Abstract
Few data are available on age-related burden and characteristics of embolic stroke of undetermined source (ESUS) in the real world clinical practice. The aim of our study was to provide information about it. We retrospectively analyzed data of patients consecutively admitted to our Stroke Unit along 1 year (2017, November 1st–2018, October 31st). The etiology of ischemic stroke was defined at hospital discharge; ESUS was considered as a subset of cryptogenic stroke, and defined according to the 2014 international criteria. In the analyzed period, 306 patients, 52.3% females, mean age ± SD 77.9 ± 11.9 years, were discharged with diagnosis of ischemic stroke. Ischemic strokes of cardioembolic and lacunar origin were the most frequent subtypes: 30.1% and 29.4%, respectively. Cardioembolic strokes were particularly frequent in patients ≥ 75 years, and almost always associated with atrial fibrillation. Overall, in 80 patients (26.1%) the etiology of stroke was undetermined; in 25 (8.2%) it remained undefined because of death or severe comorbidity, making further diagnostic work-up not worthy. Cryptogenic stroke occurred in 55 patients (18%), and ESUS criteria were satisfied in 39 of them (12.7%). According to age, cryptogenic stroke was diagnosed in 21.1% (21.1% ESUS) of patients < 65 years, 24.2% (19.4% ESUS) of patients aged 65–74 years, 15.5% (9.2% ESUS) of patients ≥ 75 years. After diagnostic work-up, patent foramen ovale was most commonly associated with ESUS (17.9%), especially in patients < 65 years (62.5%); covert paroxysmal atrial fibrillation was detected in 10.5% of ESUS patients ≥ 75 years. In the real world clinical practice, the frequency of ischemic strokes of undetermined etiology, and of those satisfying ESUS criteria, is not negligible, especially in younger patients. A thorough diagnostic work-up, with an age-specific approach, is therefore necessary and of the utmost importance for the identification of stroke etiology, in order to optimize secondary stroke prevention strategies.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Highlights
-
Defining the etiology of ischemic stroke is of the utmost importance for the appropriate secondary prevention treatment. However, literature evidence shows that in about 25% of cases the etiology remains undetermined.
-
Few data are available on age-related burden and characteristics of embolic stroke of undetermined source (ESUS) in the real world clinical practice.
-
The study provides real world data showing that the frequency of ischemic strokes of undetermined etiology, and of those satisfying ESUS criteria, is not negligible, especially in younger patients.
-
ESUS patients profile seems to be that of relatively young patients with mild strokes, better functional outcome and with lower frequencies of conventional cardiovascular risk factors compared with other ischemic stroke patients.
-
Patent foramen ovale was most commonly associated with ESUS, especially in patients younger than 65 years; covert paroxysmal atrial fibrillation was detected in a not negligible percentage of ESUS patients over 75 years.
-
A thorough diagnostic work-up, with an age-specific approach, is necessary and of the utmost importance for the identification of stroke etiology, in order to optimize secondary stroke prevention strategies.
Introduction
Defining the etiology of ischemic stroke is of the utmost importance for the appropriate acute treatment and secondary prevention. A number of pathophysiologic classifications of ischemic stroke have been proposed [1]; however, the TOAST criteria proposed in 1993 remain those most widely used worldwide [2]. TOAST criteria include extracranial or intracranial large artery atherosclerosis, small vessel occlusion, cardioembolism, other determined etiology and undetermined (cryptogenic) etiology subtypes of ischemic stroke [2]. The undetermined etiology includes three scenarios: (i) the diagnostic assessment is not performed or incomplete; (ii) two or more etiologies are plausible); (iii) no cause is found despite an extensive assessment [2].
