Abstract
Background
Volume overload is a common complication in patients with end-stage kidney disease who undergo maintenance dialysis therapy and associated with hypertension, left ventricular hypertrophy and mortality in this population. Although bioimpedance analysis (BIA), an objective method to assess overhydration, is associated with poor outcomes in observational studies, in randomized controlled trials (RCTs) the results were conflicting. We have examined the role of BIA for assessing the “dry weight” and fluid status in order to improve fluid overload in comparison with a control or clinical-based prescription in patients with ESKD receiving haemodialysis or peritoneal dialysis.
Methods
All RCTs and quasi-RCTs in which BIA was used to improve fluid overload and assess the effect on all-cause mortality, cardiovascular morbidity, systolic blood pressure and volume control and arterial stiffness were included.
Results
Seven RCTs with 1312 patients could be included in this review. In low-to-medium quality of the evidence, the use of BIA did not reduce all-cause mortality (relative risk 0.87, 95% CI 0.54–1.39) and had small to no effect on body change, but it improved systolic blood pressure control (mean difference (MD) −2.73 mmHg, 95% CI −5.00 to −0.46 mmHg) and reduce overhydration, as measured by BIA, with 0.43 L [(MD), 95% CI 0.71–0.15 L].
Conclusion
In ESKD patients, BIA-based interventions for correction of overhydration have little to no effect on all-cause mortality, whereas BIA improved systolic blood pressure control. Our results should be interpreted with caution as the size and power of the included studies are low. Further studies, larger or with a longer follow-up period, should be performed to better describe the effect of BIA-based strategies on survival.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
It is estimated that there are approximately 3 million patients with end-stage kidney disease (ESKD) in the world [1]. Although a decline in mortality has been observed in recent years, the mortality in patients starting dialysis is more than eight fold higher than in the general population [2] with more than 40% of deaths due to the cardiovascular causes [3].
Volume overload is the most common complication in ESKD ranging from 10 to 60% in previous studies [1, 4, 5] and is dependent on several factors, including sodium and fluid intake, cardiac function, residual kidney function, dialysate composition and ultrafiltration volume [1]. It is associated with hypertension, left ventricular (LV) hypertrophy and mortality in the dialysis population [6,7,8,9].
Clinical evaluation of fluid overload can be difficult in ESKD populations and prone to underestimation or overestimation. Objective methods have been proposed for defining fluid overload: inferior vena cava collapse index, left atrial volume on echocardiography, flat slopes on plasma volume slope monitoring, evaluation of NT-proBNP, lung ultrasonography or bioimpedance. The most utilized and increasingly validated approach to objectively assess (over) hydration is the use of bioimpedance. This technique has been used in different forms (single/multiple frequency, segmental/whole body) and is validated by isotope dilution methods, by accepted reference body composition methods and by techniques that measure relative changes in fluid volumes [10]. Bioelectrical impedance analysis (BIA) was also successfully used to guide HD patients towards normohydration and better blood pressure (BP) control [11].
Although initial observational studies have found an independent association between fluid overload and increased mortality in ESKD patients [12], the results from randomized trials are conflicting [13, 14]. Therefore, this review aims to critically analyse the benefits and harms of bioelectrical impedance analysis (BIA) measurements to guide fluid management in patients with ESKD receiving haemodialysis (HD) or peritoneal dialysis (PD).
Methods
We have conducted a systematic review and meta-analysis according to a previously published protocol (http://www.crd.york.ac.uk/PROSPERO/CRD42017067964). Also a Cochrane-based methodology [15] and previously published protocol was used as an example [16].
All randomized controlled trials (RCTs) and quasi-RCTs looking at BIA-based intervention to improve fluid status in people with ESKD will be eligible for inclusion.
Types of participants
Adults aged 18 years with ESKD and on chronic dialysis (>3 months).
Types of interventions
Studies assessing BIA-based strategies to improve fluid overload in comparison with a control or clinical-based prescription of a target weight were included.
Examples of interventions include BIA-based versus clinical-based prescription of target “dry weight” or BIA-based versus standard care prescription of target “dry weight”.
Types of outcome measures
Primary outcomes
-
1.
All-cause mortality.
-
2.
