Abstract
Patients with severe aortic stenosis (AS) after replacement of the transcatheter aortic valve (TAVR) are more likely to develop thrombotic complications such as cerebral embolism and artificial valve thrombosis. However, the mechanism is not yet well defined. We aimed to explore the plasma extracellular vesicles (EVs) levels and their role in the induction of procoagulant activity (PCA) in patients receiving TAVR alone or TAVR with percutaneous coronary intervention (PCI). EVs were analyzed with flow cytometer. Markers of platelet and endothelial cell activation were quantified using selective enzyme-linked immunosorbent assay (ELISA) kits. Procoagulant activity (PCA) was assessed by clotting time, purified clotting complex assays, and fibrin production assays. Our results confirmed that EVs with positive phosphatedylserin (PS+EV), platelet EVs (PEVs) and positive tissue factor EVs (TF+EVs) were higher in patients following TAVR than before TAVR, particularly in TAVR with PCI. Furthermore, endothelial-derived EVs (EEVs) were also higher in patients after TAVR with PCI than pre-TAVR, however, the EEVs levels in TAVR alone patients were gradually reduce than pre-TAVR. In addition, we further proved that total EVs contributed to dramatically shortened coagulation time, increased intrinsic/extrinsic factor Xa and thrombin generation in patients after TAVR, especially in TAVR with PCI. The PCA was markedly attenuated by approximately 80% with lactucin. Our study reveals a previously unrecognized link between plasma EV levels and hypercoagulability in patients after TAVR, especially TAVR with PCI. Blockade of PS+EVs may improve the hypercoagulable state and prognosis of patients.
Highlights
-
Patients after TAVR, especially TAVR with PCI, suffer from increased thrombotic complications, which seriously affect the prognosis of the patients.
-
Total EVs levels tend to increase after TAVR, especially TAVR with PCI, in 6 months, which positive correlation with the hypercoagulable state, and may lead to thrombosis.
-
EVs play the procoagulant role in patients after TAVR, especially TAVR with PCI.
-
Blockade of PS-positive EVs (PS+EVs) may improve the hypercoagulable state and reduce thrombotic complications in patients after TAVR.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Transcatheter aortic valve replacement (TAVR) is a less invasive alternative to traditional surgical aortic valve replacement (SAVR), with equivalent or superior outcomes, which is more suitable for some elderly patients and comprises 12.5% of all aortic valve replacements now [1,2,3]. The risk of thrombosis is a major concern and a major determinant of the prognosis and quality of life post TAVR [4,5,6]. There is a body of supporting evidence that patients after TAVR should receive thromboprophylaxis. Previous studies have shown that anticoagulant therapy, aspirin alone and aspirin plus clopidogrel only have differences in the risk of postoperative bleeding, and there is no significant difference in thromboembolic events [7, 8]. The optimal anti-thrombotic regimen is uncertain because the specific mechanism of the formation of the hypercoagulable state after TAVR has not yet been well defined, thus further research on the mechanisms of prothrombotic state after TAVR is still urgently needed.
Extracellular vesicles (EVs) are fragments released from stimulated or apoptotic cells after plasma membrane remodeling, which have been proposed to play a role in thrombosis in patients with some cardiovascular diseases [9, 10]. The presence of phosphatidylserine (PS) and tissue factor (TF) greatly increases the procoagulant activity of EVs [10, 11]. PS+EVs can facilitate the assembly of components of the clotting cascade by providing a membrane surface for the assembly of components of the coagulation protease cascade [12]. The presence of TF on EVs prominently increases their procoagulant activity because TF is a receptor for factor VII/ factor VIIa (FVII/VIIa) [10].
John D. Carroll et al. demonstrated a 94% increase in the number of patients receiving TAVR over the 7-year period between 2012 and 2019, which has become the dominant mode of intervention [13]. Although TAVR has been widely promoted all over the world, there are few studies on the changes in circulating EVs in patients after TAVR, and the procoagulant activity of EVs has not been extensively studied in these patients. Christian Jung et al. found that PEVs tended to increase and EEVs tended to decline after TAVR alone [14]. However, no procoagulant or inhibition assays were conducted to determine if changes in EV levels contribute to prothrombotic status in patients after TAVR. Previous studies indicated that both platelet-derived EVs (PEVs) and endothelial-derived EVs (EEVs) levels were elevated gradually after percutaneous coronary intervention (PCI) alone [15, 16]. Nevertheless, the EV levels in patients undergoing TAVR with PCI have not been extensively studied as well.
In this study, we analyzed the changes of different EVs, including total PS+EVs, PEVs, EEVs, and TF+EVs, as well as blood hypercoagulability indexes at 1 day, 7 days, 1 month, 3 months, and 6 months after TAVR alone or TAVR with PCI. Furthermore, we conducted coagulation function assays and inhibition assays to investigate the effect of EVs on coagulation activity in patients after TAVR alone or TAVR with PCI. Our study may help identify novel targets for thrombotic complications intervention and reduce mortality in patients after TAVR.