Cryptogenic stroke encompasses for about 25% of ischemic strokes. Literature evidence demonstrates that most cryptogenic strokes have an embolic source; therefore, in 2014 a new clinical construct, embolic stroke of undetermined source (ESUS), has been proposed [3]. ESUS refers to non lacunar stroke detected by brain computer tomography (CT) or magnetic resonance (MR), in the absence of extracranial or intracranial atherosclerosis causing more than 50% luminal stenosis in arteries supplying the ischemic area, major risk cardioembolic sources, or any other specific cause of stroke, such as arteritis, dissection, migraine/vasospasm, drug abuse [3]. Therefore, the proposed minimal diagnostic approach for ESUS definition is represented by brain CT or MR, trans-thoracic echocardiography, electrocardiographic monitoring for at least 24 hours, imaging of both the extracranial and intracranial arteries supplying the area of brain ischemia [3]. Recently, Hart RG et al. performed a systematic review and meta-analysis of literature evidence on ESUS [4]. The Authors found that the prevalence of ESUS ranges from 9 to 25% of ischemic strokes, the mean age of patients suffering from ESUS is 65 years, and about 40% of patients are females; the majority of patients are treated by antiplatelets drugs, and incidence of stroke recurrence is 4.5% per year during a mean follow up of 2.7 years [4].
The aim of our study was to analyze the age-related burden and characteristics of ESUS in the real world clinical practice.
Materials and methods
We retrospectively analyzed data of patients consecutively admitted to the Stroke Unit of San Giuseppe Hospital, Empoli, Florence, Italy, along 1 year (2017, November 1st–2018, October 31st).
For all the patients the etiology of ischemic stroke was defined referring to categories identified by TOAST classification [2]. ESUS was considered as a subset of cryptogenic stroke, and defined according to the 2014 international criteria [3]. A stroke was considered of cardioembolic origin when a “major-risk” cardioembolic source of embolism was identified [3]. Standard first level diagnostic methods for determining ischemic stroke etiology included: brain CT or MR, vascular study of extra- and intracranial vessels (with cervical arteries and trans-cranial Doppler ultrasonography, or with CT/MR angiography), electrocardiographic monitoring for at least 24 hours, and trans-thoracic echocardiography. All these investigations were performed during hospital stay in Stroke Unit or in any case completed within the first 2 weeks after the index event for those patients who were then admitted to rehabilitation care settings. The etiology of ischemic stroke was therefore defined at the time of discharge. After this standard diagnostic evaluation, patients satisfying ESUS criteria underwent further investigations for etiologic definition, including trans-cranial Doppler for right-to-left shunt evaluation and/or trans-esophageal echocardiography, prolonged (i.e. 15 days) electrocardiographic monitoring with external and/or implantable loop recorder, and thrombophilia screening or other laboratory tests, as deemed appropriate by the treating physician. Paroxysmal atrial fibrillation (AF) detected on cardiac monitoring was defined as an episode of irregular heart rhythm, without detectable P waves, of any duration.
Patients were followed-up at 90 days by a scheduled clinical visit, in order to complete the diagnostic work-up when appropriate, and to assess outcomes and disability. Outcomes at 90 days were recurrent ischemic stroke, transient ischemic attack (TIA) or systemic embolism, and major intracranial or extracranial bleeding. Ischemic stroke was defined as the sudden onset of a new focal neurological deficit of vascular origin in a site consistent with the territory of a major cerebral artery with acute infarction. TIA was defined as a transient episode of neurological dysfunction caused by focal brain ischemia without acute infarction. Systemic embolism was defined as an acute vascular occlusion of an extremity or organ confirmed by imaging. Major bleeding was defined as a fatal bleeding or a symptomatic bleeding in a critical area or organ, a reduction in the hemoglobin level of at least 2 g/dL or requiring blood transfusion of at least 2 units [5]. Disability and mortality at 90 days were also assessed using the modified Rankin Scale (mRS).
For all patients satisfying cryptogenic stroke and ESUS criteria, data on demographic, clinical [including cardiovascular risk factors, comorbidities, National Institutes of Health Stroke Scale (NIHSS)], neuroradiological, and instrumental characteristics of patients and index events, information on acute phase and secondary prevention treatments, and 90-day outcomes and disability were recorded. The analysis was conducted first on the entire population of patients with cryptogenic stroke and ESUS, and, thereafter, on subgroups of patients according to age: < 65, between 65 and 74, ≥ 75 years.
