Abstract
Purpose
This study aimed to assess the relationships between abnormal lung function and indicators of chronic kidney disease in relation to metabolic syndrome (MetS) by using data from the 2011–2013 Korea National Health and Nutrition Examination Survey.
Methods
Using the data of 8551 Korean adults (3798 men, 4753 women, ≥40 years), lung function categories [obstructive lung disease (OLD), restrictive lung disease (RLD), and non-obstructive/non-restrictive lung disease (reference group)] were defined for each gender. Albuminuria and low estimated glomerular filtration rate (eGFR) were defined as urine albumin-to-creatinine ratio ≥30 mg/g and eGFR < 60 mL/min/1.73 m2. Gender-specific logistic regression analysis was performed after adjusting for age, educational level, smoking, alcohol use, physical activity, and medication use for chronic diseases.
Results
Compared to the reference group, low eGFR was associated with higher odds for RLD in men and RLD or OLD in women when they did not have MetS. In those with MetS, low eGFR was associated with higher odds for OLD in men and RLD or OLD in women. Albuminuria was associated with higher odds for RLD in men who did not have MetS, while it was associated with higher odds for RLD or OLD in men and women who had MetS.
Conclusions
Abnormal lung function was associated with increased odds for chronic kidney disease indicators, when combined with MetS in both gender. Even in those without MetS, RLD in men was associated with increased odds for low eGFR or albuminuria, while RLD or OLD in women was associated with increased odds for low eGFR.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic lower respiratory diseases and chronic kidney disease lead to major chronic morbidity and mortality worldwide and make the sustained public burden [1, 2]. A few studies have reported that the prevalence of chronic obstructive lung disease ranges from 20 to 30% among patients with chronic kidney disease [3, 4]. Other studies have suggested that obstructive/restrictive lung disease (OLD/RLD) is associated with some manifestations of chronic kidney disease, such as albuminuria or impaired kidney function [5–7]. Although pathophysiological mechanisms for those relationships remain to be defined, systemic and glomerular endothelial dysfunction and chronic inflammation could influence on both conditions [5, 8]. Endothelial dysfunction, characterized by the loss of the physiological balance between vasodilation and vasoconstriction [5], and chronic inflammation are also considered to play significant roles in the relationship between albuminuria and metabolic syndrome (MetS) [8]. Given these pathophysiological mechanisms, the associations of OLD and RLD with MetS may be plausible. Meanwhile, some studies have indicated that RLD is associated with the odds for metabolic syndrome (MetS), and the relationship between OLD and MetS has been shown to be inconsistent [9–12]. As there is evidence supporting MetS as a risk factor for the incidence of low estimated glomerular filtration rate (eGFR) and albuminuria [13] and differences in the relationships between OLD/RLD and MetS, the relationships between OLD/RLD and indicators of chronic kidney disease, such as albuminuria and low eGFR, could be affected by MetS. However, the combined effects of RLD/OLD and MetS on impaired kidney function have not been studied in depth. Thus, we aimed to evaluate the combined effects of RLD/OLD and MetS on low eGFR and albuminuria in a representative population-based study of South Koreans.
Methods
Participants
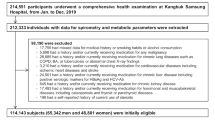
The participants were individuals from the non-institutionalized civilian population of South Korea who underwent assessment for health and nutritional status as part of the 2011–2013 Korea National Health and Nutrition Examination Survey (KNHANES), a cross-sectional, nationally representative survey [14, 15]. Among the 9564 adults who were aged ≥40 and had spirometry data available, we included 8551 adults (3798 men and 4753 women) who had complete data relating to spirometry, MetS, eGFR, urine albumin-to-creatinine ratio (UACR), health behaviors, educational attainment, and the use of medication for chronic diseases (hypertension, diabetes, dyslipidemia, cardiovascular disease, bronchial asthma, or osteoarthritis). We excluded those with a history of chronic kidney failure. Compared to 1014 individuals who were excluded, the included individuals were less likely to have albuminuria (UACR ≥ 30 mg/g; 8.5 vs. 11.7%, P = 0.021) and more likely to have MetS (32.9 vs. 28.4%, P = 0.021). However, there were no significant differences in the categories of lung function and low eGFR (eGFR < 60 mL/min/1.73 m2) between the individuals who were excluded and included. The KNHANES was conducted with ethical approval from the Institutional Review Board of the Korea Center for Disease Control and Prevention.
