Abstract
Purpose
Hyponatremia is a common disorder and hyponatremia in the outpatient setting is not extensively studied. Our aim was to investigate the characteristics of hyponatremia in ambulatory patients.
Methods
Seventy-six adult outpatients with hyponatremia were enrolled in this prospective study. Demographic features, presenting symptoms and signs, associating morbidities, medications, laboratory findings, mortalities, and length of hospital stay, were recorded.
Results
Mean age was 74.7 ± 12.7 years, and 52 (68.4 %) were female whereas 24 (31.6 %) were male. Mean sodium concentration was 123.6 ± 6.6 mEq/L. Leading cause was thiazide diuretic use (n = 37, 48.7 %) and approximately half of the patients (n = 40, 52.6 %) had a multifactorial etiology. Severe hyponatremia (sodium < 125 mEq/L) was identified in 37 (48.7 %). Thiazide diuretic use, vomiting, and apathy were independent predictors of severe hyponatremia. Eight (10.5 %) patients had a mortal course. A relatively younger age, male gender, presenting sign of lethargy, associating morbidities of malignancy, chronic liver disease, and hypoalbuminemia were risk factors for mortality.
Conclusions
Hyponatremia is prevalent among elderly, especially in women and with thiazide diuretics. Apart from the trend toward sodium depletion observed in healthy elderly which occurs due to changes in the tubular handling of sodium, a multifactorial etiology including thiazides seems to predict the occurrence and the severity of hyponatremia. Hyponatremia may be a significant cause of mortality in seniors. A relatively younger age, male gender, association of cirrhosis, malignancy, and hypoalbuminemia predict mortality. In elderly outpatients, identification of the risk factors for hyponatremia and close monitoring are imperative to reduce the related mortality and morbidity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hyponatremia, a serum sodium concentration less than 135 mEq/L, is the most common electrolyte disorder encountered in clinical practice, especially in hospital in-patients [1]. Clinical manifestations of hyponatremia are nonspecific and range from anorexia, nausea, and malaise to headache, decreased level of consciousness, seizures, and coma. Severe hyponatremia is defined as a serum sodium concentration less than 125 mEq/L and is a serious electrolyte disorder associated with significant morbidity and mortality [2, 3]. There are numerous etiologic factors for hyponatremia, covering a broad spectrum of diseases, pharmacologic agents, and physiopathological processes. The clinical management of hyponatremia basically consists of identification and treatment of the underlying cause(s) and restoring the altered salt and water balance [4].
Hyponatremia, its clinical characteristics, and the association between hyponatremia and in-hospital mortality have been well documented in hospitalized patients by numerous studies [5]. However, with regard to hyponatremia identified in the outpatient setting, there is only limited data in the literature. In this study, hyponatremia diagnosed in the outpatient setting was put under the scope and our aim was to identify the risk factors, clinical characteristics, and outcome of hyponatremia identified in the outpatient population.
Materials and methods
This was a prospective and observational study of a series of outpatients with a diagnosis of hyponatremia on their admission to hospital. The study was reviewed and approved by the local ethics committee of Ufuk University School of Medicine and was conducted according to the ethical standards laid down in the Declaration of Helsinki. All patients gave their written informed consent prior to their inclusion in the study.
Seventy-six adult outpatients were enrolled between September 2011 and February 2013. Hyponatremia was defined as a serum sodium concentration less than 135 mEq/L, while severe hyponatremia was defined as a serum sodium concentration less than 125 mEq/L [2]. With regard to eligibility, patients younger than 18 years of age and patients developing hyponatremia following hospitalization were excluded (Table 1).
The relevant data of the patients were retrieved from Ufuk University School of Medicine Hospital electronic medical record system on a day-to-day basis and patients were tracked until their discharge or deaths. The demographics, presenting symptoms and signs, associated morbidities, prior history of hyponatremia, medication history, and clinical examination findings (including a clinical evaluation of volume status) were recorded at the time of hospital admission (Table 2). As one of the main focuses of the present study was the risk factors for hyponatremia in outpatients, a careful and comprehensive etiological classification had been performed. Because of this detailed etiological classification and the frequent use of diuretics in our study population which clearly has an unargued effect on the volume status, the data regarding the volume status of the patients were not further evaluated. In addition, the admission laboratory data, the serum sodium concentration follow-up, the length of hospital stay, and the outcome of the patients were also obtained (Table 2).
