Abstract
Purpose
The increased likelihood of poor outcomes in critically ill patients with hypoalbuminemia is well recognized. However, hypoalbuminemia remains poorly defined as an independent predictor of acute kidney injury (AKI) and stage 4 chronic kidney diseases (CKD4). The aim of this study was to assess the role of hypoalbuminemia as an independent risk factor for AKI and CKD4 in critically ill patients.
Design
A retrospective cohort study.
Setting
General intensive care unit (ICU) at Anhui Provincial Hospital, PR China.
Intervention
None.
Measurements and main results
We screened patients admitted to the ICU at Anhui Provincial Hospital between January 1, 2008, and October 31, 2011, and included those aged >18 years with available records of serum albumin (SA), baseline serum creatinine, and outcome data. The exclusion criteria were: (1) patients with known AKI and CKD stage 4, 5 before ICU admission; (2) patients lost to follow-up; and (3) patients without research authorization. A total of 588 patients with available data were enrolled in the study, and 62 patients with preexisting CKD stage 4 and CKD stage 5 and 115 with preexisting AKI were excluded. Thirty patients were lost to follow-up. Ultimately, 381 patients were analyzed, 233 (61.2%) of whom developed AKI. Patients with low SA were significantly more likely than those with normal SA (p = 0.0003) to develop AKI, and to progress from AKI to CKD4 (p = 0.0229). More patients in the AKI group than in the non-AKI group had risk factors such as hypotension, mechanical ventilation (MV), proteinuria, sepsis, nephrotoxin exposure, and high-risk surgery (p < 0.01). The difference in duration of MV, ICU days, ICU mortality, hospital days, and hospital mortality between the AKI and non-AKI groups was also significant (p < 0.01). Logistic regression showed that hypoalbuminemia was significantly associated with AKI and CKD4 [odds ratio (OR) 1.810, 95% confidence interval (CI) 1.102–2.992, and OR 2.494, 95% CI 1.231–5.295, respectively]. After 4 years of follow-up, Kaplan–Meier analysis showed that survival in hypoalbuminemia patients was significantly shorter than in patients with normal SA (p = 0.0393). In the Cox proportional hazard model, hypoalbuminemia was an independent predictor of long-term mortality (hazard ratio 1.5, 95% CI 1.042–2.183, p = 0.0291).
Conclusion
Hypoalbuminemia in critically ill patients is independently associated with an increased risk of development of AKI and AKI progressing to CKD4.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute kidney injury (AKI) is a well-recognized clinical disorder in intensive care units (ICU), occurring as a complication secondary to circulatory overload, metabolic acidosis, hyperkalemia, and neurological complications [1, 2]. Studies have shown its association with increased mortality, risk of chronic kidney disease (CKD), length of hospital stay, and healthcare costs [3]. It is reported that 2147 subjects per million population per year develop AKI in the USA [4]. Furthermore, the incidence of AKI is increasing and is expected to double over the next decade with the increase in population.
Critically ill patients develop AKI at a higher rate than the general population, as they are more likely to have high-risk factors. The incidence of ICU-acquired AKI is higher than that of community-acquired kidney injury and is increasing at an alarming rate [5, 6]. Thus, early identification of risk factors is vital in improving prognosis of critically ill patients. To date, some independent risk factors for AKI have been identified, such as age, body mass index, baseline renal function, acute circulatory or respiratory failure, liver disease, infection, peripheral vascular occlusive disease, chronic obstructive pulmonary disease, chronic heart failure, lymphoma or leukemia, prior invasive procedures, and higher-risk surgery [6, 7].
Hypoalbuminemia, despite being a common laboratory finding in critically ill patients, remains a poorly defined predictor of AKI. Albumin functions as a plasma protein, binding to and transporting a wide range of endogenous and exogenous substances. It therefore plays a key role in the metabolism and also in clearance of many drugs [8]. Hypoalbuminemia is defined as a serum albumin concentration of less than 35 g/L. The reported frequency of hypoalbuminemia was 21% at the time of admission in adult hospitalized patients [9]. After admission, worsening of existing hypoalbuminemia and development of de novo hypoalbuminemia are both frequently encountered [10]. The increased likelihood of poor outcomes such as mortality, morbidity, and prolonged ICU and hospital stay in acutely ill patients with hypoalbuminemia is well recognized [11]. However, the relation between serum albumin (SA) concentration and AKI in the ICU requires further study.
