Abstract
Objective
To compare the efficacy and safety of percutaneous ethanol and polidocanol sclerotherapy in the management of simple renal cysts.
Materials and methods
Between 2008 and 2013, symptomatic Bosniak type I renal cysts with a diameter larger than 5 cm in ultrasonography (US) or computed tomography were included in the study and divided into two groups. Group 1 patients were treated by US-guided percutaneous polidocanol sclerotherapy, and group 2 patients were treated by US-guided percutaneous ethanol sclerotherapy. The pre-operative and postoperative US findings were documented to compare the cyst recurrence and the reduction in cyst size. Success was defined as complete or partial: as >90 % reduction or 50–90 % reduction in cyst size, respectively. Failure was defined as <50 % reduction in cyst size. The success rates of two groups were compared. Intraoperative pain was assessed using a visual analog scale (VAS) just after the operation.
Results
The median follow-up period was 36 months (range 12–76) in group 1 and 39 months (range 10–78) in group 2. Group 1 consists of 86 patients with 89 simple renal cysts, and group 2 consists of 57 patients with 57 simple renal cysts. Anatomical success was documented in 49 (55.1 %) and 48 (84.2 %) cysts in groups 1 and 2, respectively (p < 0.001). Clinical success was seen in 56 (65.1 %) and 43 (75.4 %) patients in groups 1 and 2, respectively. Major complication was detected in only one patient in group 2 (aseptic psoas abscess), and there was not any major complication in group 1. Minor complications had occurred in ten patients in group 2 (microscopic hematuria in six patients and fever and nausea in four patients) and in eight patients in group 1 (microscopic hematuria in six patients and fever and nausea in two patients). The mean VAS scores were 21 ± 1.04 and 4.26 ± 1.99 in ethanol and polidocanol groups, respectively (p < 0.001). Ethanol was found to be significantly painful, compared to polidocanol in the sclerotherapy of simple renal cysts.
Conclusions
Although the complication rates and VAS scores of ethanol sclerotherapy are higher than those of polidocanol sclerotherapy, its success rates appear to be also higher. The decision of which sclerosing agent will be used should be based on patients’ comorbidities, cyst location and the surgeon’s experience.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Simple renal cysts are common and usually asymptomatic in adults. However, some patients may experience symptoms and signs as flank pain, hematuria, cyst rupture, hemoperitoneum or hypertension [1]. Symptomatic renal cysts can be managed by a variety of surgical and percutaneous methods, including percutaneous aspiration (with or without injection of a sclerosing agent), endoscopic marsupialization or excision, open surgery and laparoscopic cyst excision [2, 3]. Because of less pain, less bleeding and shorter hospitalization time, percutaneous sclerotherapy is more widely used compared to the other treatment methods [4]. It can be performed as outpatient procedure, and it is reliable, easy to apply and very cost-effective [2]. The sclerosing agents used for percutaneous sclerotherapy are minocycline, bismuth phosphate, ethanolamine oleate, povidone iodine, polidocanol, ethanol and acetic acid [5–8]. There are some important factors when selecting a sclerosing agent such as availability and cost-effectiveness. It should also be very effective with minimum systemic and local complications. In this study, we wanted to compare the efficacy and safety of ethanol and polidocanol in percutaneous sclerotherapy of simple renal cysts during a 5-year period.
Materials and methods
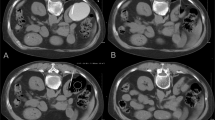
Between 2008 and 2013, symptomatic Bosniak type I renal cysts with a diameter larger than 5 cm in ultrasonography or computed tomography were included in the study and divided into two groups. Group 1 consists of 86 patients with 89 simple renal cysts treated by US-guided percutaneous polidocanol sclerotherapy, and group 2 consists of 57 patients with 57 simple renal cysts treated by US-guided percutaneous ethanol sclerotherapy. The volume (V) of each cyst was calculated as V = d3/6 (d = diameter of the cyst for a spherical lesion and d = (l × w × d)/3 for a nonspherical lesion, where l, w and d is length, width and depth of the cyst, respectively [9]. All cysts were initially evaluated with US, and if there was a suspicion of communicating with collecting system, they underwent contrasted CT or intravenous pyelography (IVP). Initial cyst puncture was performed by an 18-G needle under US guidance in prone position under local anesthesia with lidocaine. The first 10 ml of aspirate was taken for cytological and biochemical examination. In group 1, all of the cystic fluid was aspirated and 2 ml of 1 % polidocanol was injected into the cystic cavity per 100 ml of cystic fluid. In group 2, a 4.7-Fr pig-tail catheter used for aspiration, injection and drainage of ethanol solution was inserted into the cysts. After aspiration of cystic fluid, 1 ml/kg of dehydrated 95 % ethanol was injected into the cystic cavity. The patients in both groups were held in supine, prone and lateral decubitus positions for 5 min each to increase the contact between the surface of the cyst and the sclerosing agent. Afterward, the ethanol was aspirated and the polidocanol was left in the cyst. In group 1, patients were observed in outpatient setting until the first urination with clear urine, whereas in group 2, patients were hospitalized for a day and pig-tail catheter was removed before being discharged. In the follow-up period, all patients were evaluated at 3rd month, 12th month and annually afterward.
