Abstract
Introduction
Coverage decisions in publicly funded healthcare systems require a formal, systematic and transparent assessment process for policies related to distribution of resources. The process is complex and employs multiple types of information, such as clinical effectiveness, costs and health utility scores which are used to produce quality-adjusted life years. The purpose of this study was to create health utility scores for CKD patients within the Canadian population.
Methods
This is a cross-sectional study of CKD patients. We administered the Short-Form 36 Quality of Life Questions to all participants and employed the Short-Form 6 Dimension index to create health utility scores which were created using a set of parametric preference weights, nonparametric preference weights and ordinal health state valuation techniques obtained from a sample of the general population.
Results
Utility values in the dialysis group were lower than in the non-dialysis group. There was a significant relationship between age and health utility scores: As age increases, health utility scores decrease. Diabetes was associated with lower health utility scores in dialysis patients, whereas other covariates did not reach levels of statistical significance in our stepwise regression models. The parametric Bayesian model and standard gamble approach yielded the same results, while the correlation between the nonparametric and parametric methods was above 0.9.
Conclusion
Health utility scores were low relative to the general population norm in our study cohort. Longitudinal assessment of CKD patients to capture possible fluctuations in health utility scores may add useful information.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The prevalence of chronic kidney disease (CKD) worldwide is about 8–10%, and the condition is considered as an independent risk factor for morbidity and mortality [1]. Furthermore, CKD has been related to high healthcare resource use and costs [2]. Optimal management requires slowing disease progression and treating comorbidities.
Many chronic diseases, including CKD, influence quality of life with more prominent effects with increased disease severity [3,4,5]. Regular assessment, encouragement of physical activity and management of modifiable factors are recommended to improve the physical and mental well-being of CKD patients [4, 6]. Specifically, measurement of physical functioning has been suggested, using the Short-Form 36 Quality of Life Health Survey Questions (SF-36) twice a year for dialysis patients [6].
Widespread use in chronic disease populations and availability of norm-based comparisons are main advantages of SF-36 over other types of measurement tools for quality of life [7]. A score higher than 50 is deemed above the general population norm, while a score of less than 50 is considered below the general population norm [8]. SF-36 scores can also be used to produce the Short-Form 6 Dimension (SF-6D) health utility scores using various algorithms.
The SF-6D is a preference-based measurement instrument that can be used to produce patient reported health utility scores for cost-utility analysis [9]. The SF-6D has six health attributes, including physical functioning, role limitations, social functioning, pain, mental health and vitality [9]. For each domain, there are five to six levels of response. Parametric (using Bayesian and non-Bayesian techniques), nonparametric and ordinal scoring algorithms can be used to produce health utility scores using the SF-6D instrument.
Since medical technologies are associated with considerable economic costs to patients and healthcare systems, a formal, systematic and transparent assessment process is required to weigh the pros and cons of any healthcare resource. Cost-utility analysis is a preferred choice for economic evaluations and requires health utility scores for each health state to produce quality-adjusted life years and subsequently incremental cost-utility ratios measuring one or more health outcomes [10, 11].
As it is the case for many chronic conditions, the burden of CKD is considerably large in terms of health-related effects and healthcare expenditures which necessitate economic evaluations. The purpose of this study is to provide health utility scores for health states related to various stages of CKD in adult patients that can be used to produce quality-adjusted life years. We also explored the associations between age, gender, body mass index (BMI), hemoglobin, estimated glomerular filtration rate (eGFR), calcium, phosphorus as well as albumin with health utility scores in our study cohort. We hypothesized that dialysis patients would exhibit lower health utility scores than non-dialysis CKD patients. We also hypothesized that parametric methods should yield the same health utility scores and parametric inferences should be higher than nonparametric inferences.
Methods
Baseline characteristics of patients, details about the study design and primary study results have been reported previously [12, 13]. This study included adult CKD patients, including dialysis, transplantation and non-dialysis CKD patients. All patients were recruited between September 2012 and December 2012 from the Health Sciences Centre, St. Clare’s Mercy, and Waterford Hospitals in St. John’s, Newfoundland, Canada.
