Abstract
Background
Ischemia–reperfusion (I/R) injury to the kidney occurs commonly in organ transplantation from donation after cardiac death, involving many pathologic processes. In this study, we used rat model to assess whether tripterysium glycosides (TG) preconditioning could exert protective effects in renal I/R injury.
Materials and methods
All male SD rats were randomly divided into four groups (6 each): sham group, TG group, I/R group and TG + I/R group. Groups TG and TG + I/R were pretreated with TG at 0.1 mg/kg for 14 days; groups sham and I/R were administered with the same dosage of normal saline. Groups TG + I/R and I/R underwent 45 min of renal ischemia of left kidney after right nephrectomy, and then, they were subjected to 72-h reperfusion. Groups sham and TG were only received right nephrectomy. The indicators of apoptosis, fibrosis and inflammation were analyzed to evaluate the effect of tripterysium glycosides preconditioning on renal I/R injury.
Results
Pretreatment with TG significantly inhibited the levels of serum creatine and blood urea nitrogen and improved histologic lesions induced by I/R injury. Moreover, for the apoptosis signal pathway, pretreatment with TG markedly decreased the expression of caspase-3 and Bax and increased the level of Bcl-2. HMGB1, which was regarded as one of inflammation marker molecule, it was inhibited in the TG + I/R group. For the fibrosis signal pathway, the pretreatment with TG before I/R could down-regulate the expression level of typical molecules of fibrosis (TGF-β1, Smad3, p-Smad3).
Conclusions
Pretreatment with tripterysium glycosides exhibited protective effect on kidney ischemia/reperfusion injury, which might be related to the alleviation of inflammation, fibrosis and the reduction in apoptosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Renal ischemia–reperfusion injury (IRI) was one of the major impact factors for the quality of the kidney graft, which was directly related to the receiver’s survival. Some researchers identified that activation of polymorphonuclear leukocytes, eicosanoids, cytokines, reactive oxygen species and complement products were involved in the initial phase of I/R. The intracellular and extracellular accumulation of these products triggers homeostatic pathways involved with necrosis, apoptosis and possibly autophagy [1]. Furthermore, some other reports showed that renal I/R injury represented an additional risk factor for late renal allograft failure [2]. Therefore, it was important to find effective agents or intervening measures to attenuate the kidney I/R injury.
Tripterysium glycosides were the main effective ingredient of traditional Chinese Medicine, the shrub-like vine Tripterygium wilfondii Hook F. It had been widely used to treat many diseases, such as rheumatoid arthritis, lupus erythematosus, dermatomyositis, white plug syndrome and glomerulonephritis. It had multiple biological activities, such as anti-inflammation [3], immunosuppressive [4], anticancer activities [5]. Here, we supposed that tripterysium glycosides preconditioning had the ability to attenuate the I/R injury of rat kidney for its wide range of pharmacological effects.
Materials and methods
Animal preparation and experimental design
Male, adult SD rats (body weight 250–300 g) were acquired from the Experimental Animal Center of Medical College of Wuhan University (Wuhan, China). Animals were housed at the Central Animal Facility of Affiliated Renmin Hospital of Wuhan University based on standard guidelines. All experiments were performed in accordance with the guidelines of the Chinese Council for Animal Care. Rats were maintained in a homoiothermal (20–22 °C), light-controlled (light for 7 a.m.–7 p.m.) and air-filtered room, allowed voluntary feeding behaviors with standard diets.
Drugs
Tripterysium glycosides was purchased from Aladdin reagent (Aladdin, Shanghai, China).
Experimental protocol
All male SD rats were anesthetized with pentobarbital (50 mg/kg) via intraperitoneally. After 500 U heparin intraperitoneal injected, rats were placed on an electric heating pad to maintain constant body temperature at 37 °C and performed right nephrectomy. The artery and vein of left kidney were clipped by a vascular clamp for 45 min to make model of ischemia, and then, the left kidney got reperfusion for 72 h. Finally, all rats were killed.
