Abstract
Objective
This study was carried out to evaluate the relationship between dietary and serum zinc and leptin levels with protein-energy wasting (PEW) in haemodialysis patients.
Methods
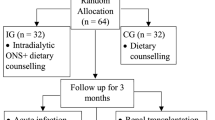
The study was conducted on 80 volunteer patients aged 19–65 years who received haemodialysis treatment three times a week for at least 1 year. Anthropometric measurements and body composition analyses were performed. Blood samples were collected for serum zinc and leptin and other biochemical parameters. Food consumption of the patients was recorded for 3 days. Malnutrition-inflammation score (MIS) was calculated for all patients. PEW was assessed according to the criteria recommended by the International Society of Renal Nutrition and Metabolism (ISRNM).
Results
According to the ISRNM criteria, 38.1% of male patients and 36.8% of female patients were diagnosed with PEW. The median serum leptin levels of patients with PEW [9.0 (16.9) ng/mL] were significantly lower than those without PEW [20.7 (38.5) ng/mL] (p < 0.05). Dietary zinc intake in patients with PEW was significantly lower than that in patients without PEW (p < 0.05). However, there was no significant difference in serum zinc levels between the patients with and without PEW. In the multivariate analyses, dietary and serum zinc and leptin was associated with PEW. After controlling for several confounding factors these associations disappeared. Dietary zinc intake and serum leptin levels were inversely correlated with MİS. There was no relationship between serum leptin and dietary and serum zinc in these patients.
Conclusion
Dietary zinc intake and serum zinc and leptin concentration were not associated with PEW. Low serum leptin levels might be the outcome rather than the cause of PEW in haemodialysis patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Protein-energy malnutrition (PEM) is a common problem in chronic kidney failure (CKF) and increases morbidity and mortality. The most important cause is insufficient food intake due to loss of appetite. The mechanisms that cause loss of appetite have not been clarified yet [1]. Recent guidelines (International Society of Renal Nutrition and Metabolism) (ISRNM) suggested using protein-energy wasting (PEW) instead of PEM to identify the clinical presentation of muscle loss, lipid loss, malnutrition and inflammation [2]. PEW is defined as a decrease in body protein reservoirs and energy (fat) resources [3]. The prevalence of PEW is reported as 18–75% in haemodialysis patients [4]. The role of adipokines in the pathogenesis of PEW is well known. Adipokine concentration increases due to a decrease in renal secretion in CKF. This causes loss of appetite, inflammation, PEW and atherosclerosis [5]. Elevation of leptin levels among adipokines may increase the risk of mortality through the loss of appetite and PEW in patients with CKF [6].
Leptin is a 16 kDa hormone which is encoded by the ob gene, mainly synthesised by adipocytes and metabolised in the kidneys. The most well-known function is to regulate food intake and energy metabolism through negative feedback and to prevent the development of obesity. Elevation of leptin levels was observed in the patients with CKF without any increase in body fat mass [7]. The causes for hyperleptinaemia include lower renal clearance, increased plasma insulin levels and inflammation. Because leptin prevents synthesis and release of neuropeptide-Y and reduces the appetite, it may play a role in anorexia and malnutrition developed in renal failure [1, 8]. The association between higher leptin levels and low protein intake in patients with CKF suggests that leptin could contribute to PEW [9].
Zinc is an essential micronutrient which acts in many biochemical processes. Zinc deficiency is associated with loss of appetite, anorexia, weight loss and developmental retardation [10, 11]. Zinc deficiency supports anorexia through different mechanisms [12]. Studies on the effects of zinc deficiency in patients with renal diseases are limited; it is suggested that the leptin hormone is an important element in explaining the physiology of anorexia [12]. Higher plasma leptin levels and serum zinc deficiency were reported in haemodialysis patients. It has been stated that these conditions cause malnutrition and may have an effect on morbidity and mortality [13]. To our knowledge, no study has evaluated the relationships between dietary and serum zinc and leptin with protein-energy wasting (PEW) in haemodialysis patients. The present study was designed and conducted to assess the association between serum leptin and dietary and serum zinc, which affects appetite, and their relationship to PEW in haemodialysis patients.
