Abstract
Venous thromboembolism (VTE) remains the number one preventable cause of hospital acquired mortality and morbidity. Each year, more than 12 million patients are at risk for VTE. The delivery of appropriate and timely VTE prophylaxis is still suboptimal in many healthcare institutions and can lead to increased readmissions, morbidity, as well as costs. To clarify this issue further, we performed a retrospective case control study at our institution to determine if poor adherence to the VTE prophylaxis guidelines could lead to an increase in VTE events. This was a retrospective case control study conducted at Winthrop-University Hospital from January 2007 to December 2011. Exclusion criteria were age < 18 and concurrent use of anticoagulant agents. Out of 322 cases of hospital acquired VTE or readmission with VTE within 30 days of discharge, 289 cases were selected for final analysis and paired with age and sex matched controls. Patients with a hospital acquired VTE or a readmission for VTE within 30 days of discharge had a significantly reduced rate of VTE prophylaxis when compared to the control group (54.0 vs. 79.2 %, p < 0.0001). The VTE risk assessment rate was also lower in the VTE group (77.2 vs. 85.5 %, p = 0.035). No difference was noted in the time to prophylaxis administration between the two groups (34.8 vs. 33.1 h, p = 0.34). Lastly, sequential compression device (SCD) documentation rate was not different: 68/116 (58.6 %) vs. 44/87 (50.6 %), p = 0.32, between the two arms. Low adherence to the American College of Chest Physician (ACCP) guidelines for VTE prophylaxis correlated with an increase in hospital acquired VTE. The decreased adherence may be linked to a lower VTE risk assessment rate, and other barriers including incorrect identification of contraindications to pharmacologic prophylaxis, and poor documentation of mechanical prophylaxis. There was no difference in SCD documentation rate and timeliness to administration of initial thromboprophylaxis between the two groups. Future studies are needed to reassess adherence and documentation rates after system-wide improvements.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Venous thromboembolism (VTE) remains the number one preventable cause of hospital-acquired morbidity and mortality [1]. Each year, more than 12 million hospitalized patients are at risk for VTE [2]. In the United States of America (USA), medical costs related to an acute VTE is estimated to be around $33,000, over 1 year per case [3]. Additionally, complications such as recurrent VTE, post-thrombotic syndrome, bleeding, and heparin-induced thrombocytopenia add to this economic burden [3–5].
In an attempt to mitigate morbidity, mortality, and medical costs related to thromboembolic disease, evidence-based guidelines were published for prevention of VTE [6]. Effective prophylaxis requires prompt administration of the proper prophylactic agent(s), based on the patient’s risk factors for VTE, weighted against their bleeding risk. Attention to adequate dosing and appropriate duration of prophylaxis is also necessary. Despite efforts to enforce these guidelines, studies have consistently shown very poor rates of adherence towards VTE prophylaxis [7, 8]. The IMPROVE trial demonstrated that, only 60 % of 15,156 medical patients from 12 countries meeting the American College of Chest Physicians (ACCP) criteria for VTE prophylaxis actually received it [9]. The ENDORSE study involving 35,329 patients across 32 countries reported that only 58.5 % of surgical patients and 38.5 % medical patients meeting ACCP guidelines were administered VTE prophylaxis [10].
Immobility is a widely-recognized risk factor for VTE. In elderly hospitalized patients with risk factors for thromboembolic disease, even short periods of immobilization can predispose to VTE [11]. Hence, delays in inpatient prophylaxis administration may correlate with increased VTE events. To examine this, we designed a case control study to evaluate the appropriateness and timeliness of initial thromboprophylaxis in patients admitted between January 2007 and December 2011, who sustained a documented hospital-acquired VTE, or were readmitted for a VTE within 30 days of discharge.