Rats were randomized into four groups: group sham (n = 6)—rats were underwent right nephrectomy but without modeling of the left renal ischemia; group TG (n = 6)—rats were administered with TG 0.1 mg/(kg day) intraperitoneally for 2 weeks in advance, and then, all the rats were performed with right nephrectomy; group ischemia/reperfusion (I/R) (n = 6)—rats were performed with right nephrectomy and made model of left renal ischemia for 45 min and then got reperfusion of 72 h; group TG + I/R (n = 6)—before I/R operation, TG were given intraperitoneally at 0.1 mg/(kg day) for 2 weeks in advance and then followed the same operation as group I/R.
Serum assays
Seventy-two hours after reperfusion, all the rats were killed to acquire blood samples from the inferior vena cava for testing the concentration of blood urea nitrogen (BUN) and creatinine (Cr). Blood samples were taken, and assays were performed according to the instructions of commercially available creatinine and urea assay kits (Nanjing Jiancheng Bioengineering Research Institute, Nanjing, China). The absorbance was measured by spectrophotometry using a Shimadzu UV-1700 spectrophotometer (Kyoto, Japan; absorbance measured at 510 and 640 nm for the creatinine and urea assay kits, respectively).
Histology
Rats were performed with left nephrectomy 72 h after reperfusion. The tissue specimens were sectioned at 4 mm thickness, fixed with 10 % phosphate-buffered formalin and embedded in paraffin according to standard procedure. Slides were gradually deparaffinized, rehydrated and subsequently observed by Periodic Acid-Schiff (PAS) staining. Morphological assessment was performed using standard method by an experienced renal pathologist without informing the grouping of the experiment.
Immunohistochemistry
Slides were manipulated based on the reagents of immunohistochemical assay (Gene Tech, Wuhan, China). The differences in protein expression of Bax, Bcl-2, caspase-3, HMGB1, TGF-β1 and Smad3 in groups were analyzed and evaluated by comparing the staining intensity (strong, mild, or negative) on microscopic examination.
Western blot analysis
Proteins were extracted and purificated from renal tissue as previously described. In brief, protein samples were prepared for gel electrophoresis to be separated on 12.5 % sodium dodecyl sulfate–polyacrylamide gels (40 μg/lane) and then transferred to a nitrocellulose membrane (Bio-Rad). The membrane was blocked with 5 % nonfat dry milk in TBST buffer and then incubated with primary antibodies overnight at homoiothermy of 4 °C. After rinsing with TBST buffer extensively, the blots were incubated with secondary antibodies and developed with the use of an enhanced chemiluminescence system (ECL kit; Pierce Biotechnology Inc., Rockford, IL) and captured on light-sensitive imaging film (Kodak) to analyze. The following kits were used as primary antibodies: the rabbit polyclonal anti-Bax (1:1000; CST, CA), caspase-3 (1:1000; CST, CA), Bcl-2 (1:1000; CST, CA), TGF-β1 (1:1000; CST, CA), HMGB1 (1:800; CST, CA), Smad3 (1:2000; abcam, CA), p-Smad3 (1:1000; abcam, CA) antibody or mouse monoclonal anti-GAPDH antibody (1:1000; Santa Cruz, CA, USA). HRP-conjugated anti-rabbit or anti-mouse secondary antibodies (Santa Cruz, CA, USA) were used as secondary antibody.
TUNEL staining
To observe cell apoptosis induced by ischemia, an in situ apoptosis detection kit (Promega, USA) was used. The TUNEL assay was performed based on the manufacturer’s instructions. Briefly, fixed in 4 % paraformaldehyde/PBS (pH 7.4) solution at 4 °C overnight, the whole specimens were extensively washed with 1*PBS solution three times, subsequently immersed into 70 % ethanol for at least 24 h at 20 °C. After washing three times adequately with PBS, the samples were immersed into a permeabilization buffer for 15 min on ice and then washed by PBS. Subsequently, they were incubated with 50 ml reaction buffer (TdT Enzyme 5 ml + Labeling Safe Buffer 45 ml) for 90 min at 37 °C. The labeling procedure was stopped by washing with a PBS solution. The image was analyzed by a Zeiss LSM 510 Confocal laser scanning microscope with a 488-nm excitation line and a 530-nm emission filter.