The size of ischemic lesions was classified as small, when < 1.5 cm in the anterior or posterior circulation; medium, when a lesion was in a cortical superficial branch of middle cerebral artery (MCA), in the MCA deep branch, in the internal border zone territories, in a cortical superficial branch of posterior cerebral artery (PCA), in a cortical superficial branch of the anterior cerebral artery (ACA); large anterior, when a lesion involved the complete territory of MCA, PCA, or ACA, in 2 cortical superficial branches of MCA, in a cortical superficial branch of MCA associated to the MCA deep branch, or in more than 1 artery territory (e.g., MCA associated to ACA territories); large posterior, when a lesion was ≥ 1.5 cm in the brain stem or cerebellum [6, 7].
Statistical analysis
Continuous variables were expressed as mean ± standard deviation (SD) or median and interquartile range (IQR), as appropriate. Categorical variables were presented as counts and percentages. Comparisons between groups (ESUS according to age) were performed using ANOVA test or Kruskal–Wallis test, as appropriate. A p value of < 0.05 was considered statistically significant. All analyses were performed using the SPSS software package version 20 (Statistical Package for Social Sciences, Chicago, Illinois, USA).
Results
Demographic characteristics of patients and etiopathogenesis of ischemic strokes
In the analyzed period, 306 patients, 52.3% females, mean age ± SD 77.9 ± 11.9 years, were discharged from our Stroke Unit with diagnosis of ischemic stroke.
Age distribution was: 12.4% of patients < 65 years, 20.3% between 65 and 74 years, and 67.3% ≥ 75 years.
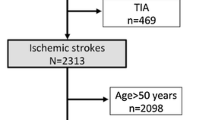
Figures 1 and 2 show the etiologic distribution of strokes in the entire cohort of patients and according to age, respectively.
Ischemic strokes of cardioembolic and lacunar origin were the most frequent subtypes: 30.1% and 29.4%, respectively. Cardioembolic strokes were particularly frequent in patients aged ≥ 75 years (37.9%), and almost always associated with AF.
Overall, in 80 patients (26.1%) the etiology of stroke was undetermined. In 25 patients (8.2%) it remained undefined because of death or severe co-morbidity, making further diagnostic work-up not worthy. Among patients with undefined etiology, 80% were aged ≥ 75 years. Cryptogenic stroke occurred in 55 patients (18%), and ESUS criteria were satisfied in 39 of them (12.7%).
According to age, cryptogenic stroke was diagnosed in 21.1% (21.1% ESUS) of patients < 65 years, 24.2% (19.4% ESUS) of patients between 65 and 74 years, and 15.5% (9.2% ESUS) of those ≥ 75 years.
Characteristics of patients with cryptogenic stroke and ESUS
Baseline characteristics of patients with cryptogenic stroke, and of the subgroup of patients satisfying ESUS criteria are reported in Table 1.
More than 50% of patients were males. Twenty percent of patients with cryptogenic stroke had a history of previous stroke/TIA, 62% had non hemodynamic carotid atherosclerosis. Left atrial enlargement was detected on echocardiography in 21.8% of cryptogenic stroke (17.9% of ESUS) patients. Median CHA2DS2-VASc score value was 3.
About 62% of patients did not assume any antithrombotic therapy before the index event, whereas about 33% was on single antiplatelet therapy.
Characteristics and data on acute and long-term treatment of the index event in patients with cryptogenic stroke and ESUS are reported in Table 2.
Median NIHSS at hospital admission was 2 (IQR 1–6) in patients with cryptogenic stroke, and 3 (IQR 1–6) in those with ESUS. Eighty percent of patients with cryptogenic stroke (76.9% of ESUS) had ischemic lesions in the anterior circulation territories, with cortical-subcortical pattern in about 69% of cases. Moreover, about 50% of patients with ESUS had multiple ischemic lesions.
Eighty percent of patients was discharged on single antiplatelet therapy.
Median hospital stay duration was 6 days. No patient died during hospital stay. Median mRS at discharge was 3.
