Abstract
Patients on long-term anticoagulation combined with antiplatelet therapy have an increased risk of bleeding compared to patients on anticoagulation alone. The aim of this study was to evaluate the appropriateness of antiplatelet therapy in patients who are on long-term warfarin therapy and are managed by Brigham and Women’s Hospital Anticoagulation Management Service (BWH AMS). This was a single-center, prospective chart review of patients managed by BWH AMS who were on long-term warfarin therapy plus full-dose aspirin (325 mg), an oral P2Y12 inhibitor (clopidogrel, prasugrel or ticagrelor) and/or acetylsalicylic acid/dipyridamole. Patients’ cardiovascular (CV) benefit and risk of bleeding were assessed according to clinical guidelines. The major objective of the study was to determine the proportion of patients on dual antithrombotic therapy (DAT) or triple antithrombotic therapy (TAT) whose risk of bleeding outweighed CV benefit. Of the 2677 patients evaluated for inclusion,145 were on concomitant long-term warfarin therapy plus aspirin (325 mg), an oral P2Y12 inhibitor and/or acetylsalicylic acid/dipyridamole. A total of 85 patients (58.6%) had no clear indication for DAT or TAT per guideline recommendations and were categorized as bleeding risk outweighing CV benefit. The remaining 60 patients (41.4%) had an appropriate indication for DAT or TAT per guidelines and were categorized as CV benefit outweighing bleeding risk. BWH AMS pharmacists made 33 (22.9%) recommendations to providers to discontinue or de-escalate antiplatelet therapy. Interventions were accepted for 10 (30.3%) patients. Pharmacist involvement in the management of patients’ antithrombotic regimens can optimize guideline-directed medical therapy and mitigate the potential risk of bleeding.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Highlights
-
Patients on combined antiplatelet and anticoagulation therapy are at an increased risk of bleeding compared to patient’s on anticoagulation therapy alone.
-
The decision to add, continue or de-escalate antiplatelet therapy requires an analysis of each patient’s risk of bleeding and cardiovascular benefit.
-
BWH AMS pharmacists intervened by reaching out to providers and recommending de-escalating or discontinuing antiplatelet therapy in patients whose risk of bleeding outweighs cardiovascular benefit, per clinical guidelines.
-
Integrating a proactive assessment tool into the BWH AMS patient enrollment process which assesses CV benefit and the risk of bleeding will help optimize treatment and reduce the potential risk of bleeding.
Introduction
Antithrombotic medications reduce the risk of thrombosis by inhibiting platelet aggregation and coagulation. Antiplatelet agents prevent platelets from aggregating and forming a clot. Anticoagulant agents inhibit clotting factors required for clot formation [1].
Patients with cardiovascular disease (CVD) are at increased risk of developing subsequent CVD events, including acute coronary syndrome (ACS), stroke, transient ischemic attack (TIA), or peripheral artery disease (PAD). For several decades, antiplatelet therapy was used for primary CVD prevention. This was due to several observational and randomized controlled trials which showed antiplatelets to be effective in reducing the risk of myocardial infarction (MI), stroke, vascular events, and mortality. However, the role of antiplatelet therapy has evolved. Recent studies have shown that the use of antiplatelet therapy solely for primary prevention of CVD provides minor benefit and is associated with an increased risk of bleeding [2,3,4]. Antiplatelet therapy is indicated for secondary CVD prevention, stable CAD, or ACS in patients who may have undergone a percutaneous coronary intervention (PCI) with placement of a stent, coronary artery bypass grafting, stroke, TIA, PAD, diabetes, and for primary prevention of colorectal cancer [4,5,6,7,8,9,10,11,12].
Anticoagulation is indicated in patients with atrial fibrillation (AF), left ventricular assist device (LVAD), venous thromboembolism (VTE) including deep vein thrombosis (DVT) and pulmonary embolism (PE), mechanical heart valve replacement or repair, acute ischemic stroke, antiphospholipid syndrome, and peripheral arterial disease [5,6,7,8, 13].
Concomitant use of anticoagulant and antiplatelet therapy increases the risk of bleeding. The risk of major bleeding is higher with combination antithrombotic and antiplatelet therapy, particularly with warfarin plus aspirin compared to warfarin alone [14,15,16]. The HAS-BLED score (hypertension, abnormal renal/liver function, stroke, bleeding history or predisposition, labile international normalized ratio (INR), age > 65 years and alcohol use) quantifies the risk of major bleeding in patients on anticoagulation [17]. Although this bleeding risk assessment tool was developed primarily for patients with AF, it has been extrapolated to anticoagulated patients without AF who are on concomitant DAT or TAT [18].