Methods
Participants
The present study was conducted in a private dialysis centre (RFM, Ankara). The study was carried out on 80 volunteer patients aged 19–65 years who received haemodialysis therapy three times a week for at least 1 year and were clinically stable and free of obvious oedema. The individuals with hepatitis, cancer, thyroid disease, liver disease, diabetes mellitus, cardiac diseases and chronic inflammation were excluded. For each patient, C-reactive protein (CRP) levels measured within the previous 6 months were reviewed from the dialysis centre’s records; patients with CRP ≤ 10 mg/dL [14] were included in the study. The Ethical Committee Approval with the number of KA48/2016 was obtained from the Ethical Board of Clinical Research of Zekai Tahir Burak Women’s Health and Training-Research Hospital. The procedure was conducted in accordance with the Declaration of Helsinki. The patients signed an informed consent form pertaining to their voluntary participation in the study.
Anthropometric measurements
Body weights of the patients were measured by an electronic scale (Medical Scale DR-Mod 85) with a sensitivity of ± 0.1 kg. Dry weight (after-dialysis weight) was used as the bodyweight of the patients [15]. Body mass index (BMI) was calculated through the formula “BMI = [after-dialysis weight (kg)/height (m2)]”. In case of a BMI under 23 kg/m2, one of the PEW criteria were deemed to be met [3].
Mid-arm circumference (MAC) was measured via a measuring tape at the mid-point between the acromial tubercle and olecranon of the elbow while the arm was bent 90° at the elbow. Triceps skin-fold thickness (TSFT) was measured with a Holtain caliper in accordance with standards. The measurements were performed from the fistula-free arm [15].
Mid-arm muscle area (MAMA) was calculated according to MAMA (cm2) = [MAC (cm)-(π × TSFT (cm)]2/4π”. An adjustment was made for the bone area; 10 cm2 in males and 6.5 cm2 in females were subtracted from the arm muscle area [15]. The MAMA was compared with the NCHS percentile values for people 18–74 years of age and the results were evaluated [16]. In case the mid-arm muscle area was below 10% of the 50th percentile, one of the PEW criteria was deemed to be met [3].
Analysis of body composition
Body composition measurement with the Bodystat-Quadscan 4000 (Bosystat Ltd; Isle of Man, UK) device was performed, with the patient lying down, by applying two electrodes onto the right hand and two electrodes onto the right foot at the end of the dialysis session. The after-dialysis body weight was used for the analysis of body composition. The body fat mass (kg), lean body mass (kg), total body water (TBW), body fat ratio (%), body fat mass index (BFMI), and fat-free mass index (FFMI) values were recorded [17].
Assessment of dietary intake
Dietary intake was assessed by three 24-h diet recalls including one dialysis day and two non-dialysis days by dietician. The average daily energy and macro and micronutrient intakes were calculated using the computer software Nutrition Information Systems (BeBiS, Version 7.0, Pasific Company, Stuttgart, Germany).
Malnutrition-inflammation score
Malnutrition-inflammation score (MIS) was calculated to evaluate the nutritional status of the patients. The MIS score is composed of three new parameters (BMI, serum albumin level and serum total iron-binding capacity) in addition to the seven parameters on the subjective global assessment (SGA). The intensity of each parameter is evaluated in 4 different stages as “0-normal” and “3-most severe”. The sum of ten different MIS criteria ranges from 0 (normal) to 30 (severe malnutrition), and high scores reflect the increased risk of malnutrition and inflammation [4].