Methods
Subjects
In this study, patients diagnosed with severe AS by thoracic echocardiography (TTE) and undergoing TAVR were continuous selection for the study from the heart center of Qingdao Municipal Hospital from December 2019 to March 2021. A total of 68 patients met the inclusion criteria and exclusion criteria, including 53 cases receiving TAVR alone and 15 cases receiving TAVR and PCI in the same time. Thirty healthy volunteers were recruited from among the hospital staff as healthy controls in the same time. The diagnostic criteria for severe AS were: peak aortic valve velocity > 4.0 m/s or mean differential pressure > 40mmHg or continuity equation valve area < 1.0 cm2 or valve area index < 0.6 cm2 by chest echocardiography [17]. All the patients were implanted with the self-expandable Venus A-valve of transcatheter artificial valve produced by Hangzhou Qiming Medical Device Co., Ltd of China through transfemoral approaches, and underwent intravenous anesthesia. This study was conducted according to the Declaration of Helsinki and approved by the Ethics Committee of Qingdao Municipal Hospital, which was shown in Appendix S1. All patients signed the informed consent form. Exclusion criteria for all patients were: malignant tumors, infectious diseases, aortic dissection, and aortic aneurysm, known contraindications to radial or brachial artery puncture, unable to tolerate TAVR surgery for any reason, the lack of data due to death or other causes during follow-up.
All patients received aspirin (300 mg loading dose and 100 mg daily) and clopidogrel (300 mg loading dose and 75 mg daily) plus standard heparin to maintain an activated clotting time of > 300 s.
Materials
We used TruCount Tube, purified CD31 (clone L133.1), CD41a (clone HIP8), and CD142 (clone HTF-1) from Becton Dickinson (San Jose, CA, USA). All monoclonal antibodies were labeled with Alexa Fluro 647 or 488 in our laboratory. Polyclonal antibody against human Tissue Factor was from American Diagnostica Inc. (Stamford, CT, USA). We prepared Alexa Fluro 647 or 488 conjugated lactadherin in our laboratory. Human factors Va, VIIa, VIII, IXa, X, Xa, prothrombin, and thrombin were all from Haematologic Technologies. Tyrode’s buffer, containing 1 mM HEPES, was prepared in our laboratory and filtered through a 0.22-mm syringe filter from EMD Millipore. Chromogenic substrates S-2765 and S-2238 were from DiaPharma Group. Calibrated polystyrene latex beads (1.0 μm) were from Sigma (UK).
Protein purification and labeling
We labeled lactadherin, purified from milk, with Alexa fluor 647 or Alexa fluor 488. The proportion of fluorescein to lactadherin was 1.1–1.2/1 [18].
Collection of blood and analysis of blood hypercoagulability indexes and blood cell activation markers
Blood samples were collected from TAVR patients and TAVR with PCI patients at different time points: before TAVR, 1 day, 7 days, 1 month, 3 months, and 6 months after AS treatment. Blood hypercoagulability index and blood cell activation markers were quantified immediately using selective ELISA kits (NeoBioscience Technology, China) based on provided instructions after the collection of blood samples.
Preparation and flow cytometric analysis of EVs
Within 30 min after blood collection, samples were centrifuged for 20 min at 1500 g, and plasma was aspirated and recentrifuged for 30 min at 20,000 g. After centrifugation, we removed the EV-depleted plasma (EDP) supernatant, collected and stored the remaining EVs at the bottom of the tube at − 80°C. PS+EVs, PEVs, EEVs and TF+EVs were characterized as lactadherin+, lactadherin+CD41a+, lactadherin+CD31+41a- and lactadherin+CD142+. We used a trucount tube to calculate the number of MP of each type per microliter after accumulation of 10,000 gated events with the following formula: n = (C × Beadsadded) / (Beadscounted × sample volume). The ‘C’ in the formula represents the number of positive events after subtracting the background signal.
Coagulation time and inhibition assays of EVs
We used a KC4A-coagulometer to evaluate the PCA of EVs. To get EV-containing suspension, we mix EV-enriched suspension and Tyrode’s buffer in a ratio of 1:9. We incubated one hundred microliters of EV-containing suspension with100 µl of EV-depleted plasma at 37 °C for 3 min. Then we added 100 µl of warmed CaCl2 (25 mM) to start the reaction and record the coagulation time. In the inhibition assay, 100 µl of EVs suspension was incubated with 50 µl of lactadherin or anti-TF for 10 min at 37 °C. Record the coagulation time after the addition of 100 µl EV-free human plasma and 50 µl of warmed CaCl2 (50 mM).
