Abstract
Background
Sarcopenia and chronic kidney disease (CKD) have been associated with negative outcomes in older people, including inflammatory profile and anemia biomarkers.
Aims
To investigate the effects of pre-dialysis resistance training (RT) on sarcopenia, inflammatory profile, and anemia biomarkers in older patients with CKD.
Methods
A total of 107 patients with CKD (65.4 ± 3.7 years) were randomly allocated into four groups: sarcopenic RT (n = 37), non-sarcopenic RT (n = 20), sarcopenic control (n = 28), and non-sarcopenic control (n = 22). DXA and handgrip strength were used to classify sarcopenia according to EWGSOP-2. Treatment groups underwent a 24-week intervention with RT before each dialysis session, three times per week. Blood sample analysis for ferritin, hepcidin, iron availability, and inflammatory profile (TNFα, IL-6, and IL-10) was conducted. All-cause mortality was recorded over 5 years.
Results
Sarcopenic RT group increased iron availability after the intervention, while their counterparts decreased. Ferritin and hepcidin significantly decreased in sarcopenic RT group. RT elicited a reduction in both TNFα and IL-6, while increasing IL-10 in both intervention groups. The rate of sarcopenic subjects substantially decreased after the intervention period (from 37 to 17 in the RT group; p = 0.01). The proportion of deaths was higher (P = 0.033) for sarcopenic subjects (Controls 35.7% vs RT 29.7%) when compared to non-sarcopenic subjects (Controls 18% vs RT 10%). The proportion of deaths decreased according to the randomization group (X2 = 8.704; P < 0.1).
Conclusions
The 24-week RT intervention elicited a better sarcopenia status, better inflammatory profile, and improved anemia biomarkers. Sarcopenia was associated with higher mortality rate in older patients with CKD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic kidney disease (CKD) is a progressive and irreversible disease of kidney function [1], which has been recognized as an important health concern. In fact, it is associated with an increased risk of mortality and negative health-related outcomes [2,3,4]. It is estimated that 15% of the worldwide population is affected by CKD [2]. In the United States, a recent estimate of CKD-related illness amounted to annual health care costs of nearly $20,000 per patient [5]. CKD has been one of the focuses of healthcare efforts, in the past 2 decades as its global prevalence has grown to around 87%, while the death rate rose by 98% [6]. It is known that aged people are more susceptible to CKD when compared to other age groups, being its prevalence higher than triple of young populations [7].
World population aging has been recognized as one of the most critical health challenges of the current century [8]. A salient feature of the aging includes loss of skeletal muscle mass, being that the muscle health conditions represent a global threat to healthy aging [9]. The significant decrease of muscle mass and strength is recognized as sarcopenia [10], and has been linked to multiple adverse outcomes among the aging population [11, 12]. Although sarcopenia is recognized as an emerging health problem, an agreement on its classification has been widely discussed in recent years [10, 13]. In this sense, the European Working Group on Sarcopenia in Older People (EWGSOP) was created and recently updated to provide a consensual, practical definition to implement in the clinical setting [10, 13]. Traits of sarcopenia (i.e., low muscle mass and poor muscle strength) are frequently observed in CKD patients, and have been related to a higher risk of morbidity and mortality in this population [14].
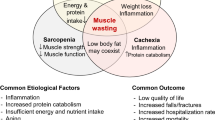
The negative effects for the coexistence of CKD and sarcopenia have been investigated because both muscle wasting and loss of strength have been linked to mortality [15,16,17,18], and these conditions are highly prevalent in patients with CKD [14, 15, 18,19,20]. In addition, it is known that anemia is an important condition for the rate of deaths among CKD patients [21, 22], which can be aggravated by a decrease in muscle mass and strength [23,24,25]. Important factors that might mediate the relationship between anemia and cardiovascular disease with CKD patients mortality are the unregulated inflammatory profile and low iron availability [26, 27]. Recent efforts have been carried out to determine non-pharmacological interventions to decrease inflammation and up-regulate iron-related signaling in CKD patients [26, 27].
