Abstract
Objective
Seminal vesicle cysts are a rare disorder of the male reproductive system. The goal of this report was to summarize the radiological manifestations and transurethral endoscopic treatment of large seminal vesicle cysts.
Materials and methods
The clinical data of seven cases of giant seminal vesicle cysts, including their symptoms, radiological images, transurethral endoscopic treatment, and postoperative follow-up, were retrospectively reviewed.
Results
Computerized tomography and magnetic resonance imaging (MRI) demonstrated the cysts behind the bladder, above the prostate, and away from the midline. The lesions ranged in size from 8.26 cm × 7.98 cm × 4.85 cm to 9.27 cm × 8.95 cm × 8.15 cm. Two cases were associated with ipsilateral renal and ureteral agenesis and were classified as congenital malformations. The other five cases were simple seminal vesicle cysts thought to be secondary to acquired ejaculatory duct obstruction. All seven cases were successfully treated using transurethral endoscopic unroofing with cautery of the mucosa. All the seminal vesicle cysts were confirmed by pathologic examination. No malignant disease was found. All preoperative symptoms resolved after surgery. No complications were observed. No patient developed abnormalities of erection, ejaculation, or orgasm. No bladder or rectal injuries were noted. The seminal vesicle cysts were significantly decreased in size or absent 3–6 months after treatment.
Conclusion
MRI best characterized seminal vesical cysts and their cause. Transurethral unroofing with cautery of the mucosa is an extension of well-accepted cystoscopic techniques. It is safe, easy to perform, and effective. It is the preferred method for the treatment of large seminal vesicle cysts.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Seminal vesicle cysts are a rare male reproductive disease, with a prevalence of about 0.005 % in men [1]. Giant seminal vesicle cysts are much less common. Symptoms associated with seminal vesicle cysts include hematospermia, terminal hematuria, lower abdomen and lumbosacral pain, and perineal and testicular discomfort. Larger cysts are associated with symptoms related to visceral compression, including difficulty with urination and defecation, and hydronephrosis. We report the clinical findings and treatment of seven patients with giant seminal vesicle cysts treated at our hospital from January 2009 to May 2014.
Materials and methods
Clinical information
The Ethical Commission of Daping Hospital approved the study protocol. All procedures in this study followed the WMA Declaration of Helsinki related to the ethical principles for medical research involving human subjects. Seven cases of giant seminal vesicle cysts were retrospectively evaluated. Patients were 23–69 years old (average age 48 years). Five patients were married and two were not. Clinical manifestations included lower abdominal or anal discomfort (n = 6), dysuria (n = 4), difficulty with defecation (n = 2), pain at the end of micturition (n = 2), and, in one patient, hematuria and hematospermia. Digital rectal examination (DRE) revealed all patients had obvious cystic enlargement in the area of prostate or superior to the prostate without tenderness. All patients underwent transrectal ultrasonography (TRUS). A pelvic cyst was identified in all patients. Further imaging included computerized tomography (CT) or magnetic resonance imaging (MRI). Imaging studies were compatible with the diagnosis of a giant seminal vesicle cyst in all patients.
Surgical treatment
All seven patients were successfully treated using transurethral endoscopic unroofing with cautery for hemostasis. The resectoscope (ACMI, USA) was inserted through the urethra, into the bladder. The bladder was examined and then the bladder neck, prostatic urethra, and verumontanum area were evaluated. No hyperemia, bleeding, vascular malformations, varices, or neoplasms were observed. The bladder neck and prostatic urethra area were deviated to one side with loss of normal symmetry in all patients. The openings of the contralateral ejaculatory ducts were seen to discharge white viscous seminal vesicle fluid during transrectal seminal vesicle massage. The opening of the affected side ejaculatory duct did not discharge any such fluid. These findings suggest the seminal vesicle cyst was associated with the ipsilateral ejaculatory duct and was obstructed. The resectoscope was used to resect a 1-cm-long and 1-cm-wide segment of tissue from the bladder neck to the verumontanum. The depth of resection was usually not more than 1 cm. The unroofed seminal vesicle cyst contained a large amount of gelatinous milky fluid or dark red to chocolate bloody fluid. Some patients had a large amount of coagulated blood filled in the seminal vesicle cyst. The seminal vesicle cyst was irrigated with saline until it become clear. A smooth, ruddy internal mucosa was visualized. One elderly patient contained a 4 cm × 3 cm mass in the cyst wall, adjacent to the posterior aspect of the prostate. The mass was resected and sent for pathologic examination. The other six patients did not contain a mass in the cyst. Cyst wall biopsy was performed in these patients. The cyst wall was then cauterized using a loop electrode. A 22-French catheter was placed without irrigation, and the procedure ended.