Intrinsic, extrinsic FXa and thrombin formation and inhibition assays of EVs
Factor Xase and prothrombinase activity assays were performed on all samples. Inhibition assays were performed at the peak time point. For intrinsic XA formation, we incubated 10 µ L EVs suspension with fixa (1 nm), FX (130 nm), FVIII (5 nm), thrombin (0.2 nm), and CaCl2 (5 mm) in FXa buffer (10 ml 1 × Incubate in TBS containing 0.2% BSA) at 25 ° C for 5 min. EDTA (7 mm final concentration) was used to stop the reaction. The generation of FXa was measured with a Universal Microplate Spectrophotometer (PowerWave XS; Bio-Tek, Winooski, VT, USA) set in kinetic mode at 405 nm after incubation with 10 µl of S-2765 (0.8 mM). The formation of extrinsic FXa was similar to that of intrinsic FXa except that EVs were cultured with FX (130 nM), FVIIa (1 nM), and CaCl2 (5 nM). For the prothrombinase assay, we incubated EVs with FVa (1 nM), 0.05 nM FXa (0.05 nM), prothrombin (1 µM), and CaCl2 (5 nM) in prothrombinase buffer (10 ml 1 × TBS with 0.05% BSA) for 5 min at 25 °C and then stopped the reaction using EDTA. We used the chromogenic substrate S-2238 to measure the amount of thrombin production by the standard dilution curve of thrombin as the substrate cleavage rate. For inhibition assays, EVs were pre-incubated with lactadherin (128 nM) or anti-TF at their peak time point for 10 min at 25 °C in Tyrode’s buffer and then we incubated the mixture with the specified clotting factors as previously described. The formation of FXa or thrombin was appraised according to the method as above.
Fibrin formation assays
Turbidity was used to assess fibrin formation. We added EVs to recalcified (10 mM, final) EV-depleted plasma (88% EV-depleted plasma, final) in the absence or presence of lactadherin/anti-TF. We measured Fibrin production by turbidity at 405 nm using a SpectraMax 340PC plate reader.
Statistical analysis
Statistical analysis was performed using the SPSS v16.0 software or GraphPad Prism 7.0. Values were presented as mean ± standard deviation (SD) and were based on at least triplicate measurements. Student’s t-test or one way ANOVA was used for statistical analysis as appropriate. Spearman’s rank correlation analysis was used to determine the correlation between continuous variables. Multiple linear regression was used to analyse the influence of confounding factors. P < 0.05 was considered statistically significant.
Results
Subject characteristics
Clinical characteristics in 30 healthy controls and patients who underwent TAVR alone and TAVR with PCI are shown in Table 1. There were no significant differences in the means of gender, smoking, alcohol, body mass index (BMI) and the levels of HDL-C between healthy controls and patients after TAVR alone or TAVR with PCI. Concerning characteristic findings, the levels of neutrophils, leukocytes, platelets, D-dimer, fibrinogen, thrombin-antithrombine (TAT), creatinine (Cr), brain natriuretic peptide (BNP), triglyceride (TG), total cholesterol (TC) and low-density lipoprotein cholesterol (LDL-C) in TAVR alone or TAVR with PCI patients were prominently higher than that in healthy controls. TAVR alone and TAVR with PCI patients did not differ with regard to age, gender, smoking, alcohol, BMI, NYHA stage, atrial fibrillation, D-dimer, fibrinogen, TAT, Cr, BNP, blood fat, AVA and valve size. However, the proportion of diabetes mellitus, hypertension, and stroke, as well as the levels of neutrophils and platelets in TAVR with PCI patients were prominently higher than that in TAVR alone patients. On the contrary, the levels of leukocytes and BNP in TAVR alone patients were higher than that in TAVR with PCI patients.
Dynamics of PS+EVs/EEVs/PEVs/TF+EVs in patients undergoing TAVR alone or TAVR with PCI
Flow cytometry was used to evaluate the total number of EVs and their phenotypic characteristics. As shown in Fig. 1, compared with healthy controls, the circulating EVs levels were significantly elevated in other two groups (all P < 0.05; Fig. 1A-D), but there was no significant difference in circulating EVs levels between TAVR alone patients and TAVR with PCI patients before interventional therapy (all P > 0.05; Fig. 1A-D). When compared to pre-TAVR, the levels of total PS+EVs, PEVs, and TF+EVs in TAVR alone and TAVR with PCI groups were significantly increased from 7 days to 6 months after TAVR, peaking at 3 months (all P < 0.001; Fig. 1A, B, D). Furthermore, compare with TAVR alone patients, total EVs, PEVs, and TF+EVs in TAVR with PCI patients were greater from 7 days to 6 months after TAVR at different time points. Among them, compare with pre-TAVR, EEVs and TF+EVs in TAVR with PCI patients increased earlier after TAVR than in the other groups, elevelevation started on the first postoperative day (P < 0.05; Fig. 1C, D). In addition, the levels of EEVs also started to have a remarkable increase from 7 days to 6 months, peaking at 1 month in TAVR with PCI patients (all P < 0.001; Fig. 1C). However, EEVs continuously decreased from 7 days to 6 months in TAVR alone patients (all P < 0.001; Fig. 1C).
