Abstract
Purpose
There is a paucity of data regarding urology involvement in the management of lower urinary tract injuries (LUTI). We seek to analyze the incidence and epidemiology of LUTI with special attention to trends in urology consultation.
Methods
A retrospective review was conducted of patients presenting to our Level I trauma center with LUTI from 2002 to 2016. Demographics, mechanism of injury, associated injuries, injury severity score (ISS), American Association for the Surgery of Trauma (AAST) injury scales, and clinical hospital course were analyzed.
Results
A total of 140 patients (0.47% of all trauma patients) were identified with LUTI, with 72.1% of these presenting with blunt trauma. Bladder injuries were more common than urethral injuries (79% vs. 14%) with 6% of patients having both. In-hospital mortality was 9.2% (13/140). Among patients with LUTI, 115 patients (82%) received urology consultation. There was no significant difference in sex, age, or LOS (hospital and ICU) between the groups. The consult group had a lower mean ISS (21.7 vs 27.9, p = 0.034), but a higher mean AAST bladder injury scale (2.57 vs 2.00, p = 0.016), than the non-consult group. There was a statistically significant difference in the diagnosis methods between the two groups (χ2 test of independence, p = 0.002).
Conclusion
Urology service is important in the management of LUTI with high AAST injury scale. While further study is needed to look at degree of urology service involvement in the management of LUTI, we recommend a consultation for severe LUTI or when the management of injuries is out of the comfort zone of the trauma surgeons. Whether consultation is obtained or not, there is room for improvement in appropriate work up of lower urinary tract injury.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
While lower urinary tract injuries (LUTI) are an uncommon finding in patients with poly-trauma, these injuries can have significant morbidity if missed or treated improperly [1,2,3,4,5,6]. To mitigate this morbidity, standardized guidelines for the evaluation of trauma to the lower urinary tract exist [7]. These guidelines are based on historical descriptions of mechanisms and comorbid injuries associated with LUTI, largely from small cohort studies [8,9,10] or large databases [11]. A core recommendation of these guidelines is urinary tract-specific imaging when suspicion of LUTI is high [12, 13]. Genitourinary specific imaging is necessary to confirm LUTI, even when injuries are suspected based on initial trauma imaging or physical exam findings such as blood at urethral meatus, pelvic fracture, or abnormal digital rectal exam.
Trauma or general surgery teams are often the first physicians to evaluate patients following a trauma, and the initial identification and work up of lower urinary tract injury is within their scope. In many institutions, these general surgery teams diagnose and treat lower urinary tract injuries without urologic consultation. A previous study has looked at the effect of preoperative medical consultations on surgical outcomes and found inconsistent effects on efficiency and quality of care in surgical patients [14]. To our knowledge, no one has described or analyzed the involvement of the urology team in the diagnosis and management of traumatic lower urinary tract injuries. Our primary aim is to retrospectively review the epidemiology of LUTI over 15 years in our trauma center’s cohort with special attention to trends in urology consultation and the effect on initial inpatient outcomes. Secondary aims include reviewing the mechanism of diagnosis of lower urinary tract; trends over time in urologic consultation and conservative management; and effect of pelvic fracture on presentation of lower urinary tract injuries. We hypothesize that urologic consultation will be associated with higher grade injuries, more appropriate work up of lower urinary tract injury, and improved short-term outcomes during initial trauma admission.
Methods
This study was approved by the institutional review board (IRB) of the University at Buffalo, the State University of New York. All patients presenting to Erie County Medical Center (ECMC) for trauma between 2002 and 2016 were identified in our institution’s trauma registry. ECMC is the only Level I trauma center in Western New York and serves a large, diverse catchment area. A retrospective chart review was conducted of all patients presenting with lower urinary tract injury. The inclusion criteria are as follows: (1) injuries to bladder or urethra identified based on International Classification of Disease version 9 diagnostic codes (ICD-9) for traumatic injuries to bladder or urethra (867.0–867.1), (2) blunt or penetrating mechanisms, (3) age ≥ 18 y/o. All iatrogenic injuries were excluded. These patients were categorized as having bladder injury, urethral injury, or both. Those with bladder injury were further stratified based on whether the injury was extraperitoneal, intraperitoneal, both, or a bladder contusion. The diagnosis of lower urinary tract injury was based on retrograde urethrogram/cystogram, CT cystogram, intraoperative findings, and/or physical exam findings. Both extraperitoneal and intraperitoneal injuries were full thickness with extravasation seen on CT or cystogram imaging or perforation of bladder seen on exploration. Bladder contusion was the diagnosis when an injury was suspected based on hematuria and mechanism of injury without extravasation seen on CT or cystogram. In one case, a urethral injury was diagnosed in a gun shot wound victim on physical exam without retrograde urethrogram.