Cardiovascular morbidity [both fatal (myocardial infarction (MI), stroke, sudden death, congestive heart failure, arrhythmia) and non-fatal cardiovascular events (MI, stroke, congestive heart failure, arrhythmia)].
Secondary outcomes
-
1.
Measures of volume status or changes in body volume, including interdialytic weight gain (IDWG) or daily weight gain and bioimpedance measurements of extracellular water (ECW).
-
2.
Side effects, e.g. any symptomatic intradialytic hypotension (number of events and number of patients with events), nausea, vomiting, muscle cramps, restlessness, dizziness, fainting or anxiety [17] or any major adverse events as reported by the authors.
-
3.
BP control SBP, MAP, DBP in mm Hg, at end of intervention, or change between beginning and end of intervention; or number of patients achieving BP target. In HD studies, pre-HD SBP measurements will be used.
-
4.
Arterial stiffness, as assessed by pulse wave velocity, in m/s, at end of intervention, or change between beginning and end of intervention.
Search methods for identification of studies
We searched MEDLINE (to 1st of February 2017), clinicaltrials.gov website, the Cochrane Controlled Clinical Trials Register Database (through Issue 2 of 12, February2017), and hand-searched reference lists for relevant articles (Supplementary Table S1). We also wrote letters seeking information about unpublished or incomplete studies to investigators known to be involved in previous studies. There was no language restriction.
The titles and abstracts were screened independently by two authors. Two authors independently assessed retrieved abstracts and, if necessary the full text, of these studies to determine which studies satisfy the inclusion criteria.
Data extraction was carried out independently by two authors using standard data extraction forms. Studies reported in non-English language journals were translated before assessment. When more than one publication of one study exists, reports were grouped together and the publication with the most complete data was used in the analyses. Any discrepancy between published versions was highlighted.
Assessment of risk of bias in included studies was independently assessed by two authors using the Cochrane risk of bias assessment tool [15].
Measures of treatment effect
For dichotomous outcomes (e.g. death, cardiovascular events), results were expressed as risk ratio (RR) with 95% confidence interval (CI). Where continuous scales of measurement are used to assess the effects of treatment (IDWG, SBP), the mean difference (MD) was used, or the standardized mean difference (SMD) if different scales have been used. For continuous data, the preferred data were the end of treatment data. If data were reported at more than one time point during the study, all data were extracted. If outcome data for a study were reported for more than one period of follow-up, we performed subgroup analyses for different periods of follow-up (≤6 weeks, >6 weeks to 12 weeks, >12 weeks). If a study had more than two intervention arms, the control group sample size was split by the number of subgroup comparisons for that study [15].
Heterogeneity was analysed using a Chi-square test on N − 1 degrees of freedom, with an alpha of 0.05 used for statistical significance and with the I 2 test [18]. I 2 values of 25, 50 and 75 correspond to low, medium and high levels of heterogeneity. If possible, funnel plots were used to assess for the potential existence of small study bias [15]. Data were pooled using the random-effects model, but the fixed-effect model was used to ensure robustness of the model chosen and susceptibility to outliers.
If a sufficient number of studies are identified, subgroup analysis was used to explore possible sources of heterogeneity. The following subgroups were explored: dialysis modality: HD and PD, type of BIAs (type of device), endpoint measurement at different time points: ≤6 weeks, >6–12 weeks, >12 weeks, time on dialysis (dialysis vintage): <6 months versus >6 months, studies with high versus low risk of bias and geographical area: North America, Latin America, Asia, Europe.
We aimed to perform sensitivity analyses in order to explore the influence of the following factors on effect size: unpublished studies, taking account of risk of bias, excluding any very long or large studies.
Results
Description of studies
Results of the literature search
The systematic review yielded 171 references, 62 of which were considered potentially eligible after initial screening of titles and abstracts, and 12 relevant review articles were obtained for reference lists. Of the full-text articles screened, seven RCTs were included and six ongoing RCTs have been identified (Fig. 1).