Statistical analysis
All data were underwent statistical analysis in SPSS version 18.0 (SPSS Inc, Chicago, IL, USA). In this study, t test was used to analyze the differences. A value of p < 0.05 was considered statistically significant.
Results
Tripterysium glycosides preconditioning improved renal function after renal IRI in a short term
Compared to the I/R group, the levels of BUN and Cr in TG + I/R group were significantly decreased. Levels of BUN and Cr had no significant difference between groups sham and TG. Generally, the tripterysium glycosides preconditioning could improve renal function after renal IRI (Fig. 1).
Tripterysium glycosides preconditioning significantly improved the renal function in I/R injury. a Tripterysium glycosides preconditioning significantly improved the renal dysfunction induced by I/R injury by decreasing the level of serum Cr. b Compared with I/R group, TG + I/R group significantly reduced the level of BUN in the model of renal ischemia–reperfusion. Meanwhile, there were no significant differences in the levels of serum Cr and BUN between groups sham and TG. (*p < 0.05 vs. sham group, # p < 0.05 vs. I/R group)
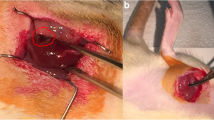
Tripterysium glycosides preconditioning alleviated morphological lesion after renal IRI
The PAS staining of I/R group showed distinct renal injury including tubular necrosis and swelling, and destruction of brush border. In comparison, these severe renal damages significantly were alleviated in the sections of TG + I/R group, and there were no significant morphological lesions in groups sham and TG (Fig. 2a–d). According to the analysis of Jablonski scores of severe acute tubular necrosis (Table 1), TG + I/R group had lower Jablonski scores than I/R group with significant difference. In general, after modeling of 45-min renal ischemia followed by 72-h reperfusion, tripterysium glycosides preconditioning could reduce Jablonski scores of severe acute tubular necrosis.
Tripterysium glycosides preconditioning improved morphological lesion after renal IRI. a–d The results of PAS staining showed that TG + I/R group significantly alleviated the severe I/R renal damages including tubular necrosis and swelling, and destruction of brush border compared with that in I/R group (magnification, 400). Jablonski scores in group TG + I/R were obviously lower than that in group I/R, and there were no significant differences in the Jablonski scores between groups sham and TG (Table 1). However, Jablonski scores in groups TG + I/R and I/R were significantly higher than those in group sham (Table 1). (a sham group, b TG group, c I/R group, d TG + I/R group). (*p < 0.05 vs. sham group, # p < 0.05 vs. I/R group)
Tripterysium glycosides preconditioning inhibited cell apoptosis after renal IRI
Compared to I/R group, apoptosis induced by renal I/R was decreased in group TG + I/R (Fig. 3). Moreover, expression levels of Bax and caspases-3 in TG + I/R group were significantly lower than group I/R. Meanwhile, the level of Bcl-2 was increased in TG + I/R group compared with group I/R according to the results of Western blot (Fig. 4) and immunohistochemistry (Fig. 5), and relevant differences were statistically significant. However, levels of all these makers had no significant difference between groups sham and TG.