Characteristics of ESUS patients according to age
Baseline characteristics of patients, characteristics and data on acute and long-term treatment of the index event in ESUS patients according to age are reported in Tables 3 and 4.
Among the 39 patients with ESUS age distribution was: 8 patients (20.5%) < 65 years, 12 patients (30.8%) between 65 and 74 years, and 19 patients (48.7%) ≥ 75 years.
Male sex was prevalent among patients aged < 65 years and among those aged between 64 and 74 years (62.5% and 66.7%, respectively), whereas patients ≥ 75 years were more frequently females (57.9%).
As regards cardiovascular risk factors and comorbidities, a significantly higher frequency of non hemodynamic carotid atherosclerosis was found in patients aged between 65 and 74 years in comparison with the other age groups (p = 0.035); prevalence of cardiovascular risk factors was lower in patients < 65 years, even if the difference was not statistically significant in comparison with the others.
ESUS patients aged ≥ 75 years, compared to the other age groups, had a higher prevalence of left atrial enlargement, and a significantly higher median value of CHA2DS2-VASc score (p < 0.001).
In patients with ESUS aged < 65 years there was a significantly higher prevalence of posterior lesions (62.5%) in comparison with the others (p = 0.006).
Potential sources of thromboembolism associated with ESUS
Potential sources of thromboembolism associated with ESUS are reported in Table 5.
Patent foramen ovale was most commonly associated with ESUS (17.9%), especially in patients aged < 65 years (62.5%). Covert paroxysmal AF was detected at prolonged electrocardiographic monitoring in 10.5% of ESUS patients aged ≥ 75 years.
In 41% of patients with ESUS the source of embolism remained undefined: in 15.4% of patients it remained undefined despite diagnostic investigations including at least prolonged electrocardiographic monitoring and trans-esophageal echocardiography; in 25.6% for incomplete diagnostic work-up due to death, patient refuse or starting of anticoagulant therapy for reasons other than stroke.
In 28.2% of patients the diagnostic work-up of ESUS is still underway.
The percentage of patients in whom the source of embolism associated with ESUS remained undefined was higher in those aged between 65 and 74 years and ≥ 75 years.
Ninety-day follow-up
Among patients with cryptogenic stroke, at 90-day follow-up, one patient died, one (ESUS) had ischemic stroke recurrence, and 2 (both ESUS) had major bleeding complications. Median 90-day mRS was 1.
Data on adverse events and residual disability at 90-day follow-up, in patients with cryptogenic stroke and ESUS, and in ESUS patients according to age, are shown in Table 6.
Discussion
Despite advances in diagnostic techniques allowing a better understanding of the pathogenetic mechanisms of ischemic stroke, the identification of stroke etiology remains a challenge in everyday clinical practice. The percentage of ischemic strokes of undefined etiology at the time of hospital discharge is still very high; this could be partly justified by the high average age of many patients, often associated with severe residual disability; however, it should be recognized that a not negligible proportion of patients, even the youngest ones, doesn’t undergo comprehensive investigations for etiological definition [4]. A thorough diagnostic work-up is necessary and of the utmost importance for the identification of stroke etiology, in order to optimize secondary prevention strategies and reduce the risk of recurrence.
In our study, we conducted a retrospective analysis on 306 consecutive patients with diagnosis of ischemic stroke, admitted to the Stroke Unit of a first level Italian hospital, in order to evaluate the epidemiology of different stroke etiopathogenetic subtypes, and the burden and characteristics of cryptogenic stroke and ESUS according to age.
A high frequency of ischemic strokes of cardioembolic and lacunar origin, and, in particular, of AF-related cardioembolic strokes in patients older than 75 years was found. These data are in agreement with the most recent epidemiological estimates (years 2013–2014) produced from a global registry encompassing 19 stroke centers from 19 countries worldwide which has shown a reduction in the occurrence of large artery atherosclerosis-related strokes, and, on the other side, an increased frequency of strokes of cardioembolic origin (about 30%) compared with the past decades in which the burden of cardioembolic strokes was 20% [8].