Included studies
Seven studies were included in this systematic review, with five studies in HD (n = 844 patients) [13, 14, 19,20,21] and two in PD (n = 468 patients) [22, 23]. Six studies were published in English, and one study was in Portuguese. The overall mean age varied from 48.56 [19] to 62.7 years [20]. Mean dialysis vintage varied from 18 [23] to 107 months [13], and the study duration ranged from 12 [22] to 42 weeks [13]. All studies reported proportion of patients with hypertension or diabetes. BCM (multi-frequency impedance) was used in five out of seven studies [13, 14, 19, 20, 22]. Single-frequency bioimpedance methods were used in two studies [19, 23]. For one study, we found two reports, but only the most recent publication was included [13, 14]. The detailed baseline studies characteristics are presented in Tables 1 and 2.
Excluded studies
All the other studies were excluded due to study design (not a RCT), or due to interventions/populations that were not eligible (Fig. 1).
Risk of bias in included studies
Risks of bias in individual studies are shown in “Supplementary Figure 1”; a summary of the overall risks of bias is provided in Fig. 2. Trials generally had very serious limitations due to risks of bias in most domains leading to downgrading of overall evidence quality. The selection bias was unclear in five studies. Blinding of the participants was of high risk in three studies [21,22,23] since the access to measurements was not blinded and we considered that this might influence the clinical practice irrespective of the study arm or protocol. A high rate of dropout (>10%) and not using intention to treat analysis was considered of high risk of bias for four studies under attrition bias [20,21,22,23].
Serious adverse events were generally not reported with one exception [20].
Effects of interventions
All-cause mortality
For all-cause mortality, we included data from six studies [13, 14, 19,20,21, 23], with 1152 patients in total. BIA-based interventions had no significant effect on all-cause mortality (relative risk (RR) 0.87, 95% CI 0.54–1.39). Heterogeneity was low (I 2 = 0) (Fig. 3).
Cardiovascular mortality/morbidity
Insufficient data were reported/available in order to perform a cumulative meta-analysis on this outcome. Hur et al. [24] reported that six patients in the intervention group and four patients in the control group were hospitalized because of new cardiovascular events during the study period. Onofriescu et al. [13] reported one death from acute myocardial infarction and one death as sudden cardiac death in the clinical-methods group. For the bioimpedance group, no death was reported due to cardiovascular cause. Ponce et al. [21] reported that three patients died of acute myocardial infarction in the control group but do not report the number of events in the active group.
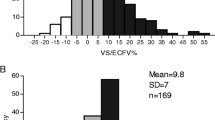
Measures of volume status or changes in body volume
Different ways of reporting this outcome were found: overhydration (L), ECW, ICW, E/I, relative fluid overload (RFO), percentage of patients overhydrated, etc. Using different methods to report changes in hydration status, all the included studies described a significant reduction in the overhydration status in the interventional arm (bioimpedance arm). For example, Onofriescu et al. [13] reported a significant decrease in relative fluid overload in the bioimpedance group, from 9.52 to 7.46% (mean difference, 2.05; 95% confidence interval [CI], 1.10–5.70%; p < 0.03). The cumulative analysis of the end of treatment level of overhydration showed a statistically significant 0.43 L less OH in the intervention arm (Fig. 4).
Effect on end of treatment body weight and change in body weight
Data regarding body weight, end of treatment value or changes during the follow-up were reported by five studies [14, 19, 20, 22, 23]. In the cumulative analysis, we found no significant difference between the standard care group and the BIA group (Fig. 5a for end of treatment body weight and Fig. 5b for change in body weight).
Blood pressure control
BIA-based interventions were associated with a 2.73 mmHg lower mean blood pressure in comparison with the control arm. The results were reported by all studies with 1197 patients in total (Fig. 6).
Effect on arterial stiffness
Hur et al. [14] and Onofriescu et al. [13] reported data on the end of treatment values of the arterial stiffness. The cumulative analysis showed a lower value in the intervention group, mean differences 1.18 m/s (95% CI −3.14, 0.78 m/s) (Fig. 7).
Side effects
Serious adverse events were not reported in any study. Darlan 2010 [19] reported no differences in terms of number of side effects between the two groups. The same results are reported by Sheng 2016 [20], Onofriescu 2014 [13] and Hur 2014 [14]. However, Luo 2011 [22] terminated their study early due to compelling benefits in the bioimpedance group regarding adverse effects and overall mortality although no data are presented to support this information). Sheng 2016 reported systematically intradialytic complications and found that no difference was found when comparing the incidence of hypotension events and cramping events [20].