Evaluation of protein-energy wasting (PEW)
The criteria suggested by ISRNM under four different categories were used for the diagnosis of PEW. The following criteria were selected: serum albumin < 3.8 g/dL and serum cholesterol < 100 mg/dL from category 1; BMI < 23 kg/m2 and body fat percentage < 10% from category 2; decrease in MAMA (a decrease of > 10% according to the 50th percentile of the reference population) from category 3; protein intake less than 0.8 g/kg body mass/day and energy intake less than 25 kcal/kg body mass/day from category 4. If three of those four categories (on the condition of meeting at least one criterion from each category) are detected in a patient, PEW was accepted as present [3].
Biochemical analysis
Blood samples were obtained before the midweek HD session after the patients had fasted overnight in a similar fashion. Patients were receiving thrice-weekly dialysis for 4 h period with a standard bicarbonate-containing dialysate bath, using a high-flux HD membrane. Serum leptin levels were measured by enzyme-linked immunosorbent assay (ELISA) using the Human Leptin Elisa Kit (Cusabio) in the Research Laboratory of Nutrition and Dietetics Department within the Gazi University Health Sciences Faculty.
Zinc analysis was performed by ICP-MS (Inductively Coupled Plasma Mass Spectrometry) (Perkin Elmer) technique in the Advanced Technology Practice Laboratory of Selçuk University.
Power calculation and statistical analysis
The sample size was calculated by G power analysis program according to the results of a similar study (13). The sample size was determined as 67 and 76 patients at 80% and 85% power (2-sided alpha, p = 0.05) respectively. Therefore, the sample size of the study (n = 80) was selected because it provided adequate power to detect the relationship between dietary and serum zinc and leptin.
Statistical analysis of the data was performed using the SPSS 22 statistical package program. The Kolmogorov–Smirnov test or the Shapiro–Wilk test of normality was used for determining data distribution. Variables with normal distribution were presented as mean (\(\bar{X}\)) and standard deviation (SD). The independent t test was applied to compare means. Non-normal distribution variables were presented as the median and interquartile range (IQR). The Mann–Whitney U test was used to compare groups. Qualitative variables were described as number (n) and percentage (%). The Spearman’s correlation coefficient was used to determine the correlation between dietary and serum zinc and leptin and the variables. Multivariate logistic regression analysis was performed including dietary and serum zinc and leptin level to investigate the associations with PEW. The lowest significance level was accepted as 0.05 in all statistical tests (p < 0.05). p values are two-tailed.
Results
In total, 80 patients were included in the study, 42 (52.5%) of whom were male and 38 (47.5%) female. The mean age of the patients was 50.6 ± 10.96 years. The patients’ characteristics are shown in Table 1. The primary aetiology of CKF was hypertension (42.5%), glomerulonephritis (10%), polycystic kidney disease (6.3%), nephrolithiasis or nephrotic syndrome (5%) and other or unknown causes (31.2%).
In female patients, TSFT, fat mass percentage, fat mass, BFMI and MIS score were significantly higher than in male patients. FFMI and dietary zinc intake were significantly lower in females than in males (p < 0.05). The median serum leptin levels of male patients were significantly lower than that of female patients (p < 0.05). There was no statistically significant gender-based difference in serum zinc levels (p > 0.05) (Table 1).
Table 2 shows the prevalence of PEW. Based on the ISRNM criteria, PEW was diagnosed in 37.5% of all patients, including 36.8% of females and 38.1% of males (Table 2).
The anthropometric measurements, biochemical parameters, and dietary intake of patients with PEW and non-PEW are presented in Table 3. The dry weight, BMI, TSFT, MAC, and MAMA means of the patients with non-PEW were found significantly higher than the means of those with PEW (p < 0.05). Fat mass, BFMI, and FFMI median values of the patients with PEW were lower than the median values of the patients with non-PEW. The difference between the groups was statistically significant (p < 0.05) (Table 3).
