Abstract
Purpose
To investigate the preventive effect of probucol combined with hydration on contrast-induced nephropathy (CIN) in patients with coronary heart disease undergoing percutaneous coronary intervention (PCI).
Methods
A total of 641 patients undergoing PCI were randomly assigned to either a probucol group (probucol 500 mg twice daily and hydration; n = 321) or a control group (hydration only; n = 320). The primary endpoint was the incidence of CIN, defined as an increase in serum creatinine (Scr) by ≥ 44.2 μmol/L or ≥ 25% within 72 h after the administration of contrast agent. Secondary endpoints were changes in Scr, cystatin-C (Cys-C), creatinine clearance rate (Ccr), C-reactive protein (CRP), superoxide dismutase (SOD), and glutathione (GSH) within 72 h, and major adverse events during hospitalization or the 14-day follow-up period.
Results
The incidence of CIN was 4.0% (13/321) in the probucol group and 10.9% (35/320) in the control group. The probucol group had lower Cys-C and higher Ccr at 48 and 72 h after PCI compared with the control group. At 48 and 72 h following the operation, Cys-C and CRP were lower in the probucol group compared with the control group, but Ccr, SOD, and GSH were higher. There were no differences in the incidence of major adverse events during hospitalization or the 14-day follow-up between the groups. Multivariate logistic regression analysis showed that probucol was an independent protective factor for CIN.
Conclusions
Probucol combined with hydration more effectively decreased the incidence of CIN in patients with coronary heart disease undergoing PCI compared with hydration alone.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Contrast-induced nephropathy (CIN) is a common complication after percutaneous coronary intervention (PCI), defined as an increase in serum creatinine (Scr) by ≥ 44.2 µmol/L or ≥ 25% within 72 h after administration of a contrast agent [1]. CIN has become the third leading cause of hospital-acquired renal injury, responsible for up to 11% of all causes of hospital-acquired renal injury [2]. CIN is associated with prolonged hospitalization as well as increased cardiovascular morbidity, renal morbidity, and all-cause mortality, with some patients requiring dialysis [3]. Strategies have been established to prevent CIN such as identifying high-risk patients who may develop CIN, reducing contrast agent volume, intensifying pre-procedural intravenous saline hydration, and using iso-osmolar contrast agent (iodixanol) along with bicarbonate hydration [4,5,6]. However, CIN is still a common serious complication after PCI, and effective preventive measures are important.
While the exact pathogenesis of CIN has not been determined, it is generally believed that contrast-mediated renal vasoconstriction, renal ischemia, inflammatory responses, and oxidative stress are the most important components of the pathophysiology of CIN [7, 8].
Probucol is a potent antioxidant and shows significant antioxidative stress and anti-inflammatory ability and improved renal vascular endothelial function [9, 10]. It is widely used in clinical practice for the prevention and treatment of atherosclerosis and diabetic nephropathy because of its strong antioxidative and lipid-lowering effects. Some studies report that probucol plays a prophylactic role in the development of CIN [11, 12], but most of these studies were single-center studies using small sample sizes. The complete nature of the preventive role of probucol in CIN remains unclear.
Given the potential role of oxidative stress in the pathophysiology of CIN and the antioxidant effects attributed to probucol, the current prospective, randomized controlled trial sought to determine whether oral probucol could reduce the incidence of CIN in patients with coronary heart disease undergoing elective PCI.
Methods
Study population
This study was approved by the ethics committees of Tianjin Chest Hospital, Tianjin First Central Hospital, Tianjin Fourth Central Hospital, and Teda International Cardiovascular Hospital. All participants provided written informed consent.
Patients undergoing non-emergent PCI at Tianjin Chest Hospital, Tianjin First Central Hospital, Tianjin Fourth Central Hospital, and Teda International Cardiovascular Hospital between January 2014 and December 2016 were screened for eligibility. Exclusion criteria were: used probucol within 1 week before PCI; allergy to contrast agent; emergency PCI; severe renal insufficiency (defined as creatinine clearance (Ccr) < 30 mL/min; Ccr = [140−age] × weight (kg)/[0.818 × Scr (μmol/L)] (× 0.85 if female); heart failure or left ventricular ejection fraction < 30%; hypotension (systolic blood pressure < 90 mmHg); balloon counter-pulsation treatment; thyroid dysfunction; recent exposure to contrast agent within 2 weeks; electrolyte imbalance; coagulopathy; cardiogenic shock; malignant neoplasms; and acute or chronic infection.