Investigation for sources of heterogeneity and publication bias
The tests for heterogeneity were not found significant when considering all-cause mortality, SBP control and end of treatment body weight. However, supplemental analysis could not be performed due to insufficient data in the following domains: heterogeneity by length of follow-up, type of compounds or quality of trials. Importantly, detection of small study (either small sample size or low number of censored events) was limited by a paucity of data in this regard throughout the sampled literature.
Discussion
In this meta-analysis, we found that in ESKD patients, BIA-based interventions for correction of overhydration have little to no effect on all-cause mortality. Bioimpedance-based dry weight assessment was associated with lower blood pressure, lower end of treatment overhydration and reduced arterial stiffness, but did not significantly impact all-cause mortality, body weight or change in body weight in this systematic review and meta-analysis of seven studies with 1312 patients.
The topic of dry weight calculation is important because it guides treatment in dialysis populations. Fluid overload contributes heavily to mortality risk in ESKD patients. Classic clinical signs of overhydration such as peripheral oedema, hypertension or pulmonary congestion lack accuracy. Hence, BIA has emerged as an objective tool to assess fluid overload. BIA provides individualized fluid status/overload assessment on the basis of normal extracellular volume, taking into account their own body composition. It is highly reproducible, relatively inexpensive, easy to use and, importantly, has already been validated clinically [25]. Despite these favourable traits, there is still a paucity of robust evidence to guide implementation of this technology clinically (as seen by the current systematic review).
In observational studies, BIA-detected overhydration was associated with all-cause mortality [6, 9, 25, 26]. In their influential paper, Wizemann et al. showed that fluid overload, as assessed by BIA, is an important and independent predictor of mortality, secondary only to diabetes [9]. Onofriescu et al. indicated that this relationship is maintained even when adjustments for echocardiographic parameters are considered [25].
Unfortunately, the results of the current study seem to go against these initial positive findings. It is possible that the existing studies are underpowered to show the effect of BIA on all-cause mortality. Even the study by Onofriescu et al. [13], the only study that showed a beneficial effect of BIA use on survival was not powered enough to properly analyse this outcome.
Another possible explanation is related to the interpretation of BIA results. Although the CLIMB study showed that aggressive dry weight reduction can have deleterious effects [27] and BIA is the only method that provides data to avoid both overhydration as well as underhydration, it has been suggested that trends rather than absolute BIA measurements may be more meaningful [28].
Our analysis showed a beneficial effect of BIA related to a better control of blood pressure and possibly to a reduction in arterial stiffness estimates. Although BIA use was not associated with a reduction or change in total body weight in our analysis, the positive effect of this technique on the assessed vascular parameters could be secondary to changes in total body compartmental composition as showed by the reduction in the overall overhydration level. BIA does not differentiate between intravascular and interstitial extracellular water excess, and these beneficial effects could be associated with a better intravascular fluid control.
Potential limitations and sources of bias in the review process
To our knowledge, this is the first systematic review that assesses the benefits and harms of bioimpedance, when compared to standard care in adult population with ESKD. The main strengths of this review include the comprehensive searches of multiple databases and application of Cochrane methodology. Core outcome domains are reported as suggested by the recent international SONG-HD initiative [29]. We managed to include data from seven studies (one unpublished studies) with more than 1300 participants. Also, all the ongoing studies and observational data are presented in detail. Nevertheless, our review has some important limitations. We acknowledge that between studies, it is difficult to quantify how different these studies may have truly been with regard to the standard of care arms since practices may have varied widely. We acknowledge that the devices have not been cross-validated and estimation algorithms are proprietary but all of devices do present validation studies, previously published [30, 31]. Also, the included studies did not standardize BP measurements. The blood pressure comparison in the HD patients included pre-HD BP. It is arguable whether this is a useful metric of overall BP burden, chronic volume overload or even overall prognosis. Also, loss or residual kidney function was not included under outcomes and this might underestimate the medium to long-term risks related to reduction in overhydration.
The included studies had small sample sizes with short follow-up and variability of follow-up period. The amount of data available on patient-relevant outcomes (e.g. mortality, cardiovascular events, side effects) is limited and reported incompletely when available. Also, the quality of the included studies is low to medium level when looking at the risk of bias scale.
