Abstract
Background: Evidence-based anticoagulation programs usually serve a local, adult patient population. Here we report outcomes for a regional combined pediatric-adult program. Aims: The aims of this study were: (1) Compare the pre- vs. post-implementation quality of therapy (% time in therapeutic range (%TTR) and compliance). (2) Assess anticoagulant-relevant outcomes (bleeding and thrombotic complications). Methods: Data were collected for the years 2014–2019. Rosendaal linear interpolation was used to calculate %TTR. Bleeding complications were categorized using ISTH-SSC standard nomenclature and new thrombotic events were reviewed. Results: The patients were divided into a long-term warfarin group (N = 308), 80.2% of whom had cardiac-related therapeutic indications (median age 24y), and a second group (N = 114) comprised of short-term and non-warfarin long-term anticoagulation (median age 16y). Median %TTR for those on long-term warfarin was 78.9%. The incidence of major and clinically relevant non-major bleeding events was 1.65 and 2.43 /100 person-years of warfarin use, respectively. Thromboembolism (TE) incidence was 0.78/100 patient-years of warfarin use. Neither bleeding nor thrombosis was associated with %TTR (p = 0.48). Anticoagulant indication was the only variable associated with bleeding risk (p = 0.005). The second group had no on-therapy TE events but 7.9% experienced bleeding. Complete data were available for a randomly sampled pre-program warfarin group (N = 26). Median %TTR improved from 17.5 to 87% pre- vs. post-implementation. Similarly, compliance (defined as ≥ 1 INR/month) improved by 34.3%. Conclusions: In conclusion, this program significantly improved and sustained %TTR and compliance. The lack of association between bleeding and thrombosis events and %TTR may be related to the high median %TTR (> 70%) achieved by this approach.
Highlights
Our combined pediatric and pediatric comprehensive anticoagulation program achieved excellent anticoagulation quality as measured by %TTR.
Median %TTR was 78.9% (recommended minimum 60%).
This high %TTR was achievable in both children and adults.
Bleeding and thrombotic events were not associated with %TTR.
Quality of anticoagulation with non-warfarin therapy should be examined in larger cohorts.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The goals of anticoagulation are to treat and/or prevent thromboembolic (TE) events while minimizing bleeding risk [1]. Comprehensive warfarin management programs incorporate patient education, care coordination, self- or laboratory-testing, and real-time dose adjustments to optimize time spent in the therapeutic range (TTR) and decrease adverse events [2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23]. Therapy-related adverse events include bleeding and TE. Most evidence supporting this approach has been developed in programs serving adult patients living within the clinic’s local catchment area. A few pediatric-only and combined pediatric-adult programs have reported improved care using this and other approaches [1,2,3,4,5,6,7,8,9, 11,12,13,14]. Because of its narrow therapeutic index, warfarin efficacy and safety are dependent upon maintaining the international normalized ratio (INR) within the therapeutic range defined by underlying indication. TTR < 60% is associated with suboptimal outcomes across the spectrum of warfarin indications [16, 20, 22, 24,25,26,27,28,29,30,31,32,33].
We established a combined pediatric-adult anticoagulation program in 2014 at a tertiary care children’s hospital that serves 225 adult congenital heart disease survivors on long-term anticoagulation in addition to children and adolescents with cardiac and non-cardiac anticoagulant indications. In contrast to previously reported models that predominantly serve adult patients living in proximity to the host hospital, our program serves patients across a large and diverse (metropolitan and rural) geographic area encompassing central, southeastern, and northwestern Ohio. This is accomplished through a network of ambulatory laboratories strategically located within our 34-county catchment area. This program provides care to both adults and children on long-term warfarin therapy; a smaller group of patients on short-term warfarin therapy or other anticoagulants are also managed. The aims of this study were to compare the impact of our program on anticoagulation quality pre- vs. post-implementation. Quality metrics included %TTR, compliance, and adverse events (bleeding and TE) [34]. Potential variables associated with suboptimal anticoagulation management and adverse events were also examined.