Data analyses were carried out using the SPSS 17 software (SPSS Statistics for Windows, version 17.0, Chicago, SPSS Inc.). Continuous variables were expressed as mean ± SD and categorical variables as percentages (%). For comparing the means of two independent groups, the t test was used, whereas comparison of the proportions of two independent groups was performed by Chi-square (χ 2) test. The risk factors associated with severe hyponatremia and mortality were further investigated using logistic regression analysis. p ≤ 0.05 was considered to be statistically significant.
Results
The mean age of the 76 patients enrolled in the study was 74.7 ± 12.7 years, and 24 (31.6 %) of these patients were male and 52 (68.4 %) were female. On admission, their mean serum sodium concentration was 123.6 ± 6.6 mEq/L and 37 (48.7 %) patients had severe hyponatremia.
The patients with a diagnosis of congestive heart failure and/or chronic liver disease had been following a low-sodium diet but as a 24-h urine analysis was not performed and 37 (48.7 %) patients were on thiazides and 33 (43.4 %) patients were on loop diuretics, it was not possible to obtain an objective measure of the patients’ sodium intake.
Most frequent constitutional and central nervous system symptoms were anorexia (n = 58, 76.3 %) and apathy (n = 27, 35.5 %), respectively. While congestive heart failure (n = 24, 31.6 %) was the most common accompanying clinical condition, thiazide diuretics (n = 37, 48.7 %) were the most commonly associated pharmacologic agents. Twenty-six (34.2 %) patients had a prior history of hyponatremia. In 36 (47.4 %) patients, only one risk factor for hyponatremia was identified, whereas 40 (52.6 %) patients had two or more risk factors for hyponatremia. The serum creatinine and hemoglobin levels were 0.86 ± 0.28 mg/dL and 11.35 ± 1.58 g/dL, respectively. The mean length of hospital stay was 10.8 ± 5.9 days and a total of 8 (10.5 %) deaths were observed. Essential clinical and laboratory characteristics of the study population are summarized in Table 3 (statistically significant values are marked in bold, p < 0.05).
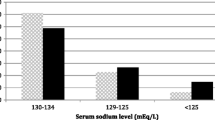
With respect to the presence of severe hyponatremia, the patients were divided into two groups, namely “Na+ < 125” (severe hyponatremia group, serum sodium concentration <125 mEq/L, n = 37) and “Na+ ≥ 125” (mild-to-moderate hyponatremia group, 125 mEq/L ≤ serum sodium concentration < 135 mEq/L, n = 39). The comparison of these two groups is presented in Table 3. As can be seen from the table, the two groups were similar with regard to demographics. Anorexia, vomiting, and apathy were more common in Na+ < 125 group (p = 0.05, p = 0.03, and p = 0.03, respectively). There was a significant association between the use of thiazide diuretics and the presence of severe hyponatremia (p = 0.01). Interestingly, both chronic liver disease and mortalities were more common in Na+ ≥ 125 group (p = 0.02 and p = 0.05, respectively). As expected, length of hospital stay was longer (p < 0.001) and therapeutic use of hypertonic saline more common (p < 0.001) in patients with severe hyponatremia.
The logistic regression analysis including the clinical characteristics associated with severe hyponatremia documented that the use of thiazide diuretics (p = 0.005), the presence of apathy (p = 0.009), and the symptom of vomiting (p = 0.01) were independent predictors of severe hyponatremia.