Flow cytometry analyses of EVs in healthy controls (n = 30), TAVR alone patients (n = 53) and TAVR with PCI patients (n = 15) at pre-TAVR and 1 day/7 days/1 months/3 months/6 months after TAVR alone or TAVR with PCI. Events were selected for their lactadherin binding, determined by positivity for Alexa Fluor 488-lactadherin. PEVs (Alexa Fluro 647-CD41a+), EEVs (Alexa Fluro 488-CD31+/Alexa Fluor 647-CD41a−) and TF+EVs (Alexa Fluor 647-CD142+) were also measured and counted. PEVs: platelet-derived extracellular vesicles; EEVs: endothelial-derived extracellular vesicles; PS+EVs: phosphatidylserine-positive extracellular vesicles; TF+EVs: tissue factor-positive extracellular vesicles. &p<0.05 TAVR alone or TAVR with PCI vs. healthy controls. *p<0.01 vs. pre-TAVR. **p<0.001 vs. pre-TAVR. #p<0.01 TAVR with PCI vs. TAVR alone
Multiple linear regression on total PS+ EVs levels at 3 months after TAVR alone or TAVR with PCI
Total PS+EVs levels reached its peak at 3 months after interventional therapy (Fig. 1A), so we conducted multiple linear regression using total PS+EVs levels at 3 months after interventional therapy as the dependent variable and other factors that may affect EVs as the independent variable. As shown in Table 2, the effects of gender, age, diabetes mellitus, hypertension and atrial fibrillation on total PS+EVs levels were not statistically significant (P>0.05) and receiving TAVR alone or TAVR with PCI had effects on total PS+EVs levels, which means that, after adjusting for gender, age, diabetes mellitus, hypertension and atrial fibrillation by multivariate linear regression analysis, this association remained statistically significant (P < 0.05).
Changes in indicators of platelet and endothelial cell activation, and blood hypercoagulability following TAVR or TAVR with PCI
Platelet granule membrane protein-140 (GMP-140) is a specific molecular marker of platelet activation, participating in the pathophysiology of thrombosis [19]. PS is an anionic phospholipid, which is strictly located on the inner leaflet of the cell membrane and externalized to the outer surface during cell activation or apoptosis, so the ratio of PS+PLT to total PLT can also be used as an indicator of platelet activation. Our data showed that GMP-140 and the ratio of PS+PLT in healthy controls were lower than that in other two groups (all P < 0.05; Fig. 2A, B). Compared to pre-TAVR, GMP-140 and the ratio of PS+PLT in TAVR alone and TAVR with PCI groups were observed to increase prominently from 7 days (P < 0.01) to 6 months (P < 0.001), peaking at 3 months (all P < 0.01; Fig. 2A, B). Furthermore, GMP-140 and the ratio of PS+PLT in patients after TAVR with PCI were maintained at relatively higher levels than that in patients after TAVR alone (all P < 0.05; Fig. 2A, B). Soluble intracellular adhesion molecule-1 (sICAM-1) and soluble vascular cell adhesion molecule-1 (sVCAM-1) are specific molecular markers of endothelial cell activation. Compared with healthy controls, sVCAM-1 and sICAM-1 levels were significantly elevated in other groups (P < 0.05; Fig. 2C, D). In TAVR with PCI patients, sVCAM-1 and sICAM-1 had the same change as GMP-140 and PS+PLT from 7 days to 6 months after the operation. However, in TAVR alone patients, sVCAM-1 and sICAM-1 showed a steady decreasing trend from 7 days (P < 0.01) to 6 months (P < 0.001; Fig. 2C, D). Our results proved the activation of platelets and endothelial cells after interventional therapy except that patients receiving TAVR alone showed decreased endothelial cell activation, which was consistent with the PEVs and EEVs variation trend.
GMP-140 (A), sVCAM-1 (C), sICAM-1 (D), D-D (E), TAT (F) and the percent of PS+PLT (B) in blood samples from healthy controls (n = 30), TAVR alone patients (n = 53) and TAVR with PCI patients (n = 15) were measured at pre-TAVR and 1 day/7 days/1 months/3 months/6 months after TAVR alone or TAVR with PCI. GMP-140: platelet granular membrane protein 140. sVCAM-1: soluble vascular cell adhesion molecule-1. sICAM-1: soluble intercellular adhesion molecule-1. D-D: d-dimer. TAT: thrombin–antithrombin complex. &p<0.05 TAVR alone or TAVR with PCI vs. healthy controls. *p <0.01 vs. pre-TAVR. **p<0.001 vs. pre-TAVR. #p<0.01 TAVR alone vs. TAVR with PCI.
D-dimer (D-D) and TAT as indicators of blood hypercoagulability were also measured and tracked in our study. D-D and TAT levels in TAVR alone patients or TAVR with PCI patients were higher than healthy controls (P < 0.05; Fig. 2E, F). The levels of D-D and TAT in both groups had a significant increase from 7 days to 6 months after TAVR. Compared to TAVR alone patients, D-D and TAT levels in TAVR with PCI patients were higher at different time points after TAVR (Fig. 2E, F). The relationships between PS+EVs/PEVs/EEVs/TF+EVs and D-D/TAT were also been analyzed. In the TAVR alone and TAVR with PCI groups, D-D and TAT had a significant positive correlation with the levels of PS+EVs/PEVs/EEVs/TF+EVs (Table 3). These data suggest that, to some extent, changes in circulating EV levels could lead to blood hypercoagulability in patients after TAVR.