The median serum leptin levels of the patients with PEW [9.0 (16.9) ng/mL] were significantly lower than in those without PEW [20.7 (38.5) ng/mL] (p < 0.05). The median serum zinc levels in patients with and without PEW were 124.5 (65.7) µg/dL and 105.4 (32.6) µg/dL, respectively; there was no statistically significant difference between the groups (p > 0.05) Dietary zinc intake in patients with PEW were significantly lower than in those without PEW (p < 0.05) (Table 3).
A comparison of dietary and serum zinc and leptin levels above and below the threshold values for each selected PEW criterion is presented in Table 4. The median serum leptin levels of the patients with a total cholesterol level below 100 mg/dL were significantly lower than in those with a total cholesterol level at or above 100 mg/dL (p < 0.05) (Table 4).
The median serum leptin levels of the patients with a BMI at or above 23 kg/m2 was significantly higher than in those with a BMI below 23 kg/m2 (p < 0.05). Serum leptin levels were significantly lower with MAMA reduction, greater than 10% according to the 50th percentile value of the reference population (p < 0.05). Serum zinc levels of the patients with a dietary protein intake below 0.8 g/kg/day were found significantly higher than in the patients with dietary protein intake at or above 0.8 g/kg/day (p < 0.05). Dietary zinc intake of the patients with a dietary protein intake below 0.8 g/kg/day and a dietary energy intake below 25 kcal/kg/day were found significantly lower than in the patients with a dietary protein intake at or above 0.8 g/kg/day and a dietary energy intake below 25 kcal/kg/day (p < 0.05) (Table 4).
The correlation of dietary and serum zinc and leptin level with various factors is presented in Table 5. There was no association detected between serum leptin levels, dietary and serum zinc levels of the patients (p > 0.05). Serum leptin levels were significantly and negatively correlated with handgrip strenght and MIS score; they were positively correlated with BMI, TSFT, MAC and MAMA. Dietary zinc intake was significantly and negatively correlated with MIS score (Table 5).
In the multivariate logistic regression analyses, dietary and serum zinc and leptin was associated with PEW (OR = 0.67, 95% CI 0.50–0.90, p < 0.05, OR = 1.00, 95% CI 1.00–1.01, p < 0.05, and OR = 0.97, 95% CI 0.95–0.99, p < 0.05, for dietary zinc intake, serum zinc and leptin levels respectively). After adjusted for age, gender, BMI, fat mass, haemodialysis vintage, and albumin the association remained significant only with dietary zinc intake in Model 2 (OR = 0.62, 95% CI 0.43–0.89, p < 0.05). However, this significant association disappeared after protein intake was considered a confounding factor in Model 3 (Table 6).
Discussion
In the present study, PEW was diagnosed in 37.5% of the patients (Table 2). A similar study conducted to evaluate PEW states in 22 haemodialysis patients according to ISRNM criteria in Spain revealed that PEW prevalence in the patients was 37% [18]. A study of 105 haemodialysis patients in Denmark reported the PEW prevalence as 29% according to the ISRNM criteria. When PEW was re-evaluated based on lean body mass index and fat mass index, the prevalence was reported as 4% [19]. A Japanese study that evaluated the PEW state in 210 patients according to three different BMI criteria found the prevalence of PEW to be 38.0%, 29.0%, and 14.8% for BMI < 23 kg/m2, BMI < 20 kg/m2, and BMI < 18.5 kg/m2, respectively [20]. The difference in PEW prevalence in those studies conducted in different countries may be connected to the difference in criteria used to evaluate PEW. Furthermore, the sample count and the average age of the patients included in the study might have been effective.
Leptin is released from adipose cells in proportion to body fat quantity; it increases energy consumption and inhibits food intake [21]. In this study, the median serum leptin levels of male and female patients were detected as 7.6 ng/mL and 38.5 ng/mL, respectively; the difference between the groups was statistically significant (p < 0.05) (Table 1). Sabbagh et al. [22] conducted a study on 104 haemodialysis patients and similarly detected serum leptin levels of male and female patients as 8.07 ± 13.08 ng/mL and 39.75 ± 42.38 ng/mL, respectively. Higher body fat percentage, more subcutaneous fat tissue, and hormonal reasons are the factors describing higher leptin levels in females [23].