Among interventions known to improve health in older patients with CKD, resistance training (RT) has shown to be beneficial for counteracting sarcopenia as well as up-regulating the inflammatory profile and iron availability [26, 28, 29]. However, most of the clinical trials available in the field have conducted RT protocols during the dialysis sessions [30, 31]. Noteworthy, there are investigations that have used exercise training before dialysis, but not systematically in all participants as some patients within studies perform their exercises after hemodialysis [32]. In addition, this might have limited the RT prescription due to the possible reduced number of exercises (usually unilateral, single-joint, and fixed-form), the discomfort caused by the fistula, and the safety of the training itself. It could be important to explore the effects of RT conducted immediately before the dialysis, when the intervention may be more properly performed and exploit its full beneficial potential [33,34,35].
To the best of our knowledge, there is a lack in literature regarding the effects of RT conducted before the dialysis session in older patients with CKD on sarcopenia, inflammatory profile, and anemia biomarkers. Therefore, the present study aimed (i) to investigate the effects of pre-dialysis RT on sarcopenia, inflammatory profile, and anemia biomarkers in older community-dwelling patients with CKD; and (ii) to describe the rate of mortality over 5 years after interventions.
Methods
Participants
One hundred and seven patients undergoing maintenance phase hemodialysis volunteered for this study. Eligibility criteria for participants were: (i) age equal to or older than 60 years; (ii) hemodialysis for at least 3 months; (iii) dialysis at least three times per week; and (iv) no significant medical complications in the last 3 months, except for vascular access correction. Exclusion criteria were: (i) recent acute myocardial infarction (within the past 3 months) or unstable angina; (ii) systemic lupus erythematosus; (iii) congenital kidney malformation or some auto-immune disease that affects the kidneys; (iv) osteoarticular complications that could compromise physical exercise; (v) decompensated heart failure that could limit participation in training; (vi) severe decompensated diabetes; or (vii) severe neuropathy, retinopathy, or diabetic nephropathy.
All participants were informed about the study procedures and voluntarily signed an informed consent form. All experiments on human subjects were conducted under the Declaration of Helsinki, and the study protocol was previously approved by the Institutional Review Board (08856012.6.0000.5505 and updated 23007319.0.0000.0029). This study was recorded in the Brazilian clinical trials registration website (URL: http://www.ensaiosclinicos.gov.br/rg/RBR-3gpg5w/, protocol number: RBR3gpg5w), and in the World Health Organization international clinical trial registry platform (URL: http://apps.who.int/trialsearch/utn.aspx, protocol number U1111-1237-8231).
Study design
The flowchart of the trial is presented in Fig. 1. Participants were divided into two groups according to the EWGSOP-2 sarcopenia definition [10]. The non-sarcopenic patients (n = 42) were then randomized into two groups, the non-sarcopenic controls (n = 22) and non-sarcopenic RT (n = 20). The same procedure was performed for the sarcopenic group (n = 65), which was randomized in sarcopenic controls (n = 28) and sarcopenic RT (n = 37). The randomization was conducted individually using an automated tool (http://www.randomization.com). The researcher doing the randomization process was not involved in the participants’ treatment. All patients received the same recommendations from a multidisciplinary team: nutritionist, psychologist, social worker, nurse, pharmacist, and nephrologist. After training period, patients were tracked over 5 years during their dialysis treatment and were included in the final analysis to investigate the associate between sarcopenia and rate of mortality in patients with CKD.
Anthropometric and body composition assessments
All subjects were weighed on a mechanical scale (Filizola®, São Paulo, Brazil), and height was measured with a stadiometer built into the scale. Body mass index was calculated, dividing body weight by the height squared (kg/m2). Body composition was measured using a Prodigy Advance Plus (LUNAR, Corp/General Electric; Madison, Wisconsin, USA) dual-energy X-ray absorptiometry (DXA) according to procedures specified elsewhere [29]. Briefly, participants laid face up on the DXA table with body centered. The software provided measures of fat-free mass for whole body.
Handgrip strength
Handgrip strength was measured with a hydraulic hand dynamometer (Jamar®—Sammons Preston, Bolingbrook, USA), according to the American Society of Hand Therapists’ recommendations [36]. Measurements were performed with participants in sitting position, elbow joint at 90°, forearm in a neutral position, and wrist between 0° and 30° of extension. The best performance of three trials in the contralateral arm of arteriovenous fistula was recorded and used for the present analyses.