Tripterysium glycosides preconditioning could alleviate renal tubular epithelial cell apoptosis induced by renal IRI. The TUNEL staining showed that tripterysium glycosides preconditioning significantly attenuated the renal I/R injury (magnification, 400). Apoptosis index in group TG + I/R was significantly lower than that in group I/R (Table 1). However, Apoptosis index in groups TG + I/R and I/R was significantly higher than that in group sham, and there were no significant differences in Apoptosis index between groups sham and TG. (a Sham group, b TG group, c I/R group, d TG + I/R group)
The tripterysium glycosides preconditioning inhibited the expression of pro-apoptosis associated molecules and promoted the up-regulation of inhibitor apoptosis protein in the I/R model. Compared to sham group, levels of caspases-3 and BAX were significantly increased in I/R group, but the level of Bcl-2 was reduced in I/R group. Compared with I/R group, group TG + I/R obviously inhibited the levels of BAX and caspase-3, and restored the level of Bcl-2. Furthermore, there were no significant differences in the levels of BAX, caspase-3 and Bcl-2 between groups sham and TG. (*p < 0.05 vs. sham group, # p < 0.05 vs. I/R group)
Tripterysium glycosides preconditioning alleviated apoptosis according to the results of immunohistochemistry (magnification, 400). Compared to group I/R, the expression levels of Bax and caspase-3 were reduced in group TG + I/R. Furthermore, the level of Bcl-2 in group TG + I/R was significantly higher than that in group I/R
Tripterysium glycosides pretreatment down-regulated the expression of inflammation marker after renal IRI
In this section, according to the results of Western blot (Fig. 6) and immunohistochemistry (Fig. 6), the expression level of HMGB1 was lower in group TG + I/R than that in group I/R. There were no significant difference in the expression of HMGB1 between groups sham and TG.
Tripterysium glycosides preconditioning reduced the level of HMGB1 in renal tissue of this model. The results of immunohistochemistry showed that level of HMGB1 was significantly reduced in group TG + I/R than that in group I/R (magnification, 400). Compared to group I/R, the level of HMGB1 in group TG + I/R was significantly reduced according to the results of Western blot. Furthermore, there were no significant differences in the level of HMGB1 between group sham and TG (*p < 0.05 vs. sham group, # p < 0.05 vs. I/R group)
Tripterysium glycosides preconditioning inhibited the renal fibrosis induced by renal IRI
In accordance with the results of analyzing the typical molecules in TGF-β/Smad signal pathway by Western blot (Fig. 7) and immunohistochemistry (Fig. 7), compared to group I/R, TG + I/R group significantly reduced the expression of TGF-β1, Smad3 and p-Smad3. However, there were no significant differences in the levels of TGF-β1, Smad3 and p-Smad3 between groups sham and TG. Tripterysium glycosides preconditioning could inhibit the expression of TGF-β1, Smad3 and p-Smad3 after renal I/R. However, there were no significant morphological differences in the Masson staining (the result did not present).
Tripterysium glycosides preconditioning reduced the levels of the renal fibrosis typical molecules in renal tissue of this model. According to the results of immunohistochemistry (magnification, 400) and Western blot, group TG + I/R could significantly down-regulate the levels of TGF-β1, Smad3 and p-Smad3 compared with those in group I/R. Meanwhile, there were no significant differences in the levels of TGF-β1, Smad3 and p-Smad3 between groups sham and TG (*p < 0.05 vs. sham group, # p < 0.05 vs. I/R group)
Discussion
Tripterysium glycosides display potent biological activities, including anti-tumor, anti-inflammatory, immunosuppressive, antifertility and anti-cystogenesis effects [6]. However, up to now, few researches focus on the effect of tripterysium glycosides preconditioning to renal ischemia/reperfusion injury in a rat model.
In this paper, compared to I/R group, tripterysium glycosides preconditioning could significantly improve the renal dysfunction caused by 45-min ischemic reperfusion, which helped to decrease the serum level of creatinine and blood urea nitrogen. A new study suggested that Tripterygium wilfordii polyglycosidium exhibited protective effect on the podocytes of rats with diabetic nephropathy, which was benefit for the improvement of renal function and liver function [7]. According to the section of PAS staining, we found that glycosides preconditioning could alleviate the morphological lesions caused by I/R. In addition, some researches reported that tripterysium glycosides could improve kidney damage to diabetic rats and delay the development of diabetic nephropathy by inhibiting the HIF-1α and ET-1 expression [8]; all those results were coincident with this study.