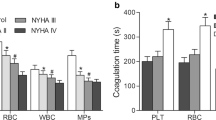
PCA of EVs following TAVR or TAVR with PCI
We used clotting time (CT), intrinsic/extrinsic factor Xa, thrombin, and fibrin formation assays to test the PCA of total EVs in healthy controls and patients after TAVR or TAVR with PCI. CT in two patients groups was longer than that in healthy controls and the production of all three procoagulant enzyme complexes and the turbidity of fibrin in two patients groups were less than that in healthy controls (P < 0.05; Fig. 3A-D). As shown in Fig. 3, CT was markedly shorter, while the production of all three procoagulant enzyme complexes and the turbidity of fibrin were increased in both groups (P < 0.001; Figs. 3A-D and 4A). Patients receiving TAVR with PCI showed higher procoagulant activity than patients receiving TAVR alone. Inhibition assays were performed using 3 months following TAVR alone and TAVR with PCI, which is the highest point of coagulation activity respectively. The addition of lactadherin prolonged the coagulation times, and reduced intrinsic/extrinsic factor Xa, thrombin, and fibrin formation (P < 0.001), whereas anti-tissue factor (anti-TF) had a negligible effect (Figs. 3E-H and 4B). Our results confirmed that the increase in total EVs levels made contributions to the high procoagulation activity after TAVR.
The PCA of EVs isolated from healthy controls (n = 30), TAVR alone patients (n = 53) and TAVR with PCI patients (n = 15) and inhibition assays. CT (A) was detected in the absence of lactadherin or anti-TF after aortic stenosis treatment. EVs was evaluated for the production of intrinsic Xa (B), extrinsic Xa (C) and thrombin (D). CT (E), intrinsic Xa (H), extrinsic Xa (F) and thrombin (G) were measured at 3 months with lactadherin/anti-TF disrupting the binding of procoagulant enzyme complexes to EVs. Lact: lactadherin. Anti-TF: anti-tissue factor. For A,B,C,D, &p<0.05 TAVR alone or TAVR with PCI vs. healthy controls. *p<0.01 vs. pre-TAVR. **p<0.001 vs. pre-TAVR. #p<0.01 TAVR alone vs. TAVR with PCI. For E,F,G,H, **p<0.001 3 months vs. 3 months + Lact/Anti-TF.
A Fibrin polymerization in samples from healthy controls (n = 30), TAVR alone patients (n = 53) and TAVR with PCI patients (n = 15) was monitored by measuring turbidity at 405 nm. B Comparison of fibrin polymerization between 3 months and 3 months + Lact/Anti-TF. Lact: lactadherin. Anti-TF: anti-tissue factor. For A, &p<0.05 TAVR alone or TAVR with PCI vs. healthy controls. *p<0.01 vs. pre-TAVR. **p<0.001 vs. pre-TAVR. #p<0.01 TAVR with PCI vs. TAVR alone. For B, **p<0.001 3 months + Lact/Anti-TF vs. 3 months
Discussion
In this study, we found that compared to pre-TAVR, EVs of patients remained at elevated levels from 7 days to 6 months after interventional therapy, especially TAVR with PCI, which had ruled out the influence of confounding factors. D-D and TAT levels also increased with increasing EVs, which were significantly associated with EVs levels. Furthermore, markers of platelet and endothelial cell activation showed the same trend as the EV levels within 6 months after TAVR or TAVR with PCI. Moreover, the intrinsic/extrinsic factor Xa, the formation of thrombin and fibrin experienced the same change as the EVs, while the coagulation time was the opposite. Additionally, PCA was effectively blocked after the inhibition assays with lactadherin. Taken together, we confirmed the hypercoagulable state after TAVR alone or TAVR with PCI, which can be partly attributed to the increase of EVs, and the patients undergoing TAVR with PCI had higher coagulation activity than patients undergoing TAVR alone.
The influence of EVs on PCA in patients after TAVR has started to draw people’s attention. Our results showed that PS+EVs, PEVs, and TF+EVs tended to increase while EEVs tended to decline after TAVR alone, however, in TAVR with PCI patients, PS+EVs, PEVs, TF+EVs, and EEVs all tended to increase after the operation from 7 days to 6 months. However, in the previous study did not observe an increase in EVs levels in a short follow-up of TAVR [19]. Furthermore, Christian Jung al. found that although PEVs tended to increase over time after TAVR procedure, which is generally consistent with our results, circulating EVs levels do decrease 3 months following TAVR [14]. These results are different from our findings. It may be one of the reasons for the discrepancy that we used lactadherin, a molecular probe different from previous studies, to measure EVs levels. As a probe for the detection of EVs, lactadherin is more effective and sensitive than annexin V [20]. Another reason may be that several follow-up windows in other researches are too short to detect changes in EVs levels post TAVR, because the acute injury of interventional operation, changes in hemodynamics, and shear stress after treatment may affect the production of EVs. Therefore, it takes enough time for the levels of EVs to change and reach a stable state [21, 22]. The follow-up window we choose in our research is long enough to observe a more dynamic evolution of the EV levels.
Moreover, we performed procoagulant or inhibition assays to authenticate that the increase of PS+EVs is responsible for high PCA after interventional therapy. Although TF can accelerate blood coagulation and TF+EVs were also observed to have the same changes as PS+EVs, in the inhibition assay, we found that the anti-TF antibody had a negative effect on the PCA of patients enrolled. In previous related studies, TF+EVs had not been found to play an important role in PCA, too [23, 24]. For this result, we take the possible reason into consideration that encrypted TF, with very little PCA, exposed to plasma primarily mostly decrypt through associating with PS [25, 26]. Thus, the simple addition of the anti-TF antibody does not have a significant effect on PCA in samples.