In our study the frequency of ischemic strokes of undetermined etiology, classified as cryptogenic, was not negligible, approximately 18% of cases; of these, 13% met the classification criteria for ESUS, after standard diagnostic investigations including at least vascular study of extra- and intracranial vessels, electrocardiographic monitoring for at least 24 hours, and trans-thoracic echocardiography for exclusion of major cardioembolic sources.
In agreement with literature data [4, 9], in our study the mean age of ESUS patients was lower than that of the whole cohort of ischemic strokes, and the diagnosis of ESUS was more frequent in patients younger than 65 years, in whom a lower prevalence of traditional cardiovascular risk factors was also observed. Male sex was prevalent in ESUS patients younger than 75 years, while older patients were mostly of female sex, as the whole cohort of ischemic strokes. The lower mean age of ESUS patients may reflect incomplete diagnostic investigation of older stroke patients that allows the diagnosis of ESUS. Indeed, in our study, in the 8.1% of patients with ischemic stroke, the etiopathogenesis remained undefined, due to death or to the presence of severe comorbidity or disability, making further diagnostic investigations not favorable in terms of cost-effectiveness; the 80% of these patients were over 75 years of age.
Another interesting finding of our study concerns clinical severity and neuroradiological characteristics of ischemic lesions in ESUS patients. The median NIHSS value at admission was found to be low, thus suggesting strokes of mild clinical severity. Ischemic lesions involved the anterior circulation in about 80% of cases (with the exception of ESUS patients younger than 65 years, in whom a significant higher prevalence of ischemic lesions involving the posterior circulation was found), and had a cortical-subcortical distribution in about 70% of cases; moreover, more than half of patients with ESUS had multiple ischemic lesions. A large vessel occlusion was found in less than 13% of patients. These clinical and neuroradiological features fit the hypothesis that ESUS is usually caused by relatively smaller emboli from valvular and arterial sources rather than larger emboli originating in the cardiac chambers, such as left atrial appendage thrombi in patients with AF, embolizing to cause large, disabling strokes [4, 9]. Therefore, ESUS patients profile seems to be that of relatively young patients with mild strokes and with lower frequencies of conventional cardiovascular risk factors compared with non-ESUS ischemic stroke patients.
From a prognostic point of view, ESUS seems to be characterized by a lower long-term mortality rate and a better functional outcome compared with cardioembolic strokes, but the recurrence rate is high despite therapy, and probably higher than other ischemic stroke subtypes [4, 10]. Due to the small sample size and the short length of follow-up, our study does not allow an appropriate estimate on short- and long-term mortality and recurrence rates. No deaths occurred during hospitalization or during the 90-day follow-up in ESUS patients; recurrence of ischemic stroke was observed in one patient older than 65 years. As regards residual disability, the median mRS value of ESUS patients was 3 (moderate disability) at discharge, and 1 (non-significant disability) at 90-day follow up, with no significant differences among age subgroups. This suggests a better functional outcome in patients with ESUS compared to other stroke etiopathogenetic subtypes. Lower age and less severe disability should encourage clinicians to look for ESUS etiology, in order to optimize treatment and minimize the risk of recurrence, an event that could significantly impact on the quality of life and subsequent prognosis of these patients.