These data were documented from the electronic records of the patients. The sclerosing agent used in the procedures was chosen according to the surgeon’s preferences. The pre-operative and postoperative US findings were documented to compare the cyst recurrence and the reduction in cyst size. Success was defined clinically and anatomically as complete or partial. More than 90 % reduction in cyst size was accepted as complete, whereas 50–90 % reduction was accepted as partial. Failure was defined as <50 % reduction in cyst size. Intraoperative pain was assessed using a visual analog scale (VAS) just after the operation where 0 point represents no pain, 5 points represents moderate pain and 10 points represents unbearable pain. The data recorded at the last control of the patients were presented in this study.
Statistical analysis
The statistical software package SPSS 20.0 version (SPSS Inc, Chicago, IL, USA) was employed for data management and analysis. Chi-square test and Fisher’s exact test were performed. Significance was set at p ≤ 0.05.
Results
Mean age was 67.2 (range 42–82) years in group 1 and 66 (range 39–83) years in group 2. The median follow-up period was 36 months (range 12–76) in group 1 and 39 months (range 10–78) in group 2. Patients’ characteristics and the locations of the cysts are summarized in Table 1. Pre-interventional symptoms and post-interventional clinical improvement rates are given in Table 2. The cytological examination was negative for neoplastic cells in all patients, and biochemical analysis was similar to the plasma. The success rates of polidocanol and ethanol groups are given in Table 3. The overall success rate of ethanol sclerotherapy was significantly higher than that of polidocanol sclerotherapy (p < 0.001). The success rates of these two groups according to the cyst localization and size are shown in Table 2. Major complication was detected in only one patient of group 2 (aseptic psoas abscess), and there was not any major complication in group 1. Minor complications had occurred in ten patients in group 2 (microscopic hematuria in six patients and fever and nausea in four patients) and in eight patients in group 1 (microscopic hematuria in six patients and fever and nausea in two patients). Although complication rates were higher in ethanol group, it was not significant (p = 0.085). The mean VAS scores were 2.1 ± 1.04 and 4.26 ± 1.99 in ethanol and polidocanol groups, respectively (p < 0.001). Ethanol was found to be significantly painful, compared to polidocanol in the sclerotherapy of simple renal cysts.
Discussion
Simple renal cyst is a common, benign disease with an incidence ranging from 10 to 30 % in adults [9]. Obstruction and ischemia of the distal convoluted tubule has been postulated as an etiology of renal cysts [10]. Most simple cysts are asymptomatic, and usually, regular follow-up is sufficient for management. A definitive treatment might be necessary when the symptoms such as pain, hematuria, hypertension, recurrent infection or obstructive uropathy had occurred [11]. Although various surgical and percutaneous methods could be used in treatment of renal cysts [12], surgical interventions are not preferred due to the risk of morbidity and mortality, especially in elderly patients [13]. The advantages of percutaneous drainage of simple renal cysts are as follows: minimal invasiveness, well tolerability, easy administration under US guidance and usually no necessity for hospitalization [14]. Due to all these reasons, this treatment modality remains always up to date. However, simple aspiration without sclerosing agents has high recurrence and low success rates [15]. Various sclerosing agents have been used to improve the efficacy of percutaneous drainage. Therefore, the combination of drainage and sclerotherapy reduces the rate of recurrence [6].