When evaluating patients who require long-term anticoagulation, the decision to add or continue antiplatelet therapy for secondary prevention of CVD requires analysis of the individual patient’s risk of bleeding and CV benefit. The three objectives of this study are: to evaluate the appropriateness of antiplatelet therapy in patients who receive concomitant long-term warfarin therapy, provide recommendations to the primary treatment team to optimize antithrombotic therapy where appropriate, and to improve our institution’s anticoagulation stewardship program.
Methods
Study design and patient selection
This was a single-center, prospective chart review at a tertiary academic medical center in Boston, Massachusetts, which was approved by the Partner’s Healthcare Institutional Review Board. Patients were included if they were managed by Brigham and Women’s Hospital Anticoagulation Management Service (BWH AMS), 18 years of age or older, and on long-term warfarin therapy plus aspirin (325 mg), an oral P2Y12 inhibitor (clopidogrel, prasugrel or ticagrelor), and/or acetylsalicylic acid/dipyridamole as of August 15, 2018. All pertinent patient information was collected between August 15, 2018 and March 31, 2019. Patients not on aspirin 325 mg, an oral P2Y12 inhibitor, and/or acetylsalicylic acid/dipyridamole or those who had an incomplete medical record (i.e., patients no longer followed by BWH AMS) were excluded. All patient information was obtained from the institution’s electronic health records (EHR), which include Epic™ and DawnAC™. Patients’ antithrombotic regimens were evaluated for compliance with clinical guidelines.
Major and minor outcomes
The major outcome of this study was the percent of patients on DAT or TAT whose risk of bleeding outweighs CV benefit. CV benefit was defined as patients having an indication for DAT or TAT based on clinical guideline recommendations [6,7,8,9, 12, 13]. High bleeding risk was defined as a HAS-BLED score greater than or equal to three. For patients with a guideline indication for DAT or TAT, bleeding risk was assessed [19, 20]. Given the high risk of bleeding and the presence of CV benefit in these patients, BWH AMS pharmacists would consider interventions to mitigate the bleeding risk by modifying the patient’s therapeutic INR range to 2–2.5, or by eliminating modifiable bleeding risk factors after discussion with the referring provider, [21, 22]. For patients without a guideline indication for DAT or TAT, regardless of the HAS-BLED score, the risk of bleeding was considered to outweigh CV benefit, and the patient’s referring provider was consulted. For example, patients on antiplatelet therapy for primary prevention of CVD are at an increased risk of bleeding as they have no indication for being on antiplatelet therapy per clinical guidelines and recent studies [2, 3].
After completing a risk versus benefit analysis for each patient, the BWH AMS pharmacist would then reach out to the patient’s referring provider via email to recommend discontinuation or de-escalation of antiplatelet therapy if a patient had no clear documented indication for being on DAT or TAT. The pharmacist would then follow-up with the primary provider on whether our recommendation was accepted and ensure that the patient’s medication list was updated with the appropriate therapy on their EHR. The percentage of recommendations accepted was captured as well as the rationale for continuing antiplatelet therapy for those recommendations not accepted. The minor outcomes of this study were to evaluate the percent of patients on DAT or TAT whose CV benefit outweighs the risk of bleeding, the percent of BWH AMS pharmacist recommendations made to primary providers to discontinue antiplatelet therapy in patients with no clear documented indication, and the rationale for the continuation of antiplatelet therapy if the BWH AMS pharmacist recommendation was not accepted by the patient’s primary provider.
Patient information collected included age, gender, primary and secondary indication of antithrombotic therapy, target INR, time in therapeutic range (TTR), other relevant co-morbidities, components of the HAS-BLED score and pertinent medications that can increase bleeding risk. Medications identified to increase the risk of bleeding included: aspirin 81 mg, azathioprine, selected herbals, H2 antagonists, non-steroidal anti-inflammatory drugs (NSAIDs), selective serotonin reuptake inhibitors (SSRIs), and serotonin and norepinephrine reuptake inhibitors (SNRIs). For the purpose of this study, when referring to antithrombotic therapy, the following were included: aspirin 325 mg, clopidogrel, prasugrel, ticagrelor, and acetylsalicylic acid/dipyridamole. Descriptive analysis was used to report outcomes.