Materials and methods
Study design
This study was undertaken at Winthrop-University Hospital, a 591-bed university affiliated teaching hospital. All cases of hospital acquired (symptomatic and asymptomatic) VTE or readmissions with VTE within 30 days of discharge between January 2007 and December 2011 were identified retrospectively. Hospital acquired VTE was defined as VTE diagnosed objectively by doppler ultrasound, ventilation/perfusion lung scan and/or computed tomographic pulmonary angiography (CTPA) in patients initially admitted with signs and symptoms not suggestive of VTE. Patients were stratified according to VTE risk categories based on the 8th edition of the ACCP guidelines and evaluated for appropriateness of VTE prophylaxis on admission. Cases were classified as having low risk, moderate risk or high risk for VTE according to published data on the rate of DVT prevalence observed in each patient group, and further subcategorized based on additional risk factors and bleeding risk as per the ACCP guidelines [12]. Utilizing the same guidelines, every effort was made to match control cases from admissions in 2011 to the VTE cases by age, gender and VTE risk category. The protocol and study design was approved by the institutional review board (IRB) and the ethics committee.
Study population
The study included all patients ≥ 18 years of age, who had an objectively confirmed pulmonary embolism (PE) or deep venous thrombosis (DVT), while hospitalized. Patients who were re-hospitalized due to VTE within 30 days of discharge were identified using diagnosis codes and included in our study. Patients already on therapeutic anticoagulation or initiated on therapeutic anticoagulation immediately at admission were excluded from the study.
Outcomes
Primary outcome for the study was to determine whether low adherence to the ACCP guidelines for VTE prophylaxis lead to increased VTE events. Secondary outcomes included rate of risk assessment for VTE, time to initial VTE prophylaxis administration, and documentation rate of mechanical VTE prophylaxis.
Data collection
Data was collected from electronic medical records and chart review. Appropriateness of VTE prophylaxis was defined by ACCP guidelines and considered acceptable only when administered and documented within the first 24 h of admission. Dosages and types of VTE prophylaxis, contraindications for VTE prophylaxis, along with risk factors associated with VTE were collected. Patient refusal of VTE prophylaxis was also documented. Patients that did not receive VTE prophylaxis despite a physician order, were classified as intention to prophylax. Rate of risk assessment was calculated via recording of attestation on departmental specific VTE risk assessment forms by the admitting physician. Documentation of mechanical prophylaxis was deemed sufficient only when documented on nursing records.
Statistical analysis
A sample size of 251 cases per arm was deemed necessary to satisfy a power of 95 % with an α value of 0.05. Rate of VTE prophylaxis administration was estimated at 60 % in the VTE arm and 75 % in the control arm. These estimates were extrapolated from earlier unpublished data, from a 1 year pilot study. Approximately 50 cases of hospital acquired VTE occurred in 1 year, thus it was estimated that 5-years of data was necessary to acquire the required sample size.
Statistical analysis were performed using Chi square test for categorical variables and two tailed t test for continuous variables. Statistical significance was considered at p values <0.05. All calculations were performed on GraphPad InStat (GraphPad Software Inc, La Jolla CA USA).
Results
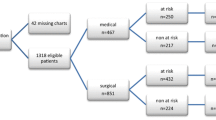
322 cases of hospital acquired VTE or readmissions for VTE within 30 days were identified between January 2007 and December 2011. One case was excluded due to age and two cases due to missing data. 30 patients were excluded either secondary to pre-existing use of therapeutic anticoagulation or its immediate administration upon admission. Therefore, 289 cases were eligible for analysis, and control cases were matched against these cases and stratified by age, gender, and risk category (Table 1). Demographic attributes including age (p = 0.68) and sex (p = 0.70) were adequately matched.
Significantly fewer patients with a hospital acquired VTE or a 30 day readmission with VTE were administered prophylaxis when compared to controls (54.0 vs. 79.2 %, p < 0.0001) (Table 1). There was also a significant difference in the VTE risk assessment rate between the VTE and the control arms (77.2 vs. 85.5 %, p = 0.035).
