdi.2008.00277
Chidambaram M, Bargman JM, Quinn RR, Austin PC, Hux JE, Laupacis A (2011) Patient and physician predictors of peritoneal dialysis technique failure: a population based, retrospective cohort study. Perit Dial Int 31:565–573. https://doi.org/10.3747/pdi.2010.00096
See EJ, Johnson DW, Hawley CM et al (2018) Risk predictors and causes of technique failure within the first year of peritoneal dialysis: an Australia and New Zealand dialysis and transplant registry (ANZDATA) study. Am J Kidney Dis 72:188–197. https://doi.org/10.1053/j.ajkd.2017.10.019
Boundville N, Ullah S, Clayton P et al (2019) Differences in peritoneal dialysis technique survival between patients treated with peritoneal dialysis systems from different companies. Nephrol Dial Transplant 34:1035–1044. https://doi.org/10.1093/ndt/gfy340
Cho Y, Johnson DW (2014) Peritoneal dialysis-related peritonitis: towards improving evidence, practices, and outcomes. Am J Kidney Dis 64:278–289. https://doi.org/10.1053/j.ajkd.2014.02.025
Nakayama T, Uchiyama K, Washida N et al (2021) Exercise parameters predict technique survival in patients on peritoneal dialysis. Blood Purif 50:380–389. https://doi.org/10.1159/000511293
Kanda Y (2013) Investigation of the freely available easy-to-use software “EZR” for medical statistics. Bone Marrow Transplant 48:452–458. https://doi.org/10.1038/bmt.2012.244
Isla RA, Mapiye D, Swanepoel CR, Rozumyk N, Hubahib JE, Okpechi IG (2014) Continuous ambulatory peritoneal dialysis in Limpopo province, South Africa: Predictors of patient and technique survival. Perit Dial Int 34:518–525. https://doi.org/10.3747/pdi.2013.00334
Descoeudres B, Koller MT, Garzoni D et al (2008) Contribution of early failure to outcome on peritoneal dialysis. Perit Dial Int 28:259–267. https://doi.org/10.1177/089686080802800312
Cueto-Manzano AM, Quintana-Piña E, Correa-Rotter R (2001) Long-term CAPD survival and analysis of mortality risk factors: 12-year experience of a single Mexican center. Perit Dial Int 21:148–153. https://doi.org/10.1177/089686080102100207
Chen HL, Tarng DC, Huang LH (2019) Risk factors associated with outcomes of peritoneal dialysis in Taiwan: an analysis using a competing risk model. Med (Baltim) 98:e14385. https://doi.org/10.1097/MD.0000000000014385
Shi Y, Zheng D, Zhang L et al (2017) Six-minute walk test predicts all-cause mortality and technique failure in ambulatory peritoneal dialysis patients. Nephrology (Carlton) 22:118–124. https://doi.org/10.1111/nep.12726
Matsui M, Akai Y, Samejima KI et al (2017) Prognostic value of predialysis indices for technique failure and mortality in peritoneal dialysis patients. Ther Apher Dial 21:493–499. https://doi.org/10.1111/1744-9987.12546
Murashima M, Hamano T, Abe M, Masakane I (2021) Combination of once-weekly haemodialysis with peritoneal dialysis is associated with lower mortality compared with peritoneal dialysis alone: a longitudinal study. Clin Kidney J 14:1610–1617. https://doi.org/10.1093/ckj/sfaa173
Tanaka M, Ishibashi Y, Hamasaki Y et al (2020) Bioimpedance spectroscopy-based fluid status in combined dialysis compared with hemodialysis and peritoneal dialysis: a cross-sectional study. Ther Apher Dial 24:373–379. https://doi.org/10.1111/1744-9987.13444
Wang AY (2007) The john F. Maher award recipient Lecture 2006. The “heart” of peritoneal dialysis: residual renal function. Perit Dial Int 27:116–124. https://doi.org/10.1177/089686080702700203
Ozener C, Arikan H, Karayaylali I et al (2014) The impact of diabetes mellitus on peritoneal dialysis: the Turkey multicenter clinic study. Ren Fail 36:149–153. https://doi.org/10.3109/0886022X.2013.843275
Nessim SJ, Bargman JM, Austin PC, Nisenbaum R, Jassal SV (2009) Predictors of peritonitis in patients on peritoneal dialysis: results of a large, prospective Canadian database. Clin J Am Soc Nephrol 4:1195–1200. https://doi.org/10.2215/CJN.00910209
Tsai CC, Lee JJ, Liu TP, Ko WC, Wu CJ, Pan CF et al (2013) Effects of age and diabetes mellitus on clinical outcomes in patients with peritoneal dialysis-related peritonitis. Surg Infect (Larchmt) 14:540–546. https://doi.org/10.1089/sur.2012.195
Conway EL, Sellick JA, Kurtzhalts K, Mergenhagen KA (2017) Obesity and heart failure as predictors of failure in outpatient skin and soft tissue infections. Antimicrobial Agents Chemother. https://doi.org/10.1128/AAC.02389-16
Falagas ME, Kompoti M (2006) Obesity and infection. Lancet Infect Dis 6:438–446. https://doi.org/10.1016/S1473-3099(06)70523-0
Long C, Bartlett G, Macgibbon B et al (2013) The effect of obesity on antibiotic treatment failure: a historical cohort study. Pharmacoepidemiol Drug Saf 22:970–976. https://doi.org/10.1002/pds.3461
Gallagher D, Heymsfield SB, Heo M, Jebb SA, Murgatroyd PR, Sakamoto Y (2000) Healthy percentage body fat ranges: an approach for developing guidelines based on body mass index. Am J Clin Nutr 72:694–701. https://doi.org/10.1093/ajcn/72.3.694
Alves Junior CA, Mocellin MC, Gonçalves ECA, Silva DA, Trindade EB (2017) Anthropometric indicators as body fat discriminators in children and adolescents: a systematic review and meta-analysis. Adv Nutr 8:718–727. https://doi.org/10.3945/an.117.015446
Funding
None.
Author information
Authors and Affiliations
Contributions
KU designed the study, and EY wrote the initial draft of the manuscript. EY, KU, TN, EK, TN, IY, KM, and NW contributed to data collection. EY and KU contributed to analysis and interpretation of data and assisted in the preparation of the manuscript. KM, NW, and HI supervised the manuscript. All authors have approved the final version of the manuscript and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
All the authors have no conflicts of interest to declare.
Ethical approval
This study and all its protocols were reviewed and approved by the ethics committee of our hospital, and informed consent was obtained from all patients prior to participation.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Hama, E.Y., Uchiyama, K., Nagasaka, T. et al. High body mass index is a risk factor for transition to hemodialysis or hybrid therapy and peritoneal dialysis-related infection in Japanese patients undergoing peritoneal dialysis. Int Urol Nephrol 54, 3193–3202 (2022). https://doi.org/10.1007/s11255-022-03252-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-022-03252-y