Abstract
The efficacy of reperfusion therapy (RT) using intravenous infusion of recombinant tissue plasminogen activator and/or endovascular therapy for minor ischemic stroke (MIS) has not yet been established. The present study aimed to elucidate the clinical features of MIS patients with atrial fibrillation (AF) and examine whether they could be potential candidates for RT. Data of MIS patients, defined as those with a score ≤ 5 on the National Institute of Health Stroke Scale, were extracted from patients admitted to our hospital between 2006 and 2018, and clinical characteristics were compared between the AF and non-AF groups. Thereafter, the impact of RT on outcomes in the AF- group was evaluated using the modified Rankin scale (mRS) score 3 months after onset and compared to that of standard medical therapy (SMT) using propensity score matching (PSM). Of 10,483 stroke patients, 3003 were shortlisted, and 457 AF patients and 2546 non-AF patients were finally selected. Patients in the AF group had more RT (13.3% vs. 5.7%, p < 0.001) than those in the non-AF group. Using PSM, 53 patients each were extracted from the AF-RT and AF-SMT groups. The frequencies of mRS = 0 or 1 for the AF-RT and AF-SMT groups were 69.8% and 64.2% (p = 0.536), respectively, with a significant difference in mRS = 0 (56.5% vs. 34.0%, p = 0.019). The present study found that MIS patients with AF underwent more RT than those without AF and that RT compared favorably with SMT for them; further study is warranted to examine whether these patients could be good candidates for RT.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Highlights
-
The efficacy of reperfusion therapy (RT) for minor ischemic stroke (MIS) is yet to be established.
-
It is not uncommon for MIS patients to present with atrial fibrillation (AF).
-
MIS patients with AF come to the hospital earlier after onset and undergo more RT than those without AF.
-
In MIS patients with AF, RT increased the ratio of best outcome compared to standard medical therapy.
Introduction
There are two established measures of reperfusion therapy (RT) against acute ischemic stroke (AIS). The first is intravenous infusion therapy with recombinant tissue plasminogen activator (iv rt-PA) [1, 2]. The second is endovascular therapy (EVT), the efficacy of which has been proven in patients with AIS using intra-arterial infusion of prourokinase within 6 h of onset [3] and which has been strongly indicated by 5 randomized controlled trials (RCTs) where stent retrievers were used [4]. Furthermore, recent studies have reported the superiority of EVT over standard medical therapy (SMT) beyond 6 h after onset [5, 6]. Based on these results, the present guidelines strongly recommend the use of RTs under certain conditions [7].
Patients with minor ischemic stroke (MIS), defined as those with a National Institute of Health Stroke Scale (NIHSS) score ≤ 5, comprise approximately two-thirds of all patients with AIS [8] and demonstrate unsatisfactory outcomes [9]. However, a meta-analysis could not find significant superiority of iv rt-PA over controls in AIS patients with NIHSS scores ≤ 5 [10]. Regarding the effectiveness of EVT, the present guideline merely describes that the use of mechanical thrombectomy with stent retrievers may be reasonable for patients with AIS with NIHSS scores < 6, although its benefits are unclear [7]. Thus, the efficacy of RT for MIS is yet to be established.
Atrial fibrillation (AF) is a major cause of cardioembolic stroke and is associated with poor prognosis [11]. It is not uncommon for MIS patients to present with AF [12]. We hypothesized that, although not all MIS patients benefit from RT, it provides a better outcome than SMT in patients with AF.
The present study aimed to elucidate the clinical features, frequency of administration of RT, and clinical outcomes in MIS patients with AF compared to those without AF and then examine whether they could be potential candidates for RT.
Methods
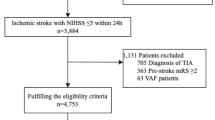
Our hospital consecutively registered stroke patients and followed them up at 3 months after onset by interview or letter between January 2006 and September 2018, after obtaining informed consent from the patients or their families. Patients fulfilling the inclusion criteria shown in Fig. 1 were included in the study.
At first, we divided these patients into 2 groups: those with AF (AF group) and those without AF (non-AF group), and we compared the clinical characteristics, frequency of performed RT, and clinical outcomes. Thereafter, RT (AF-RT group) and SMT (AF-SMT group) patients were selected from the AF group using propensity score matching (PSM), and the clinical outcomes were compared between the 2 groups. The frequency of mRS score of 0–1 (excellent outcome) and mortality at 3 months after onset were defined as primary endpoints. In addition, the frequency of mRS score of 0 at 3 months was defined as the secondary endpoint for the comparison between AF-RT and AF-SMT groups.