Measurements
Lung function was tested using a dry rolling-seal spirometer (Model 2130; SensoMedics, Yorba Linda, CA, USA) in the seated position, with nose clips, according to the manufacturer’s manual [16]. Each participant performed three–eight forced expiratory maneuvers. The forced expiratory volume for 1 s (FEV1) and the forced vital capacity (FVC) from three satisfactory maneuvers were used in the analyses. OLD was defined according to the Global Initiative for Chronic Obstructive Lung Disease criteria as an FEV1/FVC of <70% [17]. RLD was defined as an FEV1/FVC of ≥70% and an FVC < 80% of the predicted value [6]. The non-OLD and non-RLD groups were defined by an FEV1/FVC of ≥70% and an FVC of ≥80% of the predicted value.
Waist circumference (WC) was measured in the standing position at the narrowest region between the lower margin of the rib cage and the iliac crest. Blood pressure (BP) was assessed manually using a standard mercury sphygmomanometer. Venous blood samples were collected from each subject after a 12-h overnight fast. The levels of serum high-density lipoprotein cholesterol (HDL-C), fasting plasma glucose (FPG), triglycerides (TG), creatinine, urine creatinine, and albumin were measured using an automatic analyzer (Automatic Chemistry Analyzer 7600, Hitachi, Japan and Cobas 8000 C702, Roche, Germany).
The definition of MetS was adapted from the harmonized definition, in which three of five MetS components should be present [18]. The MetS criteria used in this study were as follows: WC > 90 cm in men or >85 cm in women [19]; BP ≥ 130/85 mmHg or a history of hypertension; an FPG level ≥5.6 mmol/L or a history of diabetes; a HDL-C level <1.03 mmol/L for men or <1.29 mmol/L for women; and a TG level ≥1.63 mmol/L.
UACR was calculated as the ratio of urine albumin to urine creatinine level (mg/g). eGFR was computed using the serum creatinine-based Chronic Kidney Disease Epidemiology Collaboration equation [20]. Albuminuria and low eGFR were, respectively, defined as a UACR ≥ 30 mg/g and an eGFR < 60 mL/min/1.73 m2 [21].
A standardized questionnaire was delivered using a self-administered method with the assistance of trained surveyors to assess demographic characteristics (age, gender, and educational attainment), the use of medications for chronic diseases, medical histories of hypertension, diabetes, and chronic kidney failure, and health behaviors. Health behaviors included history of smoking (non-smoker, current smoker, or ex-smoker), alcohol consumption (yes vs. no to drinking at least 1 unit of alcohol per month over the last year), and exercise (yes vs. no to engaging in regular, high-intensity exercise for >20 min/session at least 3 times/week; regular, moderate-intensity exercise for >30 min/session at least 5 times/week; and regular walking for >30 min/session at least 5 times/week).
Statistical analyses
All analyses were performed separately for men and women based on previous findings of gender-specific associations between RLD and albuminuria [22]. To compare the relationships of the three categories of lung function (non-OLD/non-RLD, RLD, and OLD) with the categories of kidney function, MetS, educational attainment, health behaviors, and medication use, we used the Chi-squared test. One-way analysis of variance with the post hoc Scheffe’s test was used to make comparison for age. Multiple logistic regression analyses were performed to determine the associations of the different categories of lung function with low eGFR and albuminuria, after adjusting for demographics, health behaviors, medication use, and other indicators of kidney function (i.e., eGFR in the analysis of albuminuria and UACR in the analysis of low eGFR). MetS was considered as a confounding factor in these models in order to identify any independent associations between the each lung function category and impaired kidney function. Finally, the same analyses were performed in the combined subgroups of the MetS (or its components) categories and lung function categories to detect the combined effects of MetS and impaired lung function on impaired kidney function. Data were analyzed using IBM Statistical Package for the Social Sciences (SPSS) software version 22.0.0.0 (IBM Corp., Armonk, NY, USA).