Study protocol
Eligible patients were randomly assigned to either the probucol group or the control group according to a computer-generated random sequence, which was carried out using undisclosed codes and recorded by a nurse. Both the physicians and patients were unaware of the group outcomes and treatment interventions. Because hydration is recognized as the most effective measure to prevent CIN, all enrolled patients were given intravenous sodium chloride at a rate of 1.0 mL−1 kg−1 h−1 from 12 h before to 12 h after the operation (at least 1000 mL hydration preoperatively and postoperatively). Patients in the probucol group received hydration and probucol (Qilu Pharmaceutical Co., Jinan, China) 500 mg twice daily at 1 day before and 3 days after the operation. Patients in the control group only received hydration. Drug delivery and hydration were performed by the nurses. The use of aspirin, clopidogrel, calcium antagonists, angiotensin-converting enzyme inhibitors, angiotensin receptor antagonists, beta receptor antagonists, statins, and diuretics was left to the discretion of the cardiologists and according to clinical requirements or recommendations in guidelines. A nonionic, low-osmolar iodinated contrast agent (ioversol; Jiangsu Hengrui Pharmaceutical Co., Nanjing, China) was used in all patients during the procedure. None of the patients received antioxidant intensive statins or N-acetylcysteine therapy. Blood samples were collected at admission and at 48 and 72 h after contrast exposure to measure the levels of blood urea nitrogen (BUN), Scr, cystatin-C (Cys-C), superoxide dismutase (SOD), glutathione (GSH), and C-reactive protein (CRP). Blood test was conducted at a single hospital laboratory, and laboratory staff was blind to the study protocol and patients. The highest Scr level at 48 and 72 h after contrast exposure was used to diagnose CIN.
Study endpoints
The primary endpoint was the incidence of CIN, defined as an increase in Scr by ≥ 44.2 µmol/L or ≥ 25% within 72 h after administration of the contrast agent. Secondary endpoints were changes in Scr, Cys-C, and Ccr within 72 h, and major adverse events (including all-cause mortality, adverse cardiac events, renal replacement therapy, internal bleeding, acute heart failure, emergency PCI or surgical coronary bypass after PCI, and cerebrovascular events) occurring during hospitalization and within the 14-day follow-up period.
Statistical analysis
Normally distributed continuous variables, expressed as mean ± standard deviations (SD), were analyzed using Student’s t tests. Non-normally distributed continuous variables, expressed as medians and interquartile ranges, were analyzed using nonparametric tests. Categorical data, expressed as percentages, were analyzed using Chi-squared or Fisher’s exact tests. Multivariate logistic regression analysis (method = forward: LR) was used to exclude the influence of confounding factors. A 95% confidence interval (95% CI) was constructed around the point estimate of the odds ratio. Those identified as independent predictors in previous studies were included in the multivariable model [13]. Based on earlier studies [14], it was determined that the incidence of CIN was 13% in the control group. We hypothesized that probucol could reduce the incidence of CIN to 5%. Accordingly, at least 269 patients from each group were required for the power of the test set at 0.95 and statistical level (two-sided) at 0.05. A P value < 0.05 was considered significant (two-sided). All statistical analyses were performed using SPSS software (ver. 20.0; SPSS, Inc., Chicago, IL, USA).
Results
Baseline characteristics
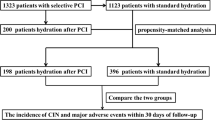
A total of 708 patients initially met inclusion criteria, with 67 meeting exclusion criteria and being excluded. Finally, 320 patients were randomly assigned to the control group and 321 to the probucol group. A flowchart of the study procedure is shown in Fig. 1. Baseline clinical, biochemical, procedural, and medication characteristics of the 641 patients are listed in Table 1. There were no significant differences in baseline characteristics between the two groups before PCI (P > 0.05).