It is well known that tripterysium glycosides possess the activity of anti-inflammation. It was reported that Tripterygium wilfordii polyglycoside treatment could reduce the expressions of inflammation cytokines in serum and kidney and relieve the nephropathy in diabetic rats mainly by suppressing the nuclear factor kappa B, chemokine (C–C motif), ligand 5 (CCL5), tumor necrosis factor alpha (TNF-α), interleukin-6 (IL-6) and other inflammatory factors [9]. Increasing evidence showed that HMGB1 was an important mediator of I/R injury in liver, spinal cord, brain and intestine, and a potentially injurious innate immune response could be also triggered by HMGB1 [10]. In this study, we found that the expression of HMGB1 was inhibited by tripterysium glycosides preconditioning before renal ischemia reperfusion. Furthermore, some researchers claimed that HMGB1 was an important biomarker of injury in kidney transplantation [11]. The release of HMGB1 during I/R was involved in ROS and Ca2+ signaling, and the activity of HMGB1 was mediated by several receptors such as TLR-4, TLR-9 and RAGE [10], which may associated with the anti-inflammation activity of tripterysium glycosides preconditioning.
The mechanisms of renal I/R injury were complex, which were considered to be associated with the endothelial and epithelial cell dysfunction, caspase activation, inflammation, free radical production, apoptosis and necrosis [12, 13]. In this study, we found that tripterysium glycosides preconditioning could down-regulate the expression of caspase-3 and Bax. Furthermore, the numbers of TUNEL-positive cells were significantly decreased, while the expression of Bcl-2 was increased. Recently, scholars have found that Triptolide and 2,4-diamino-6-hydroxypyrimidine pretreatment significantly reduced the expression of caspase-3, cleaved caspase-3 and NF-κB and increased the expression of Bcl-2 in cerebral ischemia [14]. In addition, Tripterygium glycoside significantly reduced the expression of Bax, while attenuated the reduction of Bcl-2 in the rat model of nerve transplantation [15]. All these results were consistent with our study.
To our knowledge, TGF-β1 and Smad3 are the typical molecules in TGF-β signal pathway, which are closely related to fibrosis. In this paper, we found that tripterysium glycosides preconditioning could down-regulate the expression of TGF-β1, Smad3 and p-Smad3. Though there were no significant differences in Masson staining. Other researches have showed that low-dose multi-glycoside of Tripterygium wilfordii Hook.f. could effectively and safely ameliorated the prolonged glomerulosclerosis in focal segmental glomerulosclerosis model, via the potential molecular mechanisms involved with the reduction in extracellular matrix components and the suppression of TGF-β1 over-expression, as well as the bidirectional regulation of TGF-β1/Smad signaling activity [16]. Furthermore, researches have showed that Triptolide attenuated renal interstitial fibrosis in rats with unilateral ureteral obstruction [17]. All these results demonstrated that tripterysium glycosides had the activity of alleviating fibrosis.
In summary, this study demonstrated that tripterysium glycosides preconditioning could attenuate the renal I/R injury by alleviating inflammation and reducing the apoptosis in rat model. Furthermore, it also could reduce the levels of TGF-β1, Smad3 and p-Smad3, which showed that tripterysium glycosides could help to alleviate the renal fibrosis. However, the long-term effects of tripterysium glycosides on renal ischemia–reperfusion still needed to be studied further, and additional studies exploring the exactly biological activity mechanism of tripterysium glycosides were also demanded.
Conclusion
The pretreatment with tripterysium glycosides has protective effect on kidney ischemia/reperfusion injury, and the potential mechanism might be related to the activities of anti-inflammation, reducing apoptosis and alleviating renal fibrosis.