Results
In the total cohort, 10.1% of participants had RLD and 14.5% had OLD. Men and women with RLD or OLD were more likely to have low eGFR (odds ratio [95% confidence interval] 2.41 [1.51–3.84] for RLD, 3.31 [2.36–4.62] for OLD in men; 2.85 [1.83–4.44] for RLD, 3.69 [2.33–5.84] for OLD in women) and albuminuria (odds ratio [95% confidence interval] 2.29 [1.68–3.13] for RLD, 1.59 [1.22–2.06] for OLD in men; 1.85 [1.31–2.50] for RLD, 2.13 [1.53–2.97] for OLD in women) compared to those without RLD and OLD. MetS was more likely to occur in men with RLD (odds ratio [95% confidence interval] 2.01 [1.63–2.48]) and in women with RLD or OLD (odds ratio [95% confidence interval] 2.46 [2.02–2.99] for RLD, 1.44 [1.14-–1,82] for OLD) compared to those without RLD and OLD. The categories of lung function were associated with age, smoking status, alcohol use, educational attainment, and medication use for chronic diseases in both of men and women, and with exercising habits only in women (Table 1).
The gender-specific associations between combinations of lung function/MetS (or its components) and low eGFR and albuminuria are presented in Tables 2 and 3, respectively. When the results were adjusted for confounding factors and MetS, neither RLD nor OLD was associated with low eGFR in men, while RLD was associated with higher odds of low eGFR in women compared to those in the non-OLD and non-RLD groups. In terms of the relationships between the combination of MetS (or its components) and lung function categories, the odds for low eGFR increased in men with RLD when combined with high BP or low HDL-C; in men with OLD, when combined with MetS, high WC, high BP, or low HDL-C; in women with RLD, when combined with MetS or individual MetS components; and in women with OLD, when combined with MetS, high BP, high FPG, or low HDL-C. In contrast, the odds for low eGFR increased in men with RLD who did not have MetS or high BP; in women with RLD who did not have MetS, high BP, or high FPG; and in women with OLD who did not have MetS (Table 2).
As shown in Table 3, RLD in men and OLD in women were associated with increased odds for albuminuria after adjusting for confounding factors and MetS. In the combined models for MetS (or its components) and the categories of lung function, the odds for albuminuria increased in men and women with RLD and OLD combined with MetS or individual MetS components. In addition, the odds for albuminuria increased in men with RLD when they did not have MetS, high FPG, low HDL-C, or high TG; and in women with OLD who did not have high WC (Table 3).
Discussion
In this study of a representative sample of South Koreans aged ≥40 years old, RLD and OLD were associated with increased odds of low eGFR or albuminuria when combined with MetS or its components in both gender. To our knowledge, this is the first study to report the joint gender-specific effects of MetS and impaired lung function on indicators of chronic kidney disease. The associations observed suggest that there are some variations in the individual relationships. First, the additive effects of MetS and its components tended to be more consistent for the association with albuminuria than with low eGFR. In addition, some relationships indicated significant associations between impaired lung function and impaired kidney function, even though there was no concomitant MetS or its components, and those associations were modulated by gender. For example, the odds for low eGFR increased in men and women with RLD but no MetS, in men and women with RLD but without high BP, in women with RLD but without high FPG, and in women with OLD without MetS; the odds for albuminuria increased in men with RLD but without MetS, high FPG, low HDL-C, or high TG, and in women with OLD but without high WC.
The findings of the present study agree with and extend the previously published data. Our findings concerning the relationships between RLD/OLD and impaired kidney function after adjusting for MetS were partially consistent with previously reported data. In a US population-based study, albuminuria was found to be positively associated with RLD and OLD, while a decrease in eGFR was positively associated with OLD but not with RLD after adjusting for gender, body mass index, diabetes, and hypertension [6]. Another small study of chronic obstructive lung disease suggested that an increase in urinary albumin level exists in patients with severe forms of the condition [5]. Meanwhile, another cohort study supported the increased tendency of higher odds for microalbuminuria with lower FEV1 [7]. The gender-specific associations between RLD and albuminuria in a previous Korean study [22] were replicated in the present study. The present data add to these previous findings by demonstrating the combined effects of MetS or its individual components with impaired lung function on low eGFR and albuminuria according to gender.