With regard to mortality, two groups were created, namely “mortality (+)” (n = 8) and “mortality (−)” (n = 68). The comparison of the mortality (+) and mortality (−) groups is presented in Table 3. The mean age of the mortality (+) group was significantly lower (61.8 ± 12.0 versus 76.2 ± 12.0 years, p = 0.002). There was also a statistically important gender difference between the two groups. The male/female ratio was 6/2 (3.00) in the mortality (+) group, whereas it was 18/50 (0.36) in the mortality (−) group (p = 0.01). With respect to their mean serum sodium concentrations, the mortality (+) group had a significantly higher level (128.3 ± 4.6 versus 123.1 ± 6.6 mEq/L, p = 0.03). There were associations between the presenting signs of agitation and lethargy and the occurrence of mortality (p = 0.05 and p = 0.02, respectively). Hypoalbuminemia, chronic liver disease, and malignancies were significantly more common in the mortality (+) group (p = 0.03, p = 0.005, and p < 0.001, respectively). Conversely, the use of thiazide diuretics and the occurrence of severe hyponatremia were more frequently observed in the mortality (−) group (p = 0.05 for both).
The significant characteristics associated with mortality were analyzed by logistic regression. The presenting sign of lethargy (p = 0.02) and the associated morbidities of chronic liver disease (p = 0.02) and malignancy (p = 0.01) were found to be the independent predictors of mortality.
Discussion
Hyponatremia is the most common electrolyte abnormality among hospitalized patients and is definitely associated with adverse outcomes including an increase in mortality. Regarding hyponatremia occurring in outpatients, congestive heart failure is the most frequently studied clinical scenario [6–10]. Excluding the studies performed in heart failure, the data available on hyponatremia in the ambulatory setting are limited [11–15]. Specifically focusing on hyponatremia documented in ambulatory patients, the present study not only verified several essential facts regarding hyponatremia but also pointed to some significant prognostic factors of mortality in hyponatremic outpatients.
Age-related physiological changes (e.g., decreased glomerular filtration and renal diluting capacity, reduced activity of the renin-angiotensin-aldosterone system, decreased cardiac output), associated comorbidities (e.g., congestive heart failure, chronic obstructive pulmonary disease, diarrhea, hypoalbuminemia, hypovolemia, malignancies, pneumonia, stroke, syndrome of inappropriate antidiuretic hormone secretion), and commonly used medications in the elderly (e.g., thiazide diuretics, loop diuretics, laxatives, selective serotonin reuptake inhibitors), put older people at significant risk of hyponatremia [1, 16–18]. In accordance with the literature on hyponatremia, the hyponatremic patients in our study had a mean age of 74.7 years.
An apparently idiopathic form of hyponatremia is also documented in the geriatric population and solely aging is suggested as an independent etiology for hyponatremia [14]. As is well known, with the aging of the nephron both the glomerular and the tubular functions decrease. Consequently, the aging nephron demonstrates a reduced capacity to conserve sodium, especially during a low-sodium diet [19]. The two main points emphasized with regard to urinary sodium losses in the healthy elderly are a reduced capacity for sodium reabsorption in the ascending limb of Henle and a low aldosterone level [19, 20]. Even without any additional factors, these two changes on their own seem to account for the occurrence of hyponatremia in the aged population.
Hyponatremia in general and particularly hyponatremia secondary to the use of thiazide diuretics is more prevalent among women [3, 11, 21–23]. In female subjects, a similar propensity to develop hyponatremia also seems to be valid for a couple of different etiologies [24, 25]. Correspondingly, in outpatients presenting with hyponatremia, our study documented a female-to-male ratio of approximately 2.2. While it is still unclear why hyponatremia is observed more frequently in women than men, hormones, medications, and a lower body mass index have been implicated as confounding factors. We believe that the significantly frequent use of thiazide diuretics was another important factor accounting for the female dominance documented in this study.
