Abstract
Purpose
We analyzed trends related to surgical approach for renal cell carcinoma (RCC), including partial nephrectomy (PN) or radical nephrectomy (RN), in patients with stage 4 chronic kidney disease (CKD), and identified predictors for postoperative progression to end-stage renal disease (ESRD) requiring permanent dialysis.
Methods
We enrolled patients with stage 4 CKD who underwent surgery for non-metastatic RCC. We compared their characteristics according to surgical approach (PN vs. RN). Moreover, predictors for postoperative progression to requiring permanent dialysis were determined using multivariable analyses. The Charlson comorbidity index (CCI) was adjusted for age.
Results
Fifty-one patients (PN 23, RN 28) were evaluated in the present study. Their mean preoperative estimated glomerular filtration rate (eGFR) was 24 ml/min/1.73 m2, and four patients had a solitary kidney. Three of 23 patients (13 %) who underwent PN progressed to requiring dialysis after surgery after a median 16 months. In contrast, 13 of 28 patients (46 %) who underwent RN developed dialysis immediately after surgery (median 2 days). Patients who underwent PN had lower T stages (T1, PN 100 % vs. RN 50 %, p = 0.004) and smaller tumors (31 mm vs. 65 mm, p < 0.0001) than did those who underwent RN. RN and lower preoperative eGFR significantly predicted progression to requiring dialysis, while tumor size and CCI did not.
Conclusions
PN tended to be selected for patients with lower T stage and smaller tumors in the limited cohort of stage 4 CKD patients. PN had a significant benefit of preventing dialysis in the multivariable analysis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The purpose of partial nephrectomy (PN) is to preserve kidney function to the extent possible in order to prevent cardiovascular events and to prolong life expectancy. This purpose is based on results of a previous report showing a close relationship between chronic kidney disease (CKD) and cardiovascular events [1], as well as on those of retrospective studies analyzing the rates of cardiovascular events after kidney surgery for renal tumors [2–5]. However, according to a previous randomized study, whether PN has a superior survival rate to that of radical nephrectomy (RN) in all patients with renal cell carcinoma (RCC) is unclear [6]. Long-term outcomes, like survival rate, are not only indicators to evaluate surgical outcomes after surgery for patients with RCC.
Renal replacement therapy, such as dialysis, can damage quality of life for patients; therefore, avoiding end-stage renal disease (ESRD) and the requirement for dialysis are very meaningful if oncological and survival outcomes are not damaged. Compared to RN, PN can prevent the deterioration of kidney function by preserving normal kidney parenchyma, indicating the potential for avoiding dialysis after surgery for RCC in patients with severe CKD. In addition, it is sometimes challenging to select the appropriate surgical method for RCC in patients with severe CKD because there are no standard guidelines for determining the optimal strategy for such cases. In fact, it is unclear whether the normal renal parenchyma is sufficiently preserved in PN to avoid ESRD requiring dialysis in patients with severe kidney dysfunction due to ischemic insult or perioperative complications. In this study, we analyzed trends with respect to surgical approach for RCC, including PN and RN, in patients with stage 4 CKD and identified the predictors for postoperative progression to ESRD requiring dialysis using our institute’s database.
Methods
An institutional review board-approved retrospective review was conducted on consecutive patients who underwent PN or RN at our hospital. The cohort consisted of 51 patients with stage 4 CKD [estimated glomerular filtration rate (eGFR) between 15 and 30 ml/min/1.73 m2] and localized RCC who were treated with RN or PN between 1979 and 2015. All measurements for determining preoperative eGFR were performed less than 2 months before surgery. Renal function was assessed using eGFR calculated with an adjustment for diet according to the renal disease equation recently modified for Japanese patients, as regulated by The Japanese Society of Nephrology [eGFR = 1.94 × serum creatinine (in mg/dl)1.094 × age0.287 × 0.739 (if female)] [7]. Clinicopathological factors were determined from the patients’ medical records. Tumor stage was determined according to the 2009 TNM classification [8]. The pathological diagnosis was made according to the 2004 World Health Organization classification [9]. The following variables were evaluated for each patient: age, sex, body mass index (BMI), preoperative eGFR, clinical T stage, tumor size, Charlson comorbidity index (CCI) adjusted for age, perioperative complications, postoperative length of hospital stay (PLOS), and remaining dialysis-free. Finally, predictors for the development of ESRD requiring dialysis based on surgical approach were assessed with multivariable analysis. Kidney cancerous factors were not incorporated into the CCI.