Demographics including gender, race, and age were collected on chart review. Mechanism of injury, overall injury severity score (ISS), type of LUTI, American Association for the Surgery of Trauma (AAST) bladder and urethral injury scales, associated injuries, method of diagnosis of LUTI, and hospital course were analyzed. These are the primary outcomes of this study aimed at describing the epidemiology of lower urinary tract injury at our center. The hospital course was characterized by hospital and ICU length of stay (LOS), operative vs. conservative management, in-hospital mortality, and whether urology consultation was obtained. Any intervention to primarily repair an injury by the general surgery or urology team was considered an operative treatment. Treatment of LUTI with catheterization (transurethral Foley catheter or suprapubic tube) only was considered conservative management. Mechanism of diagnosis was assessed during retrospective chart review as a secondary outcome.
Data were analyzed using IBM SPSS v21. Categorical variables were analyzed with χ2 tests and continuous variables with student’s t test in a two-sided fashion with p < 0.05 considered statistically significant. Binary logistic regression was used to control for injury severity when analyzing the association between consultation and mortality.
Results
Demographics and clinical characteristics
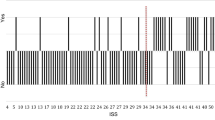
Among 29,247 trauma patients admitted to the hospital during the 15-year study period, 140 (0.47%) patients were identified with LUTI. Demographics and clinical characteristics of these 140 trauma patients are shown in Table 1. The mean age of patients with LUTI was 40.3 years (range 18–90). Blunt trauma was the cause of injury in 103 patients (73.6%) vs. penetrating trauma in 37 (26.4%). Mechanism of injury is characterized in Fig. 1. Motor vehicle collision was the most common mechanism of injury followed by falls and pedestrians struck. Gunshot wounds were the most common penetrating injuries. The mean ISS was 22.8 (range 4–66) with a mean length of stay of 14.1 days (range 1–81). Injuries were managed conservatively in 81 patients (58%). No significant difference was seen in mean LOS or ISS of those managed conservatively vs. operatively (14.2 vs. 14.9 and 21.1 vs. 22). In-hospital mortality overall was 9.2% (13/140).
Primary outcome: comparisons of LUTI with and without urology consultation
Of 140 LUTI patients, 115 patients (82%) received urology consultation. There was no significant difference in sex, age, or LOS (hospital or ICU) between the consult and non-consult groups (Table 2). The consult group had a lower mean ISS (21.7 vs. 27.9, p = 0.034) than the non-consult group. But, the consult group did have a higher mean AAST bladder injury scale (2.57 vs. 2.04, p = 0.023) than the non-consult group (Table 3). All patients with an AAST injury scale ≥ 4 received a urology consult. Mortality in the urology consultation group was significantly lower than the non-consult group (6% vs. 25%, p = 0.002). Logistic regression controlling for ISS showed that urology consultation remained significantly associated with lower mortality (OR: 0.165, p = 0.012). There was no difference in rate of urology consultation in those with hematuria vs. without (87% vs. 77%, p = 0.22). Similarly, there was no difference in conservative management between urology consult vs. no consult (60% in both groups).
Secondary outcome: diagnosis method of lower urinary tract injury
On chart review, we found that a diagnosis of LUTI was based on one of four diagnostic methods: initial trauma imaging, intraoperative finding, genitourinary specific imaging (RUG/Cystogram), or physical exam. As shown in Table 4, there was a statistically significant difference in the diagnosis methods between the consult and non-consult groups (Chi-square test of independence, p = 0.002). LUTIs in the consult group were diagnosed based on cystogram/retrograde urethrogram more often than in the non-consult group (50% vs. 20%, p = 0.007). Most LUTIs in the non-consult group were diagnosed on initial trauma imaging or intraoperative findings.
Secondary outcome: trends over time
We additionally conducted subset analysis of the three 5-year intervals in our collected cohort of patients. The number of trauma patients presenting with LUTI were 53, 45, and 42, respectively, in these intervals. During these intervals, consults were obtained in 43/53, 42/45, and 30/42 patients, respectively. These correspond to consultation rates of 81, 93, and 71%. A clear trend was seen in rising rates of conservative management during the time period of our study. During the first interval, 47% of patients were treated conservatively, 56% in the second interval, and 74% in the third interval.
Secondary outcome: affect of pelvic fracture on initial lower urinary tract injury presentation
Overall, 85 patients (60.7%) with lower urinary tract injury were diagnosed with concomitant pelvic fracture. There was no difference in rate of urology consultation (86% vs. 76%, p = 0.178) between those with pelvic fracture and those without. AAST LUTI grade showed no difference based on pelvic fracture (mean: 2.6 vs. 2.5, p = 0.844). There was no difference in rate of gross hematuria (73% vs. 75%, p = 0.272) between those with pelvic fracture and without. Age, LOS, ICU stay, and ISS were statistically significantly higher in those with pelvic fracture vs. without (Table 5).