Hyponatremia frequently has a multifactorial etiology, which is especially true for elderly patients [23, 26]. As such, nearly half (52.6 %) of the patients in this study also had two or more risk factors for hyponatremia. This value is pretty consistent with the 51 % reported by Shapiro et al. [23]. With regard to hyponatremia occurring in the outpatient setting, congestive heart failure, coronary artery disease, chronic obstructive pulmonary disease, diabetes mellitus, hypertension, stroke, cancer, cirrhosis, psychiatric disorders, and syndrome of inappropriate antidiuretic hormone secretion are the most commonly reported comorbid conditions [11–15]. Thiazides, potassium-sparing diuretics, selective serotonin reuptake inhibitors, and benzodiazepines are the pharmacologic agents associated with hyponatremia in outpatients [11–15]. Furthermore, an increased intake of fluids and strict adherence to a low-sodium diet definitely contribute to the development of hyponatremia. In the ambulatory setting, the most emphasized and also the most throughly studied risk factors for hyponatremia have been congestive heart failure and thiazide diuretics. In patients with congestive heart failure, hyponatremia often develops secondary to the activation of compensatory neurohormonal systems causing low serum sodium levels [27]. Concerning thiazides, these diuretics are known to solely cause hyponatremia or contribute to and aggravate hyponatremia caused by various other disorders [28]. While causing hyponatremia, thiazides seem to act heavily by impairing renal diluting mechanisms [28]. Consistent with the literature, the presence of congestive heart failure and the use of thiazide diuretics were the most commonly associated factors (31.6 and 48.7 %, respectively) in our series of hyponatremic outpatients.
As is known, the symptoms and signs of hyponatremia are universal and include anorexia, nausea and vomiting, fatigue, headache, apathy, confusion, progressive decrease in level of consciousness, seizures, and coma [29]. It is also known that these clinical manifestations result from the osmotic water shift leading to cerebral edema. Characteristically, as the serum sodium concentration falls, the symptoms and signs of hyponatremia become more severe. This trend was also observed in the present study. The symptoms and signs of anorexia, vomiting, and apathy were more common in patients with severe hyponatremia. Furthermore, vomiting and apathy were independent predictors of severe hyponatremia.
In this study, the use of thiazide diuretics was significantly more prevalent in the severe hyponatremia group. In our opinion, the potential explanation for this finding lies in the impairing effects of thiazides on renal diluting mechanisms. By this route, thiazides may be strongly aggravating hyponatremia caused by various other disorders. In our study, the frequency of thiazide diuretic use was 64.9 % among patients with severe hyponatremia. So it seems most probable that, in a significant proportion of severely hyponatremic patients receiving thiazides, one or more additional risk factors for hyponatremia were also present. Supportingly, in their study reviewing severe hyponatremia in elderly hospitalized patients, Shapiro et al. [23] demonstrated that all patients with thiazide-induced hyponatremia had other contributing factors. Moreover, in logistic regression, the use of thiazide diuretics was also identified as an independent predictor of severe hyponatremia. In a recent report by Rodenburg et al., the risk of severe hyponatremia was found to be eight times higher in patients receiving thiazides [30].
The present study documented a significantly higher mortality rate in the mild-to-moderate hyponatremia group compared to the severe hyponatremia group (17.9 and 2.7 %, respectively). A similar trend was also observed in the study by Waikar et al. [31]. Although different from expected, we believe that there are possible explanations for this finding. First, the well-known and significant risk for mortality observed in acute and severe hyponatremia may not be effectual for this study. As conducted on ambulatory patients, it is reasonable to state that our study mainly included chronic hyponatremia patients regardless of their sodium levels. Secondly, studies of mortality of hyponatremic patients consistently documented an increased risk of death even with mild degrees of hyponatremia [11–13, 32]. Thirdly and perhaps most importantly, there is an essential yet unanswered question which asks “whether hyponatremia itself is contributing directly to mortality or is serving as an unfavorable prognostic marker for other risk factors.” Although the exact reason of our finding of increased mortality in the less severe hyponatremia group is not clear, we believe that higher frequencies of both chronic liver disease (20.5 % for “Na+ ≥ 125” and 2.7 % for “Na+ < 125”) and malignancies (15.4 % for “Na+ ≥ 125” and 8.1 % for “Na+ < 125”) in the mild-to-moderate hyponatremia group are contributing significantly to the increased mortality rate. In patients with liver cirrhosis and congestive heart failure, hyponatremia is known to predict mortality. So it seems acceptable to propose that hyponatremia in some instances does act as a severity marker of an illness and may predict mortality rather than directly causing it.