Median serum leptin values of the patients with PEW [9.0 (16.9) ng/mL] were significantly lower than in the patients without PEW [20.7 (38.5) ng/mL] (p < 0.05) (Table 3). Similarly, Yu Chiu et al. [24] conducted a study with 188 haemodialysis patients, and serum leptin values of the patients with and without PEW were found to be 4.5 ng/mL and 14.9 ng/mL, respectively. Markaki et al. [25] measured leptin levels in the patients meeting three criteria, meeting one or two criteria, and meeting none of the ISRNM criteria for PEW as 5.3 ng/mL, 14.4 ng/mL and 18.2 ng/mL, respectively. Serum leptin levels were statistically higher in patients with greater total cholesterol levels, BMI values, and MAMA (p < 0.05) (Table 4). A positive correlation was found between serum leptin levels and dry weight, MAC, MAMA, BMI, TSFT and a negative correlation was also found with MIS (Table 5). Consistent with these findings, Montazerifar et al. [26] found a positive correlation between serum leptin levels and weight, BMI, and MAC. Similarly, a recently conducted study associated higher leptin levels with higher BMI, higher MAMA, and good nutritional status [25]. In the multivariate analyses, low leptin was associated with PEW (Table 6). However, this association lost its significance after adjusting for several confounding factors in model 2 (Table 6). Lower leptin levels in the patients with PEW compared to the patients without PEW may be explained as follows: elevation of leptin associated with renal function loss causes decreases in appetite and body fat mass. The decrease in serum leptin levels is proportional to the decrease in fat mass. Consistently, this study showed that patients with PEW had lower body fat mass compared to patients without PEW (Table 3), and serum leptin level positively correlated with fat mass (Table 5). Therefore, the lower leptin levels in the patients with PEW compared with those without PEW in the present study may be explained by decreased fat mass in the patients with PEW. Therefore, this result shows that low serum leptin levels might be the outcome rather than the cause of PEW.
The incidence of zinc deficiency is reported to range between 50 and 78% in haemodialysis patients [10, 11]. The causes of zinc deficiency in these patients include low zinc intake per diet, reduction of zinc absorption through low protein intake, and excretion of zinc in protein-zinc complexes because of increased proteinuria [12]. The European Best Practice Guideline on Nutrition and Chronic Kidney Disease recommends a daily zinc intake of 10–15 mg/day for males and 8–12 mg/day for females [27]. In this study, dietary zinc intake was determined as 7.2 ± 2.33 mg/day in male patients and 5.6 ± 1.58 mg/day in female patients (p < 0.05) (Table 1). These amounts are less than the daily recommendations. Van Duong et al. [28] reported that dietary zinc intake of haemodialysis patients as 7.5 ± 4.2 mg/day. The fact that the amount of zinc consumed daily is below the recommended value can be explained by the restriction of protein sources such as meat, fish, milk, which are the sources of zinc, to balance the serum phosphorus values of the patients.
The reference values of serum zinc levels for adults are considered to be 80–120 μg/dL [29]. In this study, the median serum zinc levels of the patients were found to be 107.7 (42.2) μg/dL (Table 1). In parallel with the results, Uslu et al. [30] found that serum zinc levels of haemodialysis patients was 104.4 ± 41.63 μg/dL. In this study, although the dietary zinc intake of the individuals was insufficient, serum zinc levels were found to be in the normal range. The reason for this might be explained as follows; in cases which short-term hunger and zinc loss increase, it is reported that temporary normal serum zinc levels can be observed due to zinc release from tissues and cells [31].