The sclerosing agents for percutaneous sclerotherapy are bismuth phosphate, minocycline, ethanolamine oleate, povidone iodine, ethanol and acetic acid [5–8]. They destroy the lining epithelium of the cyst and provoke local inflammation on the luminal surface of the cyst, leading to the adhesion of the walls [16]. Bean et al. [17] described the treatment of renal cysts with 95 % alcohol during diagnostic aspiration. He also exposed specimens of renal cysts to alcohol and discovered that epithelial lining cells were fixed and nonviable within 1–3 min. Most of the studies were carried out with ethanol injection, and it was found to be more effective than only percutaneous drainage in renal cysts [11, 16–18]. However, with the leakage of phenol or ethanol into the surrounding tissue, the minor complications such as local tissue corrosion, fever, nausea, pain and microscopic hematuria and the major complications such as aseptic psoas abscesses and severe central nervous system depression are possible [15, 16]. Because of these complications, insertion of a pig-tail catheter into the cyst and ethanol aspiration from the renal cyst after instillation were recommended, but this is controversial [6]. In the ethanol sclerotherapy, insertion of a pig-tail catheter and leaving it on the patient for one night may also cause a leakage to the retroperitoneum, especially in peripherally located cysts. We have chosen to use a pig-tail catheter for ethanol drainage to enhance the effect of ethanol. The patients in our study reported a severe pain during the instillation of ethanol solution with a mean score of 5.1 ± 2 assessed by VAS. We had to stop ethanol instillation in three patients because of unbearable pain (VAS score = 10), and lidocaine was injected through the pig-tail catheter.
Polidocanol is a sclerosing agent, which has been used for the treatment of varicose veins, venous malformations, lymphoceles and renal cysts [8, 19, 20]. Polidocanol consists of 95 % hydroxypolyethoxydodecane and 5 % ethyl alcohol as a preservative. It possesses a detergent action that produces a rapid overhydration of the cells, with consequent destruction. Small volume of substance is enough for its sclerosing effect, so its use is easier than using ethanol. Because of its well-known safety profile from the venous applications, it is used without aspiration and left in the cystic cavity to destroy the lining epithelium. This is the most important advantage of polidocanol sclerotherapy as it can be used as an outpatient procedure because there is no need for using a pig-tail catheter for drainage. Also in contrast to the ethanol sclerotherapy, this procedure has some more advantages such as painless application, no need for intracystic anesthesia or sedation for the patient.
In this study, we categorized the cysts into three groups according to their location. When we compared the success rates of percutaneous sclerotherapy according to the location, we found that the success rates of ethanol were significantly higher than those of polidocanol in all locations. It seems that ethanol is a more effective sclerosing agent than polidocanol. There are also some more reasons that may affect the outcomes. A pig-tail catheter was used for aspiration of cystic fluid in ethanol group, and the soft pig-tail catheter was better for aspirating all of the cystic fluid instead of a rigid 18-G needle used in polidocanol group. In clinical practice, it is not very easy to approach the cysts in upper pole and perihilar region, especially in patients who cannot hold their breath, so in some cases it was not possible to aspirate all of the cystic fluid with a rigid needle. Probably residual cystic fluid may have diluted the polidocanol and decreased the sclerosing effect. Also in ethanol group, the pig-tail catheter was left in the cystic cavity for 24 h and local irritation of the catheter on the luminal surface of the cyst may lead to adhesion.
In our clinic experience, we recognized that the percutaneous sclerotherapy in upper pole cysts is not as effective as in middle zone and lower poles. We did not statistically analyze the cysts according to their sizes and locations because of the limited numbers, but there was a downward trend in success rates with size and location. The least success was achieved in cysts >10 cm in upper pole. This can be explained by difficulty in approach, inadequate aspiration, mis-insertion of the pig-tail catheter and insufficient volume of sclerosing agent. Other treatment options such as laparoscopic cyst excision should be taken into consideration, especially in large cysts located in the upper pole.
In our study, all of the cysts were symptomatic, and after the intervention, most of the patients’ symptoms were improved. Type of the sclerosing agent did not influence the improvement in symptoms. Both of the agents provided clinical success. Because of increasing morbidity and mortality in elderly patients for surgical intervention, ethanol sclerotherapy could be a more viable option than polidocanol sclerotherapy. However, it should be taken into consideration that ethanol sclerotherapy can cause severe pain and urologists need to be very careful in patients with heart failure and/or arrhythmia. The polidocanol sclerotherapy is almost without complications, but its effectiveness is not at desired levels. We think that more studies with incrementally larger volumes of the polidocanol will likely be needed to reach levels of success comparable to alcohol.
Our study has some limitations. This is a single-center and a retrospective study. As this is a retrospective and non-randomized study, the selection of sclerosing agent depends on surgeon’s preference. Further prospective and randomized studies are necessary to support the findings of the current study.