The second part of our study focused on results of second level diagnostic examinations carried out in ESUS patients to identify embolic sources of ESUS, in order to define a possible diagnostic work-up to be used in everyday clinical practice. Patent foramen ovale was most commonly associated with ESUS (in about 18%), especially in patients younger than 65 years (62.5%), consistently with literature data. In a diagnostic pathway optimizing resources with diagnostic possibilities, this could imply that the search for a patent foramen ovale should be the first step in patients under 65 years, with cardiac monitoring for paroxysmal AF to be considered only after the presence of a patent foramen ovale has been excluded. Covert paroxysmal AF was the most frequent source of embolism associated with ESUS (10.5%) in patients over 75 years, thus suggesting the search for AF as first diagnostic investigation in this age subgroup. This is also supported by the fact that a higher frequency of left atrial enlargement and a significantly higher median value of CHA2DS2-VASc score were found in older ESUS patients, both considered as possible predictors of thromboembolic risk despite the absence of documented AF. These observations are in line with recent evidences that point out the so called “atrial cardiopathy” and its biomarkers, rather than AF itself, as direct causes of cardioembolic ischemic events [11]; indeed, subclinical AF episodes are predictive of ischemic stroke and systemic embolism risk without a precise temporal correlation with the occurrence of the embolic complication. This lack of temporal correlation between subclinical AF and the embolic event suggested the hypothesis that AF itself represents a marker of “atrial dysfunction”, or “atrial cardiopathy”, rather than the direct cause of thromboembolic complications. Growing evidence exists on the association between markers of “atrial dysfunction/cardiopathy” (including left atrial enlargement) and ischemic stroke regardless of the presence of AF [11,12,13,14,15]. Recently, a score, aimed at estimating the likelihood of documenting subclinical AF on prolonged cardiac monitoring in patients suffering from ESUS, has also been developed, the so called Brown ESUS-AF score [16], which includes age and left atrial enlargement as predictive variables. The percentage of detected AF ranged from 4.2% in patients with score 0 to 55.6% in patients with score 4. The predictive power of this score is high, with an area under the curve of 0.726. Finding AF would allow to introduce anticoagulant therapy, in the majority of cases with direct oral anticoagulants (DOACs), which have shown to be effective and safe in real life, even in the acute phase of AF-related ischemic stroke [17].
However, despite diagnostic investigations, the percentage of patients with ESUS in whom the embolic source remained undefined was not negligible (41%) in our study. In more than 25% of cases, the initially planned diagnostic work-up was not completed, due to patient refusal or to clinical decision to undertake a specific secondary prophylaxis strategy (i.e. oral anticoagulant therapy), deemed appropriate regardless of the possible outcome of etiological investigations. Once again, the percentage of cases with undefined etiology was higher in the older age groups. These observations reinforce the need for a well-structured diagnostic pathway for ESUS etiology definition, with a differential approach based on age and clinical characteristics of patients, in order to optimize its cost-effectiveness, since the often limited availability of diagnostic resources. Figure 3 shows the diagnostic algorithm adopted in our clinical practice.
Finally, as regards secondary prevention antithrombotic strategies in patients with ESUS, approximately 80% of our patients was discharged on antiplatelet monotherapy; this percentage is in line with that recently reported by Hart RG et al. [4]. Currently, limited data are available to guide treatment decisions in patients with ESUS; no therapies have been specifically tested in randomized trials in patients with ESUS to prevent ischemic stroke recurrence. Antiplatelet therapy is the current standard treatment for secondary stroke prevention; however, emerging evidence suggests that anticoagulation may reduce the risk of recurrent stroke in ESUS patients, even in those who do not have documented AF [18, 19]. DOACs could represent a new therapeutic perspective in patients with ischemic stroke of undetermined origin, in which an embolic source is more probable. Two randomized clinical trials comparing DOACs with antiplatelet therapy for the prevention of stroke recurrence in patients with ESUS have been recently published, and others are currently underway [20,21,22,23]. The NAVIGATE ESUS trial, comparing the efficacy and safety of rivaroxaban 15 mg OD with aspirin, was terminated early at a pre-defined interim analysis owing to increased bleeding in the rivaroxaban arm without the benefit of lower risk of stroke/systemic embolism [20]. However, a subgroup analysis of this study showed that, in patients with ESUS who have patent foramen ovale, anticoagulation might reduce the risk of recurrent stroke by about half [24]. Moreover, in a secondary analysis of the trial, aimed at analyzing the efficacy of rivaroxaban among patients with ESUS at increased risk of AF, rivaroxaban was associated with a reduced risk of recurrent stroke among patients with ESUS and moderate or severe left atrial enlargement compared with aspirin [25]. The recently published RE-SPECT ESUS trial, evaluating dabigatran 150 or 110 mg BID versus aspirin, showed that dabigatran was not superior to aspirin in preventing recurrent stroke; the incidence of major bleeding was not greater in the dabigatran group than in the aspirin group, but there were more clinically relevant non major bleeding events in the dabigatran group. A higher efficacy of dabigatran compared with aspirin in preventing recurrent stroke was observed in the subgroup of patients older than 75 years [21]. Finally, the ARCADIA trial, which began enrolling patients in January 2018, is evaluating apixaban 5 mg BID versus aspirin in patients with a recent cryptogenic stroke and evidence of atrial cardiopathy [23], and could therefore add important information for the clinical management of these subgroup of patients with ESUS.