As previously mentioned, even mild degrees of hyponatremia is shown to be associated with an increased risk of mortality [12, 13, 32]. The present study documented a mortality rate of 10.5 % which is in good accordance with the figure of 10 % reported by Vu et al. [33]. The same study, which was performed on outpatients presenting with severe hyponatremia, was not able to document an association between increased mortality and the severity of hyponatremia on admission. Likewise, on the contrary to the expected, the mean serum sodium concentration of the patients with a mortal course was significantly higher in our study. Again, rather than being a direct consequence of hyponatremia, mortalities occurring in the present study are thought to be strongly related to the markedly increased frequencies of chronic liver disease and malignancies. In other words, hyponatremia seemed not only to cause but also to predict mortality by acting as a severity marker for chronic liver disease and malignancies.
Another explanation for the deaths observed in our study may come from the age distribution of the patients. As is known, the human brain is shown to loose volume and begin to atrophy following the third decade of life [34]. Consequently, the brain volume of an 80-year-old individual is expected to decrease by nearly 25 %. It is believed that in elderly patients, the reduction in the brain volume serves as a protecting mechanism against hyponatremic brain injury. A similar protective effect of the increasing age was also documented in an experimental rat model of hyponatremic encephalopathy [35]. Accordingly, the patients demonstrating a mortal course in the present study had a relatively but significantly younger mean age with respect to the patients with no mortalities.
In patients with hyponatremia, regarding the effects of gender differences on mortality, the current literature hosts reports with conflicting results. In addition to the deleterious effects of both sexes, no significant differences in mortality with respect to gender are also reported [4, 11, 12, 23, 35–37]. In their study, Rao et al. [37] concluded that, though occurring more frequently in females, hyponatremia was better tolerated by the female patients and mortality related to hyponatremia was more prevalent in the male counterparts. The findings of our study were in accordance with the results of the study by Rao et al. and indicated a significantly increased risk of mortality in male patients with hyponatremia.
In the present study, hypoalbuminemia was shown to be a significant risk factor for mortality. Previously, in hyponatremic patients, hypoalbuminemia had been documented to be an independent risk factor for mortality. The same study had also shown that hypoalbuminemia was a predictor of neurological manifestations of hyponatremia [23]. It is important to note that in our study, the presenting sign of lethargy was also significantly more common among the patients with mortalities. As such, it seems possible that hypoalbuminemia, not on its own but when accompanying hyponatremia, potentiates the osmotic water shift leading to cerebral edema. Another important explanation for this finding may be hypoalbuminemia’s being a poor prognostic marker for both chronic liver disease and malignant neoplasms [38–41]. In this study, it is likely that serum albumin concentration was also acting as a strong indicator of disease severity. Accordingly, the logistic regression analysis documented three independent predictors of mortality in hyponatremic patients, namely the presenting sign of lethargy and the associated morbidities of chronic liver disease and malignancy, but not hypoalbuminemia.
Although prospective in design, the relatively small number of patients enrolled may be mentioned as the major limitation of our study. Nevertheless, yielding several important findings consistent with the literature and verifying many essential facts regarding hyponatremia, the present study proved its reliability with respect to data collection and analysis. So, while clearly emphasizing the importance of a larger study population, we believe that the results of this study provide valuable information with regard to hyponatremia in outpatients, specifically about factors predicting severity and mortality.
Hyponatremia is a common disorder among elderly, especially in women and when thiazide use is present. A multifactorial etiology including thiazides seems to predict the severity of hyponatremia. Vomiting and apathy are important manifestations characterizing severe hyponatremia. In the elderly population, hyponatremia may be a significant cause of mortality. A relatively younger age, male gender, association of a serious systemic disorder, and presence of hypoalbuminemia predict a mortal course among hyponatremic patients and lethargy is a pernicious sign in hyponatremia strongly associating mortality; especially in elderly outpatients, identification of the risk factors for hyponatremia and close monitoring of these patients are imperative to reduce the related mortality and morbidity. The question of “Do patients die from or with hyponatremia?” is still to be answered [42]. According to the authors of this study, there is not a single answer to this question, with the answer being dependent on the specific clinical circumstances.