AIS was defined as the presence of acute onset of neurological symptoms and detection of the culprit lesion by magnetic resonance imaging (MRI) and, if impossible, by computed tomography (CT). MIS was defined as NIHSS = 0–5. The AF group consisted of patients with AF who were diagnosed before admission or patients in whom AF was detected before discharge. Information on clinical characteristics was obtained from the patients, their families, or, if possible, from their family physician. Additionally, patients were considered as having a past history when their clinical data at admission fulfilled the criteria of hypertension, diabetes mellitus, or dyslipidemia at that time. In cases of unknown onset time of AIS, the last known time at which the patient was well was considered. RT consisted of solo iv rt-PA, solo EVT, or a combination of both; iv rt-PA (0.6 mg/kg) was administered in accordance with the Japanese guidelines of administration within 3 or 4.5 h of stroke onset [13, 14]. EVT was performed with 1 or more combinations of the following procedures: local arterial infusion of urokinase, percutaneous transluminal angioplasty, carotid artery stenting, Merci retriever, Penumbra system, and stent retrievers available at the time of patient admission. Revascularization status was assessed on the final angiogram obtained by the physician-in-charge and an experienced neurosurgeon (S.O.) and was classified according to the modified thrombolysis in cerebral ischemia (mTICI) scale [15]. Successful revascularization was defined as an mTICI scale score of 2b or 3. Symptomatic intracranial hemorrhage (sICH) was defined when worsened NIHSS score and culprit hemorrhagic lesion on CT or MRI were present. A worsened NIHSS score was defined as an increase of more than or equal to 1 point. SMT was performed with antiplatelet and/or anticoagulation therapies at the discretion of the attending physician in accordance with the Japanese guidelines at that time (https://www.jsts.gr.jp). Antiplatelet therapy comprised ozagrel, aspirin, ticlopidine, clopidogrel, and cilostazol. Anticoagulation therapy comprised heparin, argatroban, warfarin, dabigatran, rivaroxaban, apixaban, and edoxaban. ADL, assessed using the mRS score prior to onset, was inferred by conducting a survey with the patients or their families. Interviews or unified questionnaires by letter were used to assess the ADL of the patients at 3 months after onset.
Statistics
The results are presented as medians and quartiles for continuous values unless otherwise stated. Comparisons between 2 groups were performed using the Wilcoxon rank sum test for continuous values and the chi-square test or Fisher’s exact test was used for comparison of proportions. Survival analysis was done using log rank (Mantel-Cox) test. PSM was performed to balance the distribution of variables between the AF-RT and AF-SMT groups. Age, sex, and variables that showed p values < 0.2 between the 2 groups by simple comparison of each clinical characteristic were selected. The AF-SMT group was matched with the AF-RT group with a distribution ratio of 1:1 using the nearest neighbor algorithm with a caliper of 0.02. The data were analyzed using IBM SPSS version 24.0, with p values < 0.05 considered as indicating statistical significance.
Results
Of 10,483 patients with AIS admitted in our hospital, 3003 patients were shortlisted according to the above-mentioned criteria (Fig. 1), comprising 457 patients in the AF group and 2546 in the non-AF group. Comparison of clinical characteristics, frequency of RT, and clinical outcomes between the 2 groups is shown in Table 1. The AF group had a significantly shorter median time from onset to hospital (291 min vs. 469 min, p < 0.001) and more RT (13.3% vs. 5.7%, p < 0.001) than the non-AF group.