Conclusion
Bioimpedance-based dry weight assessment does not have a statistically significant effect on all-cause mortality in patients with end-stage kidney disease. However, this method can improve blood pressure control, overall overhydration and arterial stiffness measurements. Due to the small sample size of existing studies, larger studies with longer follow-up, possibly in combination with other promising methods such as lung ultrasonography, will likely shape the next generation of dry weight assessment in guiding fluid management for ESKD patients.
References
Ok E, Asci G, Chazot C, Ozkahya M, Mees EJ (2016) Controversies and problems of volume control and hypertension in haemodialysis. Lancet, London
de Jager DJ, Grootendorst DC, Jager KJ, van Dijk PC, Tomas LM, Ansell D et al (2009) Cardiovascular and noncardiovascular mortality among patients starting dialysis. JAMA 302(16):1782–1789
Collins AJ, Foley RN, Gilbertson DT, Chen SC (2015) United states renal data system public health surveillance of chronic kidney disease and end-stage renal disease. Kidney Int Suppl 5(1):2–7
Blake PG, Bargman JM, Brimble KS, Davison SN, Hirsch D, McCormick BB et al (2011) Clinical practice guidelines and recommendations on peritoneal dialysis adequacy 2011. Perit Dial Int J Int Soc Perit Dial 31(2):218–239
Wabel P, Moissl U, Chamney P, Jirka T, Machek P, Ponce P et al (2008) Towards improved cardiovascular management: the necessity of combining blood pressure and fluid overload. Nephrol Dial Transplant Off Publ Eur Dial Transpl Assoc Eur Ren Assoc 23(9):2965–2971
Chazot C, Wabel P, Chamney P, Moissl U, Wieskotten S, Wizemann V (2012) Importance of normohydration for the long-term survival of haemodialysis patients. Nephrol Dial Transplant Off Publ Eur Dial Transpl Assoc Eur Ren Assoc 27(6):2404–2410
Agarwal R (2010) Hypervolemia is associated with increased mortality among hemodialysis patients. Hypertension 56(3):512–517
Paniagua R, Ventura MD, Avila-Diaz M, Hinojosa-Heredia H, Mendez-Duran A, Cueto-Manzano A et al (2010) NT-proBNP, fluid volume overload and dialysis modality are independent predictors of mortality in ESRD patients. Nephrol Dial Transplant Off Publ Eur Dial Transpl Assoc Eur Ren Assoc 25(2):551–557
Wizemann V, Wabel P, Chamney P, Zaluska W, Moissl U, Rode C et al (2009) The mortality risk of overhydration in haemodialysis patients. Nephrol Dial Transplant Off Publ Eur Dial Transpl Assoc Eur Ren Assoc 24(5):1574–1579
Wabel P, Chamney P, Moissl U, Jirka T (2009) Importance of whole-body bioimpedance spectroscopy for the management of fluid balance. Blood Purif 27(1):75–80
Machek P, Jirka T, Moissl U, Chamney P, Wabel P (2010) Guided optimization of fluid status in haemodialysis patients. Nephrol Dial Transplant Off Publ Eur Dial Transpl Assoc Eur Ren Assoc 25(2):538–544
Marcelli D, Usvyat LA, Kotanko P, Bayh I, Canaud B, Etter M et al (2015) Body composition and survival in dialysis patients: results from an international cohort study. Clin J Am Soc Nephrol CJASN 10(7):1192–1200
Onofriescu M, Hogas S, Voroneanu L, Apetrii M, Nistor I, Kanbay M et al (2014) Bioimpedance-guided fluid management in maintenance hemodialysis: a pilot randomized controlled trial. Am J Kidney Dis Off J Natl Kidney Found 64(1):111–118
Hur E, Usta M, Toz H, Asci G, Wabel P, Kahvecioglu S et al (2013) Effect of fluid management guided by bioimpedance spectroscopy on cardiovascular parameters in hemodialysis patients: a randomized controlled trial. Am J Kidney Dis Off J Natl Kidney Found 61(6):957–965
Higgins JPT GSe (2011) Cochrane handbook for systematic reviews of interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.handbook.cochrane.org
Wong MMY, Craig JC, Levin A, Strippoli GFM. Interventions for promoting adherence to fluid intake and dietary salt restriction in people with end-stage kidney disease. Cochrane Database of Systematic Reviews. 2014(11)