Zinc deficiency is associated with decreased appetite and low body weight [32]. There is a limited number of studies on the effects of zinc deficiency, which has a wide biological activity range and is associated with anorexia in the patient with renal diseases [12]. In this study, dietary zinc intake in patients with PEW were significantly lower than in those without PEW (p < 0.05) (Table 4). Dietary zinc intake was negatively correlated with MİS (p < 0.05) (Table 5). Multiviarate regression analysis showed that lower dietary zinc intake was associated with PEW, however, this significant association disappeared after the multivariate analysis that included protein intake as a confounding factor in model 3 (Table 6). It is well known that protein-rich sources such as meat, fish and dairy foods are good sources of zinc. In this study, low zinc intake in patients with pew can be explained by the lower protein intake of patients with pew than those without pew. In this study, the protein intake of patients is low. Consistent with this result, in a study conducted by Kim et al. [33], patients’ daily protein intake was determined to be 0.9 ± 0.3 g/kg/day. In a study conducted with 128 haemodialysis patients in Turkey, it is found that dietary protein intake was lower than recommended in 78.1% of patients [34]. Dietary protein intake tend to be low in hemodialysis patients because these patients are often undernourished due to chronic inflammation, uremia, and food restrictions. In this study, low protein intake may be attributed to the patients’ inadequate energy intake and the fact that the phosphorus sources that should be restricted in these patients are also protein-rich sources.
It has been reported that the leptin hormone is an important factor in explaining zinc deficiency-induced anorexia in renal patients, and zinc may significantly affect leptin secretion [35]. Lee et al. [36] found in their study that zinc deficiency increased serum leptin levels, whereas supplementation of zinc reduced such levels. Chen et al. [37] found a significant increase in urinary zinc excretion in obese rats with higher leptin and lower zinc levels. It was reported in the same study that supplementation of zinc caused an increase in leptin levels and prevention of obesity; the leptin resistance found in obesity may be caused by zinc deficiency. Moreover, it has been reported that zinc may affect gene expression of leptin directly, or it may cause leptin production by increasing the use of glucose by adipose tissue. Konukoğlu et al. [35] suggested that lower zinc levels in obese patients cause leptin resistance. However, in the present study, there was no significant association between serum leptin level and zinc (p > 0.05) (Table 5). Moreover, there was no significant difference in serum zinc levels between the patients with and without PEW (Table 3). In line with the study above, Şahin et al. [38] reported that there was no correlation between serum zinc and leptin levels. In the present study, a lack of association between serum leptin and zinc may be explained by the lower number of patients of zinc deficiency.
The most important strength of this study is that it is the first study to evaluate the relationship between dietary and serum zinc and leptin levels and PEW. Another strength of our study is the use of ICP-MS, a highly sensitive, modern and sensitive method that eliminates analytical errors for serum zinc analysis. The present study has also some limitations. First, the sample size was relatively small. The power of the statistical analysis could be increased by increasing sample size. Second, causal relationships between PEW and dietary and serum zinc and leptin levels could not be determined from this study due to its cross-sectional design. Therefore, future randomized control studies are required to clarify these relationships.
Conclusion
The results of this study suggest that PEW is prevalent in haemodialysis patients. Dietary zinc intake and serum zinc and leptin concentration were not associated with PEW. Low serum leptin might be the outcome rather than the cause of PEW in haemodialysis patients. There was no relationship between serum leptin and dietary and serum zinc in these patients. More studies with the large sample are needed to understand the association between dietary zinc and serum zinc and leptin levels and protein-energy wasting in these patients.