Results
Patient analysis
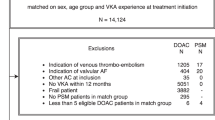
Overall, 2677 patient charts were evaluated for inclusion, and 145 patients were included in the final analysis. Of the total population initially screened, 2531 patients were excluded for not being on aspirin 325 mg, an oral P2Y12 inhibitor or acetylsalicylic acid/dipyridamole, and one patient was excluded due to having an incomplete medical record. Notably, among the 2531 patients who were excluded, 787 patients had documentation of low-dose aspirin 81 mg (n = 695) or aspirin with no dose (n = 92) defined in their EHR. These patients were not included in our data analysis. However, by identifying these patients, the BWH AMS pharmacists had the opportunity to intervene on these patients and/or update their medication list in the EHR to be more accurate.
A total of 143 patients were on DAT and two patients were on TAT (Fig. 1). Of the 143 patients on DAT, 91 patients were on warfarin plus clopidogrel, 44 patients were on warfarin plus aspirin 325 mg, four patients were on warfarin plus ticagrelor, three patients were on warfarin plus prasugrel, and one patient was on warfarin plus acetylsalicylic acid/dipyridamole. The two patients who were on TAT were on warfarin, clopidogrel and aspirin 325 mg.
Baseline characteristics
Patients included in the final analysis were primarily male (68%). In the overall group analyzed, the mean age was 66.3 ± 15.1 years with an average TTR of 69.2 ± 19.1. When evaluating each patient’s antiplatelet therapy, patients were on clopidogrel (64.1%), aspirin 325 mg (31.7%), prasugrel (2.1%), ticagrelor (1.4%), and acetylsalicylic acid/dipyridamole (0.7%). With regard to the primary indication for anticoagulation, 32.6% had AF, 22.9% had an LVAD, 11.1% had DVT/PE, 7.6% had an arterial embolism, 5.6% had an aortic/mitral valve replacement, 5.6% had a stroke/TIA, 4.9% had a mural thrombus, 4.1% had antiphospholipid syndrome, 2.8% had peripheral vascular disease, 2.1% had graft/stent thrombosis and 0.7% had cardiomyopathy/low ejection fraction (Table 1).
Of the 145 patients on DAT or TAT, 60 (41.4%) were on appropriate therapy and had a guideline indication, while 85 (58.6%) patients had no clear guideline indication for DAT or TAT. Of these patients, 41 (48.2%) already had undergone an intervention during the analysis period, and antiplatelet therapy was either discontinued or the patient was transitioned to a direct oral anticoagulant (DOAC). The remaining 44 (51.8%) patients required a pharmacist intervention. When evaluating the 44 patients, 11 patients were excluded (6 patients died, 3 patients transferred care, and 2 patients transitioned to a DOAC during the data collection period). For the remaining 33 patients, a BWH AMS pharmacist contacted the patient’s referring provider via email and recommended discontinuation or de-escalation of antiplatelet therapy due to lack of an appropriate indication for antiplatelet therapy documented in the EHR. The email consisted of a summary of the patient’s past medical history and indication for anticoagulation, his/her current antithrombotic therapy and the pharmacist’s recommendation to discontinue or de-escalate therapy. We also asked providers to clarify if there is an appropriate indication that may not have been documented in the patient’s EHR. The pharmacist would then follow-up with the patient’s referring provider to ensure that the antiplatelet agent was discontinued or de-escalated, and the patient’s medication list was updated with the current antithrombotic therapy. If the provider chose to continue antithrombotic therapy, despite the pharmacist’s recommendation, the reason for continuation was documented in the patient’s EHR (Fig. 2).
A total of 10 (30.3%) providers accepted the recommendation, 11 (33.3%) providers rejected the recommendation due to provider preference or deferring to patient’s alternative provider outside of BWH, 8 (24.2%) providers did not respond, and 4 (12.1%) patients had already stopped taking antiplatelet therapy which had not yet been reflected on their medication list in the EHR. The pharmacist updated each patient’s medication list if a discrepancy was identified. The major outcome occurred in 58.6% of patients who were on concomitant anticoagulant and antiplatelet therapy without a clear indication for DAT/TAT. The minor outcome for CV benefit outweighing bleeding risk was identified in 41.4% of patients (Table 2).