References
Gorsuch WB, Chrysanthou E, Schwaeble WJ et al (2012) The complement system in ischemia–reperfusion injuries. Immunobiology 217(11):1026–1033
Ditonno P, Impedovo SV, Palazzo S et al (2013) Effects of ischemia-reperfusion injury in kidney transplantation: risk factors and early and long-term outcomes in a single center. Transplant Proc 45(7):2641–2644
Lin Na, Liu Chun-fang, Xiao Cheng et al (2007) Triptolide, a diterpenoid triepoxide, suppresses inflammation and cartilage destruction in collagen-induced arthritis mice. Biochem Pharmacol 73(1):136–146
Zhou Heng, Guo Wei, Long Cong et al (2015) Triptolide inhibits proliferation of Epstein-Barr virus-positive B lymphocytes by down-regulating expression of a viral protein LMP1. Biochem Biophys Res Commun 456(3):815–820
Wong KF, Yuan Y, Luk JM (2012) Tripterygium wilfordii bioactive compounds as anticancer and anti-inflammatory agents. Clin Exp Pharmacol Physiol 39(3):311–320
Zhou Zhao-Li, Yang Ya-Xi, Ding Jian et al (2012) Triptolide: structural modifications, structure–activity relationships, bioactivities, clinical development and mechanisms. Nat Prod Rep 29(4):457–475
Hao Li, Pan Meng-shu, Zheng Y et al (2014) Effect of Cordyceps sinensis and Tripterygium wilfordii polyglycosidium on podocytes in rats with diabetic nephropathy. Exp Ther Med 7(6):1465–1470
Chen WD, Chang BC, Zhang Y et al (2015) Effect of Tripterygium glycosides on expression of hypoxia inducible factor-1α and endothelin-1 in kidney of diabetic rats. Nan Fang Yi Ke Da Xue Xue Bao 35(4):499–505
Liu G, Shen Y, You L et al (2014) Tripterygium wilfordii polyglycoside suppresses inflammatory cytokine expression in rats with diabetic nephropathy. Xi Bao Yu Fen Zi Mian Yi Xue Za Zhi 30(7):721–724
Kang Rui, Chen Ruo-chan, Zhang Qiu-hong et al (2014) HMGB1 in health and disease. Mol Aspects Med 40:1–116
Krüger B, Krick S, Dhillon N et al (2009) Donor Toll-like receptor 4 contributes to ischemia and reperfusion injury following human kidney transplantation. Proc Natl Acad Sci USA 106(9):3390–3395
Burne-Taney MJ, Kofler J, Yokota N et al (2003) Acute renal failure after whole body ischemia is characterized by inflammation and T cell-mediated injury. Am J Physiol Renal Physiol 285(1):F87–F94
Yang B, Jain S, Pawluczyk IZ et al (2005) Inflammation and caspase activation in long-term renal ischemia/reperfusion injury and immunosuppression in rats. Kidney Int 68(5):2050–2067
Li W, Yang Y, Hu Z et al (2015) Neuroprotective effects of DAHP and Triptolide in focal cerebral ischemia via apoptosis inhibition and PI3 K/Akt/mTOR pathway activation. Front Neuroanat 9:48
Huang Y, Jiang D, Chen L et al (2009) Effects of Tripterygium glycoside on apoptosis of the skeletal muscle after nerve allograft. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 23(1):101–105
Wan YG, Che XY, Sun W et al (2014) Low-dose of multi-glycoside of Tripterygium wilfordii Hook.f., a natural regulator of TGF-β1/Smad signaling activity improves adriamycin-induced glomerulosclerosis in vivo. J Ethnopharmacol 151(3):1079–1089
Yuan XP, He XS, Wang CX et al (2011) Triptolide attenuates renal interstitial fibrosis in rats with unilateral ureteral obstruction. Nephrology 16(2):200–210
Acknowledgments
This study was supported by the National Natural Science Foundation of China (No. 81400753), Hubei Natural Science Foundation (No. 2014CFB362), the bureau of public health of Hubei province (JX6B14) and the project of Wuhan Municipal Science and Technology Bureau (2013062301010808).
Author’s contributions
Zhi-shun Wang carried out the design of the study. Tao Qiu participated in the design and helped to draft the manuscript. Zhong-bao Chen carried out the experiment. Xiu-heng Liu performed the statistical analysis. Jiang-qiao Zhou, Long Zhang, Ye Shen and Lu Zhang carried out some parts of the study. All authors read and approved the final manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest.
Additional information
Zhi-shun Wang and Tao Qiu contributed equally to this work as co-first authors.
Rights and permissions
About this article
Cite this article
Wang, Zs., Qiu, T., Liu, Xh. et al. Tripterysium glycosides preconditioning attenuates renal ischemia/reperfusion injury in a rat model. Int Urol Nephrol 48, 213–221 (2016). https://doi.org/10.1007/s11255-015-1160-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-015-1160-4