Abstract
Purpose
To evaluate the predictive value of attenuation value (HU) in renal pelvis urine for detecting renal pelvis urine culture (RPUC) positivity in obstructed urinary systems.
Methods
The study group consisted of patients who had nephrostomy insertion performed because of obstructed system and suspicion of pyonephrosis and percutaneous nephrolithotomy (PCNL) patients who had obstructed calculi. Group 1 consisted of RPUC positive 28 patients during nephrostomy insertion or needle access in PCNL and group 2 consisted of 23 patients with negative RPUC. RPUC results and non-contrast computed tomography measurements [Hounsfield unit (HU)] were compared between group 1 and group 2. A cut-off value was determined for HU. All patients were grouped according to whether they were above or below this value.
Results
The median HU calculated from the renal pelvis was − 8.5 (range − 29/− 1) and 10 (range− 4/+ 17) (p < 0.001) in group 1 and group 2, respectively. The cut-off value of HU that predicted positive RPUC was 0. Sensitivity and specificity of HU when considering this cut-off value were 100% and 96%, respectively (p < 0.001). Whereas RPUC positivity was found in 96.6% (28/29) of patients with HU < 0, there were no patients with HU > 0 where RPUC positivity was detected (p < 0.001).
Conclusion
In this cohort, we found that HU of the urine in the renal pelvis can be used to predict RPUC positivity.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Any blockage in the upper urinary tract may cause hydronephrosis, which leads to incomplete destruction of bacteria and an increase in bacterial resistance [1]. The bacterial overgrowth in the obstructed system may then cause pyonephrosis which is a urological emergency. This can rapidly progress to urosepsis and septic shock. It was reported that urinary tract obstruction was the underlying cause in up to 85% of patients who develop urosepsis and shock [2,3,4]. The septic shock associated mortality rate can be up to 50% [5,6,7,8]. If bacterial overgrowth can be detected by any method patients can be treated with antibiotics prior to any intervention or drainage. Negative urethral urine susceptibility test results do not correlate well with upper urinary tract infection [9]. Especially in obstructed systems, the renal pelvis urine culture (RPUC) can be positive although the micturated urine culture (MUC) is sterile.
So, it is important to detect significant bacterial presence in the obstructed system before the clinical signs appear. In a recent study, we showed that the attenuation value [Hounsfield unit (HU)] of urine can be used to predict the culture positivity with high sensitivity and specificity [10]. We aimed to study the predictive role of HU of renal pelvis urine in detecting RPUC positivity in obstructed urinary systems.
Methods
A total of 31 patients with percutaneous nephrostomy insertion (PCN) performed because of obstructive urinary tract infection (UTI) and 22 patients with obstructed calculi who underwent PCNL between Feb 2017 and May 2018 were retrospectively evaluated. Patients were divided into two groups according to the presence of positive or negative RPUC. Group 1 consisted of RPUC positive patients with PCN insertion or needle access in PCNL and group 2 consisted of RPUC negative patients during these interventions (Fig. 1). Patients in both groups were evaluated for non-contrast computed tomography (NCCT) images, MUC, urine analysis, RPUC, leukocytosis and fever. Patients with contrast-enhanced CT were not included in the study because the enhancement can change the attenuation values. Patients with inadequate dilatation (Grade 1 hydronephrosis) were not included in the study. Also patients with the lack of RPUC results and who had positive preoperative urine culture and treated with antibiotics were excluded from the study in PCNL patients.
When clinical improvement was not detected in patients with obstructive urinary tract infection within 48–72 h of adequate antimicrobial treatment and/or there was progress into urosepsis, a drainage procedure was performed under the guidance of ultrasonography. All cases of PCN were performed under ultrasonographic guidance with local anesthesia with the patient in a prone or prone-oblique position.
This study was approved by the Institutional Review Boards of HSU Izmir Bozyaka Training and Research Hospital.
Informed consent was obtained from all individual participants included in the study prior to surgery.
Imaging technique
The imaging data were gathered from our electronic imaging database system. A 64 detector CT scanner (Toshiba®Aquilion64) was used for all cases. Unprocessed data acquired on axial plane with a slice thickness of 1 mm were processed and 5 mm axial and 3 mm slice coronal and sagittal images were obtained from non-contrast CT images. In addition, antero-posterior renal pelvis diameter and renal pelvis area were measured on NCCT images using the same system.