Patients who survive an episode of AKI are still at high risk of progressing to advanced stages of CKD [12, 13]. About 20% of patients with an in-patient diagnosis of acute tubular necrosis progress to CKD stage 4 or greater within 18–24 months [12]. The continuity of disease from AKI to CKD to end-stage renal disease (ESRD) has been recognized by most clinicians. Nevertheless, few studies explore whether patients with hypoalbuminemia are at greater risk of CKD. The aim of this study was therefore to assess whether hypoalbuminemia is an independent factor of AKI and CKD4 in critically ill patients and to compare survival time between patients with hypoalbuminemia and those with normal SA.
Materials and methods
Study population
This was a retrospective study. We screened patients admitted to the ICU at Anhui Provincial Hospital between January 1, 2008, and October 31, 2011. The inclusion criteria were: (1) adult patients older than 18 years and (2) all enrolled patients with available records of serum albumin, baseline serum creatinine, and outcome data. The exclusion criteria were: (1) patients with known AKI and CKD stage 4 or CKD stage 5 before ICU admission; (2) patients lost to follow-up; and (3) patients without research authorization. A total of 588 patients with available data were enrolled. Sixty-two patients with preexisting CKD stage 4 and CKD stage 5, 115 with AKI before admission, and 30 patients lost to follow-up were excluded. Ultimately, 381 patients were analyzed (Fig. 1). This study was approved by the Ethics Committee of Anhui Provincial Hospital.
Data collection
SA was measured using the photometric method within the first 72 h of admission to the ICU. The severity of illness was estimated according to the sequential organ failure assessment (SOFA) score. Baseline demographic parameters, creatinine level during ICU, and other clinic data including comorbidities, laboratory data, length of mechanical ventilation, length of stay in ICU, and mortality were obtained from Anhui Provincial Hospital Patient Database.
Outcomes
The primary outcome was incidence of AKI and CKD4. AKI was defined by the Acute Kidney Injury Network criteria [14], and CKD by the Kidney Disease: Improving Global Outcomes CKD Work Group [15]. CKD4 was defined as the first date on which estimated glomerular filtration rate decreased below 30 mL/min per 1.73 m2 without increasing above 30 mL/min per 1.73 m2 again [15]. The secondary outcome was survival duration of patients with low versus normal SA.
Long-term follow-up
The long-term follow-up (4 years) data for these patients were obtained from Anhui Provincial Hospital Patient Database.
Statistical analysis
The data were analyzed using JMP™ version 10 (SAS Inc., Cary, NC, USA). Chi-square test was used for the analysis of categorical variables. Student’s t test or Mann–Whitney test was utilized to compare measurement variables. Logistic regression was used to identify variables that predict AKI and CKD4. Kaplan–Meier method was used to compare survival time of patients with low and normal SA. Cox proportional hazard regression model was utilized to identify the independent predictors for AKI mortality. A two-sided p value <0.05 was considered to indicate statistical significance.
Results
Baseline demographic, clinical characteristics, and clinical outcomes between the two groups (SA ≥ 3.5 g/dL and SA < 3.5 g/dL) are summarized in Table 1. Of the 381 patients included, 233 (61.2%) developed AKI, 76 (32.6%) of whom required hemodialysis or renal replacement therapy. Of patients with normal SA, 51.9% (97/187) developed AKI, compared with 70.1% (136/194) of patients with SA. The difference was found to be statistically significant (p = 0.0003). The differences between groups in age, gender, BMI, serum creatinine, and comorbidities were not significant. Patients with low SA were found to have increased incidences of chronic liver disease, MV, and sepsis, and significantly higher SOFA scores (p < 0.001) compared to those with normal SA. Furthermore, duration of MV in patients with low SA was longer than in those with normal SA (p = 0.0011), as was the duration of ICU and hospital stay (p < 0.0001). Hospital mortality in patients with low SA was significantly higher compared with normal SA (p = 0.033), while no difference was found in ICU mortality (p = 0.065). After 4 years of follow-up, 56/233 (24.0%) AKI patients progressed to CKD4, including 16 in the normal-SA group and 40 in the low-SA group (p = 0.0229).