Despite differences in appropriateness or rate of prophylaxis assessment, no difference was noted from time of presentation in the emergency department (ED) to prophylaxis administration between the two groups (34.8 vs. 33.1 h, p = 0.34). Finally, sequential compression device (SCD) documentation rate was not different between the VTE and control groups; 68/116 (58.6 %) and 44/87 (50.6 %) respectively (p = 0.32) (Table 1).
Post-hoc subset analysis
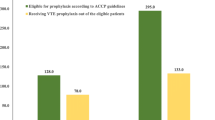
Thromboprophylaxis adherence rates by subgroup are depicted in Fig. 1. There was no statistically significant difference between the different risk groups except for the cardiothoracic group. In the cardiothoracic group, appropriate VTE prophylaxis was administered in 7.7 % of the cases who subsequently sustained a VTE, well below the composite rate of 54 %. Meanwhile, the control group adherence rate was only 46 %, also well below the composite rate of 79 %.
Subset analysis of adherence rates, stratified by VTE risk group. VTE venous thromboembolism, DVT deep venous thrombosis. Medical: medical admission with moderate VTE risk. General surgery: including trauma, urology, and gynecologic oncology surgical services. Neurosurgery: includes surgery for acute spinal cord injury. Central nervous system bleeds were excluded. Elective spinal surgery: including discectomy, elective laminectomy, etc. Orthopedic surgery: hip surgery or knee surgery, including replacement and arthroplasty surgeries. Cardiothoracic: major thoracic surgeries including cardiac bypass and valve replacement surgeries. High bleed risk: all cases of actively bleeding patients or with very high risk for bleeding, including intracranial and gastrointestinal bleeds. Low DVT risk: all cases among the groups (medical or surgical) which were regarded low risk for VTE
The subset of patients who were either actively bleeding or were at high risk for bleeding were categorized as high bleed risk, and pharmacologic prophylaxis was contraindicated; thus mechanical prophylaxis alone would have been sufficient to satisfy the guidelines. There was no difference in the adherence rates between the two groups in this category (40.5 vs. 45.9 %, p = 0.08). In keeping with aforementioned data on SCD documentation rates, there was a high rate of cases lacking documentation of mechanical prophylaxis in both groups (40.5 vs. 51.4 %, p = 0.08).
Prophylaxis choice and contraindications
There were more cases with no prophylaxis ordered in the VTE arm (n = 50, 17.3 %) when compared to the control arm (n = 17, 5.9 %) (p = 0.012). In two of the 50 VTE cases, an absence of VTE prophylaxis was acceptable (low-risk group). Of the 48 remaining cases, twelve did not have their VTE risk assessment form completed, and two others did not have a VTE risk assessment opportunity. Thus, 71 % had a VTE risk assessment performed, and still had no VTE prophylaxis ordered. Meanwhile, there were seventeen cases in the control arm without prophylaxis, but it was acceptable in five cases (low-risk group). Among the remaining twelve cases, seven did not have their VTE risk assessment form completed, and one did not have a risk assessment opportunity, signifying a meagre 25 % risk assessment rate.
The most common reasons for contraindication for prophylaxis in the VTE group were active bleeding (16.3 %), high-risk of bleed (11.4 %) and impending procedure (9.0 %) vs. active bleeding (12.3 %), impending procedure (10.4 %) and low-risk of thrombosis on assessment (6.6 %) in the control group (Table 2). Of note, “same day discharge” was recorded as a contraindication in five patients who suffered a VTE event. 77 of VTE cases and 64 of control cases did not have a documented contraindication for prophylaxis.