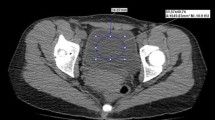
An ellipse-shaped line that included all the urine inside the renal pelvis was created and HU was calculated on axial NCCT images (Fig. 2).
All CT scans were reviewed by two experienced urologists blindly and the HU were gathered from the PACS system which were calculated automatically and the results were analyzed according to the mean of these two values. The HU value measured from the mentioned localization was calculated for every patient and the relation between HU and RPUC positivity was investigated.
Microbiological diagnosis
Urine culture was performed using 5% sheep blood agar and eosin-methylene blue agar and incubated at 37 °C for 18–24 h. The results were quantitatively evaluated [11]. The bacterial growth of ≥ 105 cfu/ml was determined as positive and as an inclusion criterion for the study. Two groups were compared in terms of white blood cell (WBC), presence of diabetes mellitus, hydronephrosis degree and pelvis antero-posterior (AP) diameter.
Statistical analysis
Data were analyzed using the Statistical Package for Social Sciences, version 20.0 (SPSS, Chicago,Ill) software program. The Mann–Whitney U test and Chi-square test were used for comparing RPUC positive and negative groups. Receiver operating characteristic (ROC) Curve analysis was performed to determine the cut-off value for HU and to calculate the sensitivity and specificity rates for predicting positive RPUC. Patients were grouped according to the cut-off value. Group 1 included patients with HU results under the cut-off value. Group 2 included patients with HU results above the cut-off value. The Mann–Whitney U test and Chi-square test were also applied to compare the results of these two groups. Statistical significance was defined as p < 0.05.
Results
The mean age of all patients was 53.5 (27–80) years and 12 of these were female. The comparison of data between the two groups is shown in Table 1. The minimum and maximum duration between the CT scan and the intervention was 2 days and 7 days, respectively. Two groups were similar for AP renal pelvis diameter, renal pelvis area, age and presence of DM. The presence of stones in group 1 and group 2 was 89.3% and 84%, respectively (p = 0.570). The RPUC positive patients had more leukocytosis and fever. The median HU calculated from the renal pelvis at the level of largest AP diameter on the axial images was − 8.5 (range − 29/− 1) and 10 (range − 4/+ 17 HU) (p < 0.001) in group 1 and group 2, respectively (Table 1).
The cut-off value of HU that predicts positive RPUC was calculated as 0 HU based on ROC curve analysis. Sensitivity and specificity of HU when considering this cut-off value were 100% and 96%, respectively (AUC: 0.989, p < 0.001) (Fig. 3).
Whereas RPUC positivity was found in 96.6% (28/29) of patients with HU < 0, there were no patients with HU > 0 with RPUC positivity detected (p < 0.001, OR = 0.04, CI = 0.006–0.273) (Table 2). The comparison of HU with RPUC results is illustrated in Fig. 4.
Discussion
The MUC may be negative in patients with urinary obstruction although infection persists in the upper system. In 10.1% of patients RPUC were positive and preoperative MUC were negative [9]. This data resulted from that study confirms the mentioned theory. Not all the patients with a positive RPUC may necessarily have signs and symptoms of infection, so not all of them received antibiotics prior to surgery. The patients who were given antibiotherapy due to signs and symptoms of urinary infection were excluded from the study, as stated in the material and method section.
Radiological examinations are important because a quick result can be obtained. In pyelonephritis, CT imaging is often associated with nonspecific findings such as thickening of the renal pelvis and stranding of perirenal fat [12,13,14].
The Hounsfield scale of tissue density is related to two values: air with − 1000 HU (minimum HU value) and water with 0 HU. Density of other tissues varies around this range, usually from − 1000 to + 1000 HU (− 1024 to 1024 or 3072 according to the coding of the particular vendor) [15]. HU can be used in a variety of clinical applications [16,17,18,19].
In their population-based study, Zeb et al. calculated HU in the evaluation of fatty liver disease and they concluded that fatty liver can be diagnosed using NCCT [16]. Pickhard et al. showed that lower CT attenuation values were related with osteoporosis [17]. In urological practice, CT attenuation values were used for predicting urinary stone composition and success of extracorporeal shock wave lithotripsy [19].