Incidence of CIN and multiple logistic regression analysis
The incidence of CIN was 4.0% (13/321) in the probucol group and 10.9% (35/320) in the control group (χ 2 = 10.97, P = 0.01). Multivariate logistic regression analysis was used to analyze possible factors influencing CIN, including myocardial infarction, left ventricular ejection fraction < 45%, contrast volume, diuretics, Ccr < 60 mL/min, diabetes, hydration volume, hypertension, statins, age, and probucol. CIN was used as the dependent variable to exclude confounding factors. Multivariate logistic regression results showed that probucol was a protective factor of CIN (odds ratio 0.342, 95% CI: 0.174–0.672; P = 0.002) (Table 2).
Major adverse events during the in-hospital stay and 14-day follow-up period
Major adverse events occurred in seven patients (one death from cardiac rupture, four acute heart failure, one stroke, and one emergency PCI for acute thrombosis) in the probucol group and nine patients (one upper gastrointestinal bleeding, one ventricular fibrillation, six acute heart failure, and one temporary dialysis) in the control group during hospitalization and the 14-day follow-up period (2.2 vs. 2.8%; χ 2 = 0.263, P = 0.624). There were no significant differences between the two groups in the incidence of major adverse events.
Changes in BUN, Scr, Ccr, SOD, GSH, and CRP
Changes in BUN, Scr, Ccr, Cys-C, SOD, GSH, and CRP were compared between the two groups (Table 3). There were no significant differences in BUN, Scr, Ccr, Cys-C, SOD, GSH, and CRP at baseline between the probucol group and the control group before PCI. In both the probucol group and the control group at 48 and 72 h after the operation, Cys-C, CPR, SOD, and GSH were higher compared with baseline (P < 0.05), but Ccr decreased significantly after the operation in both groups (P < 0.05). At 48 h after the operation, Cys-C and CRP were lower in the probucol group compared with the control group (P < 0.05), but Ccr was higher (P < 0.05). At 72 h after the operation, CRP was lower in the probucol group compared with the control group (P < 0.05), and Ccr, SOD, and GSH were higher in the probucol group compared with the control group (P < 0.05).
Discussion
In this study, we found that administration of probucol 500 mg twice daily 1 day before and 3 days after the operation could reduce the incidence of CIN in patients undergoing a PCI. Probucol combined with hydration appeared is more effective at decreasing the incidence of CIN in patients with coronary heart disease undergoing PCI compared with hydration alone.
The exact pathogenesis of CIN has not been fully determined. It is thought that contrast-mediated inflammatory responses and oxidative stress are the most important factors contributing to the pathogenesis of CIN [7, 8]. Contrast agent filtered by glomeruli, actively taken up by renal tubular cells, and retained within cells and the peritubular space not only has a direct toxic action on renal tubular cells, increasing oxygen consumption, but also induces vasoconstriction of the vasa recta, decreasing oxygen delivery and inducing hypoxia. Contrast agent triggers a series of reactions that lead to the release of free radicals, causing renal cellular damage and initiating a vicious cycle of oxidative stress and inflammation. A possible treatment strategy for CIN could involve the use of medication that targets the regulators of both renal oxidative stress and inflammation [15, 16].