Peritoneal Dialysis Adequacy 2006 Work Group (2006) Clinical practice guidelines for peritoneal adequacy, update 2006. Am J Kidney Dis 48(Suppl 1):S91–S97. doi:10.1053/j.ajkd.2006.05.016
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327(7414):557–560
Darlan F (2010) Comparacao da pressao arterial, aferida por mapa apos sessao de hemodialise, em pacientes submetidos a avaliacao clinica de bioimpedancia, para determinacao de peso seco. Dissertacao de Mestrado;Universidade Federal Do Rio Grande Do Sul
Huan-Sheng C, Yeong-Chang C, Ming-Hsing H, Fan-Lieh T, Chu-Cheng L, Tsai-Kun W et al (2016) Application of bioimpedance spectroscopy in Asian dialysis patients (ABISAD-III): a randomized controlled trial for clinical outcomes. Int Urol Nephrol 48(11):1897–1909
Ponce P, Pham J, Gligoric-Fuerer O, Kreuzberg U (2014) Fluid management in haemodialysis: conventional versus body composition monitoring (BCM) supported management of overhydrated patients. Port J Nephrol Hypertens 28:239–248
Luo YJ, Lu XH, Woods F, Wang T (2011) Volume control in peritoneal dialysis patients guided by bioimpedance spectroscopy assessment. Blood Purif 31(4):296–302
Tan BK, Yu Z, Fang W, Lin A, Ni Z, Qian J et al (2016) Longitudinal bioimpedance vector plots add little value to fluid management of peritoneal dialysis patients. Kidney Int 89(2):487–497
Hur E, Usta M, Toz H, Asci G, Wabel P, Kahvecioglu S et al (2013) Effect of fluid management guided by bioimpedance spectroscopy on cardiovascular parameters in hemodialysis patients: a randomized controlled trial. Am J Kidney Dis 61(6):957–965
Onofriescu M, Siriopol D, Voroneanu L, Hogas S, Nistor I, Apetrii M et al (2015) Overhydration, cardiac function and survival in hemodialysis patients. PLoS ONE 10(8):e0135691
Dekker MJ, Marcelli D, Canaud BJ, Carioni P, Wang Y, Grassmann A et al (2017) Impact of fluid status and inflammation and their interaction on survival: a study in an international hemodialysis patient cohort. Kidney Int 91(5):1214–1223
Reddan DN, Szczech LA, Hasselblad V, Lowrie EG, Lindsay RM, Himmelfarb J et al (2005) Intradialytic blood volume monitoring in ambulatory hemodialysis patients: a randomized trial. J Am Soc Nephrol JASN 16(7):2162–2169
Davies SJ, Garcia Lopez E, Woodrow G, Donovan K, Plum J, Williams P et al (2008) Longitudinal relationships between fluid status, inflammation, urine volume and plasma metabolites of icodextrin in patients randomized to glucose or icodextrin for the long exchange. Nephrol Dial Transpl 23(9):2982–2988
Tong A, Manns B, Hemmelgarn B, Wheeler DC, Evangelidis N, Tugwell P et al (2017) Establishing core outcome domains in hemodialysis: report of the standardized outcomes in nephrology-hemodialysis (SONG-HD) consensus workshop. Am J Kidney Dis 69(1):97–107
Moissl UM, Wabel P, Chamney PW, Bosaeus I, Levin NW, Bosy-Westphal A et al (2006) Body fluid volume determination via body composition spectroscopy in health and disease. Physiol Meas 27(9):921–933
Davies SJ, Davenport A (2014) The role of bioimpedance and biomarkers in helping to aid clinical decision-making of volume assessments in dialysis patients. Kidney Int 86(3):489–496
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Adrian Covic received speaker honoraria from Amgen, Roche, Fresenius Medical Care and Abbott and is a member of the European Renal Best Practices Board. All the other authors have nothing to declare.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Covic, A., Ciumanghel, AI., Siriopol, D. et al. Value of bioimpedance analysis estimated “dry weight” in maintenance dialysis patients: a systematic review and meta-analysis. Int Urol Nephrol 49, 2231–2245 (2017). https://doi.org/10.1007/s11255-017-1698-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-017-1698-4