HU on NCCT can be performed to differentiate the substances in the ascites. Mizimura et al. found that intraabdominal acid due to bladder rupture could be differentiated by HU measurement on NCCT. In their study, the value of ascites in patients with bladder rupture (median 5.7; range 3.1−6.1) was significantly lower compared with cases diagnosed with gastrointestinal perforation and intestinal ischemia [20].
We investigated the correlation of bladder urine HU on NCCT images with MUC results in a recent published study. As a result, our study showed that when a cut-off value of − 1 is used for HU, MUC positivity can be predicted with 92.9% sensitivity and 100% specificity (AUC: 0.977, p < 0.001). In that study, MUC was positive in all patients with HU < − 1; however, only 6.2% of those with HU > − 1 had MUC positivity (p < 0.001, OR: 14) [10].
In another paper published by Yuruk et al. the authors found that the HU of the renal pelvis in patients with pyonephrosis and urine culture positivity obtained during nephrostomy insertion was significantly higher than for patients with hydronephrosis (13.51 ± 13.29 vs. 4.67 ± 5.37, p = 0.0001). A HU of 9.21 or over diagnosed pyonephrosis accurately with 65.96% sensitivity and 87.93% specificity [21]. This study had some limitations. Contrast-enhanced CT was used in most of the patients except the ones with contrast allergy in the mentioned study, while non-contrast CT was used without exception for imaging in our study. It is known that there are three phases of contrast media excretion including the vascular, nephro-graphic, and pyelographic phases. The pyelographic or excretory phase is reached 3 min after injection of IV contrast material [22]. It is impossible to determine the exact time for the pyelographic phase of contrast material excretion and, furthermore, the HU of the renal pelvis changes with contrast material excretion in the collecting system. In our study the attenuation values had lower values, whereas in the study mentioned above attenuation values were 13.51 ± 13.29 in patients with culture positivity. This can be attributed to imaging with contrast-enhanced CT in that study.
In this study, we concluded that when the cut-off value for HU was considered as 0, the sensitivity and specificity of HU was 100% and 96%, respectively. The evaluation of HU on NCCT can be practically achieved as we have mentioned. It is definitely not our aim to suggest CT imaging to diagnose UTI. Nevertheless, for patients with an acute incident which may be related to urinary tract symptoms, when the patient undergoes NCCT, the evaluation of HU may provide additional information to the clinician for the probable diagnosis of UTI. The results of the recent study implicate the importance of CT-imaging in acute evaluation of pyonephrosis. Using the HU in addition to the classical parameters (thickening of the renal pelvis and stranding of the perirenal fat) for pyonephrosis in CT-imaging allows responsible physicians to make earlier diagnosis and earlier interventions. In addition, knowledge about UTI is important preoperatively in renal stone patients with urinary system obstruction, because in the case of purulent urine being found during access the operation is postponed. Using the method we explained if UTI present physicians can place a nephrostomy tube and plan antibiotherapy and avoid unnecessary operations. This information may be used to discover patients who will need preoperative nephrostomy tube placement prior to a PCNL procedure.
The mechanism that leads to attenuation values becoming negative for renal pelvic urine in patients with upper tract infection is unknown. In our opinion, it can be attributed to bacterial load and/or disintegrated urine molecules by the colonizing bacteria.
The current study has some limitations; a limited number of patients were included because of the strict inclusion criteria, there was no control NCCT after treatment and the design was retrospective.
Conclusions
In this study, we found that the HU value of urine in the renal pelvis may predict the RPUC positivity. This information may be used to determine patients who will need preoperative nephrostomy tube placement prior to a PCNL procedure. Future studies are necessary to understand what may cause this decrease in attenuation when urine is infected.