In the present study, we also found that there was a notable discrepancy in levels of EVs after treatment between the two groups. Although the preoperative EVs levels of the two groups were the same, the circulating levels of EVs in patients receiving TAVR and PCI were significantly higher than that in patients receiving TAVR alone after the operation from the 7 days. Koganti S et al. have found that the EVs levels of patients receiving PCI alone increased within 6 months, which, to some extent, was consistent with our conclusion [27, 28]. Our results corroborated the increase in EEVs levels after TAVR with PCI. Consistent with our results, Zhou BD al. also demonstrated that EEVs levels dramatically decreased immediately after PCI, and then increased gradually with time [15]. When interpreting the divergence of EEVs levels, it is maybe ascribed to the following reasons: (1) the procedure of PCI directly causes damage to vascular wall endothelial cells, resulting in increased release of EEVs; (2) EEVs have been reported to be a cause of fibrinolysis [29, 30] and after the reperfusion of the occluded coronary artery, plenty of EEVs enter the circulation promptly, so EEVs levels will rise to antagonize the increase of procoagulant PEVs.
It is well-known that, in vivo, levels of PEVs and EEVs are mainly regulated by shear stress and proinflammatory mediators [31,32,33,34,35,36]. Generally speaking, proinflammatory mediators can increase the release of PEVs and EEVs by promoting apoptosis and activation [31, 35, 36]. High shear stress can promote the release of PEVs [32,33,34], but there are some investigates observing the negative association between EEVs levels and arterial shear stress under pathological conditions, because high shear stress can limit EEVs release in nitric oxide (NO)-dependent regulation of ATP-binding cassette transporter A1 (ABCA1) expression and of cytoskeletal reorganization [31, 37, 38]. Thus, on the basis that TAVR can significantly reduce the shear stress on blood vessels [39], it is interesting that we observed the sustained and significant decrease in EEVs level in TAVR alone patients from 7 days to 6 months, and, consistent with our results, the previous study also provided evidence that TAVR alone procedure reduced the number of circulating EEVs [14]. This may indicate that proinflammatory mediators play a more important role in the formation of EEVs in AS patients than shear stress. Patients after TAVR received less direct stimulation to the vascular wall, which decreased circulating EMP levels. Although the relevant mechanism is not involved in this study, the effect of proinflammatory mediators on EEVs levels in AS patients receiving TAVR will be further explored in the next study.
Furthermore, we confirmed that the increase of EVs can raise the coagulation activity of patients receiving TAVR alone or TAVR with PCI, thereby increasing the risk of thrombosis. Consistent with our results, previous studies have shown that high levels of EVs can increase the risk of thrombosis in patients with coronary heart disease [40, 41]. Therefore, considering that the EVs levels of TAVR with PCI patients were higher than that of TAVR alone patients, the former has higher blood procoagulant activity and more attention should be paid to the antithrombotic therapy of them. Because the thrombotic complications of patients are mostly asymptomatic cerebral embolism and valve thrombosis, only a few patients were willing to undergo these diagnostic tests. Therefore, we were unable to fully collect relevant data. However, clinical stroke or transient ischemic attack, one-half of which being disabling strokes, is not rare after TAVR, ranging in the randomized studies from 5 to 6% at 1 month to 8–10% at 1 year [42]. Previous studies showed that the incidence of silent cerebral embolism is much higher than that of clinical stroke, almost occurring in 75% of the cases after TAVR, which leads to a high risk for cognitive deterioration [43, 44]. In addition, Ryo Yanagisawa al. found that the accumulated incidence of hypoattenuating leaflet thickening, possibly indicating artificial valve thrombosis, was 10.0% at 6 months [6, 45]. This is consistent with the increase in EVs levels in our study in terms of time. We believe that this can also prove, to some extent, that these changes in EVs and coagulations tests are clinically relevant. In future research, we will continue to collect data on postoperative thrombotic complications in patients to help us better explore the clinical relevance between the EVs levels and thrombotic complications.
Preventing these thrombotic complications is an important measure to improve the prognosis of patients. Nevertheless, antithrombotic therapy commonly used after TAVR at present, dual antiplatelet therapy for 1 to 6 months, is totally empirical [46]. Our data demonstrated that consistent with the occurrence time of cerebral embolism and artificial valve thrombosis, EVs levels, and PCA remained at a high level from 7 days to 6 months after the operation and peaked at 3 months. In the meantime, the PCA can be blocked with lactadherin effectively. This opens up a new idea for postoperative antithrombotic therapy. Perhaps, in addition to antiplatelet therapy, anticoagulant therapy and blockade of PS+EVs should also be applied in time after TAVR, especially TAVR with PCI, starting at 7 days at the latest.
Our study was a single-center and small sample size study. Therefore, from a statistical point of view, it is slightly underpowered for evaluating the clinical implication. Our follow-up was only half a year, and how EV levels change thereafter remains unclear. Simultaneously, we only investigated PS+EVs, EEVs, PEVs and TF+EVs, but other EVs from other sources in the blood that may increase PCA were not included in the research. Therefore, their impact on PCA after TAVR cannot be determined.