This study was approved by the provincial Health Research Ethics Authority and Research Proposal Approval Committee of Eastern Health for the secondary use of data. We obtained the license agreement for the use of the SF-6D algorithm as wells as SF-36 questionnaire [9, 14, 15].
We included adult patients (18 years or older) with some degree of kidney dysfunction—eGFR less than 60 ml/min/1.73 m2. We excluded those with severe vision and/or hearing problems that interfered with the informed consent process and those who declined research participation.
Kidney dysfunction was defined by an eGFR calculated using the Modification of Diet in Renal Disease formula. We recorded patient’s characteristics including age, gender, BMI, smoking, diabetes, blood pressure parameters (systolic and diastolic blood pressure), hemoglobin, glucose, calcium, albumin, phosphate, parathyroid hormone level and eGFR on a case report form for each participant.
The SF-36 was administered by the principal investigator (NS), who read out the statements and asked the participants to choose the most appropriate response for his or her current condition. Consequently, the selected statement was circled. The questionnaires were self-administered by those who did not require any assistance.
The SF-36 form has 36 questions, eight scales and two summary measures. The eight scales are as follows: physical functioning (PF), role physical (RP), bodily pain (BP), general health (GH), vitality (VT), social functioning (SF), role emotional (RE) and mental health (MH). PF, RP and BP contribute to the PCS, whereas MH, RE and SF contribute to the MCS. VT, GH and SF contribute to both summary measures (Item S1) [8, 16]. The SF-6D has six domains, including physical functioning, role limitations, social functioning, pain, mental health and vitality [9].
We converted SF-36 data into the SF-6D health states and produced heath utility scores for each participant [15]. We used a set of preference weights created by parametric, nonparametric and ordinal health state valuation algorithms obtained from a sample of the general population [9]. Subsequently, we produced SF-6D health utility scores using standard gamble (parametric random effects model), parametric Bayesian, nonparametric Bayesian and ordinal scoring algorithms for each participant. We then calculated means and standard deviations for each patient group.
Parametric random effects model—either in the frequentist or Bayesian framework—and nonparametric Bayesian model are commonly used to create SF-6D health state utility scores [17]. The means of parametric inferences are expected to be higher than the means of nonparametric posterior inferences [17]. Parametric models make an assumption for the distribution of parameters, whereas nonparametric models provide more flexibility in terms of the shape of the distribution [17]. Furthermore, nonparametric models can incorporate skewness in valuation. Because of these advantages, it was shown that the predictive ability of nonparametric models was superior to the parametric models [17].
Health state valuation data can be also modeled by ordinal scoring algorithm (also called discrete choice experiment) [18]. The main difference between ordinal scoring algorithm and other methods is that the ordinal scoring algorithm allows utility values below zero [18].
We performed stepwise regression with a forward selection procedure. We tested predictor variables (i.e., age, gender, BMI, diabetes mellitus, smoking, hemoglobin, eGFR, systolic blood pressure, diastolic blood pressure, parathyroid hormone, phosphorus, calcium, albumin and glucose) in our stepwise regression and employed a significance level of 0.1 for retention in the multivariate models.
The scores of the SF-36 questionnaire, both standard and norm based, are calculated by the software (QualityMetric Health Outcomes ™ Scoring Software 4.5) after individual patient SF-36 questionnaire responses are inputted in the program [19]. We used an Excel program to convert SF-36 scores to SF-6D and produced health utility scores for each participant using the SF-6D algorithms as previously described. All other data analyses were performed using Stata (StataCorp. 2013. Stata Statistical Software: Release 13. College Station, TX: StataCorp LP). We employed two-sided tests with a significance level of 0.05.
Results
The details about the patient characteristics have been previously described and are indicated in Table 1 [12, 13]. The mean age was 62.7 (14.5) years, and 41% of the participants were female [12, 13]. There were no significant differences in age, gender, marital status, BMI, diabetes or smoking between the groups [12, 13]. Dialysis CKD patients had significantly lower serum albumin and hemoglobin as compared to non-dialysis CKD patients [12, 13].