Materials and methods
Medical records of patients receiving anticoagulant care at Nationwide Children’s Hospital (a large tertiary care children’s hospital that provides care for children and adult survivors of complex pediatric conditions) during 2014–2019 were reviewed. The study was approved by the Nationwide Children’s Institutional Review Board. The requirement for informed consent was waived according to 45 CFR 46.116(d) of the US Code of Federal Regulations.
The cohort was divided into two groups: (1) Long-term warfarin therapy and (2) Short-term warfarin (6 weeks to 6 months) and/or non-warfarin anticoagulation. A sub-sample of patients who were followed from 2014 to 2019 and had adequate data to calculate pre-program implementation %TTR and compliance were used to evaluate the impact of the program on quality of care. Patient demographics, anticoagulant indication, anticoagulant agent, target INR range (if applicable), comorbidities (e.g., obesity, hypertension, liver, renal disease, diabetes mellitus, smoking), %TTR, compliance, bleeding, and thrombotic event data were collected.
Rosendaal linear interpolation was used to calculate %TTR [26]. %TTR was calculated for each patient annually and for the entire study period. Compliance was defined as ≥ 1 INR per month and was reported # of months with at least one INR / # of months followed per patient and calendar year [34]. INRs could be obtained from the hospital laboratory using a venipuncture sample or from a fingerstick point-of-care device. Our program utilizes the CoaguChek®XS system (Roche Diagnostics, Indianapolis, IN) for point-of-care testing in our ambulatory lab network. Results from both the hospital laboratory and point-of-care devices are routed to the clinical team via the electronic medical record for same-day clinical decision making. Clinical outcomes such as bleeding and TE were calculated as event rates per 100 person-years of warfarin use. Qlikview software was used to obtain anticoagulation quality data (https://www.qlik.com/us/info/software-ula). This software is linked to the EMR and captures data points of interest for TTR, compliance and duration of anticoagulation. Data for the 26 pre-implementation patients was manually abstracted and analyzed using INRPro© Reporting Systems which utilizes the Rosendaal method for TTR calculation.
Bleeding complications were categorized according to the ISTH-SSC standards for non-surgical anticoagulated patients [35]. Briefly, Major Bleeding was defined as (a) Fatal hemorrhage, and/or (b) Symptomatic bleeding in a critical organ or area, and/or (c) Bleeding causing a ≥ 20 g/L drop in hemoglobin level or leading to transfusion of ≥ 2 units of blood [35]. Clinically relevant non-major bleeding (CRNMB) was defined as any sign or symptom of hemorrhage that did not meet the major bleeding criteria but did meet ≥ 1of the following criteria: (a) Requiring medical intervention by a healthcare professional, (b) Leading to hospitalization or increased level of care, or (c) Prompting a face-to-face evaluation [36]. All bleeds not meeting the Major Bleeding or CRNMB criteria were classified as Minor Bleeding. New or recurrent TE events while receiving anticoagulation were adjudicated by chart and imaging review by one of the authors (VR).
All data were summarized using descriptive statistics. Comparisons of %TTR and compliance between groups were made using Wilcoxon rank sum or Kruskal Wallis test. When comparing more than two groups, p-values were adjusted as appropriate using Dunn’s method. Wilcoxon signed rank tests were used to compare pre- and post-implementation %TTR and compliance on the subset of patients who had pre-implementation data. Chi-square or Fisher’s exact tests were used to compare characteristics of those with or without bleeding and thrombotic events. P-values less than 0.05 were considered statistically significant. Analyses were performed using SAS software, version 9.4 (SAS Institute, Cary NC).
Results
Demographics
Our anticoagulation program served 422 patients from 2014 to 2019. 73% (N = 308) received long-term warfarin while the remainder (N = 114) were on short-term warfarin or other anticoagulants (Table 1). At its inception in 2014, the program served nearly 150 patients and saw steady growth thereafter (Figure S1). The median age of the long-term warfarin patients was 24 years (range: 2–69), 70.5% of these patients were ≥ 18 years old and 80.2% had cardiac-related warfarin indications. This group accumulated 1,028.2 patient-years of warfarin treatment. The short-term group median age was 16 years (range: 0–45) and was predominantly comprised of children (86%) with TE.