Sarcopenia classification
Sarcopenia was defined according to the EWGSOP-2 recommendations [10]. Briefly, this classification considered results from both muscle strength (i.e., handgrip strength) and body composition [i.e., fat-free mass divided by height squared (fat-free mass index, FFMI)] assessments. Given the high specificity presented by this sample (sarcopenic and/or CKD patients) for muscle mass, the lowest tertile of FFMI was classified as low muscle mass [37, 38]. The cut-points for the FFMI were 15.3 and 15.6 kg/m2 for men and women, respectively. Cut-points for the handgrip strength were 30 kg and 20 kg for men and women, respectively [39]. The sarcopenia condition was characterized by the simultaneous presence of low handgrip strength and low FFMI.
Resistance training protocol
Subjects allocated in the intervention groups took part in a 24-week RT program. Before the training period, participants underwent through three familiarization sessions over a week. The RT program was performed three times per week for 24 weeks, 1 h previous the hemodialysis and each training session took approximately 40 min. The protocol was conducted immediately before each dialysis session. It involved the following exercises: chest press, squat, unilateral row, unilateral knee extension, unilateral knee flexion, unilateral shoulder press, hip thrust, biceps curl, unilateral hip adduction, unilateral hip abduction, elbow extension with dumbbells, and seated calf raise. The e-Lastic cable was used to perform the chest press, unilateral row, unilateral hip adduction, and unilateral hip abduction exercises [the e-Lastic load record was the peak (maximum) load achieved in each movement to count the repetitions]. Dumbbells were used for the performance of the shoulder press, biceps curl, and elbow extension. Weighted cuffs were used for the knee extension (wrapped at the ankle), knee flexion (wrapped at the ankle), hip thrust (positioned at the hips), and seated calf raise (wrapped across the quadriceps). In the squat exercise, due to the fragility of the lower limbs of hemodialysis patients, we chose to use only bodyweight to perform the squat exercise with just four repetitions at the beginning of the protocol. For upper-limb exercises, we prioritized unilateral exercises as a conservative measure to preserve arteriovenous fistula. Training loads were monitored and adjusted using the OMNI rating of perceived exertion (RPE) scale [40]. Initially, participants trained with a load corresponding to 8 repetitions at an RPE scale of 5–6 for the first 12 weeks, and 7–8 over the final 12 weeks. When the RPE indicated the load was too easy, the number of repetitions was first increased. If the participant exceeded 12 repetitions, then the load was increased. Each exercise was performed in 3 sets with approximately 2-min rest between the sets. All training sessions were supervised by experienced professionals. Moreover, except for the implementation of the RT program, all patients (controls and RT) were asked to maintain their habitual physical activity throughout the study.
Functional performance
Functional performance was measured by the Timed Up-and-Go test (TUG) (Mathias, Nayak, and Isaacs, 1986). Procedures were fully explained before the assessment, followed by a familiarization attempt. Briefly, volunteers were individually seated in a standard chair with 45 cm of height, with the back against the chair, both arms resting along the body, and both feet completely resting on the floor. Participants were instructed to get up and walk 2 m forward, as fast as possible, turn around an obstacle, return to the chair, and sit down again. Three attempts with 60 s of rest between them were timed. The best performance was recorded and used for the present analyses.
Ascertainment of deaths
All-cause mortality events were recorded over 5 years. In summary, as a clinic routine procedure, every single outflow was monitored regarding transplantations, deaths, or change of clinic for 5 years after RT protocol.
Statistical analysis
The primary outcome of the present study was the effect of RT on inflammatory and anemia biomarkers in sarcopenic CKD patients. The secondary outcome was the effect of RT on body composition, handgrip strength, and functional performance. In addition, the present study also described the rate of mortality over 5 years after interventions. Descriptive characteristics are presented as means and standard deviations unless otherwise noted. The Shapiro–Wilk test and Levene were used to verify data distribution nature and homogeneity, respectively. X2 tests were performed to compare categorical variables, while continuous variables were tested for significance by performing a multivariate two-way mixed analysis of variance [2 × 2 groups (sarcopenic and non-sarcopenic) × treatments (Control and RT)]. Kruskal–Wallis test and Dunns’ multiple comparison analysis were applied when necessary. Results were considered significant at P < 0.05, and all statistical analyses were performed using SPSS 20.0 (SPSS Inc., Chicago, United States of America).
Results
The baseline characteristics of the participants are presented in Table 1. The prevalence of sarcopenia was 60.7% (95% confidence interval, 95% CI 50.5–70.1), and no differences for handgrip strength were observed among the groups (Table 1).
Changes in the traits of sarcopenia, functional variables, and renal and profiles of the participants after the RT are presented in Table 2. Handgrip strength increased after the RT program, regardless of sarcopenia. TUG and body fat mass significantly improved (Table 2).