Discussion
Our purpose is to retrospectively analyze and describe the involvement of urologic surgeons in patients with lower urinary tract injuries and the effect of this consultation on clinical outcomes. We found that the urologic service is frequently consulted for LUTI, and that while ISS was higher in the non-consult group, organ-specific AAST injury grade was higher in the consultation group. We also showed that the diagnostic modality was significantly different between consulted and non-consulted groups.
Overall, the incidence rate of lower urinary tract injuries in our study is in line with other estimates (0.47%) [2]. Similar to other recent studies, blunt trauma was more common than penetrating mechanism, and very often associated with pelvic fracture [1, 2, 15]. The rate of pelvic fracture-associated LUTI among blunt trauma patients was 3.6% in our cohort compared to 4.2% in the Vanderbilt cohort [1].
The urology consultation rate has not been previously described in any other study. This rate will vary regionally with access to urologic specialists and comfort of general surgery/trauma surgery teams with treatment of urinary tract injuries. Urology consultation was obtained in 82% of the patients in our study. We saw that the mean ISS scores were higher in patients who did not get a consult. The mortality rate was also significantly higher in the non-consult group. These both could be due to urology consultation not being obtained in trauma patients who are unstable on presentation to ER and proceed directly to the operating room. It is possible that the most severely injured patients do not live long enough for consultation to be obtained. In our cohort, three patients died on day of presentation and three more on hospital day 1. All six of these patients did not get urology consultation. Our logistic regression analysis controlling for ISS demonstrated that consultation remained significantly associated with mortality. The strength of this assertion suffers from the small number of mortalities in our cohort and should not be over interpreted.
Diagnosis of lower urinary tract injuries is important and can be established through several mechanisms as described in our study. While trauma imaging may be suggestive of LUTI, this must be confirmed on genitourinary specific imaging. Our study showed that the method of diagnosis was significantly different in the consultation group and non-consultation group. Specifically, many more patients in the consultation group are getting CT cystograms and retrograde urethrograms. This is an important finding that may be suggestive of a larger underlying issue. While 50% of the patients in the consultation group had a cystogram or retrograde urethrogram, only 20% of patients in the non-consult group did. This type of imaging is important, because it can show location of injury and differentiating between extraperitoneal and intraperitoneal injuries changes management. Additionally, even those with intraoperative findings of LUTI require genitourinary specific imaging. It would be easy to miss a second bladder injury or a urethral injury that is concomitant with a bladder injury. While we cannot describe how common this is, it is possible that bladder or urethral injuries may have been missed both in the consult and non-consult groups. While the consultation group did have a higher percentage of patients diagnosed based on the genitourinary specific imaging, this rate in this group was still concerningly low at only 50%.
While our study is not primarily focused on pelvic fractures, these injuries cannot be ignored when describing lower urinary tract injuries. Pelvic fractures are signs of significant force of injury and when present raise the suspicion of LUTI. Pelvic fractures were seen in 60.7% of all patients with lower urinary tract injury, and 77.7% of those with blunt mechanism of injury. As shown in Table 5, pelvic fracture is a significant contributor to ICU and hospital length of stay and is associated with ISS.
There was no difference seen in ICU length of stay or overall length of stay between the consultation group with higher grade urologic injury and non-consultation group with lower grade urologic injury. Pelvic fracture on the other hand was significantly associated with length of stay. This is unsurprising as pelvic fracture can limit mobility and ability to participate in physical therapy, which are crucial steps in preparing for discharge [16]. Many of the urologic injuries in our study were treated conservatively with catheterization. Presence of a catheter should not be limiting in progression from ICU to floor or floor to home. Even when urologic injury is repaired operatively, cystorrhaphy is a procedure with minor morbidity. The morbidity of urologic injury often presents years later with urethral stricture or bladder neck contracture [6, 17] and would not be apparent on initial trauma admission as shown in our study.
Limitations of our study include that we were unable to analyze any long-term follow-up for the patients seen with LUTI. We cannot assess effectiveness of conservative vs. operative management or difference in long-term outcome between patients getting a consult vs. not. Another limitation of our study is that due to the rarity of these injuries, we had to look at an extended retrospective cohort. It is possible that trends have changed with new faculty both in general surgery and urology departments at our trauma center. We did show that consultation and conservative management rates varied during the time period of our analysis. These differences seen on subgroup analysis are highly dependent on the small numbers of injuries seen during each 5-year period.