Probucol is a conventional agent for the reduction in elevated serum cholesterol and has the main chemical composition of 4,4′-[(1-methylethylidene)bis(thio)]bis-[2,6-bis(1,1-dimethylethyl)phenol]. Probucol has antioxidant and anti-inflammatory properties and has been shown to have clinical benefits such as regression of atherosclerosis and reduction in post-angioplasty restenosis in coronary arteries [17, 18]. It is widely used in clinical practice for the prevention and treatment of atherosclerosis [19] and diabetic nephropathy [20] because of its strong antioxidative and lipid-lowering effects. Recent studies have reported that probucol could decrease the incidence of CIN in patients undergoing coronary angiography or PCI. A randomized clinical trial involving 205 patients undergoing coronary angiography or intervention reported that the incidence of CIN was slightly lower in the probucol group compared with the control group (7.84 vs. 14.56%). While not being statistical significant, the post-procedure mean peak of Scr (1.15 ± 0.49 vs. 1.33 ± 0.78 mg/dL; P = 0.04) and the post-procedure increase in Scr from baseline (0.15 ± 0.22 vs. 0.25 ± 0.21 mg/dL; P = 0.001) in the probucol group were significantly lower than those in the control group [21]. In contrast, Yin et al. [22] found that probucol significantly reduced the incidence of CIN (defined as an increase in Scr ≥ 25% or an absolute increase of ≥ 0.5 mg/dL (≥ 44.2 μmol/L) within 72 h) in high-risk CIN patients with acute coronary syndrome undergoing primary or urgent angioplasty (4.2% (4/96) vs. 21.3% (23/108); P < 0.001), and the incidence of Csy-C-based CIN, defined as an increase in serum Csy-C ≥ 10% from baseline within 72 h, was significantly lower in the probucol group (29.2 vs. 51.9%; P < 0.001) compared with the control group. In addition, Li Hong et al. [23] found that probucol combined with atorvastatin could reduce serum uric acid levels and improve contrast-induced acute kidney injury in patients undergoing coronary angiography or PCI.
The findings of the current study are consistent with the studies noted above, with the incidence of CIN being lower in the probucol group than in the control group (4.0 vs. 10.9%; P < 0.05). At 48 and 72 h after the operation, Cys-C was lower in the probucol group compared with the control group (P < 0.05), but Ccr was higher (P < 0.05). These results suggest that probucol treatment was associated with a significantly lower incidence of CIN and had a renoprotective effect.
CRP is a sensitive marker of the inflammatory response [24] and is closely associated with CIN [25]. SOD and GSH are indicators of oxidative stress, which can remove oxygen free radicals and prevent lipid peroxidation. In the current study, both the probucol and control groups had higher CRP, SOD, and GSH at 48 and 72 h after the operation compared with baseline (P < 0.05), indicating that inflammation and oxidative stress occurred after contrast agent exposure. At 48 and 72 h after the operation, CPR was lower in the probucol group compared with the control group (P < 0.05), but SOD and GSH were higher compared with the control group (P < 0.05), indicating that treatment with probucol had a certain anti-inflammatory and antioxidative effect. Wang et al. [26] administered probucol to a rat model of CIN and found that it effectively protected renal function, reduced 24-h urinary protein, increased SOD in renal tissue, decreased malondialdehyde content, reduced the proportion of 8-hydroxy-2-deoxyguanosine-positive tubules, and reduced the typical pathological changes associated with CIN, such as tubular epithelial vacuolar degeneration, brush border disintegration and shedding, and mitochondria swelling. Another experimental animal study reported that probucol attenuated the inhibition of renal glutathione peroxidase activity by high iodinated osmolar contrast agent [27]. Recently, a randomized clinical study reported that probucol combined with telmisartan more effectively reduced urinary protein levels than telmisartan alone in patients with diabetic nephropathy by antioxidative stress damage [28]. Taken together, we suggest that the renoprotective effect of probucol may be associated with its antioxidative effect.
This study had some limitations. First, the study excluded patients with severe renal insufficiency (Ccr < 30 mL/min), severe heart failure (left ventricular ejection fraction < 30%), hypotension (systolic blood pressure ≤ 90 mmHg), and emergency PCI. This means that the preventive effects of probucol observed in this study cannot be generalized to patients at high risk of CIN. Second, we only measured CRP, SOD, and GSH; the exact preventive mechanism of probucol on CIN requires further study. Third, the study was not a double-blind study. Therefore, the results need to be validated in larger double-blind multicenter studies.
In conclusion, prophylactic administration of probucol may prevent CIN in coronary heart disease patients undergoing PCI.