Table 2 shows baseline demographics, clinical characteristics, and outcomes in the AKI and non-AKI groups. Compared with patients without AKI, those with AKI were older; had more comorbidities including diabetes, hypertension, chronic liver disease, chronic lung disease, CKD (p < 0.05); and more high-risk factors such as hypotension, MV, proteinuria, sepsis, nephrotoxin exposure, and high-risk surgery (p < 0.01). The AKI patients had higher SOFA scores and serum creatinine levels than non-AKI patients. In addition, the difference in length of MV, ICU days, ICU mortality, hospital days, and hospital mortality between the two groups was significant (p < 0.01).
Logistic regression was used to analyze independent risk factors for AKI (Table 3). Hypoalbuminemia [odds ratio (OR) 1.810, 95% confidence interval (CI) 1.102–2.992], male sex (OR 0.409, 95% CI 0.241–0.686), nephrotoxin exposure (OR 7.642, 95% CI 2.091–38.210), mechanical ventilation (OR 1.919, 95% CI 1.148–3.234), high-risk surgery (OR 2.177, 95% CI 1.184–4.105), hypotension (OR 12.455, 95% CI 3.453–80.145), and serum creatinine (>1.3 mg/dL) on admission (OR 5.964, 95% CI 3.491–10.513) were significantly associated with AKI. However, chronic liver disease was not significant (OR 1.133, 95% CI 0.419–3.059). Table 4 shows risk factors for CKD4. Hypoalbuminemia (OR 2.494, 95% CI 1.231–5.295), nephrotoxin exposure (OR 4.974, 95% CI 1.816–14.064), and serum creatinine (OR 5.608, 95% CI 2.637–12.955) were significantly associated with CKD4, while age and gender were not.
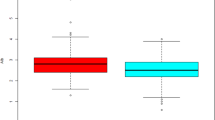
After 4 years of follow-up, Kaplan–Meier survival analysis showed that patients with hypoalbuminemia died earlier than those with normal SA (Fig. 2) (p = 0.0393). In the Cox proportional hazard model, chronic lung disease [hazard ratio (HR) 1.509, 95% CI 1.056–2.152)], hypoalbuminemia (HR 1.5, 95% CI 1.402–2.183), and serum creatinine (HR 1.944, 95% CI 1.3–2.929) were strong independent predictors of long-term mortality (Table 5).
Discussion
AKI is a major health hazard affecting 10–20% of hospitalized patients. Certain patient groups are at particular risk, especially patients in the ICU, those with preexisting CKD, and patients receiving nephrotoxic agents. Any novel factor for accurately predicting AKI would be highly advantageous. This study demonstrated that patients with hypoalbuminemia in the ICU have increased risk not only of developing AKI, but also of further progression to CKD4. Duration of MV, length of ICU, and hospital stay, and hospital mortality are all higher in patients with low SA than in normal SA. After 4 years of follow-up, patients with hypoalbuminemia have higher mortality than those with normal SA. A Cox regression model showed that hypoalbuminemia has a significant association with AKI. Our results therefore suggest hypoalbuminemia is an independent prognostic factor for AKI and CKD4 in the ICU.
It is well known that normal serum albumin in healthy adults is approximately 35–50 g/L. Hypoalbuminemia (SA < 3.5 g/dL) is a common phenomenon in critically ill patients as they often have comorbidities that reduce serum albumin levels. Factors that contribute to reduced serum albumin include systemic inflammation, peritoneal and urinary losses of protein, and liver synthesis dysfunction. A meta-analysis showed that hypoalbuminemia was an independent risk factor both for developing AKI and for AKI-related mortality [16]. These results are consistent with our findings. However, few studies have shown the relation between hypoalbuminemia and CKD4 and long-term follow-up of patients with AKI.
Our study found that nearly two-thirds of patients in the ICU are at high risk of developing AKI, proving that AKI is an important health hazard in the ICU and that emphasis should be placed on identifying risk factors for its occurrence. Over the past decade, many studies have focused on the independent risk factors for AKI in specific clinical settings, such as in critically ill children, and after cardiac surgery, contrast exposure, and high-risk surgery [17–20]. Few studies have focused on occurrence of AKI in the general ICU. In addition to the high incidence of AKI, we found that patients with hypoalbuminemia had longer duration of MV, and of ICU and hospital stays. Albumin is critical for physiological function of macromolecules and carriers in vivo, and decrease of albumin in blood may cause multiple organ dysfunctions. Therefore, patients with hypoalbuminemia have more comorbidities and complications.