References
Anderson RJ, Chung HM, Kluge R, Schrier RW (1985) Hyponatremia: a prospective analysis of its epidemiology and the pathogenetic role of vasopressin. Ann Intern Med 102:164–168
Mount DB (2012) Fluid and electrolyte disturbances. In: Longo DL, Fauci AS, Kasper DL, Hauser SL, Jameson JL, Loscalzo J (eds) Harrison’s principles of internal medicine, 18th edn. McGraw-Hill, New York, pp 341–359
Tzamaloukas AH, Malhotra D, Rosen BH, Raj DS, Murata GH, Shapiro JI (2013) Principles of management of severe hyponatremia. J Am Heart Assoc 2:e005199
Lien YH, Shapiro JI (2007) Hyponatremia: clinical diagnosis and management. Am J Med 120:653–658
Corona G, Giuliani C, Parenti G et al (2013) Moderate hyponatremia is associated with increased risk of mortality: evidence from a meta-analysis. PLoS One 8:e80451
Bavishi C, Ather S, Bambhroliya A et al (2014) Prognostic significance of hyponatremia among ambulatory patients with heart failure and preserved and reduced ejection fractions. Am J Cardiol 113:1834–1838
Miller WL, Grill DE, Struck J, Jaffe AS (2013) Association of hyponatremia and elevated copeptin with death and need for transplantation in ambulatory patients with chronic heart failure. Am J Cardiol 111:880–885
Gheorghiade M, Abraham WT, Albert NM et al (2007) Relationship between admission serum sodium concentration and clinical outcomes in patients hospitalized for heart failure: an analysis from the OPTIMIZE-HF registry. Eur Heart J 28:980–988
Bettari L, Fiuzat M, Shaw LK et al (2012) Hyponatremia and long-term outcomes in chronic heart failure—an observational study from the Duke Databank for Cardiovascular Diseases. J Card Fail 18:74–81
Gheorghiade M, Rossi JS, Cotts W et al (2007) Characterization and prognostic value of persistent hyponatremia in patients with severe heart failure in the ESCAPE trial. Arch Intern Med 167:1998–2005
Mohan S, Gu S, Parikh A, Radhakrishnan J (2013) Prevalence of hyponatremia and association with mortality: results from NHANES. Am J Med 126:1127–1137
Gankam-Kengne F, Ayers C, Khera A, de Lemos J, Maalouf NM (2013) Mild hyponatremia is associated with an increased risk of death in an ambulatory setting. Kidney Int 83:700–706
Liamis G, Rodenburg EM, Hofman A, Zietse R, Stricker BH, Hoorn EJ (2013) Electrolyte disorders in community subjects: prevalence and risk factors. Am J Med 126:256–263
Miller M, Hecker MS, Friedlander DA, Carter JM (1996) Apparent idiopathic hyponatremia in an ambulatory geriatric population. J Am Geriatr Soc 44:404–408
Miller M, Morley JE, Rubenstein LZ (1995) Hyponatremia in a nursing home population. J Am Geriatr Soc 43:1410–1413
Ayus JC, Arieff AI (1996) Abnormalities of water metabolism in the elderly. Semin Nephrol 16:277–288
Cowen LE, Hodak SP, Verbalis JG (2013) Age-associated abnormalities of water homeostasis. Endocrinol Metab Clin North Am 42:349–370
Mannesse CK, Vondeling AM, van Marum RJ, van Solinge WW, Egberts TC, Jansen PA (2013) Prevalence of hyponatremia on geriatric wards compared to other settings over four decades: a systematic review. Ageing Res Rev 12:165–173
Epstein M, Hollenberg NK (1976) Age as a determinant of renal sodium conservation in normal man. J Lab Clin Med 87:411–417
Dontas AS, Marketos SG, Papanayiotou P (1972) Mechanisms of renal tubular defects in old age. Postgrad Med J 48:295–303
Sonnenblick M, Friedlander Y, Rosin AJ (1993) Diuretic-induced severe hyponatremia. Review and analysis of 129 reported patients. Chest 103:601–606