Normalized scores from the eight scales and two summary measures of the SF-36 questionnaire are calculated. Only two participants did not complete the survey. PF, RP and VT normalized scores were lower than the general population mean of 50 in the study cohort [12, 13].
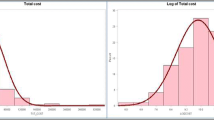
Table 2 depicts utility values of the study cohort, dialysis and non-dialysis CKD patients. Utility values in the dialysis group were lower when compared to the non-dialysis group. Means and medians of the utility values were equal, and the data were normally distributed (Figs. 1, 2).
We tested the associations between health utility scores and covariates. In the study cohort, there was a significant relationship between age and health utility scores: As age increases, health utility scores decrease (Fig. 3). In the dialysis group, diabetes mellitus was associated with lower health utility scores (β coefficient = −0.05, 95% CI −0.09 to −0.01) (Table 3). Other covariates did not reach levels of statistical significance in our stepwise regression models.
We included a comparison of health utility scores from different SF-6D algorithms. Our results showed the variability in health utility scores was similar between the groups when we used the standard gamble SF-6D algorithm (Table 2).
We produced the same results using non-Bayesian parametric and Bayesian parametric methods in all groups (Table 4). In our study, parametric inferences—either using Bayesian models or standard gamble method (non-Bayesian models)—were higher than nonparametric inferences (Table 4). For non-dialysis CKD patients, we created the same mean values using the ordinal scoring algorithm and parametric methods; however, the variability was lower in the parametric methods (SD = 0.10 in parametric models vs. SD = 0.13 in the ordinal scoring algorithm) (Table 4).
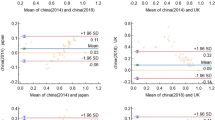
We compared parametric and nonparametric health utility scores in the study cohort, dialysis and non-dialysis CKD patients. The correlation coefficient was 0.92 for both the study cohort and non-dialysis CKD patients, while the coefficient was 0.91 for dialysis patients.
Discussion
The main objective of this study was to estimate SF-6D-based health utility scores for the Canadian CKD population. We also examined the correlations between health utility scores and patient demographics, clinical and laboratory variables. Our study found that (1) age was correlated with health utility scores in the study cohort; (2) diabetes mellitus was associated with health utility scores in dialysis patients; (3) we produced the same means and standard deviations of health utility scores using parametric methods in all groups; (4) the correlation between parametric and nonparametric methods was acceptable; and (5) we produced larger standard deviations in all groups when we used the ordinal scoring algorithm.
These findings are consistent with previous research relating age, disease severity and health utility scores. Evidence suggests health utility scores may be influenced by age [20]. We also showed that age was associated with health utility scores.
Depression has been linked to quality of life in several reports and has been associated with low health utility scores [21,22,23,24]. The findings reported in the literature suggest the possible correlation between disease severity and health utility scores [25,26,27]. Our findings showed that the mean of health utility scores was higher in non-dialysis CKD patients than in dialysis patients. This is an explicit link between disease severity and health utility scores as dialysis stage indicates severe loss of kidney function.
However, our study failed to prove a significant linear relationship between eGFR and health utility scores. Nevertheless, we cannot conclude the degree of kidney functions was not related to health utility score. This negative finding can be translated into two categories: (1) the effect is quite small or (2) the analysis had poor power to detect even a large effect.
Direct and indirect methods are used to measure health utilities which range from 0 to 1 (0 indicates death and 1 indicates perfect health) [11]. Direct methods include visual analog scale, the time trade-off and the standard gamble, collectively defined as category scaling [9]. The direct methods are more time-consuming and cumbersome [11]. Indirect methods require the transformation of SF-36 scores into SF-6D using different algorithms as previously described [28]. The Health Utilities Index and EuroQol-5D are other questionnaires that are used to produce health utility scores and considered indirect methods [29, 30].