Anticoagulation quality
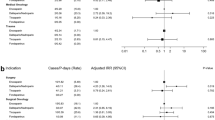
Following program implementation, %TTR was 78.9% (range 80–100%; Figure S2) in the long-term warfarin group. Mean compliance was 79.5% (range 14.8–100%). %TTR was not different between adult (80.3%) and pediatric patients (77.6%; p = 0.90). However, pediatric compliance was higher (87.6% vs. 77.2%; p = 0.0005). There was no difference in %TTR between females and males (77.4% vs. 79.4%; p = 0.84) but compliance was significantly higher in females (84.8% vs. 76.9%; p = 0.0352). Indication and target INR range were both associated with %TTR (p = 0.0055 and p < 0.0001, respectively; Fig. 1). Patients with mechanical valves had a lower %TTR compared to those with TE (adjusted p = 0.0343) but no other significant differences were noted by indication. Patients with target INR 1.5–2.5 had a significantly higher %TTR than those with a goal of 2.0–3.0 (adjusted p = 0.0164) or 2.5–3.5 (adjusted p < 0.0001). Compliance did not differ by indication or INR goal (data not shown).
Time in Therapeutic Range was Influenced by Diagnostic Indication and Goal INR Range. (A) Patients on long-term anticoagulation due to mechanical valve (Mech. Valve) placement spent less time in their goal therapeutic range than did patients being treated to prevent venous thromboembolism (TE) recurrence. No other between indication group differences were significant. (B) Patients on prophylactic warfarin with goal INR 1.5–2.5 achieved a significantly higher percentage time in therapeutic range (%TTR) than did patients whose therapeutic goal was to achieve a higher therapeutic range (2.0–3.0 or 2.5–3.5). A-fib/flutter: atrial fibrillation/flutter. P-values are adjusted using Dunn’s method and denoted as: * < 0.05, ** < 0.01, *** <0.001, **** <0.0001. Median %TTR in each group is displayed with the horizontal bar
Twenty-six (8.4%) of the long-term therapy patients who were followed at our institution and had complete data for both the pre- and post-program implementation periods were subjected to pre-implementation data collection and analysis [median follow up 4.1 years (range: 0.1–12.5 years)] (Table S1). Median pre-implementation %TTR for these 26 patients improved from 17.5 to 87% post-implementation (p < 0.0001; Fig. 2), resulting in a 62.7% overall improvement with 25 (96%) of the patients experiencing %TTR improvement. Compliance also significantly improved in this sub-cohort after program implementation (50% vs. 84.3%, pre- vs. post-, respectively; p < 0.0001; Fig. 2).
Both Time in Therapeutic Range (%TTR) and Compliance Improved after Implementation of the Comprehensive Anticoagulation Management Program. (A) Twenty-five (96.2%) of the 26 patients included in the pre- vs. post-implementation analysis achieved an improved percentage of Time in Therapeutic Range (%TTR). (B) Similarly, 80.8% (21 of 26) patients were more compliant with INR therapeutic monitoring
Bleeding and thrombosis outcomes
Following program implementation, the incidence of major bleeding events was 1.65/100 person-years of warfarin use whereas the incidence of CRNMB/minor bleeding events was 2.43/100 person-years of warfarin use. The incidence of TE was 0.78/100 person-years warfarin use for the long-term warfarin group. Neither bleeding nor TE complications were associated with %TTR when compared to those without an event (p = 0.48; Fig. 3). The underlying diagnosis or indication for anticoagulation was the only identifiable factor associated with bleeding risk (p = 0.0048; Table 2). Five patients died during the study period due complications related to their underlying condition (no deaths were attributable to bleeding or TE). In the pre- vs. post-implementation analysis, there was a trend toward fewer TE post-implementation (p = 0.15; Table S1). Bleeding complications were also insignificantly reduced.