Sarcopenic patients allocated in the RT group increased iron after the training period (24-week intervention), meanwhile their counterparts decreased (P < 0.05). On the other hand, ferritin and hepcidin significantly decreased for sarcopenic subjects submitted to RT program (Fig. 2). RT elicited similar responses in both groups (non-sarcopenic and sarcopenic) promoting a reduction in both TNFα and IL-6, while increasing IL-10 and its ratios (Fig. 3).
Figure 4 presents the prevalence of sarcopenic and non-sarcopenic patients according to each group, before and after the intervention. Considering all subjects allocated into the intervention groups, the number of sarcopenic patients substantially decreased after the RT program (from 37 to 17; P = 0.01). No differences were observed for what concerns the prevalence of sarcopenia in the Control Group.
Death events over the 5-year period of follow-up according to groups are presented in Fig. 5. The overall deaths rate was 25.2% (95% CI 16.8–33.6). It was observed that the proportion of deaths was higher for sarcopenic subjects (Control n = 35.7% vs RT n = 29.7%) compared to non-sarcopenic subjects (Control n = 18% vs RT n = 10%). Mortality was lower in those who had been included in the RT group (P = 0.03; Fig. 5).
Prevalence of men was 52.4% and 75.4% (P = 0.01) among non-sarcopenic and sarcopenic subjects, respectively. The prevalence of diabetes was higher for non-Sarcopenic when compared to sarcopenic subjects (71.4% vs 30.8%; χ2 = 16.94; P < 0.0001), while no differences were found for smoking status (23.8% vs 21.5%; χ2 = 0.076; P = 0.783). No differences were found for the following medicines: ACE inhibitors, AT1R antagonist, Statins, Anti-hyponitic, Anti-depressive, Erythropoietin, and Ferrous sulfate (χ2 < 3.92; all P > 0.05). All participants were hypertensive.
Discussion
This randomized controlled trial sought to investigate the chronic health benefits of RT immediately conducted before the dialysis session in older patients with CKD. In our study, RT positively influenced traits of sarcopenia also reducing the prevalence of sarcopenia in older subjects with CKD. Furthermore, subjects submitted to pre-dialysis RT positively increased iron status, while reducing ferritin, hepcidin, TNFα, and IL-6. It is noteworthy that the sarcopenic group presented higher all-cause mortality rates over 5 years.
Sarcopenia is defined as the progressive decline of skeletal muscle mass and strength that occurs with advancing age [10]. Muscle wasting and loss of strength are prevalent in patients with CKD [14, 19], which has a multifactorial cause. The current findings revealed that the RT administered immediately before dialysis positively influenced both muscle strength and mass in older people with CKD. An increase in muscle mass might be attributed to either a decrease in protein degradation, or an increase in protein synthesis, which might explain CKD-induced skeletal muscle modifications [14]. It is expected that RT improves protein signaling synthesis, which favors the process of increasing muscle mass and strength [41]. In addition, neuromuscular responses imposed by RT may explain the increase in muscle strength [42]. Even though it is well established that RT can positively influence neuromuscular and metabolic aspects of aged people, including CKD [42, 43], to the best of our knowledge, there are no previous studies that have investigated the effects of RT before dialysis sessions on sarcopenia in CKD patients.
Evidence has already demonstrated the benefits of RT on muscle mass and strength in the persons with CKD [26, 42]. However, most clinical trials have administered the RT protocol during the dialysis session [30, 31]. Despite the emerging interest in managing RT during the dialysis session, it can make the prescription of training limited due to the reduced number of exercises (usually unilateral, single-joint, and fixed-form), the discomfort caused by the fistula, and the training safety itself. In this sense, further research should explore exercise prescriptions immediately before dialysis due to their potential for proper full-body training. Moreover, according to the movement specificity theory, it is postulated that the closer movement patterns during RT are to the desired activity (i.e., free weight and full-body exercise are closer to daily living activities), greater will be the functional gains; hence, RT has been presented to be highly effective in improving performance and functionality in different populations [33,34,35]. Thus, prescribing RT immediately before dialysis can provide a broader range of exercises (including full-body and free weights), increasing the possibility of functional transfer to activities of daily living.