The potential mechanisms for the associations between impaired lung function and impaired kidney function are multifactorial and not entirely understood: Impaired lung function induces hypoxic damage to the renal tubules and interstitium, systemic inflammation and oxidative stress, and glomerular injury caused by arterial stiffness [6, 9, 23–25]. The mechanistic link between MetS and impaired kidney function is also complex and multifactorial, involving insulin resistance, activation of the renin–angiotensin–aldosterone system, insulin/insulin-like growth factor-1 signaling pathways, reactive oxygen species formation [26], and other mechanisms in obesity [27]; nephrosclerosis and activation of the sympathetic system, interference with glomerular hemodynamics, and inflammatory mechanisms in high BP; and inflammatory and oxidative stress pathways in dyslipidemia [28]. In addition, some mechanisms, such as adiposity-induced effects on the lung airways, may involve both MetS and lung function impairment [29]. Therefore, the increased risk of impaired kidney function when combined with MetS may be explained by interactions between these complicated and common mechanisms.
So far, there are no plausible explanations for the gender-specific associations between impaired lung function and impaired kidney function. A previous Korean study and the current study both demonstrated gender-related difference in the relationship between RLD and albuminuria after adjusting for confounding factors including some components of MetS [22]. However, the current study adds new findings: There were gender-related differences in these relationships in participants without MetS or its components, but no gender-related differences in those with MetS or its components. Most probably gender-related differences in the underlying causes for RLD or the duration and severity of RLD, in addition to unmeasured environmental factors such as treatment of those conditions, cumulative exposure to smoking, and nutritional status, also contribute to the observed gender-related differences.
As the data used in this study were drawn from a representative population sample, the current observations can be generalized to South Korean adults aged ≥40 years old. However, the cross-sectional design of this study precludes us from making any causal inferences regarding the relationships among impaired lung function, MetS, and impaired kidney function. Making classifications based on a single measurement of UACR, creatinine and MetS components can lead to the misclassification of some individuals. Similarly, impaired lung function may also have been misclassified in some cases because post-bronchodilator spirometry measurements were not conducted for the classification of OLD, and RLD may not be capable of predicting true RLD [30]. Finally, although we attempted to adjust for all potential confounding factors, other may still have had an effect on the results.
In conclusion, this representative Korean study demonstrated that RLD or OLD was associated with increased odds for low eGFR or albuminuria, when combined with MetS in both gender. Even when MetS was not present, RLD in men was associated with increased odds for low eGFR or albuminuria, while RLD and OLD in women were associated with increased odds for low eGFR. Further studies will be necessary in order to elucidate whether these links represent the coexistence of the conditions or the causal relationships.
References
Lozano R, Naghavi M, Foreman K et al (2012) Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380(9859):2095–2128
Jha V, Garcia-Garcia G, Iseki K et al (2013) Chronic kidney disease: global dimension and perspectives. Lancet 382(9888):260–272
Incalzi RA, Corsonello A, Pedone C et al (2010) Chronic renal failure: a neglected comorbidity of COPD. Chest 137(4):831–837
van Gestel YR, Chonchol M, Hoeks SE et al (2009) Association between chronic obstructive pulmonary disease and chronic kidney disease in vascular surgery patients. Nephrol Dial Transplant 24(9):2763–2767
Bulcun E, Ekici M, Ekici A, Kisa U (2013) Microalbuminuria in chronic obstructive pulmonary disease. COPD 10(2):186–192
Navaneethan SD, Mandayam S, Arrigain S, Rahman M, Winkelmayer WC, Schold JD (2016) Obstructive and restrictive lung function measures and CKD: National Health and Nutrition Examination Survey (NHANES) 2007–2012. Am J Kidney Dis 68:414–421
