Abstract
Purpose
The optimal vitamin D3 therapy for the treatment of secondary hyperparathyroidism (SHPT) in chronic hemodialysis patients is still controversial. Recent studies suggest that uremia in end-stage renal disease is associated with enzymatic hepatic dysfunction altering 25-hydroxylation of vitamin D3. The goal of our study was to compare the efficacy of calcitriol, the fully hydroxylated active form of vitamin D3, to alfacalcidol which needs 25-hydroxylation to be effective, for the treatment of SHPT in chronic hemodialysis patients.
Methods
We retrospectively reviewed 45 chronic hemodialysis patients who were switched from oral alfacalcidol to oral calcitriol for the treatment of SHPT. Parathyroid hormone (PTH), serum calcium and serum phosphorus levels were compared pre- and post-conversion using paired Student’s t tests.
Results
The mean dose of active vitamin D3 decreased from 3.50 mcg/week at baseline to 2.86 mcg (P < 0001) after the switch from alfacalcidol to calcitriol. PTH significantly decreased from 94.4 to 82.6 pmol/L (−11.8 pmol/L, P = 0.02). The mean corrected calcium increased from 2.17 to 2.25 mmol/L (+0.08 mmol/L, P < 0.001) without any clinically significant hypercalcemia, and phosphorus levels were stable. Results were similar in a subgroup of patients (n = 17) for whom the medication was administrated during the hemodialysis session, ensuring a complete compliance.
Conclusions
According to our study, calcitriol in equal dosage is more effective than alfacalcidol in lowering serum PTH level in chronic hemodialysis patients. This suggests that calcitriol may be the optimal active vitamin D3 for the treatment of SHPT in chronic hemodialysis patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Secondary hyperparathyroidism (SHPT) is a common complication in chronic hemodialysis patients, occurring in almost all hemodialysis patients [1]. If not adequately controlled, SHPT can lead to significant consequences such as bone structure and mineralization anomalies, hypercalcemia, accelerated vascular calcification and is associated with higher morbidity and mortality [2, 3].
Hyperphosphatemia, hypocalcemia and diminished production of 1,25-dihydroxyvitamin D3 by the kidney all contribute to the augmentation of parathyroid hormone (PTH) and therefore SHPT. In many cases, despite nutritional counseling and the use of phosphate binders, it is difficult to attain PTH targets recommended by the KDIGO guidelines [4]. The addition of an active vitamin D3 is thus necessary to achieve an optimal control of the SHPT in the context of insufficient production. Alfacalcidol and calcitriol are currently the only available active vitamin D3 in Canada. Alfacalcidol, 1-alpha-hydroxyvitamin D3, is hydroxylated in position 1 but not in position 25. Therefore, it requires hydroxylation by the liver in position 25 to become the fully active 1,25-dihydroxyvitamin D3. On the other hand, calcitriol is already hydroxylated in positions 1 and 25, thus is already fully active.
There is currently limited data in the literature regarding the most efficient vitamin D3 for the treatment of SHPT in chronic hemodialysis patients. A recent study by Michaud et al. suggests that uremia is associated with hepatic enzymatic dysfunction altering calcidiol 25-hydroxylation in rats [5]. Their results show that the production of calcitriol after the administration of 1-alpha-hydroxyvitamin D3 was significantly reduced by 48% (p < 0.05) in rats with chronic renal failure compared with controls. Therefore, in uremia, calcitriol, the fully hydroxylated active form of vitamin D3, could be more effective than alfacalcidol for PTH suppression.
The goal of this study was to compare the efficacy of calcitriol and alfacalcidol, for the treatment of SHPT in chronic hemodialysis patients and to verify the dose equivalence of these two active vitamins D3.
Subjects and methods
To compare the efficacy of calcitriol and alfacalcidol, we conducted a retrospective study of 45 chronic hemodialysis patients for whom alfacalcidol administration was switched to calcitriol for the treatment of SHPT between March 2011 and January 2013.
Inclusion criteria were patients over 18 years old, receiving 4-hour hemodialysis treatments three times weekly and treated for SHPT who were switched from oral alfacalcidol to oral calcitriol.
Exclusion criteria were parathyroidectomy, hepatic insufficiency and any modification of the medication used in their treatment of hyperparathyroidism (phosphate binder, cinacalcet) during the study period or incomplete data.
Primary endpoint was to compare the efficacy of calcitriol and alfacalcidol in lowering PTH levels in the treatment of SHPT in chronic hemodialysis patients. Intact PTH assays were performed on a i2000 immunoassay analyzer from Abbott Diagnostics.
Secondary endpoints were to examine changes in phosphorus and calcium after the switch. Calcium was corrected for the albumin level according to this formula; Corrected calcium (mmol/L) = Calcium measured (mmol/L) + 0.02 × (40-albumin (g/L).