There was No Difference in Median Time in Therapeutic Range for Patients with versus without Bleeding or Thromboembolic Events. Median (IQR) %TTR was similar in patients with vs. without an anticoagulant complication (bleeding or thromboembolic event), likely because the comprehensive anticoagulation management program was able to achieve the published goal %TTR (> 60%) beyond which no additional safety benefit is expected
Discussion
Anticoagulation programs were established with the goal to centralize, standardize, and improve the care of patients on warfarin therapy. Originally, they were implemented for adults with atrial fibrillation, but their scope soon expanded to other anticoagulant indications [37,38,39,40,41,42]. Several studies have documented the ability of these programs to reduce adverse events [2, 3, 5, 7,8,9, 13, 15, 19, 21, 23, 37,38,39,40,41, 43, 44]. Warfarin remains a commonly prescribed anticoagulant that is challenging to manage due to its long-onset and -offset of action, food-drug and drug-drug interactions, and narrow therapeutic index [44]. Moreover, the underlying indication and comorbidities may additionally complicate achievement of high-quality warfarin management. Whereas anticoagulation programs have traditionally served adult patients living near the host facility, pediatric patients and adult survivors of complex pediatric conditions often live over a geographically dispersed area served by a tertiary care children’s hospital which adds logistical complexity to the provision of high-quality anticoagulant management.
Our program provides comprehensive care to both pediatric and adult patients using the previously established model of care but modified to efficiently serve a wider geographic area through a statewide network of ambulatory laboratories [5]. The team is comprised of three physicians (VR, CC, BAK), a nurse practitioner (JG), and two registered nurse clinicians (KM, JC) who provide multidisciplinary care through collaborations between hematology, laboratory medicine, pharmacy, cardiology, and other referring sub-specialties (see Figure S4). The excellent anticoagulation management parameters reported here are made possible through integrated practices. Prescribing practice variation is reduced through implementation of guidelines for each anticoagulant medication. The team provides consulting services to discuss indications, medication choice, therapeutic duration, patient/family education, counseling, care coordination, monitoring, and follow-up. The nurse clinicians are primarily involved in care coordination, laboratory results follow-up, and dose adjustment communicating to the patient/family. Testing compliance is enhanced through collaboration with laboratory medicine to make point-of-care INR monitors available in our ambulatory laboratories (“Close to Home SM Centers”). Patients on long-term warfarin who meet third-party payor pre-authorization criteria are prescribed in-home point-of-care INR monitors to further facilitate compliance. This integrated approach significantly improved %TTR and compliance as demonstrated by our pre- vs. post-implementation data. The median %TTR achieved by this approach (78.9%) exceeded the > 60% target previously proposed as the ideal adult patient goal [17, 20]. Compliance plateaued at 75–80%, further supporting the benefits of this integrated, multidisciplinary approach.
Pediatric warfarin therapy has similar or even greater challenges than encountered in adult populations. Factors affecting warfarin therapy in pediatrics are age-related dose-response rates, concurrent medications, dietary differences, and frequent concurrent illnesses [12, 14, 45,46,47,48]. Nonetheless, high-quality therapy is possible in this age group. An Australian program reported 63.4% TTR in 94 children with 1 major bleeding episode and 2 TE for a combined complication rate of 1.86 events/year [3]. All-cause mortality was 6.9% with 1 event related to thrombosis. A systematic review of 36 pediatric anticoagulation management studies, reported > 60% TTR with 0.5–1.7% bleeding and 1.3-7% TE per year for an overall adverse event rate of 0.5–3.2% per patient/year [1]. In the present study, our pediatric patient bleeding, TE, and %TTR (77.2%) were not significantly different from those of our adult patients.
Warfarin efficacy and safety is related to its pharmacodynamics as measured by INR and proportion of time spent within the prescribed therapeutic INR range [37, 49]. Low INR values increase TE risk and high INR values increase bleeding risk. It is challenging to maintain a high %TTR due to wide inter- and intra-individual warfarin effects that lead to sub- or supra-therapeutic INRs 25–40% of the time [26, 49,50,51,52,53]. %TTR is inversely correlated with bleeding complications, thus the benefits of anticoagulation diminish with poor-quality warfarin therapy [24, 27, 28]. However, the correlation between %TTR and bleeding disappears when TTR is > 70% [55]. Several studies have demonstrated that bleeding and TE primarily occur with lower %TTR and the association between %TTR and complications is nonlinear [16, 28, 29, 56]. These data suggest that adverse events are much less likely when %TTR is > 70%. Thus, the lack of %TTR correlation with bleeding and TE in our long-term warfarin patients is likely explained by our program’s achievement of %TTR > 70%.