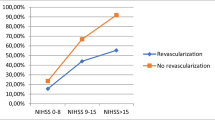
Subjects in the AF group were divided into AF-RT and AF-SMT groups. Comparison of clinical characteristics and frequency of RT between the 2 groups before PSM is shown in Table 2. The selected variables for PSM were sex, hypertension, past history of stroke, time from onset to hospital, and initial NIHSS score. After PSM, each of the 53 patients in the AF-RT and AF-SMT groups were extracted. Table 2 shows the clinical characteristics of patients in both groups after PSM. The status of ADL before stroke onset was identical between the 2 groups: 50 patients of mRS = 0 and 3 patients of mRS = 1. In the AF-RT group, the overall successful revascularization rate by EVT was 62.5%. Two patients in AF-RT group (3.8%) and none in AF-SMT group (0%) had symptomatic ICH, showing no significant difference between 2 groups (p = 0.495). Following RT in the AF-RT group, we initiated antiplatelet therapy in 5 patients (9.4%), anticoagulant therapy in 34 (64.2%), and dual therapies in 10 (18.9%). Conversely, the AF-SMT group consisted of 7 (13.2%), 32 (60.4%), and 7 (13.2%) patients who received antiplatelet therapy, anticoagulation therapy, and dual therapies, respectively. The frequency of any initiated antithrombotic therapies was not significantly different between the 2 groups (p = 0.904). The distribution of mRS scores at 3 months in each group is shown in Fig. 2. An excellent outcome was reported at 3 months in 37 (69.8%) and 34 (64.2%) patients in the AF-RT and SMT groups, respectively, without a significant difference (p = 0.536). However, the AF-RT group had a significantly higher ratio of mRS = 0 than the AF-SMT group (56.6% vs. 34.0%, p = 0.019). Regarding mortality, 4 patients (7.5%) in the AF-RT group and 2 (3.8%) in the AF-SMT group died at 3 months; however, this rate was not significantly different (p = 0.678) between the 2 groups. Survival analysis also showed no significant difference between the 2 groups (p = 0.412).
Comparison of the distribution of mRS scores at 3 months between the AF-RT and AF-SMT groups. AF-RT group had non-significantly higher frequency of mRS = 0–1 (69.8% vs. 64.2%, p = 0.536) than AF-SMT group, but that of mRS = 0 with significant difference (56.5% vs. 34.0%, p = 0.019). The mortality was not significantly different (7.5% vs. 3.8%, p = 0.678). AF atrial fibrillation, mRS modified Rankin scale, RT reperfusion therapy, SMT standard medical therapy
Discussion
The present study found that MIS patients with AF came to the hospital sooner after onset and underwent more RT than those without AF. In the AF group, although the difference in the frequency of an excellent outcome (mRS = 0–1) between RT and SMT was not significant, RT significantly increased the ratio of mRS = 0 compared to SMT.
Refining therapeutic strategy for MIS is very important, considering the high proportion of cases [8] and unsatisfactory outcomes [16]. For AIS patients, the present guidelines strongly recommend the use of RTs under certain conditions [7]. However, a meta-analysis could not find significant superiority of iv rt-PA over the control group in AIS patients with NIHSS scores ≤ 5 [10]. In cases of stroke patients with large vessel occlusion, a meta-analysis did not show significant superiority of combined iv rt-PA + EVT therapy over iv rt-PA therapy for AIS patients with NIHSS scores ≤ 10 [4]. From these studies, it was thought that not all MIS patients, defined as NIHSS score ≤ 5, benefited from RT. A recent study combining two cohorts reported that MIS patients with stroke subtype of large artery atherosclerosis might benefit more from iv rt-PA therapy [17]. In terms of ischemic stroke with AF, it was reported that AF had a significant negative impact on morbidity and mortality in all ischemic stroke [18] and minor stroke, defined as NIHSS score ≤ 3 [19]. In the above-mentioned report [17], the benefit of iv rt-PA therapy in patients with cardioembolism was not demonstrated; however, the number of AF patients in rt-PA and non-rt-PA groups (10 and 21) was too small to evaluate the effectiveness. Therefore, I believe that the present study targeting MIS patients with AF is of significance.
The present study also showed significant higher mortality and a tendency of lower frequency of an excellent outcome among MIS patients with AF than among those without AF. The frequency of AF in MIS patients is not uncommon. Our study showed a frequency of 15.2%, which was comparable to 12.3%, as reported by a registry study in Korea [12]. We observed that MIS patients with AF underwent more RT than those without AF, probably because they come to the hospital sooner after onset. The difference in frequency of an excellent outcome between RT and SMT groups was not significant, while RT significantly increased the frequency of mRS = 0 compared to SMT, suggesting that MIS patients with AF could be good candidates for RT.
There were several limitations to the present study. This was a retrospective study conducted in a single hospital over 13 years, during which therapy for AIS, especially EVT, evolved constantly with time. Despite such a long-term registry, the number of MIS patients who received RT was small, and the clinical characteristics of the AF-RT group were very different at some points from the AF-SMT group before PSM. Because many patients received SMT, extracting matched patients to those with RT was accomplished. At present, we have not been able to obtain sufficient therapeutic decision-making evidence for MIS patients from previous studies. Despite these limitations, however, the results from the present study are clinically relevant.