We are aware that our study has some limitations, including the single-center retrospective design, the small sample size and the short length of follow-up; therefore, the results may be not generally applicable, and the study is not powered enough for estimating outcomes. However, patients were consecutively enrolled, and reflect a real-world unselected population of ischemic stroke patients.
Conclusion
In our clinical practice, ischemic strokes of cardioembolic and lacunar origin were the most frequent stroke subtypes, with a particularly high frequency of AF-related ischemic stroke in patients over 75 years. The frequency of strokes of undetermined etiology, and of those satisfying ESUS criteria, was not negligible, especially in patients under 65 years. A thorough diagnostic work-up, with an age-specific approach, is therefore necessary and of the utmost importance for the identification of ischemic stroke etiology, in order to optimize secondary stroke prevention strategies and reduce the risk of recurrence.
References
Chen PH, Gao S, Wang YJ et al (2012) Classyfing ischemic stroke, from TOAST to CISS. CNS Neurosci Ther 00:1–5. https://doi.org/10.1111/j.1755-5949.2011.00292.x
Adams HP Jr, Bendixen BH, Kappelle LJ et al (1993) Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke 24:35–41
Hart RG, Diener HC, Coutts SB, for the Cryptogenic Stroke/ESUS International Working Group et al (2014) Embolic strokes of undetermined source: the case for a new clinical construct. Lancet Neurol 13:429–438. https://doi.org/10.1016/S1474-4422(13)70310-7
Hart RG, Catanese L, Perera KS et al (2017) Embolic stroke of undetermined source. A systematic review and clinical update. Stroke 48:867–872. https://doi.org/10.1161/STROKEAHA.116.016414
Schulman S, Kearon C, Subcommittee on Control of Anticoagulation of the Scientific and Standardization Committee of the International Society on Thrombosis and Haemostasis (2005) Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non-surgical patients. J Thromb Haemost 3:692–694. https://doi.org/10.1111/j.1538-7836.2005.01204.x
Tatu L, Moulin T, Bogousslavsky J et al (1996) Arterial territories of the human brain: brainstem and cerebellum. Neurology 47:1125–1135
Tatu L, Moulin T, Bogousslavsky J et al (1998) Arterial territories of the human brain: cerebral hemispheres. Neurology 50:1699–1708
Perera KS, Vanassche T, Bosch J, Global Registry Investigators ESUS et al (2016) Global survey of the frequency of atrial fibrillation associated stroke: embolic stroke of undetermined source global registry. Stroke 47:2197–2202. https://doi.org/10.1161/STROKEAHA.116.013378
Perera KS, Vanassche T, Bosch J et al (2016) Embolic strokes of undetermined source: prevalence and patient features in the ESUS Global Registry. Int J Stroke 11:526–533. https://doi.org/10.1177/1747493016641967
Ntaios G, Papavasileiou V, Milionis H et al (2015) Embolic strokes of undetermined source in the Athens stroke registry: an outcome analysis. Stroke 46:2087–2093. https://doi.org/10.1161/STROKEAHA.115.009334
Van Gelder IC, Healey JS, Crijns HJGM et al (2017) Duration of device-detected subclinical atrial fibrillation and occurrence of stroke in ASSERT. Eur Heart J 38:1339–1344. https://doi.org/10.1093/eurheartj/ehx042
Glotzer TV, Daoud EG, Wyse DG et al (2009) The relationship between daily atrial tachyarrhythmia burden from implantable device diagnostics and stroke risk: the TRENDS study. Circ Arrhythm Electrophysiol 2:474–480. https://doi.org/10.1161/CIRCEP.109.849638