Statistical analysis
All statistical analysis was performed with JMP 11.2.0 (SAS Institute, Cary NC, USA). Univariate comparisons were made using the Chi-square or Mann–Whitney U tests, as appropriate. The rate of remaining dialysis-free was calculated using the Kaplan–Meier method, and statistical significance was determined by the log-rank test. The predictors for the development of dialysis were determined with a multivariable Cox proportional hazards model. Statistical significance was set at p < 0.05.
Results
Twenty-three and 28 patients underwent PN and RN, respectively. Table 1 shows a comparison of patient characteristics. The mean age of all patients at surgery was 67 years, and 84 % were men. The mean BMI was 24 kg/m2, the mean CCI score was 4.9, and the mean preoperative eGFR was 24 ml/min/1.73 m2. Fourteen percent of patients had multifocal tumors. Four patients with solitary kidney were included. These variables were not significantly different between the PN and RN groups. However, differences were significant for the following variables: The mean tumor size was smaller in the PN than in the RN group (31 vs. 65 mm; p < 0.001). Patients in the PN group had higher rates of diabetes mellitus (39 vs. 14 %, p = 0.043) and hypertension (91 vs. 50 %, p = 0.002) before surgery than did those in the RN groups. Patients in the PN group had a less advanced tumor stage (T1: 100 %) than did those in the RN group (T1: 50 %; T3: 46 %; T4: 4 %; p = 0.004). Thirteen of 28 patients (46 %) in the RN group progressed to ESRD requiring permanent dialysis after surgery, whereas 3 of 23 patients (13 %) in the PN group did (p = 0.0106). PLOS was shorter in the PN than in the RN group (PN 9.8 days; RN 14 days; p = 0.0021).
Figure 1 shows the trends for surgical approach according to eGFR distribution. Thirteen of 25 patients (52 %) with an eGFR of 25–30 ml/min/1.73 m2 underwent PN, whereas 7 of 16 (44 %) with an eGFR of 20–25 ml/min/1.73 m2 and 3 of 10 (30 %) with an eGFR of 15–20 ml/min/1.73 m2 underwent PN. Patients with less kidney function tended to undergo RN more frequently in this cohort.
Trends for surgical approaches according to eGFR distribution. Thirteen of 25 patients (52 %) with eGFR 25–30 ml/min/1.73 m2 underwent PN, whereas 7 of 16 (44 %) patients with eGFR 20–25 ml/min/1.73 m2 and 3 of 10 (30 %) patients with eGFR 15–20 ml/min/1.73 m2 underwent PN. eGFR estimated glomerular filtration rate, PN partial nephrectomy
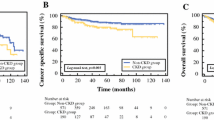
The dialysis-free rate is shown in Fig. 2. The two-year dialysis-free rate was 88 % in the PN group and 63 % in the RN group (p = 0.016). Table 2 provides the details of patients who progressed to requiring permanent dialysis. As noted above, 3 of 23 (13 %) patients who underwent PN ultimately required dialysis. One patient with a preoperative eGFR of 16 ml/min/1.73 m2 began dialysis 1 month after surgery, and the other two patients with preoperative eGFRs of 16–20 ml/min/1.73 m2 progressed to requiring dialysis 16 and 48 months after surgery, respectively. On the other hand, 13 of 28 (46 %) patients who underwent RN progressed to requiring dialysis. Most patients with an eGFR of 15–25 ml/min/1.73 m2 began undergoing hemodialysis immediately following surgery. Three patients with an eGFR of 25–30 ml/min/1.73 m2 progressed to requiring dialysis 23–52 months after surgery.
Table 3 shows the results of the multivariable analysis of the predictors for developing ESRD requiring dialysis after surgery. RN (vs. PN, odds ratio 5.38, p = 0.030) and lower preoperative eGFR were significant risk factors. However, significant differences were not observed for tumor size and CCI.
Discussion
PN can preserve more renal parenchyma than can RN, which may help to avoid worsening kidney function. Although a randomized study from the EORTC study group could not show better survival following PN than following RN or differences with respect to the development of advanced CKD (eGFR < 30 ml/min/1.73 m2 or <15 ml/min/1.73 m2), the population of this study was comprised of patients with comparatively good kidney function [6, 10]. Dharam and colleagues evaluated the comparative overall survival and renal function in patients following PN and RN for benign renal tumors [11]. Their study included patients with comparatively poor kidney function, such as those with stage 3a CKD (30 %) and stage 3b CKD (4 %). A multivariate analysis showed that patients treated with RN were significantly more likely to die from any cause [hazard ratio (HR) 1.73, p < 0.001] or to develop stage 4 CKD (HR 4.23, p < 0.001) compared with patients who underwent PN, suggesting that even patients with comparatively poor kidney function can receive more kidney functional benefits from PN than from RN.