References
Doğukan A, Utaş C (1998) Kronik böbrek yetersizliği ve leptin. Turk Neph Dial Transpl 3:129–131
Harvinder GS, Swee WCS, Karupaiah T, Sahathevan S, Chinna K, Ahmad G, Bavanandan S, Leong Goh B (2016) Dialysis Malnutrition and Malnutrition Inflammation Scores: screening tools for prediction of dialysis–related protein-energy wasting in Malaysia. Asia Pac J Clin Nutr 25(1):26–33
Fouque D, Kalantar-Zadeh K, Kopple J et al (2008) A proposed nomenclature and diagnostic criteria for protein–energy wasting in acute and chronic kidney disease. Kidney Int 73(4):391–398
Kalantar-Zadeh K, Ikizler TA, Block G et al (2003) Malnutrition-inflammation complex syndrome in dialysis patients: causes and consequences. Am J Kidney Dis 42(5):864–881
Niemczyk S, Romejko-Ciepielewska K, Niemczyk L (2011) Adipocytokines and sex hormone disorders in patients with chronic renal failure (CRF). Endokrynologia Polska 63(2):148–155
Kaynar K, Kural BV, Ulusoy S et al (2014) Is there any interaction of resist in and adiponectin levels with protein-energy wasting among patients with chronic kidney disease. Hemodial Int 18(1):153–162
Sharma K, Considine RV (1998) The Ob protein (leptin) and the kidney. Kidney Int 53(6):1483–1487
Amela Dervisevic AS, Avdagic N, Zaciragic A et al (2015) Elevated serum leptin level is associated with body mass index but not with serum C-reactive protein and erythrocyte sedimentation rate values in haemodialysis patients. Mater Socio-med 27(2):99
Young G, Woodrow G, Kendall S et al (1997) Increased plasma leptin/fat ratio in patients with chronic renal failure: a cause of malnutrition? Nephrol Dial Transpl 12(11):2318–2323
Dvornik S, Cuk M, Racki S, Zaputović L (2006) Serum zinc concentrations in the maintenance hemodialyzed patients. Coll Antropol 30(1):259–263
Lee SH, Huang JW, Hung KY et al (2000) Trace metals abnormalities in hemodialyzed patients, relationship with medications. Artif Organs 24(11):841–844
Lobo JC, Aranha LN, Moraes C, Brito LC, Mafra D (2012) Linking zinc and leptin in chronic kidney disease: future directions. Biol Trace Elem Res 146(1):1–5
Aranha LN, Lobo JC, Stockler-Pinto MB, de Oliveira Leal V, Torres JPM, Mafra D (2012) Relationship between zinc levels and plasma leptin in haemodialysis patients. J Trace Elem Med Biol 26(4):238–242
/DOQI (2005) Clinical practice guidelines for cardiovascular disease in dialysis patients. Am J Kidney Dis 4(Supplement):16–153
Gibson RS (1990) Principles of nutritional assessment. Oxford University Press, New York
Pekcan G (2008) Beslenme Durumunun Saptanması. In: Baysal, A, Aksoy M, Besler T, et al. “Diyet El Kitabı. 5. baskı.” Ankara: Hatipoğlu Yayınevi 67-141. P
Forque DPJ (2003) Management of the renal patient clinical algorithms on the nutritional status and its relation to inflammation. Pasts Science Publishers, California
Gracia-Iguacel C, González-Parra E, Pérez-Gómez MV et al (2013) Prevalence of protein-energy wasting syndrome and its association with mortality in haemodialysis patients in a centre in Spain. Nefrologia 33(4):495–505
Koefoed M, Kromann CB, Juliussen SR, Hvidtfeldt D, Ekelund B, Frandsen NE et al (2016) Nutritional status of maintenance dialysis patients: low lean body mass index and obesity are common, protein-energy wasting is uncommon. PLoS One 11(2):e0150012
Kanazawa Y, Nakao T, Murai S, Okada T, Matsumoto H (2017) Diagnosis and prevalence of protein-energy wasting and its association with mortality in japanese haemodialysis patients. Nephrology 22(7):541–547 (2016)