Conclusions
Percutaneous ethanol and polidocanol sclerotherapy in the management of simple renal cysts are minimal invasive, effective interventions with minimal complications. Both of the agents provide anatomical and clinical success. Although percutaneous ethanol sclerotherapy is very painful in some patients, this complication is rare and it provides significantly more anatomical success than polidocanol. More studies are needed to find the standard dosage of polidocanol for successful treatment. Other treatment options such as laparoscopic cyst excision should be considered, especially in large cysts located in the upper pole.
References
Mohsen T, Gomha MA (2005) Treatment of symptomatic simple renal cysts by percutaneous aspiration and ethanol sclerotherapy. BJU Int 96:1369–1372
Martino P, Palazzo S, Crudele V et al (2010) Echo-guided treatment of simple renal cysts: our experience from 1995 to 2010. Arch Ital Urol Androl 82:284–286
Okeke AA, Mitchelmore AE, Keeley FX et al (2003) A comparison of aspiration and sclerotherapy with laparoscopic de-roofing in the management of symptomatic simple renal cysts. BJU Int 92:610–613
Delakas D, Karyotis I, Loumbakis P et al (2001) Long-term results after percutaneous minimally invasive procedure treatment of symptomatic simple renal cysts. Int Urol Nephrol 32:321–326
Seo TS, Oh JH, Yoon Y et al (2000) Acetic acid as a sclerosing agent for renal cysts: comparison with ethanol in follow-up results. Cardiovasc Interv Radiol 23:177–181
Hanna RM, Dahniya MH (1996) Aspiration and sclerotherapy of symptomatic simple renal cysts: value of two injections of a sclerosing agents. AJR Am J Roentgenol 167:781–783
Phelan M, Zajko A, Hrebinko RL (1999) Preliminary results of percutaneous treatment of renal cysts with povidone-iodine sclerosis. Urology 53:816–817
Jain R, Bandhu S, Sawhney S et al (2002) Sonographically guided percutaneous sclerosis using 1 % polidocanol in the treatment of vascular malformations. J Clin Ultrasound 30:416–423
Terada N, Ichioka K, Matsuta Y et al (2002) The natural history of simple renal cysts. J Urol 67(21–3):15
Cho DS, Ahn HS, Kim SI et al (2008) Sclerotherapy of renal cysts using acetic acid: a comparison with ethanol sclerotherapy. Br J Radiol 81:946–949
El-Diasty TA, Shokeir AA, Tawfeek HA et al (1995) Ethanol sclerotherapy for symptomatic simple renal cysts. J Endourol 9:273–276
Busato WF Jr, Bettega LB (2010) Percutaneous endocystolysis, a safe and minimally invasive treatment for renal cysts: a 13-year experience. J Endourol 24:1405–1410
Kropp KA, Grayhack JT, Wendel RM et al (1967) Morbidity and mortality of renal exploration for cyst. Surg Gynecol Obstet 125:803–806
Aribas BK, Dingil G, Doğan K et al (2009) Single-session percutaneous sclerotherapy in symptomatic simple renal cysts: long-term results. Minerva Urol Nefrol 61:129–136
Martino P, Annunziata G, Saracino GA (2002) Aspiration versus aspiration plus ultrasonography-guided alcohol administration for simple renal cysts: recurrence and complications. Arch Ital Urol Androl 74:216–218
Brown B, Sharifi R, Lee M (1995) Ethanolamine sclerotherapy of a renal cyst. J Urol 153:385–386
Bean WJ (1981) Renal cysts: treatment with alcohol. Radiology 138:329–331
Falci-Junior R, Lucon AM, Cerri LM et al (2005) Treatment of simple renal cysts with single-session percutaneous ethanol sclerotherapy without drainage of the sclerosing agent. J Endourol 19:834–838
Trombetta C, Salisci E, Deriu M et al (1994) Role of echography in the diagnostic-therapeutic management of renal cysts. Arch Ital Urol Androl 66:145–150
Brunken C, Pfeiffer D, Tauber R (2002) Long term outcome after percutaneous sclerotherapy of renal cysts with polidocanol. Urol A 41:263–266
Conflict of interest
None.
Ethical standard
The study was approved by the local ethics committee. All the patients gave their informed consent prior to inclusion in the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yonguc, T., Sen, V., Aydogdu, O. et al. The comparison of percutaneous ethanol and polidocanol sclerotherapy in the management of simple renal cysts. Int Urol Nephrol 47, 603–607 (2015). https://doi.org/10.1007/s11255-015-0953-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-015-0953-9