We compared different components of mineral metabolism (PTH, calcium, phosphorus, alkaline phosphatase) with paired Student’s t tests at baseline and approximately 50 days post-conversion, to ensure metabolic stabilization. We also analyzed a subgroup of patients receiving their vitamin D3 during their hemodialysis sessions, thus ensuring 100% compliance.
Results
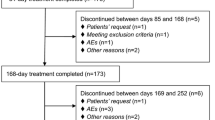
Fifty patients were initially selected for analysis, but five were excluded (Fig. 1). Baseline characteristics of patients are outlined in Table 1. All patients had hemodialysis sessions three times per week for an average of 12.6 h/week and mean single-pool Kt/V was 1.66. The mean dialysis vintage was 4.8 years.
The mean dose of alfacalcidol before the conversion was 3.50 ± 1.52 mcg/week, and the mean dose of calcitriol was 2.86 ± 1.40 mcg/week after the conversion, which represents a 20% reduction in the active vitamin D3 (P < 0.001). We observed a significant decrease in PTH with a mean of 94.4 ± 42.6 and 82.6 ± 53.0 pmol/L, pre- and post-conversion, respectively (−11.8 ± 33.5 pmol/L; P = 0.02). Mean corrected calcium for albumin increased from 2.17 to 2.25 mmol/L (+ 0.08 mmol/L; P < 0.0001). No clinically significant hypercalcemia was observed during this study (maximum value of 2.78 mmol/L). There was no significant change in the phosphorus serum levels (Table 2).
In a subgroup of 17 patients for whom their vitamin D3 was administrated during the hemodialysis sessions, thus ensuring 100% compliance, we observed a mean reduction in PTH of 9.4 ± 19.9 pmol/L (P = 0.07) as well as an increase in the mean calcium of 0.05 mmol/L (P = 0.051; Table 3).
Discussion
Chronic kidney disease mineral and bone disorders regroup anomalies in bones, in calcium, phosphorus, PTH or vitamin D metabolism and vascular or other soft-tissue calcifications [4]. Following the KDIGO guidelines, treatment of dialysis patients in this study aimed to normalize calcium and phosphorus levels and to maintain PTH within two to nine times the upper normal limit of 7.2 pmol/L of our laboratory, thus targeting 14.4–64.8 pmol/L [4]. In this study, 45 patients were switched from alfacalcidol to calcitriol because of the theoretical deficit in 25-hydroxylation in those patient.
According to our study, calcitriol is more effective than alfacalcidol in lowering serum PTH in chronic hemodialysis patients, despite a 20% reduction in the vitamin D3 dose. There were no significant adverse effects observed after the conversion. This PTH reduction toward the recommended target may have been achieved with an increased in the alfacalcidol dose, but demonstrates nevertheless the advantage of calcitriol over alfacalcidol in this population. This increase efficacy of calcitriol compared to alfacalcidol could be attributable to hepatic enzymatic dysfunction altering the 25-hydroxylation in uremic patients. As demonstrated on murine models, chronic kidney disease is associated with a down-regulation of the cytochrome P450 isoform in the liver, which is involved in the conversion of 25-hydroxyvitamin D3 to 1,25-dihydroxyvitamin D3. This reduction in enzyme activity could be secondary to the PTH increase in end-stage renal disease (ESRD). This was shown by the correction of de 1,25-dihydroxyvitamin vitamin D3 deficiency after a parathyroidectomy in rats with ESRD and by an increase in 25-hydroxyvitamin vitamin D3 levels following parathyroidectomy in patients with primary hyperparathyroidism [5–7].
There are few studies comparing alfacalcidol and calcitriol for the treatment of SHPT. Arenas et al. conducted a retrospective study on 21 hemodialysis patients with SHPT after the hospital pharmacy substituted calcitriol with alfacalcidol. After the switch, they observe an increase of 38% of the mean PTH level (P < 0.001) [8]. A small randomized, crossover trial study of five patients by Moe et al. [9] showed a better suppression of the PTH with calcitriol compared to alfacalcidol. More recently, Kiattisunthorn et al. conducted a randomized trial comparing calcitriol and alfacalcidol for the treatment of SHPT in 32 hemodialysis patients. After 24 weeks of follow-up, the number of patients who achieved target PTH was similar in the two groups despite a significantly higher dose of alfacalcidol (6.9 mcg/week) compared to calcitriol (4.1 mcg/week; P < 0.001). They concluded that alfacalcidol could be used at doses 1.5–2 times higher than the calcitriol dose to treat SHPT [10]. Bezzaoucha et al. also conducted a small retrospective study in ten alfacalcidol-resistant peritoneal dialysis patients with SHPT whom were switch from alfacalcidol to calcitriol [11]. With a similar dose of calcitriol, they observed a significant decrease in PTH level from 101 ± 75 to 43 ± 24 pmol/L (P < 0.05) and a significant increase in serum 1,25-dihydroxyvitamin vitamin D3 levels from 23 ± 9 to 50 ± 21 pmol/L (P < 0.05), which suggest that calcitriol is more effective in increasing 1,25-dihydroxyvitamin vitamin D3 level than alfacalcidol because of an hepatic enzymatic dysfunction altering the 25-hydroxylation of alfacalcidol in uremic patients.