Özkök AİB, Erdemoğlu E, Özberk O et al (2014) Leptin parameters are associated with inflammation and both anthropometric and serum markers of protein-energy wasting in haemodialysis patients. Turk Neph Dial Transpl 23(2):85–89
Ghorban-Sabbagh M, Nazemian F, Naghibi M et al (2016) Correlation between serum leptin and bone mineral density in haemodialysis patients. J Renal Inj Prev 5(3):112
Haffner S, Gingerich R, Miettinen H, Stern M (1996) Leptin concentrations in relation to overall adiposity and regional body fat distribution in Mexican Americans. Int J Obes Relat Metab Disord 20(10):904–908
Chiu TTY, Liao SC, Lee WC et al (2015) Gelsolin and adipokines are associated with protein-energy wasting in haemodialysis patients. Art organs 39(2):150–155
Markaki A, Grammatikopoulou MG, Venihaki M, Kyriazis J, Perakis K, Stylianou K (2016) Associations of adiponectin and leptin levels with protein-energy wasting, in end stage renal disease patients. Endocrinol Nutr 63(9):449–457
Montazerifar F, Karajibani M, Hassanpour Z, Pourmofatteh M (2015) Study of serum levels of leptin, C-reactive protein and nutritional status in haemodialysis patients. Iran Red Crescent Med J 17(8):e26880
Fouque D, Vennegoor M, Ter Wee P et al (2007) EBPG guideline on nutrition. Nephrol Dial Transpl 22:45–87
Van Duong T, Wong T-C, Su C-T et al (2018) Associations of dietary macronutrients and micronutrients with the traditional and nontraditional risk factors for cardiovascular disease among haemodialysis patients: a clinical cross-sectional study. Medicine 97(26):e11336
Burtis CA, Ashwood C, Bruns ERD (2012) Tietz textbook of clinical chemistry and molecular diagnostics (Fifth Edition). Elsevier/Saunders, Philadelphia, pp 1523–1525
Uslu S, Çolak Ö, Demir TA et al (2005) Hemodiyaliz Hastalar› nda Kardiak Belirteçler ve‹ z Elementler. Türk Klinik Biyokimya Dergisi 3(2):85–93
Aydın MZ (2012) Hemodiyaliz hastalarında serum çinko düzeyi ile anemi ve tedavisi ve diğer ilişkili faktörlerin değerlendirilmesi. Dissertation, University of Kocaeli
Jing M-Y, Sun J-Y, Wang J-F (2008) The effect of peripheral administration of zinc on food intake in rats fed Zn-adequate or Zn-deficient diets. Biol Trace Elem Res 124(2):144–156
Kim H, Lim H, Choue R (2015) A better diet quality is attributable to adequate energy intake in hemodialysis patients. Clin Nutr Res 4:46–55
Ekenci KD, Türker PF, Ercan A (2020) Hemodiyaliz Hastalarının Demografik Özelliklerine Göre Beslenme Durumlarının Değerlendirilmesi. Beslenme ve Diyet Dergisi 3(2):1–11
Konukoglu D, Turhan MS, Ercan M, Serin O (2004) Relationship between plasma leptin and zinc levels and the effect of insulin and oxidative stress on leptin levels in obese diabetic patients. J Nutr Biochem 15(12):757–760
Lee S-L, Kwak E-H, Kim Y-H (2003) Leptin gene expression and serum leptin levels in zinc deficiency: implications for appetite regulation in rats. J Med Food 6(4):281–289
Chen M-D, Song Y-M, Lin P-Y (2000) Zinc may be a mediator of leptin production in humans. Life Sci 66(22):2143–2149
Şahin H, Uyanik F, Inanç N, Erdem O (2009) Serum zinc, plasma ghrelin, leptin levels, selected biochemical parameters and nutritional status in malnourished haemodialysis patients. Biol Trace Elem Res 127(3):191–199
Funding
The authors declare that they have no relevant financial interests. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yurtdaş, G., Karabudak, E. & Mandıroğlu, F. Relationship of dietary and serum zinc and leptin levels with protein energy wasting in haemodialysis patients. Int Urol Nephrol 52, 1969–1977 (2020). https://doi.org/10.1007/s11255-020-02573-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-020-02573-0