Romundstad S, Naustdal T, Romundstad PR, Sorger H, Langhammer A (2014) COPD and microalbuminuria: a 12-year follow-up study. Eur Respir J 43(4):1042–1050
Rowley K, O’Dea K, Best JD (2003) Association of albuminuria and the metabolic syndrome. Curr Diab Rep 3(1):80–86
Cebron Lipovec N, Beijers RJ, van den Borst B, Doehner W, Lainscak M, Schols AM (2016) The prevalence of metabolic syndrome in chronic obstructive pulmonary disease: a systematic review. COPD 13(3):399–406
Ford ES, Cunningham TJ, Mercado CI (2014) Lung function and metabolic syndrome: findings of National Health and Nutrition Examination Survey 2007–2010. J Diabetes 6(6):603–613
Nakajima K, Kubouchi Y, Muneyuki T, Ebata M, Eguchi S, Munakata H (2008) A possible association between suspected restrictive pattern as assessed by ordinary pulmonary function test and the metabolic syndrome. Chest 134(4):712–718
Paek YJ, Jung KS, Hwang YI, Lee KS, Lee DR, Lee JU (2010) Association between low pulmonary function and metabolic risk factors in Korean adults: the Korean National Health and Nutrition Survey. Metabolism 59(9):1300–1306
Thomas G, Sehgal AR, Kashyap SR, Srinivas TR, Kirwan JP, Navaneethan SD (2011) Metabolic syndrome and kidney disease: a systematic review and meta-analysis. Clin J Am Soc Nephrol 6(10):2364–2373
Korea Centers for Disease Control and Prevention. (2010) Guidelines for using the third year, fourth National Healthy and Nutition Examination Survey (KNHANES IV), 2009. In, Osong, Chungcheong Buk-Do, Republic of Korea, Korea Centers for Disease Control and Prevention
Korea Centers for Disease Control and Prevention (2011) Guidelines for using the Fifth National Healthy and Nutition Examination Survey (KNHANES V-1), 2010
Yoo K (2012) Education and quality control of pulmonary function test and chest X-ray in the National Health and Nutrition Examination Survey 2012. Seoul: The Korean Academy of Tuberculosis and Respiratory Diseases 2012 Dec. 10th Contract No.: 2012E3501200
Vestbo J, Hurd SS, Agusti AG et al (2013) Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med 187(4):347–365
Alberti KG, Eckel RH, Grundy SM et al (2009) Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 120(16):1640–1645
Lee SY, Park HS, Kim DJ et al (2007) Appropriate waist circumference cutoff points for central obesity in Korean adults. Diabetes Res Clin Pract 75(1):72–80
Levey AS, Stevens LA, Schmid CH et al (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med 150(9):604–612
Stevens PE, Levin A, Kidney Disease: Improving Global Outcomes Chronic Kidney Disease Guideline Development Work Group Members (2013) Evaluation and management of chronic kidney disease: synopsis of the kidney disease: improving global outcomes 2012 clinical practice guideline. Ann Intern Med 158(11):825–830
Yoon JH, Won JU, Ahn YS, Roh J (2014) Poor lung function has inverse relationship with microalbuminuria, an early surrogate marker of kidney damage and atherosclerosis: the 5th Korea National Health and Nutrition Examination Survey. PLoS ONE 9(4):e94125
Casanova C, de Torres JP, Navarro J et al (2010) Microalbuminuria and hypoxemia in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 182(8):1004–1010
Mannino DM, Ford ES, Redd SC (2003) Obstructive and restrictive lung disease and markers of inflammation: data from the Third National Health and Nutrition Examination. Am J Med 114(9):758–762
Mapel D (2014) Renal and hepatobiliary dysfunction in chronic obstructive pulmonary disease. Curr Opin Pulm Med 20(2):186–193
Sarafidis PA, Ruilope LM (2006) Insulin resistance, hyperinsulinemia, and renal injury: mechanisms and implications. Am J Nephrol 26(3):232–244
Amann K, Benz K (2013) Structural renal changes in obesity and diabetes. Semin Nephrol 33(1):23–33
Tanner RM, Brown TM, Muntner P (2012) Epidemiology of obesity, the metabolic syndrome, and chronic kidney disease. Curr Hypertens Rep 14(2):152–159
Baffi CW, Wood L, Winnica D et al (2016) Metabolic syndrome and the lung. Chest 149(6):1525–1534
MacIntyre NR, Selecky PA (2010) Is there a role for screening spirometry? Respir Care 55(1):35–42
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author declares that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Lee, K. Lung function and impaired kidney function in relation to metabolic syndrome. Int Urol Nephrol 49, 1217–1223 (2017). https://doi.org/10.1007/s11255-017-1567-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-017-1567-1