References
Wang J, Ai X, Li L, Gao Y, Sun N, Li C, Sun W (2017) Alprostadil protects type 2 diabetes mellitus patients treated with metformin from contrast-induced nephropathy. Int Urol Nephrol. doi:10.1007/s11255-017-1639-2
Nash K, Hafeez A, Hou S (2002) Hospital-acquired renal insufficiency. Am J Kidney Dis 39(5):930–936
Firouzi A, Maadani M, Kiani R, Shakerian F, Sanati HR, Zahedmehr A, Nabavi S, Heidarali M (2015) Intravenous magnesium sulfate: new method in prevention of contrast-induced nephropathy in primary percutaneous coronary intervention. Int Urol Nephrol 47(3):521–525
Bei W, Li H, Lin K (2017) Post-Hoc Study: intravenous Hydration Treatment in Chinese Patients with High Risk of Contrast-Induced Nephropathy Following Percutaneous Coronary Intervention. Sci Rep 7(3):45023
Song T, Song M, Ge Z (2017) Comparison of the nephrotoxic effects of iodixanol versus iohexol in patients with chronic heart failure undergoing coronary angiography or angioplasty. J Interv Cardiol 30(3):281–285
Owen RJ, Hiremath S, Myers A (2014) Canadian Association of Radiologists consensus guidelines for the prevention of contrast-induced nephropathy: update 2012. Can Assoc Radiol J 65(2):96–105
Heyman SN, Rosen S, Khamaisi M, Idée JM, Rosenberger C (2010) Reactive oxygen species and the pathogenesis of radio contrast-induced nephropathy. Invest Radio 145(4):188–195
Liu YH, Jiang L, Chen JY, Tan N, Liu Y, He PC (2016) Does N-terminal pro-brain natriuretic peptide add prognostic value to the Mehran risk score for contrast-induced nephropathy and long-term outcomes after primary percutaneous coronary intervention? Int Urol Nephrol 48(10):1675–1682
He P, Kawamura H, Takemoto M, Maezawa Y, Ishikawa T, Ishibashi R, Sakamoto K, Shoji M, Hattori A, YamagaM Ide S, Ide K, Hayashi A, Tokuyama H, KobayashiK Yokote K (2016) Combination ofcilostazol and probucol protected podocytesfromlipopolysaccharide-induced injury by both anti-inflammatory and anti-oxidative mechanisms. J Nephroldoi. doi:10.1007/s40620-016-0361-y
Zhang Q, Chen L, Si Z, Bu H, Narasimhulu CA, Song X, Cui MY, Liu H, Lu T, He G, Parthasarathy S, Cui L, Liu Z, Cui Y (2016) Probucol protects endothelial progenitor cells against oxidized low-density lipoprotein via suppression of reactive oxygen species formation in vivo. Cell Physiol Biochem 39(1):89–101
Lee HC, Sheu SH, Liu IH, Lee CC, Hsieh CC, Yen HW, Lai WT, Chang JG (2012) Impact of short-duration administration of N-acetylcysteine, probucol and ascorbic acid on contrast-induced cytotoxicity. J Nephrol 25(1):56–62
Navarese EP, Gurbel PA, Andreotti F, Kołodziejczak MM, Palmer SC, Dias S, Buffon A, Kubica J, Kowalewski M, Jadczyk T, Laskiewicz M, Jędrzejek M, Brockmeyer M, Airoldi F, Ruospo M, De Servi S, Wojakowski W, O’ Connor C, Strippoli GF (2017) Prevention of contrast-induced acute kidney injury in patients undergoing cardiovascular procedures-a systematic review and network meta-analysis. PLoS ONE 12(2):e0168726
Toprak O (2017) Risk markers for contrast-induced nephropathy. Am J Med Sci 334(4):283–290
Su X, Xie X, Liu L, Lv J, Song F, Perkovic V, Zhang H (2017) Comparative effectiveness of 12 treatment strategies for preventing contrast-induced acute kidney injury: a systematic review and Bayesian network meta-analysis. Am J Kidney Dis 69(1):69–77
Pflueger A, Abramowitz D, Calvin AD (2009) Role of oxidative stress in contrast-induced acute kidney injury in diabetes mellitus. Med Sci Monit 15(6):125–136
Liu Y, Tan N, Zhou YL (2012) High-sensitivity C-reactive protein predicts contrast-induced nephropathy after primary percutaneous coronary intervention. J Nephrol 25(3):332–340