The bleeding and TE rates in this study are similar to those reported in other studies [1, 3, 18, 20, 57]. Comorbidities did not significantly influence adverse outcomes in this study (Table 2). However, warfarin indication was significantly associated with bleeding, with the mechanical valve group appearing to drive this association, perhaps because these patients were more likely to be prescribed a higher target INR goal (50% of the patients with mechanical valves were in the highest INR range; Figure S3). Other factors such as age, gender, dual therapy with aspirin, and comorbidities were not associated with bleeding risk (Table 2). The 26-patient comparator cohort demonstrated that bleeding and TE complications were insignificantly reduced after program implementation. However, this analysis may have been underpowered due to the low number of patients with complete data available for inclusion. The second group of patients on short-term warfarin or other anticoagulants experienced no TE during the study period but did have 9 bleeding events (Table 1). Low molecular weight heparin and direct oral anticoagulant care quality should be explored in future studies, particularly in pediatrics.
Limitations
We were unable to obtain pre-implementation %TTR, compliance, bleeding, and thrombosis data on the entire cohort due to the lack of an electronic medical record (EMR) system that consistently captured these data. Our program was implemented concurrently with our hospital’s adoption of Epic Healthcare Systems (Verona, WI) EMR which enabled the capture of these data post-implementation. Fortunately, we were able to manually abstract these data on 26 patients who were followed both pre- and post-implementation. These records enabled an evaluation of pre- versus post-implementation warfarin quality. Nonetheless, this small sample limited our ability to comprehensively compare outcomes for the entire cohort. An important strength, however, is that each of these 26 patients served as his/her own pre-implementation control. Although our program is moderate-to-large in comparison to patient volumes reported elsewhere, we were inadequately powered to perform comprehensive analyses adjusting for age, comorbidities, INR range, or underlying diagnoses. Compliance was measured in this study as ≥ 1 INR per month, a more comprehensive compliance definition might include patient/family understanding of medication adherence and cognizance of potential dietary and drug interactions, as reported elsewhere [58, 59]. Sociodemographic determinants impacting healthcare access and therapeutic compliance should be further explored in different models of anticoagulant care.
Another limitation to our study was the wide variability of surgical procedures and interventions in the CHD cohort, which limited our ability to compare groups of patients who underwent similar procedures and interventions. However, thrombotic events were reviewed for each patient through their EMR. These events relied on clinical documentation in the EMR. Additionally, Fontan patients are heterogenous in terms of their management (e.g., aspirin use, surgical interventions, type of anticoagulant used) limiting our ability to utilize this subgroup as a comparator. Only those patients managed with warfarin were used for comparative analysis. In addition, similar to other anticoagulation quality data it is not possible to causally link TTR and clinical endpoints (e.g. thrombosis, bleeding).
Conclusion
Our multidisciplinary comprehensive anticoagulation program consistently demonstrated > 70% TTR for both children and adults on warfarin therapy. This optimal %TTR and compliance was sustained during the study period, resulting in relatively low bleeding and TE rates. Further analysis suggested that underlying diagnosis is significantly associated with bleeding events, perhaps driven by patients with mechanical heart valves who often require a higher target INR range. %TTR did not differ between patients with vs. without a bleeding or TE event, likely because the program achieved a high median %TTR (> 70%) that has been reported to stabilize these event rates. This study demonstrates that both pediatric and adult patients can achieve high-quality anticoagulant therapy when managed by a multidisciplinary team using an integrated approach to serve a wide geographic area.