In addition to the aforementioned neuromuscular gains, sarcopenic subjects with CKD had iron status positively modified, while their counterparts were negatively modified. Noteworthy, iron supplements were equally distributed across the four groups. In general, older subjects with CKD present low iron availability [23, 44], which has been linked to an increased risk of anemia [25]. It can be explained by a decreased glomerular filtration rate leading to inadequate production of erythropoietin for erythropoiesis and, consequently, iron deficiency [26, 45]. In addition, very low iron availability and anemia conditions have been associated with higher levels of inflammatory markers [46, 47], inducing a negatively impact on sarcopenia [48,49,50].
The RT protocol also promoted a decrease in ferritin, hepcidin, and inflammatory markers (TNF-α and IL-6). Recently, Ray et al. [26] showed that a 24 week RT led to an increase in iron bioavailability, a decrease in hepcidin levels, and an improvement of the inflammatory profile (increasing IL-10 levels; decreasing TNF-α and IL-6) in older individuals with end-stage renal disease. Thus, as related in the previously mentioned study, the improvement in iron levels can be justified by the decrease of hepcidin, a bioregulator of cellular iron efflux [26, 51]. In addition to iron status, hepcidin is also stimulated by pro-inflammatory cytokines via Janus kinase/signal transducers and activators of transcription-3 signaling [24], especially by IL-6. Of note, hepcidin expression has been strongly linked to the inflammatory process; thus, the improvement of the inflammatory profile influenced by the RT protocol may explain its reduction [24].
In the present study, sarcopenic subjects presented higher mortality rates when compared to their counterparts, regardless of exercise intervention. However, the subgroup undergoing the RT protocol presented a lower mortality rate. Although the present study recorded only all-cause mortality, it is reported that most deaths among CKD patients have been linked to cardiovascular diseases. Furthermore, iron deficiency has also been linked to higher cardiovascular risk factors [52]. Thus, we speculate that the lack of responsiveness to an increase in iron from sarcopenic subjects who did not undergo the RT protocol might be an indicator for a higher mortality rate in this group. Moura et al. [26] demonstrated that RT up-regulated iron availability among CKD patients, and this effect might be important in the management of anemia and cardiovascular complications in this population [21, 53].
The current study has several strengths and limitations. The strengths are RT protocol immediately before the dialysis, objective measurements of sarcopenia, and the many biomarkers related to CKD. A limitation of the present study could be found in the low internal validity of the load progression during the 24-week RT protocol. However, our findings demonstrated that the RT protocol was effective for both strength and lean mass gains, demonstrating an opportunity with high ecological validity. The study sample was composed of functionally independent community-dwelling older people with CKD, so the results may not apply to frailer individuals. A relatively high number of participants dropped out (RT = 20.8% and Control = 25.4) and were excluded from the present analysis. However, participants who quit the project were checked for similarity to those who completed the 24-week follow-up at the baseline analysis and no differences were found. Moreover, food intake, especially regarding protein consumptions was not controlled in the present analysis. Finally, the present study did not perform a sample size calculation, thus, we recognize it as a potential limitation of the present study and encourage further studies to control the aforementioned topics.
Conclusion
In summary, a 24-week program of RT administrated before dialysis promoted clinical and biological benefits in older patients with CKD, especially in terms of muscle health, inflammatory profile, and anemia biomarkers. Sarcopenia was also associated with higher mortality rate in older patients with CKD. Further studies are needed to confirm and extend our findings, in particular, to find ways for large-scale implementation of physical activity protocols in patients with CKD.