The application of our findings is important locally and generally. This study will serve as an opportunity for quality improvement. While no length of stay benefit was demonstrated in patients who get a urology consultation, the patients with most severe injuries are getting consultation. Patients without urology consultation are more likely to not get genitourinary specific imaging, which is a crucial diagnostic step in all urologic trauma guidelines. However, even some patients with urology consultation never get this definitive diagnostic imaging. This is an opportunity for us to work together to develop better protocols, as many patients both with and without urologic consultation are not receiving appropriate initial work up. More generally, this study poses an important question that can be addressed at other trauma centers and for other injury types. Treatment of trauma is shared between many departments and excellent communication is necessary for best outcomes.
Conclusion
Our data demonstrate that, although not a major determinant in LOS, urology service consultation plays an important role in the management of LUTI with high AAST injury scale. While more studies are needed to look at the degree of urology service involvement in the management of LUTI, we recommend a urological consultation be initiated for severe LUTI or when the management of injuries is out of the comfort zone of the trauma surgeons. Lastly, whether urologic consultation is obtained or not, there is room for improvement in the appropriate work up of lower urinary tract injury in the patient with poly-trauma.
References
Johnsen NV, Dmochowski RR, Young JB et al (2017) Epidemiology of blunt lower urinary tract trauma with and without pelvic fracture. Urology 102:234–239
Kong JP, Bultitude MF, Royce P, Gruen RL, Cato A, Corcoran NM (2011) Lower urinary tract injuries following blunt trauma: a review of contemporary management. Rev Urol 13(3):119–130
Zaid UB, Bayne DB, Harris CR et al (2015) Penetrating trauma to the ureter, bladder, and urethra. Curr Trauma Rep 1(2):119–124
Lumen N, Kuehhas FE, Djakovic N et al (2015) Review of the current management of lower urinary tract injuries by the EAU trauma guidelines panel. Eur Urol 67(5):925–929
Johnsen NV, Young JB, Reynolds WS, Kaufman MR, Milam DF, Guillamondegui OD, Dmochowski RR (2016) Evaluating the role of operative repair of extraperitoneal bladder rupture following blunt pelvic trauma. J Urol 195(3):661–665. https://doi.org/10.1016/j.juro.2015.08.081
Morey AF, Hernandez J, McAninch JW (1999) Reconstructive surgery for trauma of the lower urinary tract. Urol Clin N A 26(1):49–60
Gomez RG, Ceballos L, Coburn M et al (2004) Consensus statement on bladder injuries. BJU Int 94:27–32
Udekwu PO, Gurkin B, Oller DW (1996) The use of computed tomography in blunt abdominal injuries. Am Surg 62:56–59
Corriere JN, Sandler CM (1986) Management of the ruptured bladder: seven years of experience with 111 cases. J Trauma 26:830–833
Cass A, Luxenberg M (1987) Features of 164 bladder ruptures. J Urol 138(4 Part 1):743–745
Bjurlin MA, Fantus RJ, Mellett MM, Goble SM (2009) Genitourinary injuries in pelvic fracture morbidity and mortality using the National Trauma Data Bank. J Trauma 67:1033–1039
Sandler CM, Goldman SM, Kawashima A (1998) Lower urinary tract trauma. World J Urol 16(1):69–75
Morey AF, Iverson AJ, Swan A, Harmon WJ, Spore SS, Bhayani S, Brandes SB (2001) Bladder rupture after blunt trauma: guidelines for diagnostic imaging. J Trauma Acute Care Surg 51(4):683–686
Auerbach AD, Rasic MA, Sehgal N, Ide B, Stone B, Maselli J (2007) Opportunity missed. Arch Intern Med 167(21):2338
Andrich DE, Day AC, Mundy AR (2007) Proposed mechanisms of lower urinary tract injury in fractures of the pelvic ring. BJU Int 100:567–573
Morshed S, Knops S, Jurkovich GJ, Wang J, MacKenzie E, Rivara FP (2015) The impact of trauma-center care on mortality and function following pelvic ring and acetabular injuries. JBJS 97(4):265–272
Horiguchi A, Shinchi M, Masunaga A, Okubo K, Kawamura K, Ojima K, Azuma R (2017) Primary realignment for pelvic fracture urethral injury is associated with prolonged time to urethroplasty and increased stenosis complexity. Urology 108:184–189
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Michael Ernst, Amanda Sherman, Teresa Danforth, and W. Alan Guo declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ernst, M., Sherman, A., Danforth, T. et al. Lower urinary tract injury: is urology consultation necessary?. Int Urol Nephrol 52, 489–494 (2020). https://doi.org/10.1007/s11255-019-02326-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-019-02326-8