References
Jones S et al (2011) Assessing outcome measures of oral anticoagulation management in children. Thromb Res 127(2):75–80
Jones S et al (2016) Safety and Efficacy Outcomes of Home and Hospital Warfarin Management within a Pediatric Anticoagulation Clinic. J Pediatr Hematol Oncol 38(3):216–220
Newall F et al (2004) Anticoagulation clinics for children achieve improved warfarin management. Thromb Res 114(1):5–9
Biss TT et al (2011) Comparison of ‘time within therapeutic INR range’ with ‘percentage INR within therapeutic range’ for assessing long-term anticoagulation control in children. J Thromb Haemost 9(5):1090–1092
Murray JM et al (2015) Utility of a dedicated pediatric cardiac anticoagulation program: the Boston Children’s hospital experience. Pediatr Cardiol 36(4):842–850
Maagdenberg H et al (2018) Characteristics and quality of oral anticoagulation treatment in pediatric patients in the Netherlands based on the CAPS cohort. J Thromb Haemost 16(1):116–124
Bauman ME et al (2009) KIDCLOT©: the importance of validated educational intervention for optimal long term warfarin management in children. Thromb Res 123(5):707–709
Bradbury MJE et al (2008) A comparative study of anticoagulant control in patients on long-term warfarin using home and hospital monitoring of the international normalised ratio. Arch Dis Child 93(4):303
Christensen TD et al (2004) Oral anticoagulation therapy in children: successfully controlled by self-management. Heart Surg Forum 7(4):E321–E325
Christensen TD et al (2003) Mechanical heart valve patients can manage oral anticoagulant therapy themselves. Eur J Cardiothorac Surg 23(3):292–298
Mähönen S et al (2004) Oral anticoagulant treatment in children based on monitoring at home. Acta Paediatr 93(5):687–691
Massicotte P et al (1995) Home monitoring of warfarin therapy in children with a whole blood prothrombin time monitor. J Pediatr 127(3):389–394
Newall F, Monagle P, Johnston L (2006) Home INR monitoring of oral anticoagulant therapy in children using the CoaguChek S point-of-care monitor and a robust education program. Thromb Res 118(5):587–593
Streif W et al (1999) Analysis of warfarin therapy in pediatric patients: a prospective cohort study of 319 patients. Blood 94(9):3007–3014
Rivera-Caravaca JM et al (2020) A nurse-led atrial fibrillation clinic: impact on anticoagulation therapy and clinical outcomes. Int J Clin Pract 74(12):e13634
Vestergaard AS et al (2017) The importance of mean time in therapeutic range for complication rates in warfarin therapy of patients with atrial fibrillation: a systematic review and meta-regression analysis. PLoS ONE 12(11):e0188482
Proietti M, Lip GYH (2018) Impact of quality of anticoagulation control on outcomes in patients with atrial fibrillation taking aspirin: an analysis from the SPORTIF trials. Int J Cardiol 252:96–100
Oake N et al (2008) Anticoagulation intensity and outcomes among patients prescribed oral anticoagulant therapy: a systematic review and meta-analysis. CMAJ 179(3):235–244
Ingram SJ et al (2018) Moving anticoagulation initiation and monitoring services into the community: evaluation of the Brighton and hove community pharmacy service. BMC Health Serv Res 18(1):91
Veeger NJ et al (2005) Individual time within target range in patients treated with vitamin K antagonists: main determinant of quality of anticoagulation and predictor of clinical outcome. A retrospective study of 2300 consecutive patients with venous thromboembolism. Br J Haematol 128(4):513–519
Witt DM et al (2005) Effect of a centralized clinical pharmacy anticoagulation service on the outcomes of anticoagulation therapy. Chest 127(5):1515–1522
Faircloth JM et al (2017) Time in therapeutic range as a marker for thrombotic and bleeding outcomes in Fontan patients. J Thromb Thrombolysis 44(1):38–47
Lee T, Davis E, Kielly J (2016) Clinical impact of a pharmacist-led inpatient anticoagulation service: a review of the literature. Integr Pharm Res Pract 5:53–63