Results
Imaging features
One patient was imaged using CT alone, one using CT and MRI, and five using MRI alone. All imaging features were compatible with a cystic mass in the pelvis located posterior to the bladder and superior to the prostate. Three were located on the left side and four on the right. Two cases were associated with ipsilateral renal agenesis. Cysts were located where the seminal vesicle was normally positioned. A normal seminal vesicle was not observed on the affected side. The morphology and size of the contralateral seminal vesicle were normal, although they were compressed by the cyst.
Typical imaging findings
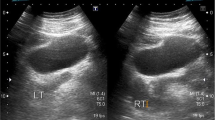
MRI showed a large cystic mass at the location of the left seminal vesicle (Fig. 1) just off the midline. The T1-weighted cross-sectional image showed a 9.3 cm × 8.9 cm × 8.2 cm cystic lesion with heterogeneous intermediate internal signal intensity. The T2-weighted cross-sectional imaging showed heterogeneous high signal intensity.
Typical case 1: pelvic MRI before (a, b) and after surgery (c, d). a T1-weighted imaging shows a large cystic mass (9.3 cm × 8.9 cm × 8.2 cm) in the left seminal vesicle area. The lesion had intermediate signal intensity (long arrow). The right seminal vesicle was normal in size and shape and had intermediate signal intensity (short arrow). b T2-weighted imaging shows the left seminal vesicle cystic lesion to have intermediate-to-high signal intensity (long arrow). The right seminal vesicle had high signal intensity (short arrow). The rectum was significantly compressed by the cyst. c T1-weighted imaging shows symmetrical seminal vesicles of normal size and homogeneous low signal intensity 3 months later after surgery. d T2-weighted imaging shows both seminal vesicles had high signal intensity with the normal coiled glandular structure
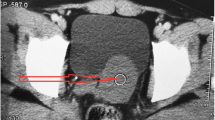
MRI and CT imaging showed a right seminal vesicle cyst accompanied with right renal agenesis (Fig. 2). The T1-weighted cross-sectional image demonstrated a 8.3 × 8.0 × 4.9 cm cyst in the right seminal vesicle region with homogeneous low-to-intermediate signal intensity. No normal right seminal vesical was seen. The T2-weighted imaging showed the cyst was of high signal intensity. The size and signal of left side seminal vesicle were normal in both T1- and T2-weighted images. CT imaging showed right renal agenesis.
Typical case 2: pelvic MRI and CT imaging before (a–c) and after surgery (d, e). a T1-weighted imaging shows a cyst with a thin irregular wall (8.3 × 8.0 × 4.9 cm). The lesion had intermediate signal intensity in the right seminal vesicle region with a smooth cystic wall and distinct boundary. The right side of the bladder was compressed by the cyst (long arrow). The left seminal vesicle was normal in size and shape and had low signal intensity (short arrow). b T2-weighted imaging shows a cystic lesion with homogeneous high signal intensity. No normal coiled glandular structure was seen (long arrow). The left seminal vesicle had normal high signal intensity with a coiled glandular structure (short arrow). c Coronal CT images shows a right seminal vesicle cyst and right renal agenesis. d T1-weighted imaging shows the right seminal vesicle cyst was significantly reduced in size from before surgery. The seminal vesicle was normal in size and had homogeneous low signal intensity (long arrow). e T2-weighted imaging shows the right seminal vesicle had high signal intensity (long arrow)
Treatment results
All the seven patients were successfully treated using transurethral endoscopic unroofing and electrocautery. The average operation time was 61 min (range 45–75 min). Average blood loss was 18 ml (range 10–30 ml). No complications were observed. Postoperative pathology confirmed the diagnosis of seminal vesicle cyst in all patients. No tuberculosis or tumor was identified. A Foley catheter was left indwelling for 1–3 days after surgery. Patients were followed up for 3–24 months (average 11 months). The preoperative symptoms resolved in all patients after unroofing. TRUS and MRI showed that all the originally large cysts were significantly reduced in size or absent (Figs. 1, 2) after surgery. No cyst recurrence was found during the period of follow-up. No operative complications such as urinary reflux, urinary incontinence, erectile dysfunction, ejaculation dysfunction, or lack of orgasm were found. Two young unmarried men had a semen analysis 3 months later after the operation, which was unchanged from their preoperative evaluation.