Martin DT, Bersohn MM, Waldo AL et al (2015) Randomized trial of atrial arrhythmia monitoring to guide anticoagulation in patients with implanted defibrillator and cardiac resynchronization devices. Eur Heart J 36:1660–1668. https://doi.org/10.1093/eurheartj/ehv115
Goette A, Kalman JM, Aguinaga L et al (2016) EHRA/HRS/APHRS/SOLAECE expert consensus on atrial cardiomyopathies: definition, characterization, and clinical implication. Europace 18:1455–1490. https://doi.org/10.1093/europace/euw161
Guichard J-B, Nattel S (2017) Atrial cardiomyopathy: a useful notion in cardiac disease management or a passing fad? J Am Coll Cardiol 70:756–765. https://doi.org/10.1016/j.jacc.2017.06.033
Ricci B, Chang AD, Hemendinger M et al (2018) A simple score that predicts paroxysmal atrial fibrillation on outpatient cardiac monitoring after embolic stroke of unknown source. J Stroke Cerebrovasc Dis 27:1692–1696. https://doi.org/10.1016/j.jstrokecerebrovasdis.2018.01.028
Masotti L, Grifoni E, Dei A et al (2019) Direct oral anticoagulants in the early phase of non valvular atrial fibrillation-related acute ischemic stroke: focus on real life studies. J Thromb Thrombolysis 47:292–300. https://doi.org/10.1007/s11239-018-1775-2
Hankey GJ (2002) Warfarin-Aspirin Recurrent Stroke Study (WARSS) trial: is warfarin really a reasonable therapeutic alternative to aspirin for preventing recurrent noncardioembolic ischemic stroke? Stroke 33:1723–1726
Sacco RL, Prabhakaran S, Thompson JLP et al (2006) Comparison of warfarin versus aspirin for the prevention of recurrent stroke or death: subgroup analyses from the Warfarin-Aspirin Recurrent Stroke Study. Cerebrovasc Dis 22:4–12. https://doi.org/10.1159/000092331
Hart RG, Sharma M, Mundl H et al (2018) Rivaroxaban for stroke prevention after embolic stroke of undetermined source. N Engl J Med 378:2191–2201. https://doi.org/10.1056/NEJMoa1802686
Diener HC, Sacco RL, Easton JD, RE-SPECT ESUS Steering Committee and Investigators et al (2019) Dabigatran for prevention of stroke after embolic stroke of undetermined source. N Engl J Med 380:1906–1917. https://doi.org/10.1056/NEJMoa1813959
Geisler T, Poli S, Meisner C et al (2017) Apixaban for treatment of embolic stroke of undetermined source (ATTICUS randomized trial): rationale and study design. Int J Stroke 12:985–990. https://doi.org/10.1177/1747493016681019
Kamel H, Longstreth WT, Tirschwell DL et al (2019) The atrial cardiopathy and antithrombotic drugs in prevention after cryptogenic stroke randomized trial: rationale and methods. Int J Stroke 14:207–214. https://doi.org/10.1177/1747493018799981
Kasner SE, Swaminathan B, Lavados P et al (2018) Rivaroxaban or aspirin for patent foramen ovale and embolic stroke of undetermined source: a prespecified subgroup analysis from the NAVIGATE ESUS trial. Lancet Neurol 17:1053–1060. https://doi.org/10.1016/S1474-4422(18)30319-3
Healey JS, Gladstone DJ, Swaminathan B et al (2019) Recurrent stroke with rivaroxaban compared with aspirin according to predictors of atrial fibrillation: secondary analysis of the NAVIGATE ESUS Randomized clinical trial. JAMA Neurol. https://doi.org/10.1001/jamaneurol.2019.0617
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Grifoni, E., Giglio, D., Guazzini, G. et al. Age-related burden and characteristics of embolic stroke of undetermined source in the real world clinical practice. J Thromb Thrombolysis 49, 75–85 (2020). https://doi.org/10.1007/s11239-019-01951-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-019-01951-5