References
Levey AS, Coresh J (2012) Chronic kidney disease. Lancet 379(9811):165–180. https://doi.org/10.1016/S0140-6736(11)60178-5
Levin A, Tonelli M, Bonventre J, Coresh J, Donner J-A, Fogo AB, Fox CS, Gansevoort RT, Heerspink HJ, Jardine M (2017) Global kidney health 2017 and beyond: a roadmap for closing gaps in care, research, and policy. The Lancet 390(10105):1888–1917
Masson P, Webster AC, Hong M, Turner R, Lindley RI, Craig JC (2015) Chronic kidney disease and the risk of stroke: a systematic review and meta-analysis. Nephrol Dial Transplant 30(7):1162–1169
Webster AC, Nagler EV, Morton RL, Masson P (2017) Chronic kidney disease. The Lancet 389(10075):1238–1252
Takemoto Y, Naganuma T (2019) Economic issues of chronic kidney disease and end-stage renal disease. In: CKD-Associated Complications: Progress in the Last Half Century. Karger Publishers 198. pp 87–93
Xie Y, Bowe B, Mokdad AH, Xian H, Yan Y, Li T, Maddukuri G, Tsai C-Y, Floyd T, Al-Aly Z (2018) Analysis of the global burden of disease study highlights the global, regional, and national trends of chronic kidney disease epidemiology from 1990 to 2016. Kidney Int 94(3):567–581
Mallappallil M, Friedman EA, Delano BG, McFarlane SI, Salifu MO (2014) Chronic kidney disease in the elderly: evaluation and management. Clinical Practice (London, England) 11(5):525
Organization WH (2015) World report on ageing and health. World Health Organization,
Briggs AM, Cross MJ, Hoy DG, Sanchez-Riera L, Blyth FM, Woolf AD, March L (2016) Musculoskeletal health conditions represent a global threat to healthy aging: a report for the 2015 World Health Organization world report on ageing and health. The Gerontologist 56(suppl_2):S243–S255
Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyère O, Cederholm T, Cooper C, Landi F, Rolland Y, Sayer AA (2019) Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing 48(1):16–31
Tanimoto Y, Watanabe M, Sun W, Sugiura Y, Hayashida I, Kusabiraki T, Tamaki J (2014) Sarcopenia and falls in community-dwelling elderly subjects in Japan: defining sarcopenia according to criteria of the European working group on sarcopenia in older people. Arch Gerontol Geriatr 59(2):295–299
Gadelha AB, Neri SGR, Bottaro M, Lima RM (2018) The relationship between muscle quality and incidence of falls in older community-dwelling women: an 18 month follow-up study. Exp Gerontol 110:241–246. https://doi.org/10.1016/j.exger.2018.06.018
Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, Martin FC, Michel JP, Rolland Y, Schneider SM, Topinkova E, Vandewoude M, Zamboni M (2010) Sarcopenia: European consensus on definition and diagnosis: report of the European working group on sarcopenia in older people. Age Ageing 39(4):412–423. https://doi.org/10.1093/ageing/afq034
Watanabe H, Enoki Y, Maruyama T (2019) Sarcopenia in chronic kidney disease: factors, mechanisms, and therapeutic interventions. Biol Pharm Bull 42(9):1437–1445
Androga L, Sharma D, Amodu A, Abramowitz MK (2017) Sarcopenia, obesity, and mortality in US adults with and without chronic kidney disease. Kidney Int Rep 2(2):201–211
Li R, Xia J, Zhang X, Gathirua-Mwangi WG, Guo J, Li Y, McKenzie S, Song Y (2018) Associations of muscle mass and strength with all-cause mortality among US older adults. Med Sci Sports Exerc 50(3):458
Pereira RA, Cordeiro AC, Avesani CM, Carrero JJ, Lindholm B, Amparo FC, Amodeo C, Cuppari L, Kamimura MA (2015) Sarcopenia in chronic kidney disease on conservative therapy: prevalence and association with mortality. Nephrol Dial Transplant 30(10):1718–1725
Ziolkowski SL, Long J, Baker JF, Chertow GM, Leonard MB (2019) Relative sarcopenia and mortality and the modifying effects of chronic kidney disease and adiposity. J Cachexia, Sarcopenia Muscle 10(2):338–346
Carrero JJ, Chmielewski M, Axelsson J, Snaedal S, Heimbürger O, Bárány P, Suliman ME, Lindholm B, Stenvinkel P, Qureshi AR (2008) Muscle atrophy, inflammation and clinical outcome in incident and prevalent dialysis patients. Clin Nutr 27(4):557–564
Moorthi RN, Avin KG (2017) Clinical relevance of sarcopenia in chronic kidney disease. Curr Opin Nephrol Hypertens 26(3):219