Sharabi Y, Illan R, Kamari Y et al (2002) Diuretic induced hyponatraemia in elderly hypertensive women. J Hum Hypertens 16:631–635
Shapiro DS, Sonnenblick M, Galperin I, Melkonyan L, Munter G (2010) Severe hyponatraemia in elderly hospitalized patients: prevalence, aetiology and outcome. Intern Med J 40:574–580
Schucany WG (2007) Exercise-associated hyponatremia. Proc (Bayl Univ Med Cent) 20:398–401
Moritz ML, Kalantar-Zadeh K, Ayus JC (2013) Ecstacy-associated hyponatremia: why are women at risk? Nephrol Dial Transplant 28:2206–2209
Correia L, Ferreira R, Correia I et al (2014) Severe hyponatremia in older patients at admission in an internal medicine department. Arch Gerontol Geriatr 59:642–647
Filippatos TD, Elisaf MS (2013) Hyponatremia in patients with heart failure. World J Cardiol 5:317–328
Hix JK, Silver S, Sterns RH (2011) Diuretic-associated hyponatremia. Semin Nephrol 31:553–566
Schrier RW (2010) Does “asymptomatic hyponatremia” exist? Nat Rev Nephrol 6:185
Rodenburg EM, Hoorn EJ, Ruiter R et al (2013) Thiazide-associated hyponatremia: a population-based study. Am J Kidney Dis 62:67–72
Waikar SS, Mount DB, Curhan GC (2009) Mortality after hospitalization with mild, moderate, and severe hyponatremia. Am J Med 122:857–865
Hoorn EJ, Zietse R (2013) Hyponatremia and mortality: moving beyond associations. Am J Kidney Dis 62:139–149
Vu T, Wong R, Hamblin PS, Zajac J, Grossmann M (2009) Patients presenting with severe hypotonic hyponatremia: etiological factors, assessment, and outcomes. Hosp Pract 37:128–136
Courchesne E, Chisum HJ, Townsend J et al (2000) Normal brain development and aging: quantitative analysis at in vivo MR imaging in healthy volunteers. Radiology 216:672–682
Arieff AI, Kozniewska E, Roberts TP, Vexler ZS, Ayus JC, Kucharczyk J (1995) Age, gender, and vasopressin affect survival and brain adaptation in rats with metabolic encephalopathy. Am J Physiol 268:R1143–1152
Ayus JC, Achinger SG, Arieff A (2008) Brain cell volume regulation in hyponatremia: role of sex, age, vasopressin, and hypoxia. Am J Physiol Renal Physiol 295:F619–624
Rao MY, Sudhir U, Anil Kumar T, Saravanan S, Mahesh E, Punith K (2010) Hospital-based descriptive study of symptomatic hyponatremia in elderly patients. J Assoc Physicians India 58:667–669
Jalan R, Bernardi M (2013) Effective albumin concentration and cirrhosis mortality: from concept to reality. J Hepatol 59:918–920
Gines P, Guevara M (2008) Hyponatremia in cirrhosis: pathogenesis, clinical significance, and management. Hepatology 48:1002–1010
Phillips A, Shaper AG, Whincup PH (1989) Association between serum albumin and mortality from cardiovascular disease, cancer, and other causes. Lancet 2:1434–1436
Goldwasser P, Feldman J (1997) Association of serum albumin and mortality risk. J Clin Epidemiol 50:693–703
Chawla A, Sterns RH, Nigwekar SU, Cappuccio JD (2011) Mortality and serum sodium: do patients die from or with hyponatremia? Clin J Am Soc Nephrol 6:960–965
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no potential conflicts of interests with respect to the authorship and/or publication of this article.
Rights and permissions
About this article
Cite this article
Tasdemir, V., Oguz, A.K., Sayın, I. et al. Hyponatremia in the outpatient setting: clinical characteristics, risk factors, and outcome. Int Urol Nephrol 47, 1977–1983 (2015). https://doi.org/10.1007/s11255-015-1134-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-015-1134-6