Despite these studies, uncertainty remains on how the superiority of calcitriol over alfacalcidol influences the treatment of SHPT in hemodialysis patients. All studies were small with few patients, and the largest including 32 patients was conducted in an Asian population. We conducted the present study, in a Canadian chronic hemodialysis population, to validate the previously observed results.
One limitation of our study is that it is a single-center, retrospective study. However, our study is the largest on the subject. We also analyzed a subgroup of patients whose compliance was assured, since their active vitamin D3 was administered during hemodialysis sessions under nursing supervision and we observed the same result.
In conclusion, bypassing hepatic 25-hydroxylation appears to be associated with greater efficacy of calcitriol at increasing serum calcium and inhibiting PTH secretion. These observations must be taken into consideration before choosing a vitamin D3 or switching from one to another. In light of these results, calcitriol may be the treatment of choice for SHPT in chronic hemodialysis patients, especially for those with resistant hyperparathyroidism, which does not respond adequately to alfacalcidol. Alfacalcidol remains a valid option in some predialysis patients with mild secondary hyperparathyroidism easily controlled with alfacalcidol.
References
Levin A, Bakris GL, Molitch M, Smulders M, Tian J, Williams LA, Andress DL (2006) Prevalence of abnormal serum vitamin D, PTH, calcium, and phosphorus in patients with chronic kidney disease: results of the study to evaluate early kidney disease. Kidney Int 71(1):31–38
Block GA, Kilpatrick RD, Lowe KA, Wang W, Danese MD (2013) CKD-mineral and bone disorder and risk of death and cardiovascular hospitalization in patients on hemodialysis. Clin J Am Soc Nephrol 8(12):2132–2140. doi:10.2215/cjn.04260413
Ketteler M, Gross M-L, Ritz E (2005) Calcification and cardiovascular problems in renal failure. Kidney Int 67(S94):S120–S127
Kidney Disease: Improving Global Outcomes CKD-MBD Working Group (2009) KDIGO clinical practice guideline for the diagnosis, evaluation, prevention, and treatment of Chronic Kidney Disease-Mineral and Bone Disorder (CKD-MBD). Kidney Int Suppl 113:S1–130. doi:10.1038/ki.2009.188
Michaud J, Naud J, Ouimet D, Demers C, Petit JL, Leblond FA, Bonnardeaux A, Gascon-Barre M, Pichette V (2010) Reduced hepatic synthesis of calcidiol in uremia. J Am Soc Nephrol 21(9):1488–1497. doi:10.1681/ASN.2009080815
Michaud J, Naud J, Chouinard J, Desy F, Leblond FA, Desbiens K, Bonnardeaux A, Pichette V (2006) Role of parathyroid hormone in the downregulation of liver cytochrome P450 in chronic renal failure. J Am Soc Nephrol 17(11):3041–3048. doi:10.1681/ASN.2006010035
Lamarche C, Leblond F, Ouimet D, Pichette V (2015) Effect of parathyroidectomy on vitamin D levels. World J Surg 39(5):1333–1334. doi:10.1007/s00268-014-2836-0
Arenas MD, Muray S, Amoedo ML, Egea JJ, Millan I, Gil MT (2006) A long-term comparative study of calcitriol versus alphacalcidol in patients with secondary hyperparathyroidism on hemodialysis. Nefrologia: Publicacion Oficial de la Sociedad Espanola Nefrologia 26(2):226–233
Moe S, Wazny LD, Martin JE (2008) Oral calcitriol versus oral alfacalcidol for the treatment of secondary hyperparathyroidism in patients receiving hemodialysis: a randomized, crossover trial. Can J Clin Pharm 15(1):e36–e43
Kiattisunthorn K, Wutyam K, Indranoi A, Vasuvattakul S (2011) Randomized trial comparing pulse calcitriol and alfacalcidol for the treatment of secondary hyperparathyroidism in haemodialysis patients. Nephrology 16(3):277–284. doi:10.1111/j.1440-1797.2010.01398.x
Funding
This study was funded by La Fondation de l’Hôpital Maisonneuve-Rosemont: la néphrologie et son impact.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All Authors declare that we have no conflict of interest.
Ethical approval
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standard. The study protocol was approved by our institution’s research ethics committee.
Rights and permissions
About this article
Cite this article
Rauscher, S., Lafrance, JP., Pichette, V. et al. Conversion of oral alfacalcidol to oral calcitriol in the treatment of secondary hyperparathyroidism in chronic hemodialysis patients. Int Urol Nephrol 49, 325–328 (2017). https://doi.org/10.1007/s11255-016-1446-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-016-1446-1