Agarwal R, Kusek JW, Pappas MK (2015) A randomized trial of intravenous and oral iron in chronic kidney disease. Kidney Int 88(4):905–914
Rocco MV, Cheung AK, Greene T, Eknoyan G (2005) The HEMO study: applicability and generalizability. Nephrol Dial Transplant 20(2):278–284
McClellan W, Aronoff SL, Bolton WK, Hood S, Lorber DL, Tang KL, Tse TF, Wasserman B, Leiserowitz M (2004) The prevalence of anemia in patients with chronic kidney disease. Curr Med Res Opin 20(9):1501–1510
Ueda N, Takasawa K (2018) Impact of inflammation on ferritin, hepcidin and the management of iron deficiency anemia in chronic kidney disease. Nutrients 10(9):1173
Wong MM, Tu C, Li Y, Perlman RL, Pecoits-Filho R, Lopes AA, Narita I, Reichel H, Port FK, Sukul N (2019) Anemia and iron deficiency among chronic kidney disease Stages 3–5ND patients in the chronic kidney disease outcomes and practice patterns study: often unmeasured, variably treated. Clin Kidney J 13(3):269–273. https://doi.org/10.1093/ckj/sfaa102
Moura SRG, Corrêa HL, Neves RVP, Santos CAR, Neto LSS, Silva VL, Souza MK, Deus LA, Reis AL, Simões HG, Beal FLR, Moraes MR, Navalta J, Prestes J, Gadelha AB, Rosa TdS (2020) Effects of resistance training on hepcidin levels and iron bioavailability in older individuals with end-stage renal disease: A randomized controlled trial. Exp Gerontol 139:111017
Domínguez R, Sánchez-Oliver AJ, Mata-Ordoñez F, Feria-Madueño A, Grimaldi-Puyana M, López-Samanes Á, Pérez-López A (2018) Effects of an acute exercise bout on serum hepcidin levels. Nutrients 10(2):209
Oliveira PF, Gadelha AB, Gauche R, Paiva FM, Bottaro M, Vianna LC, Lima RM (2015) Resistance training improves isokinetic strength and metabolic syndrome-related phenotypes in postmenopausal women. Clin Interv Aging 10:1299–1304. https://doi.org/10.2147/CIA.S87036
Gadelha AB, Paiva FM, Gauche R, de Oliveira RJ, Lima RM (2016) Effects of resistance training on sarcopenic obesity index in older women: a randomized controlled trial. Arch Gerontol Geriatr 65:168–173. https://doi.org/10.1016/j.archger.2016.03.017
Anding K, Bär T, Trojniak-Hennig J, Kuchinke S, Krause R, Rost JM, Halle M (2015) A structured exercise programme during haemodialysis for patients with chronic kidney disease: clinical benefit and long-term adherence. BMJ open 5(8):e008709
Howden EJ, Coombes JS, Strand H, Douglas B, Campbell KL, Isbel NM (2015) Exercise training in CKD: efficacy, adherence, and safety. Am J Kidney Dis 65(4):583–591
Dong J, Sundell MB, Pupim LB, Wu P, Shintani A, Ikizler TA (2011) The effect of resistance exercise to augment long-term benefits of intradialytic oral nutritional supplementation in chronic hemodialysis patients. J Renal Nutrition 21(2):149–159
Augustsson J, Esko A, Thomeé R, Svantesson U (1998) Weight training of the thigh muscles using closed versus open kinetic chain exercises: a comparison of performance enhancement. J Orthop Sports Phys Ther 27(1):3–8
Campos GE, Luecke TJ, Wendeln HK, Toma K, Hagerman FC, Murray TF, Ragg KE, Ratamess NA, Kraemer WJ, Staron RS (2002) Muscular adaptations in response to three different resistance-training regimens: specificity of repetition maximum training zones. Eur J Appl Physiol 88(1–2):50–60
Johnen B, Schott N (2018) Feasibility of a machine vs free weight strength training program and its effects on physical performance in nursing home residents: a pilot study. Aging Clin Exp Res 30(7):819–828
Mathiowetz V, Weber K, Volland G, Kashman N (1984) Reliability and validity of grip and pinch strength evaluations. J hand surgery 9(2):222–226
Gadelha AB, Neri SGR, Oliveira RJ, Bottaro M, David AC, Vainshelboim B, Lima RM (2018) Severity of sarcopenia is associated with postural balance and risk of falls in community-dwelling older women. Exp Aging Res 44(3):258–269. https://doi.org/10.1080/0361073X.2018.1449591
Gadelha AB, Vainshelboim B, Ferreira AP, Neri SGR, Bottaro M, Lima RM (2018) Stages of sarcopenia and the incidence of falls in older women: a prospective study. Arch Gerontol Geriatr 79:151–157. https://doi.org/10.1016/j.archger.2018.07.014