Previous reports showed higher health utility scores with the direct techniques (i.e., standard gamble and time trade-off) [31]. Researchers also explored potential differences in health utility scores using various indirect methods. The standard gamble health utility scores were higher than utility values produced by ordinal scoring algorithm in hemodialysis patients [32]. This is congruent with our findings: Standard gamble method produced higher health utility scores as compared to the nonparametric techniques and the ordinal scoring algorithm. This emphasizes the importance of reporting the algorithm that was used (parametric vs. nonparametric vs. ordinal scoring algorithm) in an economic evaluation as various methods yield different health utility scores [18].
We used the SF-6D utility elucidation technique and a sample of the general population provided a set of nonparametric preference weights and parametric preference weights as previously described in “Methods” section. It is an indirect method for the estimation of preference-based health utility scores and likely underestimates utility values [31]. One possible limitation of our study is the lack of evaluation of the SF-36 scores over time. Furthermore, there may be differences between those who volunteered to participate in our study than those who did not.
Conclusion
This study provides health utility scores for CKD patients. We found that dialysis patients have lower health utility scores as compared to the non-dialysis CKD patients. This is the first study that created health utility scores for CKD patients in the Canadian population using various SF-6D algorithms. The parametric Bayesian method and standard gamble approach provided the same health utility scores as expected. The ordinal algorithm models produced larger standard deviations, while nonparametric models created lower health utility values. Longitudinal assessment of quality of life in CKD patients may add useful information.
References
Kidney Disease: Improving Global Outcomes (KDIGO) CKD–MBD Work Group (2009) KDIGO clinical practice guideline for the diagnosis, evaluation, prevention, and treatment of chronic kidney disease–mineral and bone disorder (CKD–MBD). Kidney Int 76(Suppl 113):S1–S130
Eriksson JK, Neovius M, Jacobson SH, Elinder CG, Hylander B (2016) Healthcare costs in chronic kidney disease and renal replacement therapy: a population-based cohort study in Sweden. BMJ Open 6(10):e012062
Osthus TB, Dammen T, Sandvik L, Bruun CM, Nordhus IH, Os I (2010) Health-related quality of life and depression in dialysis patients: associations with current smoking. Scand J Urol Nephrol 44(1):46–55
Smith DH, Gullion CM, Nichols G, Keith DS, Brown JB (2004) Cost of medical care for chronic kidney disease and comorbidity among enrollees in a large HMO population. J Am Soc Nephrol JASN 15(5):1300–1306
Covic A, Rastogi A (2013) Hyperphosphatemia in patients with ESRD: assessing the current evidence linking outcomes with treatment adherence. BMC Nephrol 14(1):153
Foundation NK (2005) KDOQI clinical practice guidelines for cardiovascular disease in dialysis patients. In: Guideline 14: smoking, physical activity, and psychological factors
Ware JE Jr, Sherbourne CD (1992) The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 30(6):473–483
Ware JE Jr, Kosinski M, Dewey JE (2000) How to score version 2 of the SF-36 health survey. QualityMetric Incorporated, Lincoln
McCabe C, Brazier J, Gilks P et al (2006) Using rank data to estimate health state utility models. J Health Econ 25(3):418–431
Laupacis A, Feeny D, Detsky AS, Tugwell PX (1992) How attractive does a new technology have to be to warrant adoption and utilization? Tentative guidelines for using clinical and economic evaluations. CMAJ Can Med Assoc J 146(4):473–481
Whitehead SJ, Ali S (2010) Health outcomes in economic evaluation: the QALY and utilities. Br Med Bull 96:5–21
Sekercioglu N, Curtis B, Murphy S, Barrett B (2015) Sleep quality and its correlates in patients with chronic kidney disease: a cross-sectional design. Ren Fail 37(5):757–762
Sekercioglu N, Curtis B, Murphy S, Barrett B (2015) Sleep apnea in patients with chronic kidney disease: a single center experience. Ren Fail 37(1):83–87