Conclusions
In conclusion, our data corroborated the existence of the hypercoagulable state in patients after TAVR and that there was an increase in EVs in TAVR alone patients and TAVR with PCI patients, which may lead to the hypercoagulable state. Moreover, patients after TAVR with PCI had higher EV levels and coagulation activity than patients after TAVR alone. In addition to antiplatelet therapy, anticoagulant therapy and blockade of PS+EVs have the possibility to improve the hypercoagulable state and prognosis of patients.
References
Hu PP (2012) TAVR and SAVR: current treatment of aortic stenosis. Clin Med Insights Cardiol 6:125–139
Yutzey KE, Demer LL, Body SC et al (2014) Calcific aortic valve disease: a consensus summary from the Alliance of investigators on calcific aortic valve disease. Arterioscler Thromb Vasc Biol 34:2387–2393
Cappabianca G, Ferrarese S, Musazzi A et al (2016) Predictive factors of long-term survival in the octogenarian undergoing surgical aortic valve replacement: 12-year single-centre follow-up. Heart Vessels 31:1798–1805
Mastoris I, Schoos MM, Dangas GD et al (2014) Stroke after transcatheter aortic valve replacement: incidence, risk factors, prognosis, and preventive strategies. Clin Cardiol 37:756–764
Auffret V, Regueiro A, Trigo MD et al (2016) Predictors of early cerebrovascular events in patients with aortic stenosis undergoing transcatheter aortic valve replacement. J Am Coll Cardiol 68:673–684
Yanagisawa R, Hayashida K, Yamada Y et al (2016) Incidence, predictors, and mid-term outcomes of possible leaflet thrombosis after TAVR. JACC Cardiovasc Imaging
Brouwer J, Nijenhuis VJ, Delewi R et al (2020) Aspirin with or without Clopidogrel after Transcatheter aortic-valve implantation. N Engl J Med 383:1447–1457
Nijenhuis VJ, Brouwer J, Delewi R et al (2020) Anticoagulation with or without Clopidogrel after Transcatheter aortic-valve implantation. N Engl J Med 382:1696–1707
Yeung T, Gilbert GE, Shi J et al (2008) Membrane phosphatidylserine regulates surface charge and protein localization. Science 319:210–213
Owens AP 3rd, Mackman N (2011) Microvesicles in hemostasis and thrombosis. Circ Res 108:1284–1297
Mackman N, Tilley RE, Key NS (2007) Role of the extrinsic pathway of blood coagulation in hemostasis and thrombosis. Arterioscler Thromb Vasc Biol 27:1687–1693
Perez-Pujol S, Marker PH, Key NS (2007) Platelet microvesicles are heterogeneous and highly dependent on the activation mechanism: studies using a new digital flow cytometer. Cytometry A 71:38–45
Carroll JD, Mack MJ, Vemulapalli S et al (2020) STS-ACC TVT Registry of Transcatheter aortic valve replacement. J Am Coll Cardiol 76:2492–2516
Jung C, Lichtenauer M, Figulla H-R et al (2017) Microvesicles in patients undergoing transcatheter aortic valve implantation (TAVI). Heart Vessels 32:458–466
Zhou B, Li J, Chen S et al (2016) Time course of various cell origin circulating microvesicles in ST-segment elevation myocardial infarction patients undergoing percutaneous transluminal coronary intervention. Exp Ther Med 11:1481–1486
Jung RG, Duchez A, Simard T et al (2022) Plasminogen activator inhibitor-1-Positive platelet-derived extracellular vesicles predicts MACE and the Proinflammatory SMC phenotype. JACC Basic Transl Sci 7:985–997
Joseph J, Naqvi SY, Giri J et al (2017) Aortic stenosis: pathophysiology, diagnosis, and Therapy. Am J Med 130:253–263
Shi J, Heegaard CW, Rasmussen JT et al (2004) Lactadherin binds selectively to membranes containing phosphatidyl-L-serine and increased curvature. Biochim Biophys Acta 1667:82–90
Marchini JF, Miyakawa AA, Tarasoutchi F et al (2016) Endothelial, platelet, and macrophage microparticle levels do not change acutely following transcatheter aortic valve replacement. J Negat Results Biomed 15:7
He Z, Si Y, Jiang T et al (2016) Phosphotidylserine exposure and neutrophil extracellular traps enhance procoagulant activity in patients with inflammatory bowel disease. Thromb Haemost 115:738–751
Horn P, Stern D, Veulemans V et al (2015) Improved endothelial function and decreased levels of endothelium-derived microvesicles after transcatheter aortic valve implantation. EuroIntervention 10:1456–1463
Petrov G, Regitz-Zagrosek V, Lehmkuhl E et al (2010) Regression of myocardial hypertrophy after aortic valve replacement: faster in women? Circulation 122:23–28
Li J, Tong D, Chen F et al (2021) Inflammatory cytokines enhance procoagulant activity of platelets and endothelial cells through phosphatidylserine exposure in patients with essential hypertension. J Thromb Thrombolysis 51:933–940
Atmaca HU, Akbas F, Aral H (2019) Relationship between circulating microvesicles and hypertension and other cardiac disease biomarkers in the elderly. BMC Cardiovasc Disord 19:164