Kasai T, Miyauchi K, Kubota N, Kajimoto K, Amano A, Daida H (2012) Probucol therapy improves long-term (> 10-year) survival after complete revascularization: a propensity analysis. Atherosclerosis 220(2):463–469
Liu J, Li M, Lu H, Qiao W, Xi D, Luo T, Xiong H, Guo Z (2015) Effects of probucol on restenosis after percutaneous coronary intervention: a systematic review and meta-analysis. PLoS ONE 10(4):e0124021
Adameova A, Xu YJ, Duhamel TA, Tappia PS, Shan L, Dhalla NS (2009) Anti-atherosclerotic molecules targeting oxidative stress and inflammation. Current Pharm Des 15(27):3094
Yoshida M, Kimura H, Kyuki K, Ito M (2006) Combined effect of probucol and insulin on renal damage in diabetic rats fed a high cholesterol diet. Eur J Pharmacol 48(1–3):174
Li G, Yin L, Liu T, Zheng X, Xu G, Xu Y, Yuan R, Che J, Liu H, Zhou L, Chen X, He M, Li Y, Wu L, Liu E (2009) Role of probucol in preventing contrast-induced acute kidney injury after coronary interventional procedure. Am J Cardiol 103(4):512
Yin L, Li G, Liu T, Yuan R, Zheng X, Xu G, Xu Y, Che J, Liu X, Ma X, Li F, Liu E, Chen X, Wu L, Fan Z, Ruan Y, He M, Li Y (2013) Probucol for the prevention of cystatin C-based contrast-induced acute kidney injury following primary or urgent angioplasty: a randomized, controlled trial. Int J Cardiol 167(2):426–429
Li H, Li X, Ma H, Wang Y, Fu N, Jin D, Cong H (2014) Atorpvastatin combining with probucol: a new way to reduce serum uric acid level during perioperative period of interventional procedure. Sci W J. doi:10.1155/2014/565367
Börekçi A, Gür M, Türkoğlu C, Çaylı M, Selek Ş, KaypaklıO Uçar H, Coşkun M, Şeker T, Koç M, Gökdeniz T, Gözükara MY (2015) Oxidative stress and paraoxonase 1 activity predict contrast-induced nephropathy in patients with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. Angiology 66(4):339–345
Jian-Wei Z, Yu-Jie Z, Shu-Jun C, Qing Y, Shi-Wei Y, Bin N (2014) Impact of preprocedural high-sensitivity C-reactive protein on contrast-induced nephropathy in patients undergoing primary percutaneous coronary intervention. Angiology 65(5):402–407
Wang N, Wei RB, Li QP, Yang X, Li P, Huang MJ (2015) Renal Protective Effect of Probucol in Rats with Contrast-Induced Nephropathy and its Underlying Mechanism. Med Sci Monit 21:2886–2892
Yen HW, Lee HC, Lai WT, Sheu SH (2007) Effects of acetylcysteine and probucol on contrast medium-induced depression of intrinsic renal glutathione peroxidase activity in diabetic rats. Arch Med Res 38(3):291–296
Zhu H, Chen X, Cai G, Zheng Y, Liu M (2016) Telmisartan combined with probucol effectively reduces urinary protein in patients with type 2 diabetes: a randomized double-blind placebo-controlled multicenter clinical study. J Diabetes 8(5):677
Acknowledgements
This study was funded by a grant from the Tianjin Municipal Health and Family Planning Commission (Grant Number: 14KG124). We thank Alexander Pishief, LLB, BBmedSc, from Liwen Bianji, Edanz Group China (www.liwenbianji.cn/ac), for editing the English text of a draft of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Human and animal rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Fu, N., Yang, S., Zhang, J. et al. The efficacy of probucol combined with hydration in preventing contrast-induced nephropathy in patients with coronary heart disease undergoing percutaneous coronary intervention: a multicenter, prospective, randomized controlled study. Int Urol Nephrol 50, 105–112 (2018). https://doi.org/10.1007/s11255-017-1718-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-017-1718-4