Conclusion
The present study suggests that RT compares favorably with SMT for MIS patients with AF; however, this should be examined through further studies using new thrombotic agents and devices for EVT.
References
National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group (1995) Tissue plasminogen activator for acute ischemic stroke. N Engl J Med 333:1581–1587
Hacke W, Kaste M, Bluhmki E et al (2008) Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med 359:1317–1329
Furlan A, Higashida R, Wechsler L et al (1999) Intra-arterial prourokinase for acute ischemic stroke. The PROACT II study: a randomized controlled trial. Prolyse in Acute Cerebral Thromboembolism. JAMA 282:2003–2011
Goyal M, Menon BK, van Zwam WH et al (2016) Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet 387:1723–1731
Nogueira RG, Jadhav AP, Haussen DC et al (2018) Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med 378:11–21
Albers GW, Marks MP, Kemp S et al (2018) Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med 378:708–718
Powers WJ, Rabinstein AA, Teri Ackerson T et al (2018) 2018 Guidelines for the early management of patients with acute ischemic stroke. a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 49:e46–e110
Reeves M, Khoury J, Alwell K et al (2013) Distribution of National Institutes of Health stroke scale in the Cincinnati/Northern Kentucky Stroke Study. Stroke 44:3211–3213
Khatri P, Conaway MR, Johnston KC et al (2012) Acute Stroke Accurate Prediction Study (ASAP) Investigators. Ninety-day outcome rates of a prospective cohort of consecutive patients with mild ischemic stroke. Stroke 43:560–562
Yeo LLL, Ho R, Paliwal P et al (2014) Intravenously administered tissue plasminogen activator useful in milder strokes? A meta-analysis. J Stroke Cerebrovasc Dis 23:2156–2162
Steger C, Pratter A, Martinek-Bregel M et al (2004) Stroke patients with atrial fibrillation have a worse prognosis than patients without: data from the Austrian Stroke registry. Eur Heart J 25:1734–1740
Park HK, Kim BJ, Han MK et al (2017) One-year outcomes after minor stroke or high-risk transient ischemic attack: Korean Multicenter Stroke Registry Analysis. Stroke 48:2991–2998
Yamaguchi T, Mori E, Minematsu K et al (2006) Alteplase at 0.6 mg/kg for acute ischemic stroke within 3 hours of onset: Japan Alteplase Clinical Trial (J-ACT). Stroke 37:1810–1815
Minematsu K, Toyoda K, Hirano T et al (2013) Guidelines for the intravenous application of recombinant tissue-type plasminogen activator (alteplase), the second edition, October 2012: a guideline from the Japan Stroke Society. J Stroke Cerebrovasc Dis 22:571–600
Zaidat OO, Yoo AJ, Khatri P et al (2013) Recommendations on angiographic revascularization grading standards for acute ischemic stroke: a consensus statement. Stroke 44:2650–2663
Smith EE, Fonarow GC, Reeves MJ et al (2011) Outcomes in mild or rapidly improving stroke not treated with intravenous recombinant tissue-type plasminogen activator: findings from Get With The Guidelines-Stroke. Stroke 42:3110–3115
Chen W, Pan Y, Zhao X et al (2017) Intravenous thrombolysis in Chinese patients with different subtype of mild stroke: thrombolysis in patients with mild stroke. Sci Rep 23:2299. https://doi.org/10.1038/s41598-017-02579-2
Alkhouli M, Alqahtani F, Aljohani S et al (2018) Burden of atrial fibrillation-associated ischemic stroke in the United States. JACC Clin Electrophysiol 4:618–625
Wu L, Wang A, Wang X et al (2015) Factors for short-term outcomes in patients with a minor stroke: results from China National Stroke Registry. BMC Neurol 15:253. https://doi.org/10.1186/s12883-015-0505-z
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest:
All the authors declared that they have no conflict of interest.
Ethics approval: The study protocol was approved by our institutional review board.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nomura, E., Takemaru, M., Himeno, T. et al. Clinical features and efficacy of reperfusion therapy in minor ischemic stroke patients with atrial fibrillation. J Thromb Thrombolysis 50, 608–613 (2020). https://doi.org/10.1007/s11239-020-02057-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-020-02057-z