CKD progression is thought to increase the prevalence of cardiovascular events and mortality rates in the general population [1]. Based on this theory, PN is recommended for patients with small RCCs to preserve renal function, which means that the ultimate target for preserving kidney function is to prolong survival. However, preventing the progression to ESRD requiring renal replacement therapy, such as dialysis, is also an important function for PN in patients with severe CKD. Under the conditions of a kidney donor shortage, dialysis is inevitable for patients with ESRD, which damages their quality of life and increases medical expenditures. Some population-based cohort studies assessed the correlation of progression to ESRD after surgery between PN and RN [12, 13]. Yap and colleagues demonstrated that PN was associated with less ESRD requiring renal replacement therapy than was RN in a modern cohort (2003–2010) of patients with RCC [12]. On the other hand, Lin and colleagues reported that patients with RCC undergoing RN do not have a significantly higher risk of developing ESRD compared to those undergoing PN [13]. Needless to say, patient backgrounds between these two studies were different, suggesting that this controversial result was dependent on various limitations such as patient background or era. These large cohort studies did not incorporate preoperative kidney function into the multivariate analysis, possibly due to study limitations.
In patients with severe kidney dysfunction, such as stage 4 CKD (eGFR 15–30 ml/min/1.73 m2), it is unclear whether PN can preserve sufficient kidney function to avoid renal replacement therapy even if normal renal parenchyma is preserved, possibly influenced by ischemic insult or perioperative complications. Although surgical approaches, including PN or RN, are determined according to tumor size, patient age, or comorbidities, there is currently no evidence, such as a guideline, for managing these patients. In addition, there are no reports on treatment strategies for RCC in patients with severe CKD. As shown in Fig. 1, patients with less kidney function tended to undergo RN in this cohort. Although other important factors for determining surgical approach, such as tumor size, tumor stage, or patient comorbidities, were not incorporated into this analysis, we might choose RN for patients with extensive severe CKD because such patients could not avoid ESRD requiring dialysis using PN due to ischemic insults or other factors.
In our cohort, 3 of 23 patients (13 %) who underwent PN progressed to ESRD requiring dialysis. This included one patient with a preoperative eGFR 15–20 ml/min/1.73 m2 and a 23-mm tumor who underwent PN and who began hemodialysis 1 month after surgery. However, this patient had been affected by nephrosis syndrome and had a solitary kidney. The other two patients have remained hemodialysis-free for over 12 and 60 months. Two of 7 (29 %) patients with a preoperative eGFR of 20–25 ml/min/1.73 m2 who underwent PN commenced hemodialysis 16 and 48 months after surgery, with a tumor size of 47 mm and 30 mm, respectively. The other 5 patients have remained hemodialysis-free over a follow-up period between 1 and 48 months (mean 21 months, median 12 months). All 13 patients with preoperative eGFRs of 25–30 ml/min/1.73 m2 have remained hemodialysis-free over a follow-up period between 3 and 72 months (mean 17 months, median 24 months). In summary, most patients with severe CKD who underwent PN avoided ESRD requiring dialysis for a comparatively long period, except for a patient who had nephrosis syndrome.
All patients who underwent PN in our cohort underwent open surgery with no ischemia (2 cases) or cold ischemia (21 cases). In addition, mean and median cold ischemia time were 37 and 40 min (range 7–82 min), respectively, suggesting that kidney function may be preserved even with relatively long ischemia times, even in patients with severe CKD. We have sometimes noted that ischemic damage in the kidney seemed to be influenced to a greater degree by poorer kidney function than by stronger kidney function, which may lead to avoiding PN in patients with severe kidney dysfunction. Mir and colleagues addressed the ability of different functional strata of kidneys to recover from ischemic insults during PN [14]. They measured preservation rates of split renal function and renal parenchymal mass in the operated kidney in patients who underwent PN and compared recovery from ischemia, defined as percent GFR saved/percent volume saved, according to ischemia type or ischemia time. Median recovery from ischemia for poorly functioning kidneys (GFR < 30 ml/min/1.73 m2) was 99 %. Corresponding values in kidneys with GFRs of 31–45, 46–60, and >60 m/min/1.73 m2 were 93, 95, and 97 %, respectively (p = 0.24). Their study suggested that even poorly functioning kidneys recover well from the ischemic insult proportionate to the amount of parenchyma preserved, as long as hypothermia or limited-warm ischemia were used.