Discussion
Seminal vesicle cysts are a rare finding in the male reproductive system disease. Their detection rate has increased with modern imaging. Seminal vesicle cysts are usually benign and are classified as congenital or acquired lesions. Congenital seminal vesicle cysts are usually related to abnormalities of the mesonephric duct (Wolffian duct) [2]. Seminal vesicle cysts are frequently associated with other genitourinary malformations [3] including ipsilateral renal agenesis (Zinner syndrome), ectopic ureter, hypospadia, cryptorchidism, and hermaphroditism [4–7]. The frequency of presumed seminal vesicle cysts with ipsilateral renal agenesis or dysplasia was 0.0046 % in the renal sonographic screening of 280,000 children in Taipei [1]. Acquired seminal vesicle cysts are usually caused by ejaculatory duct obstruction related to reproductive system infection, posterior urethral inflammation, or ejaculatory duct stones. The size of seminal vesicle cysts in patients we examined ranged from 8.3 × 8.0 × 4.9 cm to 9.3 × 8.9 × 8.2 cm. Two patients we evaluated had seminal vesicle cysts with ipsilateral renal agenesis, which were classified as congenital seminal vesicle cysts. The remaining five patients had a single pelvic cystic lesion at the location of seminal vesicle without any other abnormality. These were classified as acquired seminal vesicle cysts.
Symptoms associated with early or small seminal vesicle cysts may be nonspecific [8]. The most common associated symptoms include hematospermia, terminal hematuria, and dull pain or discomfort in the lower abdomen, perineal, lumbosacral, or testicular area. Larger cysts can cause symptoms related to compression of adjacent viscera, including difficulty with urination and defecation and hydronephrosis. The diagnosis of seminal vesicle cyst should be considered if a male patient presents with the above symptoms or symptoms not explained by any other disease. Six patients we examined had chronic discomfort in the lower abdomen and perianal areas, four had dysuria, and two had difficulty with defecation. Digital rectal examination is important in screening for seminal vesicle cysts. The cystic mass has a smooth margin and is uniformly compressible. All the patients we examined with dysuria or difficulty with defecation were primarily diagnosed by digital rectal examination.
Imaging examinations used for the diagnosis of seminal vesicle cysts include TRUS, CT, and MRI. TRUS clearly images the area posterior to the bladder and distinguishes solid from cystic structures. It is simple to use, effective, and inexpensive, making it the preferred imaging modality. All our patients were examined with TRUS. The cystic mass was identified in all patients, but it looks like TRUS does not well locate cysts or their causes and further imaging was required to complete the diagnosis. CT and MRI can identify the size and nature of pelvic cysts and their relationship to the seminal vesicles [9]. Typical features of seminal vesicle cysts on CT are a thin-walled single cyst in the pelvis with a smooth cyst wall and distinct boundary. The cyst is generally located superior to the prostate gland, in the location of the seminal vesicles, off the midline. The internal signal intensity depends on the protein content of the cyst fluid. The cyst wall generally enhances, while the cyst fluid does not. MRI better characterizes the soft tissue nature of the lesion. MRI demonstrates the lesion size, cystic nature, the presence of blood in the cyst fluid, and obstruction of the ejaculatory duct or distal reproductive tract. Thus, MRI has better diagnostic accuracy than CT in the imaging of male reproductive tract diseases, which is confirmed by our previous reports [9, 10]. Five patients we evaluated were imaged using MRI. The seminal vesicle cysts were definitively diagnosed using MRI, as confirmed by transurethral surgery and pathologic examination of the tissue. Seminal vesicle cysts and Mullerian duct cysts can be differentiated with imaging. Seminal vesicle cysts are generally located off the midline and are associated with absence of the ipsilateral seminal vesicle. Mullerian duct cysts are usually located in the midline and cause posterior displacement of the normal seminal vesicle.