Brazier JE, Roberts J (2004) The estimation of a preference-based measure of health from the SF-12. Med Care 42(9):851–859
Kharroubi SA, Brazier JE, Roberts J, O’Hagan A (2007) Modelling SF-6D health state preference data using a nonparametric Bayesian method. J Econ 26(3):597–612
Ware JE Jr (2000) SF-36 health survey update. Spine 25(24):3130–3139
Kharroubi SA, Brazier JE, Roberts J, O’Hagan A (2007) Modelling SF-6D health state preference data using a nonparametric Bayesian method. J Health Econ 26(3):597–612
Norman R, Viney R, Brazier J, Burgess L, Cronin P, King M et al (2014) Valuing SF-6D Health States Using a Discrete Choice Experiment. Med Decis Mak Int J Soc Med Decis Mak 34(6):773–786
The QualityMetric Health Outcomes TM Scoring Software 4.5 [computer program]. Version 4.5.4330.22306
Fang M, Oremus M, Tarride JE, Raina P (2016) A comparison of health utility scores calculated using United Kingdom and Canadian preference weights in persons with Alzheimer’s disease and their caregivers. Health Qual Life Outcomes 14(1):105
Naglie G, Hogan DB, Krahn M et al (2011) Predictors of patient self-ratings of quality of life in Alzheimer disease: cross-sectional results from the Canadian Alzheimer’s Disease Quality of Life Study. Am J Geriatr Psychiatry 19(10):881–890
Gonzalez-Saenz de Tejada M, Bilbao A, Bare M et al (2016) Association between social support, functional status and change in health related quality of life and changes in anxiety and depression in colorectal cancer patients. Psycho-Oncology 25(8):891–897
Li C, Mao W, Liu X (2014) Depression, anxiety and reduced quality of life in predialysis: differences across the CKD stages? Int J Clin Pract 68(5):657–658
Zucchella C, Bartolo M, Bernini S, Picascia M, Sinforiani E (2015) Quality of life in Alzheimer disease: a comparison of patients’ and caregivers’ points of view. Alzheimer Dis Assoc Disord 29(1):50–54
Ahmad H, Taylor BV, van der Mei I et al (2016) The impact of multiple sclerosis severity on health state utility values: evidence from Australia. In: Multiple sclerosis. Houndmills, Basingstoke, England
Casellas F, Arenas JI, Baudet JS et al (2005) Impairment of health-related quality of life in patients with inflammatory bowel disease: a Spanish multicenter study. Inflamm Bowel Dis 11(5):488–496
Gregor JC, McDonald JW, Klar N et al (1997) An evaluation of utility measurement in Crohn’s disease. Inflamm Bowel Dis 3(4):265–276
Brazier J, Roberts J, Deverill M (2002) The estimation of a preference-based measure of health from the SF-36. J Health Econ 21(2):271–292
Kind P, Spilker B (1996) The EuroQol instrument: an index of health-related quality of life. Quality of Life and Pharmacoeconomics in Clinical Trials, Lippincott-Raven, Philadelphia
Horsman J, Furlong W, Feeny D, Torrance G (2003) The Health Utilities Index (HUI): concepts, measurement properties and applications. Health Qual Life Outcomes 1:54
Wyld M, Morton RL, Hayen A, Howard K, Webster AC (2012) A systematic review and meta-analysis of utility-based quality of life in chronic kidney disease treatments. PLoS Med 9(9):e1001307
Revicki DA (1992) Relationship between health utility and psychometric health status measures. Medical Care 30(5 Suppl):Ms274–Ms282
Authors’ contributions
NS, BB, BC and SM were involved in conception and design; NS analyzed the data; NS, BB, BC, SM and GB were involved in interpretation of results; NS, BB, BC and SM drafted the manuscript; NS, BB, BC and SM reviewed and approved the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethical approval
We conducted this study in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from the individual study participants for our original project. This project reports a post hoc analysis, and additional consent was not required.
Rights and permissions
About this article
Cite this article
Sekercioglu, N., Curtis, B., Murphy, S. et al. Estimates of health utility scores in chronic kidney disease. Int Urol Nephrol 49, 2043–2049 (2017). https://doi.org/10.1007/s11255-017-1664-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-017-1664-1