Connolly SJ et al (2008) Benefit of oral anticoagulant over antiplatelet therapy in atrial fibrillation depends on the quality of international normalized ratio control achieved by centers and countries as measured by time in therapeutic range. Circulation 118(20):2029–2037
White HD et al (2007) Comparison of outcomes among patients randomized to warfarin therapy according to anticoagulant control: results from SPORTIF III and V Archives of internal medicine. 167:239–2453
Rosendaal FR et al (1993) A method to determine the optimal intensity of oral anticoagulant therapy. Thromb Haemost 69(3):236–239
Wan Y et al (2008) Anticoagulation control and prediction of adverse events in patients with atrial fibrillation: a systematic review. Circ Cardiovasc Qual Outcomes 1(2):84–91
Van Den Ham HA et al (2013) The patterns of anticoagulation control and the risk of stroke, bleeding and mortality in patients with non-valvular atrial fibrillation. J Thromb Haemost 11(1):107–115
Senoo K, Lip GY (2015) Relationship of Age with stroke and death in anticoagulated patients with Nonvalvular Atrial Fibrillation: AMADEUS Trial. Stroke 46(11):3202–3207
Pokorney SD et al (2015) Patients’ time in therapeutic range on warfarin among US patients with atrial fibrillation: results from ORBIT-AF registry. Am Heart J 170(1):141–148e1
Chan PH et al (2016) Time in Therapeutic Range and Percentage of International Normalized Ratio in the Therapeutic Range as a Measure of Quality of Anticoagulation Control in Patients With Atrial Fibrillation Can J Cardiol, 32(10): p. 1247.e23-1247.e28
Miah MK et al (2019) Chap. 29 - clinical pharmacokinetics. Clinical Pharmacy Education, Practice and Research. Elsevier, pp 409–424. D. Thomas, Editor
Marcatto LR et al (2018) Pharmaceutical Care increases time in therapeutic range of patients with poor quality of Anticoagulation with Warfarin. Frontiers in Pharmacology, p 9
Ansell J et al (2004) The pharmacology and management of the vitamin K antagonists: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy Chest, 126(3 Suppl): p. 204s-233s
Schulman S, Kearon C (2005) Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non-surgical patients. J Thromb Haemost 3(4):692–694
Kaatz S et al (2015) Definition of clinically relevant non-major bleeding in studies of anticoagulants in atrial fibrillation and venous thromboembolic disease in non-surgical patients: communication from the SSC of the ISTH. J Thromb Haemost 13(11):2119–2126
Ansell JE, Hughes R (1996) Evolving models of warfarin management: anticoagulation clinics, patient self-monitoring, and patient self-management. Am Heart J 132(5):1095–1100
Rudd KM, Dier JG (2010) Comparison of two different models of anticoagulation management services with usual medical care. Pharmacotherapy 30(4):330–338
Garrison SR, Allan GM (2014) Do specialty anticoagulation clinics really outperform primary care at INR management? J Thromb Thrombolysis 38(3):420–421
McGuinn TL, Scherr S (2014) Anticoagulation clinic versus a traditional warfarin management model. Nurse Pract 39(10):40–46
Stoudenmire LG, DeRemer CE, Elewa H (2014) Telephone versus office-based management of warfarin: impact on international normalized ratios and outcomes. Int J Hematol 100(2):119–124
Entezari-Maleki T et al (2016) A systematic review on comparing 2 common models for management of warfarin therapy; pharmacist-led service versus usual medical care. J Clin Pharmacol 56(1):24–38
Hendriks JML et al (2019) Integrated specialized atrial fibrillation clinics reduce all-cause mortality: post hoc analysis of a randomized clinical trial. Europace 21(12):1785–1792
Barnes GD et al (2018) Structure and function of anticoagulation clinics in the United States: an AC forum membership survey. J Thromb Thrombolysis 46(1):7–11
Monagle P et al (2012) Antithrombotic therapy in neonates and children: antithrombotic therapy and Prevention of thrombosis, 9th ed: american college of chest Physicians evidence-based clinical practice guidelines.Chest, 141(2 Suppl): p. e737S-e801S.