There are several possible mechanisms by which serum albumin protects kidney function: (a) Specific ligand-binding properties of albumin may mediate renoprotection [21]. (b) Albumin mitigates the nephrotoxicity of interleukin-2 (IL-2). Serum albumin concentration increased by approximately 1% could benefit survival of cultured renal tubular cells independently of either bound lipid or colloid osmotic pressure [22]. (c) The renoprotective action of albumin is mediated by its capabilities of scavenging reactive oxygen species, preventing oxidative damage, and binding and delivering lysophosphatidic protective acid [23]. (d) Albumin can prolong potent renal vasodilatation by reacting with oxides of nitrogen or by binding of platelet-activating factor, which resulted in improved renal perfusion [24]. (e) Albumin can also stimulate renal tubular cell DNA synthesis via signaling pathways involving Ca2+, protein kinase C, epidermal growth factor receptor, mitogen-activated protein kinases, and nuclear factor-KB [25, 26].
There is strong evidence that hypoalbuminemia is associated with poor outcomes in a variety of diseases including ESRD, surgical illness, and acute stroke [27]. Therefore, serum albumin level has been included as one of the component parameters in the Acute Physiology and Chronic Health Evaluation III score because of its importance as an outcome predictor [28].
Although our study identified hypoalbuminemia is an independent prognostic factor for AKI and AKI progressing to CKD4 in the ICU, a study about albumin replacement showed that correction of hypoalbuminemia did not improve patient outcomes [29]. At the heart of the controversy is causality—whether hypoalbuminemia directly contributes to poor outcomes, in which case albumin replacement therapy might be beneficial, or merely serves as a marker for other “upstream” pathologic processes such as malnutrition or inflammation, in which case exogenous albumin might be ineffective in altering the clinical course.
Conclusion
Hypoalbuminemia in the general ICU is independently associated with an increased risk of development of AKI and of AKI progressing to CKD4.
References
Uchino S, Kellum JA, Bellomo R et al (2005) Acute renal failure in critically ill patients: a multinational, multicenter study. JAMA 294(7):813–818
Waikar SS, Liu KD, Chertow GM (2008) Diagnosis, epidemiology and outcomes of acute kidney injury. Clin J Am Soc Nephrol 3(3):844–861
Bellomo R, Kellum JA, Ronco C (2012) Acute kidney injury. Lancet 380(9843):756–766
Ali T, Khan I, Simpson W et al (2007) Incidence and outcomes in acute kidney injury: a comprehensive population-based study. J Am Soc Nephrol 18(4):1292–1298
Joannidis M, Metnitz B, Bauer P et al (2009) Acute kidney injury in critically ill patients classified by AKIN versus RIFLE using the SAPS 3 database. Intensive Care Med 35(10):1692–1702
Metnitz PG, Krenn CG, Steltzer H et al (2002) Effect of acute renal failure requiring renal replacement therapy on outcome in critically ill patients. Crit Care Med 30(9):2051–2058
Joannidis M, Metnitz PG (2005) Epidemiology and natural history of acute renal failure in the ICU. Crit Care Clin 21(2):239–249
Rothschild MA, Oratz M, Schreiber SS (1988) Serum albumin. Hepatology 8(2):385–401
Herrmann FR, Safran C, Levkoff SE et al (1992) Serum albumin level on admission as a predictor of death, length of stay, and readmission. Arch Intern Med 152(1):125–130
McCluskey A, Thomas AN, Bowles BJ et al (1996) The prognostic value of serial measurements of serum albumin concentration in patients admitted to an intensive care unit. Anaesthesia 51(8):724–727
Margarson MP, Soni N (1998) Serum albumin: touchstone or totem? Anaesthesia 53(8):789–803
Amdur RL, Chawla LS, Amodeo S et al (2009) Outcomes following diagnosis of acute renal failure in U.S. veterans: focus on acute tubular necrosis. Kidney Int 76(10):1089–1097
Wald R, Quinn RR, Luo J et al (2009) Chronic dialysis and death among survivors of acute kidney injury requiring dialysis. JAMA 302(11):1179–1185