The results of this study allowed BWH AMS to improve the institution’s standardized referral process and antithrombotic stewardship program. By identifying different patient populations prescribed concomitant anticoagulation and antiplatelet therapy, we adjusted the BWH AMS referral process by including specific questions regarding concomitant antiplatelet therapy when enrolling patients at BWH AMS. Now, referring providers are also asked if the patient is currently taking one or more antiplatelet agent; and if yes, which agent it is and the indication for treatment. The AMS intake form now includes a request for the provider to indicate when antiplatelet therapy can be discontinued. Some patients may be referred to BWH AMS by a provider who does not longitudinally follow the patient (i.e., patients admitted to the emergency department who require a referral to BWH AMS). For these patients, we included an “unable to confirm” option for providers to choose. By doing so, BWH AMS pharmacists can then follow up with the patient and patient’s primary provider to ensure appropriate therapy and indication is correctly documented in the patient’s EHR.
Discussion
Of the 145 patients analyzed, 60 patients had an appropriate guideline indication for DAT or TAT, and 85 patients had no clear documented indication for DAT or TAT per guidelines. Of the 85 patients with no indication, 41 patients already had an intervention to discontinue antiplatelet therapy or transition to a DOAC completed by another provider outside of AMS [18, 21, 23]. Transitioning from warfarin to a DOAC has been associated with a lower risk of bleeding in patients on DAT or TAT in clinical trials [17, 18, 23]. The remaining 44 patients required a BWH AMS pharmacist intervention, who recommended either discontinuation or de-escalation of antiplatelet therapy. Notably, 12 (34%) patients who were considered to be on DAT (with a P2Y12 inhibitor) were also on low-dose aspirin 81 mg, with no clear indication or explanation to why they were on dual antiplatelet therapy.
When evaluating patients for DAT or TAT, the primary references used were the American College of Cardiology (ACC)/American Heart Association (AHA) guideline for primary prevention of CVD (2019), the AHA/ACC/Heart Rhythm Society (HRS) updated guideline on the management of patients with AF (2019), the CHEST guideline on antithrombotic therapy for AF (2018), the updated ACC/AHA guidelines for the management of valvular heart disease (2017), and the CHEST guideline on primary and secondary prevention of CVD [5,6,7,8,9]. These guidelines recommend the use of both antiplatelet and anticoagulation therapy in secondary CVD prevention, acute anterior MI or left ventricular thrombus (with or without stent placement), AF (with ACS or elective PCI), valvular heart disease, and LVAD. The recommendations for each of these conditions may vary from one clinical guideline to another in terms of duration of treatment (Online Resource 1), but overall, no guideline recommends TAT for greater than 6 months. When assessing patients for DAT, they need to be evaluated individually to ensure appropriate therapy and duration of treatment is being met.
A limitation of this study was that this was a single-center prospective chart review which only provided descriptive data. Patients who were taking low-dose aspirin 81 mg were not captured as part of our inclusion criteria due to the inconsistency of aspirin 81 mg recorded in the medication list in the EHR. There were 787 patients who were either on aspirin 81 mg or aspirin with no defined dose. However, despite the exclusion of these patients from this analysis, BWH AMS pharmacists continued to evaluate these patients to provide antithrombotic stewardship. Additionally, patients on oral anticoagulation other than warfarin were not evaluated due to the small population of patients in our clinic on DOACs who were on DAT or TAT.
In this model, the AMS pharmacist worked under a collaborate drug therapy management (CDTM) agreement with providers allowing them to manage a patient’s drug therapy. This agreement allowed the pharmacist to reach out to providers to discontinue or de-escalate therapy and update patient’s medication list. Similar interventions could be completed by other advanced practice clinicians such as registered nurses, physician assistants and nurse practitioners if they work under a CDTM agreement, which could be further adjusted to fit the needs of the institution.
Conclusion
Pharmacist involvement in the management of patients’ antithrombotic regimens facilitates optimization of patient treatment plans and mitigates the potential risk of bleeding. By completing this prospective study, we were able to evaluate all updated clinical guideline recommendations on the use of antiplatelet and anticoagulation therapy to ensure patients at BWH AMS are being managed appropriately. The results of this study were utilized to incorporate proactive assessment tools of DAT or TAT into the BWH AMS patient enrollment and referral process. The new patient enrollment process allows AMS pharmacists to screen all patients for antiplatelet therapy upon referral, then as part of the annual review process, patient records will be re-assessed for the need of concomitant antiplatelet therapy. By implementing an efficient, sustainable, and evidence-based system at our institution, patient care will be standardized, leading to improved patient outcomes and reduced risk of anticoagulant-related adverse drug events [24].