References
Reyner K, Heffner AC, Karvetski CH (2016) Urinary obstruction is an important complicating factor in patients with septic shock due to urinary infection. Am J Emerg Med 34:694
Wagenlehner FM, Pilatz A, Weidner W (2011) Urosepsis—from the view of the urologist. Int J Antimicrob Agents 38:51–57
Hoffmann H, Schmoldt S, Trülzsch K, Stumpf A, Bengsch S, Blankenstein T et al (2005) A Nosocomial urosepsis caused by Enterobacter kobei with aberrant phenotype. Diagn Microbiol Infect Dis 53:143–147
Serniak PS, Denisov VK, Guba GB, Zakharov VV, Chernobrivtsev PA, Berko EM et al (1990) The diagnosis of urosepsis. Urol Nefrol 4:9–13
Brun-Buisson C (2000) The epidemiology of the systemic inflammatory response. Intensive Care Med 26:64–74
Brun-Buisson C, Doyon F, Carlet J (1996) Bacteremia and severe sepsis in adults: a multicenter prospective survey in ICUs and wards of 24 hospitals. French Bacteremia-Sepsis Study Group. Am J Respir Crit Care Med 154:617–624
Rangel-Frausto MS, Pittet D, Costigan M, Hwang T, Davis CS, Wenzel RP et al (1995) The natural history of the systemic inflammatory response syndrome (SIRS). A prospective study. JAMA 273:117–123
Sands KE, Bates DW, Lanken PN, Graman PS, Hibberd PL, Kahn KL et al (1997) Academic Medical Center Consortium Sepsis Project Working Group. Epidemiology of sepsis syndrome in 8 academic medical centers. JAMA 278:234–240
McDougall EM, Liatsikos EN, Dinlenc CZ, Smith AD (2002) Percutaneous approaches to the upper urinary tract. In: Walsh PC, Retik AB, Vaughan ED, Wein AJ (eds) Campbell’sUrology, 8th edn. W.B. Saunders Company, Philadelphia, pp 3327–3452
Basmaci I, Bozkurt IH, Sefik E, Celik S, Yarimoglu S, Degirmenci T (2018) A novel use of attenuation value (Hounsfield unit) in non-contrast CT: diagnosis of urinary tract infection. Int Urol Nephrol 50:1557–1562
Garcia LS, Isenberg HD (2010) Clinical Microbiology Procedures Handbook, 3rd edn. ASM Press, Washington DC
Kaplan DM, Rosenfield AT (1997) Smith RC Advances in the imaging of renal infection: helical CT and modern coordinated imaging. Infect Dis Clin North Am 11:681–705
Fultz PJ, Hampton WR (1993) Totterman SM Computed tomography of pyonephrosis. Abdom Imaging 18:82–87
Kawashima A, Sandler CM, Ernst RD, Goldman SM, Raval B, Fishman EK (1997) Renal inflammatory disease: the current role of CT. Crit Rev Diagn Imaging 38:369–415
Hounsfield GN (1980) Nobel lecture, 8 December 1979. Computed medical imaging. J Radiol 61:459–468
Zeb I, Li D, Nasir K, Katz R, Larijani VN, Budoff MJ (2012) Computed tomography scans in the evaluation of fatty liver disease in a population based study: the multi-ethnic study of atherosclerosis. Acad Radiol 19:811–818
Pickhardt PJ, Pooler BD, Lauder T, del Rio AM, Bruce RJ, Binkley N (2013) Opportunistic screening for osteoporosis using abdominal computed tomography scans obtained for other indications. Ann Intern Med 158:588–595
Bruni SG, Patafio FM, Dufton JA, Nolan RL (2013) Islam O The assessment of anemia from attenuation values of cranial venous drainage on unenhanced computed tomography of the head. Can Assoc Radiol J 64:46–50
Ouzaid I, Al-qahtani S, Dominique S, Hupertan V, Fernandez P, Hermieu JF et al (2012) A 970 Hounsfield units (HU) threshold of kidney stone density on non-contrast computed tomography (NCCT) improves patients’ selection for extracorporeal shockwave lithotripsy (ESWL): evidence from a prospective study. BJU Int 110:438–442
Mizumura N, Okumura S, Toyoda S, Imagawa A, Ogawa M, Kawasaki M (2016) Non-traumatic bladder rupture showing less than 10 Hounsfield units of ascites. Acute Med Surg 4:184–189
Yuruk E, Tuken M, Sulejman S, Colakerol A, Serefoglu EC, Sarica K (2017) Computerized tomography attenuation values can be used to differentiate hydronephrosis from pyonephrosis. World J Urol 35:437–442
Yuh BI, Cohan RH (1999) Different phases of renal enhancement: role in detecting and characterizing renal masses during helical CT. AJR Am J Roentgenol 173:747–755
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Author Basmaci I declares that he has no conflict of interest. Author Sefik E declares that he has no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Basmaci, I., Sefik, E. A novel use of attenuation value (Hounsfield unit) in non-contrast CT: diagnosis of pyonephrosis in obstructed systems. Int Urol Nephrol 52, 9–14 (2020). https://doi.org/10.1007/s11255-019-02283-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-019-02283-2