The present study had some limitations including its retrospective, single-center design and the tertiary care patient population that was evaluated. In addition, the small sample size might have limited our statistical power in the multivariate analysis for determining the predictors of progression to ESRD requiring dialysis. Moreover, we could not incorporate risk factors for CKD, such as family history of CKD, presence of hyperlipidemia, hypertension, or BMI, into the multivariate analysis to maintain statistical power with the small sample size. There was a strong selection bias for the surgical method, as patients in the PN group had a less advanced tumor stage (T1: 100 %) than did those in the RN group (T1: 50 %; T3: 46 %; T4: 4 %; p = 0.004). The strength of this study is that it is possibly the first to focus on patients with severe kidney dysfunction when comparing kidney functional outcomes between PN and RN. In addition, we showed that PN can avoid permanent dialysis, even in patients with severe kidney dysfunction. Although the surgical approach is usually decided based on tumor size, stage, or patient background, PN may be recommended for patients with severe CKD in order to avoid renal replacement therapy as long as possible.
Conclusions
We showed that PN was better at preventing the progression to ESRD requiring dialysis than was RN in patients with stage 4 CKD. Although surgeons debate whether to select PN or RN for patients with severe kidney dysfunction based on the consideration of damage to the preserved renal parenchyma due to ischemic insult or other factors in PN, PN for RCC in such patients should be considered to prolong duration to the requirement for renal replacement therapy.
Abbreviations
- BMI:
-
Body mass index
- CCI:
-
Charlson comorbidity index
- CKD:
-
Chronic kidney disease
- eGFR:
-
Estimated glomerular filtration rate
- ESRD:
-
End-stage renal disease
- HR:
-
Hazard ratio
- PLOS:
-
Postoperative length of stay
- PN:
-
Partial nephrectomy
- RCC:
-
Renal cell carcinoma
- RN:
-
Radical nephrectomy
References
Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY (2004) Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med 351:1296–1305
Tan HJ, Norton EC, Ye Z, Hafez KS, Gore JL, Miller DC (2012) Long-term survival following partial vs radical nephrectomy among older patients with early-stage kidney cancer. JAMA 307:1629–1635
Weight CJ, Lieser G, Larson BT et al (2010) Partial nephrectomy is associated with improved overall survival compared to radical nephrectomy in patients with unanticipated benign renal tumours. Eur Urol 58:293–298
Weight CJ, Miller DC, Campbell SC, Derweesh IH, Lane BR, Messing EM (2013) The management of a clinical t1b renal tumor in the presence of a normal contralateral kidney. J Urol 189:1198–1202
Huang WC, Elkin EB, Levey AS, Jang TL, Russo P (2009) Partial nephrectomy versus radical nephrectomy in patients with small renal tumors–is there a difference in mortality and cardiovascular outcomes? J Urol 181:55–61 (discussion 61–52)
Van Poppel H, Da Pozzo L, Albrecht W et al (2011) A prospective, randomised EORTC intergroup phase 3 study comparing the oncologic outcome of elective nephron-sparing surgery and radical nephrectomy for low-stage renal cell carcinoma. Eur Urol 59:543–552
Matsuo S, Imai E, Horio M et al (2009) Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis 53:982–992
Sobin LH, Compton CC (2010) TNM seventh edition: what’s new, what’s changed: communication from the International Union Against Cancer and the American Joint Committee on Cancer. Cancer 116:5336–5339
Lopez-Beltran A, Scarpelli M, Montironi R, Kirkali Z (2006) 2004 WHO classification of the renal tumors of the adults. Eur Urol 49:798–805
Scosyrev E, Messing EM, Sylvester R, Campbell S, Van Poppel H (2014) Renal function after nephron-sparing surgery versus radical nephrectomy: results from EORTC randomized trial 30904. Eur Urol 65:372–377
Kaushik D, Kim SP, Childs MA et al (2013) Overall survival and development of stage IV chronic kidney disease in patients undergoing partial and radical nephrectomy for benign renal tumors. Eur Urol 64:600–606
Yap SA, Finelli A, Urbach DR, Tomlinson GA, Alibhai SMH (2015) Partial nephrectomy for the treatment of renal cell carcinoma (RCC) and the risk of end-stage renal disease (ESRD). BJU Int 115:897–906
Lin W-Y, Liang F-W, Lu T-H (2015) Risk of end-stage renal disease after cancer nephrectomy in Taiwan: a nationwide population-based study. PLoS One 10:e0126965
Mir MC, Takagi T, Campbell RA et al (2014) Poorly functioning kidneys recover from ischemia after partial nephrectomy as well as strongly functioning kidneys. J Urol 192:665–670
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
IRB approval number
3748.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Takagi, T., Kondo, T., Omae, K. et al. Comparison of progression to end-stage renal disease requiring dialysis after partial or radical nephrectomy for renal cell carcinoma in patients with severe chronic kidney disease. Int Urol Nephrol 48, 1421–1427 (2016). https://doi.org/10.1007/s11255-016-1317-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-016-1317-9