References
Schafer AI (2008) 50 years in hematology, Chapter 3: platelet and blood clotting. Antithromb Ther Am Soc Hematol 3:28–32
McNeil JJ et al (2018) Effect of aspirin on all-cause mortality in the healthy elderly (ASPREE trial). N Engl J Med 379:1519–1528
McNeil JJ et al (2018) Effects of aspirin on cardiovascular events and bleeding in the healthy elderly. N Engl J Med 379:1509–1518
Ridker PM et al (2005) A randomized trial of low-dose aspirin in the primary prevention of cardiovascular disease in women. N Engl J Med 352:1293–1304
Vandvik PO et al (2012) Primary and secondary prevention of cardiovascular disease: antithrombotic therapy and prevention of thrombosis, 9th ed. CHEST 141(2):e637S–e668S
January CT et al (2019) AHA/ACC/HRS focused update of the 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation. Circulation 140:e125–e151
Nishimura RA et al (2017) ACC/AHA focused update of the 2014 AHA/ACC guideline for the management of patients with valvular heart disease. Circulation 135:e1159–e1195
Kernan WN et al (2014) Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack. Stroke 45:2160–2236
Angiolillo DJ et al (2007) Antiplatelet therapy in type 2 diabetes mellitus. Curr Opin Endocrinol Diabetes Obes 14:124–131
Engstrom PF et al (2009) (2009) Colon Cancer, clinical practice guidelines in oncology. JNCCN 7:778–831
Dube C et al (2007) The use of aspirin for primary prevention of colorectal cancer: a systematic review prepared for the U.S. preventive service task force. Ann Intern Med 146(5):365–375
Levine GN et al (2016) American College of Cardiology (ACC)/American Heart Association (AHA) guideline focused update on duration of dual antiplatelet therapy in patients with coronary artery disease. Circulation 134:e123–e155
Kirchhof P et al (2016) European Society of Cardiology (ESC): guidelines for the management of atrial fibrillation developed in collaboration with European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J 37:2893–2962
Dentali F, Douketis JD, Lim W, Crowther M (2007) Combined aspirin-oral anticoagulant therapy compared with oral anticoagulant therapy alone among patients at risk for cardiovascular disease: a meta-analysis of randomized trials. Arch Intern Med 167:117–124
Johnson SG, Rogers K, Delate T et al (2008) Outcomes associated with combined antiplatelet and anticoagulant therapy. CHEST 133:948–954
Marik PE, Cavallazzi R (2015) Extended anticoagulant and aspirin treatment for the secondary prevention of thromboembolic disease: a systematic review and meta-analysis. PLoS One 359:143–252
Roldan V et al (2013) The HAS-BLED score has better prediction accuracy for major bleeding than CHADS2 or CHADS2-VASc scores in anticoagulated patient with atrial fibrillation. J Am Coll Cardiol
Omran H et al (2012) The HAS-BLED score predicts bleedings during bridging of chronic oral anticoagulation. Results from the national BNK online bRiDging REgistRy (BORDER). Thromb Haemost 108(1):65–73
Shireman TI, Howard PA, Kresowik TF et al (2004) Combined anticoagulant-antiplatelet use and major bleeding events in elderly atrial fibrillation patients. Stroke 35:2362–2367
Turan B, Demir H, Mutlu A et al (2016) Inappropriate combination of warfarin and aspirin. Anatol J Cardiol 16:189–196
Cannon CP et al (2017) Antithrombotic therapy with dabigatran after PCI in atrial fibrillation (RE-DUAL PCI trial). N Engl J Med 377:1516–1524
Lopes RD et al (2019) Antithrombotic therapy after acute coronary syndrome or PCI in atrial fibrillation (AUGUSTUS trial). N Engl J Med 380:1509–1524
Gibson MC et al (2016) Prevention of bleeding in patients with atrial fibrillation undergoing PCI (PIONEER-AF-PCI trial). N Engl J Med 375:2423–2434
Kaatz S et al (2019) Core elements of anticoagulation stewardship programs. Anticoagulation Forum, 1–21
Acknowledgements
Results of this trial were presented at the American Society of Health-System Pharmacists Eastern States Conference, Hershey PA: 2019 as a short platform presentation. A methods poster was presented at the Vizient University Health System Consortium Anaheim, CA: 2018.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This prospective chart review study involving human participants was in accordance with the ethical standards of the institutional and national research committee. The Partners Healthcare Institutional Review Board (IRB) approved this study.
Informed consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zekery-Saad, S.A., Lewin, A., Pham, M. et al. Evaluation and optimization of prescribed concomitant antiplatelet and anticoagulation therapy centrally managed by an anticoagulation management service. J Thromb Thrombolysis 51, 405–412 (2021). https://doi.org/10.1007/s11239-020-02207-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-020-02207-3