The management of seminal vesicle cysts depends on their size, clinical symptoms, and patient’s age. The goal of treatment is to relieve the clinical symptoms and preserve the normal function of the seminal vesicle. Conservative treatment is feasible with small seminal vesicle cysts or in patients without clinical symptoms or complications. Surgery is generally indicated for the treatment of large seminal vesicle cysts associated with significant symptoms. The location of the seminal vesicles in the deep pelvis, posterior to the prostate, makes open anterior surgical approaches difficult. Cystoscopic treatment is less invasive, provides good visualization, is quick to perform, and is associated with few complications. It is the preferred method for the treatment of seminal vesical cysts [11]. Gozen et al. [12] reported a case of seminal vesicle cyst with right renal agenesis in a young patient treated successfully with transurethral unroofing. The broad acceptance of transurethral endoscopic surgery [12–15] led us to treat our patients using transurethral unroofing of the cyst with cautery of the mucosa. This approach gives easy access to the cyst with little trauma or bleeding. It is associated with rapid recovery and few complications. None of our patients developed urinary reflux, urinary incontinence, infection, or retrograde ejaculation after surgery, and all the preoperative symptoms resolved. This report is limited by its small size due to the rarity of this lesion. This case series may be the largest published to date. Further studies are needed to validate the long-term effectiveness and safety of this transurethral technique.
Conclusion
Transurethral unroofing with cautery of the mucosa is an extension of well-accepted cystoscopic techniques. It is safe, easy to perform, and effective. It is the preferred method for the treatment of seminal vesicle cysts.
References
Sheih CP, Hung CS, Wei CF et al (1990) Cystic dilatations within the pelvis in patients with ipsilateral renal agenesis or dysplasia. J Urol 144(2 Pt 1):324–327
Patel B, Gujral S, Jefferson K et al (2002) Seminal vesicle cysts and associated anomalies. BJU Int 90:265–271
Giglio M, Medica M, Germinale F et al (2002) Renal dysplasia associated with ureteral ectopia and ipsilateral seminal vesical cyst. Int J Urol 9(1):63–66
Ahallal Y, Tazi MF, Khallouk A et al (2011) Conservative management of a congenital seminal vesicle cyst associated with ipsilateral renal agenesis revealed by cystitis: one case report. Case Rep Urol 2011:125753
Cherullo EE, Meraney AM, Bernstein LH et al (2002) Laparoscopic management of congenital seminal vesicle cysts associated with ipsilateral renal agenesis. J Urol 167:1263–1267
Selli C, Cavalleri S, De Maria M et al (2008) Robot-assisted removal of a large seminal vesicle cyst with ipsilateral renal agenesis associated with an ectopic ureter and a Mullerian cyst of the vas deferens. Urology 71:1226
Jang KD, Choi KH, Yang SC et al (2011) Laparoendoscopic single-site surgery (LESS) for excision of a seminal vesicle cyst associated with ipsilateral renal agenesis. Korean J Urol 52(6):431–433
Razi A, Imani B (2000) Seminal vesicle cyst presenting with lower urinary tract symptoms and huge abdominal mass. J Urol 164(4):1309–1310
Bj Li, Zhang C, Li K et al (2013) Clinical analysis of the characterization of magnetic resonance imaging in 102 cases of refractory haematospermia. J Androl 1(6):948–956
Li YF, Liang PH, Sun ZY et al (2012) Imaging diagnosis, transurethral endoscopic observation and management for 43 cases of severe and refractory hematospermia. J Androl 33(5):906–916
Jarzemski P, Listopadzki S, Kowalski M (2014) Laparoscopic removal of a congenital seminal vesicle cyst in Zinner’s syndrome. JSLS 18(2):367–371
Gozen AS, Alagol B (2006) Endoscopic management of seminal-vesical cyst with right renal agenesis causing acute urinary retention: case report. J Endourol 20(11):919–922
Gonzalez CM, Dalton DP (1998) Endoscopic incision of a seminal vesicle cyst. Urology 51:831–832
Okoye BO, Jones BO, Lancashire MJ et al (1995) Transvesical endoscopic drainage of a seminal vesicle cyst. Br J Urol 76:810
Razvi HA, Denstedt JD (1994) Endourologic management of seminal vesicle cyst. J Endourol 8:429
Acknowledgments
This study was supported by the Project of Prenatal and Postnatal Care Center of PLA in Daping Hospital (505-1539).
Conflict of interest
All authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Ming-Song Wang and Bo-Jun Li have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Wang, MS., Li, BJ., Huang, ZM. et al. Transurethral endoscopic treatment of seminal vesicle cysts (report of seven cases). Int Urol Nephrol 47, 717–721 (2015). https://doi.org/10.1007/s11255-015-0944-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-015-0944-x