Shaw AW, Pureza VS, Sligar SG et al (2007) The local phospholipid environment modulates the activation of blood clotting. J Biol Chem 282:6556–6563
Rao LVM, Kothari H, Pendurthi UR (2012) Tissue factor encryption and decryption: facts and controversies. Thromb Res 129:13–17
Koganti S, Eleftheriou D, Gurung R et al (2021) Persistent circulating platelet and endothelial derived microparticle signature may explain on-going pro-thrombogenicity after acute coronary syndrome. Thromb Res 206:60–65
Biasucci LM, Porto I, Di Vito L et al (2012) Differences in microparticle release in patients with acute coronary syndrome and stable angina. Circ J 76:2174–2182
Lacroix R, Dignat-George F (2012) Microvesicles as a circulating source of procoagulant and fibrinolytic activities in the circulation. Thromb Res 129:27–29
Lacroix R, Plawinski L, Robert S et al (2012) Leukocyte- and endothelial-derived microvesicles: a circulating source for fibrinolysis. Haematologica 97:1864–1872
Vion AC, Ramkhelawon B, Loyer X et al (2013) Shear stress regulates endothelial microparticle release. Circ Res 112:1323–1333
Nomura S, Tandon NN, Nakamura T et al (2001) High-shear-stress-induced activation of platelets and microvesicles enhances expression of cell adhesion molecules in THP-1 and endothelial cells. Atherosclerosis 158:277–287
Nomura S, Komiyama Y (1997) Shear stress and platelet-derived microvesicles. Rinsho Byori 45:927–933
Ding J, Chen Z, Niu S et al (2015) Quantification of Shear-Induced platelet activation: high shear stresses for short exposure time. Artif Organs 39:576–583
Giannella A, Ceolotto G, Radu CM et al (2021) PAR-4/Ca(2+)-calpain pathway activation stimulates platelet-derived microvesicles in hyperglycemic type 2 diabetes. Cardiovasc Diabetol 20:77
Nomura S, Imamura A, Okuno M et al (2000) Platelet-derived microvesicles in patients with arteriosclerosis obliterans: enhancement of high shear-induced microparticle generation by cytokines. Thromb Res 98:257–268
Leroyer AS, Ebrahimian TG, Cochain C et al (2009) Microvesicles from ischemic muscle promotes postnatal vasculogenesis. Circulation 119:2808–2817
Karten B, Campenot RB, Vance DE et al (2006) Expression of ABCG1, but not ABCA1, correlates with cholesterol release by cerebellar astroglia. J Biol Chem 281:4049–4057
Komoriyama H, Kimiya K, Nagai T et al (2021) Blood flow dynamics with four-dimensional flow cardiovascular magnetic resonance in patients with aortic stenosis before and after transcatheter aortic valve replacement. J Cardiovasc Magn Reson 23:81
Leroyer AS, Isobe H, Leseche G et al (2007) Cellular origins and thrombogenic activity of microvesicles isolated from human atherosclerotic plaques. J Am Coll Cardiol 49:772–777
Viera AJ, Mooberry M, Key NS (2012) Microvesicles in cardiovascular disease pathophysiology and outcomes. J Am Soc Hypertens 6:243–252
Barthélémy O, Collet JP, Montalescot G (2016) Cerebral embolism: a silent iatrogenic complication of TAVR that needs voiced consideration. J Am Coll Cardiol 68:600–602
Nombela-Franco L, Webb JG, Jaegere PP et al (2012) Timing, predictive factors, and prognostic value of cerebrovascular events in a large cohort of patients undergoing transcatheter aortic valve implantation. Circulation 126:3041–3053
Ghanem A, Kocurek J, Sinning J-M et al (2013) Cognitive trajectory after transcatheter aortic valve implantation. Circ Cardiovasc Interv 6:615–624
Pache G, Schoechlin S, Blanke P et al (2016) Early hypo-attenuated leaflet thickening in balloon-expandable transcatheter aortic heart valves. Eur Heart J 37:2263–2271
Holmes DR Jr, Mack MJ, Kaul S et al (2012) 2012 ACCF/AATS/SCAI/STS expert consensus document on transcatheter aortic valve replacement. J Am Coll Cardiol 59:1200–1254
Acknowledgements
We thank FX for blood sample collection; and JZ and DT for excellent technical assistance.
Funding
This study was supported by the Medical and Health Science and Technology Development Plan Project of Shandong Province (202003010399).
Author information
Authors and Affiliations
Contributions
DT and JL conceived the study. HC, FX, GZ and JZ conducted the assays. GJ, YS and HC collected and analyzed the data, and made the tables and figures, wrote and retouch the manuscript. All authors approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
Authors, HC, YS, FX, GZ, JZ, GJ, DT and JL declare to have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chi, H., Shao, Y., Xie, F. et al. Procoagulant effect of extracellular vesicles in patients after transcatheter aortic valve replacement or transcatheter aortic valve replacement with percutaneous coronary intervention. J Thromb Thrombolysis 56, 264–274 (2023). https://doi.org/10.1007/s11239-023-02835-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-023-02835-5