Kim J-K, Kim SG, Oh J-E, Lee Y-K, Noh J-W, Kim HJ, Song YR (2019) Impact of sarcopenia on long-term mortality and cardiovascular events in patients undergoing hemodialysis. The Korean J Int Med 34(3):599
Robertson RJ, Goss FL, Rutkowski J, Lenz B, Dixon C, Timmer J, Frazee K, Dube J, Andreacci J (2003) Concurrent validation of the OMNI perceived exertion scale for resistance exercise. Med Sci Sports Exerc 35(2):333–341
Chan KN, Chen Y, Lit Y, Massaband P, Kiratli J, Rabkin R, Myers JN (2019) A randomized controlled trial of exercise to prevent muscle mass and functional loss in elderly hemodialysis patients: rationale, study design, and baseline sample. Contemp Clini Trials Commun 15:100365
Gollie JM, Harris-Love MO, Patel SS, Argani S (2018) Chronic kidney disease: considerations for monitoring skeletal muscle health and prescribing resistance exercise. Clinical Kidney Journal 11(6):822–831
Fragala MS, Cadore EL, Dorgo S, Izquierdo M, Kraemer WJ, Peterson MD, Ryan ED (2019) Resistance training for older adults position statement from the National strength and conditioning association. J Strength Cond Res 33(8):2019–2052
Cappellini MD, Comin-Colet J, de Francisco A, Dignass A, Doehner W, Lam CS, Macdougall IC, Rogler G, Camaschella C, Kadir R (2017) Iron deficiency across chronic inflammatory conditions: International expert opinion on definition, diagnosis, and management. Am J Hematol 92(10):1068–1078
Bilar JM, da Silva FP, Feldner AC, Caravalho Filho R, Silva I, Pestana JM, Ferraz ML (2020) Iron overload in renal transplant patients: the role of hepcidin and erythropoietin. Transplantation proceedings 52, No 1, pp 169–174
Fraenkel PG (2017) Anemia of inflammation: a review. Medical Clinics 101(2):285–296
Olivares M, Hertrampf E, Capurro M, Wegner D (2000) Prevalence of anemia in elderly subjects living at home: role of micronutrient deficiency and inflammation. Eur J Clin Nutr 54(11):834–839
Cesari M, Penninx BW, Pahor M, Lauretani F, Corsi AM, Williams GR, Guralnik JM, Ferrucci L (2004) Inflammatory markers and physical performance in older persons: the InCHIANTI study. J Gerontol Series A: Biol Sci Med Sci 59(3):M242–M248
Visser M, Pahor M, Taaffe DR, Goodpaster BH, Simonsick EM, Newman AB, Nevitt M, Harris TB (2002) Relationship of interleukin-6 and tumor necrosis factor-α with muscle mass and muscle strength in elderly men and women: the Health ABC Study. J Gerontol Series A: Biol Sci Med Sci 57(5):M326–M332
Hangelbroek RW, Knuiman P, Tieland M, de Groot LC (2018) Attenuated strength gains during prolonged resistance exercise training in older adults with high inflammatory status. Exp Gerontol 106:154–158
Nemeth E, Tuttle MS, Powelson J, Vaughn MB, Donovan A, Ward DM, Ganz T, Kaplan J (2004) Hepcidin regulates cellular iron efflux by binding to ferroportin and inducing its internalization. Science 306(5704):2090–2093
Von Haehling S, Jankowska EA, Van Veldhuisen DJ, Ponikowski P, Anker SD (2015) Iron deficiency and cardiovascular disease. Nat Rev Cardiol 12(11):659
Wilkinson TJ, Shur NF, Smith AC (2016) “Exercise as medicine” in chronic kidney disease. Scand J Med Sci Sports 26(8):985–988
Acknowledgements
The authors would like to thank the patients who participated in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all the authors, the corresponding author states that there is no conflict of interest.
Statement of human and animal rights
All the experiments on human subjects were conducted in accordance with the Declaration of Helsinki and the study protocol was previously approved by the Institutional Review Board (08856012.6.0000.5505 and updated 23007319.0.0000.0029).
Informed consent
All volunteers were informed about the study procedures and voluntarily signed an informed consent form.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gadelha, A.B., Cesari, M., Corrêa, H.L. et al. Effects of pre-dialysis resistance training on sarcopenia, inflammatory profile, and anemia biomarkers in older community-dwelling patients with chronic kidney disease: a randomized controlled trial. Int Urol Nephrol 53, 2137–2147 (2021). https://doi.org/10.1007/s11255-021-02799-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-021-02799-6