Monagle P et al (2018) American Society of Hematology 2018 guidelines for management of venous thromboembolism: treatment of pediatric venous thromboembolism. Blood Adv 2(22):3292–3316
Andrew M (1996) Indications and drugs for anticoagulation therapy in children. Thromb Res 81(2 Suppl):S61–73
Andrew M et al (1994) Oral anticoagulation therapy in pediatric patients: a prospective study. Thromb Haemost 71(3):265–269
Hirsh J et al (2003) American Heart Association/American College of Cardiology Foundation guide to warfarin therapy. J Am Coll Cardiol 41(9):1633–1652
Hirsh J (1991) Oral anticoagulant drugs. N Engl J Med 324(26):1865–1875
Cannegieter SC et al (1995) Optimal oral anticoagulant therapy in patients with mechanical heart valves. N Engl J Med 333(1):11–17
Azar AJ et al (1996) Optimal intensity of oral anticoagulant therapy after myocardial infarction. J Am Coll Cardiol 27(6):1349–1355
Rosendaal FR (1996) The Scylla and Charybdis of oral anticoagulant treatment. N Engl J Med 335(8):587–589
Kirchhof P et al (2016) ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS Eur Heart J, 2016. 37(38): p. 2893–2962
Sandén P et al (2015) Warfarin treatment complications do not correlate to cTTR when above 70. Thromb Res 136(6):1185–1189
Cancino RS et al (2014) Comparing patient-level and site-level anticoagulation control as predictors of adverse events. Thromb Res 133(4):652–656
Levine MN et al (2001) Hemorrhagic complications of anticoagulant treatment. Chest 119(1 Suppl):108s–121s
Huber CS, Levett JM, Atkinson JM (2008) Advances in Patient Safety A Tool to assess compliance in Anticoagulation Management. In: Henriksen K et al (eds) Advances in Patient Safety: new directions and alternative approaches (Vol. 3: performance and tools). Rockville (MD), Agency for Healthcare Research and Quality (US)
Orensky IA, Holdford DA (2005) Predictors of Noncompliance with Warfarin Therapy in an Outpatient Anticoagulation Clinic Pharmacotherapy: The Journal of Human Pharmacology and Drug Therapy, 25(12): p. 1801–1808
Funding
No internal or external source of funding was used for this study.
Author information
Authors and Affiliations
Contributions
VR designed study design, performed retrospective data acquisition and drafted the manuscript. JS performed statistical analysis and review manuscript. AD, CC, AS, KM, JG, JC reviewed the manuscript. BK contributed to study design and writing of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest to declare that are relevant to the content of this article.
Ethical approval
This study was approved by the Nationwide Children’s Institutional Review Board. The requirement for informed consent was waived according to 45 CFR 46.116(d) of the US Code of Federal Regulations.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
*This study was presented as an abstract and poster at the International Society on Thrombosis and Haemostasis, July 17-21, 2021.
Electronic supplementary material
Below is the link to the electronic supplementary material.
11239_2023_2806_MOESM2_ESM.docx
Supplementary Material 2: Figure S1: Steady Growth of a Comprehensive Anticoagulation Management Program Serving Children and Adult Survivors of Complex Pediatric Conditions at a Large Tertiary Care Children’s Hospital. Number of long-term warfarin therapy patients served per year (orange bars) and patients per year treated with short-term warfarin therapy or other anticoagulants (blue bars)
Figure S2: % TTR and % Compliance Following Implementation Anticoagulation Clinic. (A) %TTR (± standard error) for each post-implementation year of the program. (B) Mean compliance (± standard error) for each post-implementation year of the program. Compliance was measured as ≥ 1 INR/month and the average calculated per year
Figure S3: Target INR is Dictated by Warfarin Indication and Influences %TTR. Patients with mechanical valves were more likely to be prescribed a higher INR goal range and %TTR tended to decrease as the INR goal range increased, suggesting that it is more difficult to maintain high quality anticoagulation in patients with higher INR goal ranges
11239_2023_2806_MOESM5_ESM.docx
Supplementary Material 5: Figure S5: Anticoagulation Program Organizational Diagram
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rodriguez, V., Stanek, J., Cua, C.L. et al. A regional anticoagulation program improves safety and outcomes for both children and adults. J Thromb Thrombolysis 56, 27–36 (2023). https://doi.org/10.1007/s11239-023-02806-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-023-02806-w