Mehta RL, Kellum JA, Shah SV et al (2007) Acute Kidney Injury Network: report of an initiative to improve outcomes in acute kidney injury. Crit Care 11(2):R31
Kasiske BL, Wheeler DC (2014) Kidney disease: improving global outcomes—an update. Nephrol Dial Transpl 29(4):763–769
Wiedermann CJ, Wiedermann W, Joannidis M (2010) Hypoalbuminemia and acute kidney injury: a meta-analysis of observational clinical studies. Intensive Care Med 36(10):1657–1665
Kheterpal S, Tremper KK, Heung M et al (2009) Development and validation of an acute kidney injury risk index for patients undergoing general surgery: results from a national data set. Anesthesiology 110(3):505–515
Matheny ME, Miller RA, Ikizler TA et al (2010) Development of inpatient risk stratification models of acute kidney injury for use in electronic health records. Med Decis Making 30(6):639–650
Basu RK, Zappitelli M, Brunner L et al (2014) Derivation and validation of the renal angina index to improve the prediction of acute kidney injury in critically ill children. Kidney Int 85(3):659–667
Cruz DN, Ferrer-Nadal A, Piccinni P et al (2014) Utilization of small changes in serum creatinine with clinical risk factors to assess the risk of AKI in critically lll adults. Clin J Am Soc Nephrol 9(4):663–672
Contreras AM, Ramirez M, Cueva L et al (1994) Low serum albumin and the increased risk of amikacin nephrotoxicity. Rev Invest Clin 46(1):37–43
Levine JS, Koh JS, Triaca V et al (1997) Lysophosphatidic acid: a novel growth and survival factor for renal proximal tubular cells. Am J Physiol 273(4 Pt 2):F575–F585
Iglesias J, Abernethy VE, Wang Z et al (1999) Albumin is a major serum survival factor for renal tubular cells and macrophages through scavenging of ROS. Am J Physiol 277(5 Pt 2):F711–F722
Kaufmann MA, Castelli I, Pargger H et al (1995) Nitric oxide dose-response study in the isolated perfused rat kidney after inhibition of endothelium-derived relaxing factor synthesis: the role of serum albumin. J Pharmacol Exp Ther 273(2):855–862
Lee YJ, Han HJ (2008) Albumin-stimulated DNA synthesis is mediated by Ca2+/PKC as well as EGF receptor-dependent p44/42 MAPK and NF-kappaB signal pathways in renal proximal tubule cells. Am J Physiol Renal Physiol 294(3):F534–F541
Dixon R, Brunskill NJ (1999) Activation of mitogenic pathways by albumin in kidney proximal tubule epithelial cells: implications for the pathophysiology of proteinuric states. J Am Soc Nephrol 10(7):1487–1497
Gariballa SE, Parker SG, Taub N et al (1998) Influence of nutritional status on clinical outcome after acute stroke. Am J Clin Nutr 68(2):275–281
Knaus WA, Wagner DP, Draper EA et al (1991) The APACHE III prognostic system. Risk prediction of hospital mortality for critically ill hospitalized adults. Chest 100(6):1619–1636
Caironi P, Tognoni G, Masson S et al (2014) Albumin replacement in patients with severe sepsis or septic shock. N Engl J Med 370(15):1412–1421
Authors’ contributions
MS participated in the design and drafted the paper. SYW contributed equally with MS to the paper. PKP participated in critical review of the manuscript. MS played a principal role in the design, analysis, and preparation of the manuscript.
Acknowledgements
The present study was supported by the Natural Science Foundation of Anhui Province (grant no.1408085MH170) and the medical research projects of Anhui provincial health department (grant no.13zc024).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There are no conflicts in our manuscript file.
Additional information
Min Shao and Shengyu Wang have contributed equally to this work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Shao, M., Wang, S. & Parameswaran, P.K. Hypoalbuminemia: a risk factor for acute kidney injury development and progression to chronic kidney disease in critically ill patients. Int Urol Nephrol 49, 295–302 (2017). https://doi.org/10.1007/s11255-016-1453-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-016-1453-2