Barriers to guideline adherence
Upon review, there were a high number of cases without any VTE prophylaxis ordered, 17.3 % and 5.9 % in the VTE and control arms respectively. Adjusting for guideline adherence, 16.6 % (48/289, VTE group) and 4.2 % (12/289, control group) were inappropriately admitted without VTE prophylaxis. Most of the 48 patients in the VTE arm had VTE risk assessment (34/48, 71 %), and this figure is similar to the composite rate of 77.2 %. Meanwhile, the control arm had a very low risk assessment rate (4/12, 25 %). Upon further review, the VTE risk group composition was different. Whereas 14 of the 17 (82 %) control arm cases were either medicine or of low VTE risk, only 26 of the 50 cases (52 %) were in the above mentioned two categories in the VTE arm. This indicates that there were more cases in the VTE arm that were admitted to the surgical service and thus, were at a higher risk for VTE. This highlights the difficult balance a physician must make to address the thrombotic risk inherent with surgery and yet at the same time, also address the risks of excessive bleeding, while administering pharmacologic prophylaxis.
Barriers to decreased adherence for VTE prophylaxis are summarized in Table 3. Many cases in the VTE arm were labeled as ‘high risk for bleeding’ but were not in fact ‘high-risk’. For example, a patient with a history of ulcerative colitis (a known hypercoagulable condition) without symptoms of exacerbation was listed as high bleeding risk. In twelve other cases, patients admitted for surgery were also assessed as high bleeding risk, but in review did not have an identifiable risk factor. Additionally, there were five other cases who did not receive pharmacologic prophylaxis as they needed to undergo same-day procedures such as elective cardiac catheterizations or pacemaker implantations. In nearly every instance, the VTE risk assessment was performed and accurately completed. As the risk assessment form was a paper worksheet and orders were written electronically, this allowed practitioners to deviate from established guidelines.
Documentation of mechanical prophylaxis
One alarming finding in our study was the rate of mechanical prophylaxis orders without documentation of application, which was similar in both arms (58.6 % in the VTE arm, 50.6 % in the control arm). SCD documentation was only evaluated if there was a contraindication to pharmacologic prophylaxis. Thus in each case, the patient’s only VTE prophylaxis available was mechanical, and if it were documented, would have sufficed for guideline adherence. Indeed, if each instance was documented, the adherence rate would be 11.1 % and 11.8 % more in each arm, or a total of 65 % in the VTE arm and 91 % in the control arm. The importance of mechanical prophylaxis is highlighted by the LIFENOX study which failed to show a difference in all-cause mortality in acutely ill medical patients receiving enoxaparin prophylaxis with knee-length graduated compression stockings compared to those receiving knee-length graduated compression stockings alone [13].
Discussion
VTE prophylaxis adherence rates
289 elderly patients (median age: 69 years), diagnosed with a hospital associated VTE between January 2007 and December 2011 were matched by age, gender and VTE risk group to 289 control patients in this case control study. Our investigation met its primary endpoint in determining that poor adherence to the ACCP guidelines correlated with increased VTE events and one of its secondary endpoints, confirming lower rates of initial VTE risk assessment in the VTE group. Our study did not show a significant difference in SCD documentation rate and total time to initial VTE prophylaxis.
In comparison to previous investigations reporting adherence rates between 38 % and 60 % with the ACCP guidelines, our study showed overall compliance rates of 54 % and 79.2 %, in the VTE and control arms, respectively [9, 10, 14]. While our figures compare favorably to published rates of compliance, there is still room for improvement. The underutilization of VTE thromboprophylaxis highlights the need for a multidisciplinary approach to educate healthcare providers on appropriate thromboprophylaxis and contraindications to chemical prophylaxis [15]. In light of this, six VTE related core measures were approved in the Joint Commission’s performance measurement and improvement initiative [16]. These core measures include VTE prophylaxis in medical, surgical and intensive care unit (ICU) patients, overlap of anticoagulation therapy, platelet count monitoring while on unfractionated heparin, and others.
At our institution, each department has its own VTE risk assessment worksheet that accompanies every admission. This worksheet assists the admitting physician to identify the severity of VTE risk, while at the same time, suggesting the appropriate thromboprophylaxis. In our study, the VTE risk assessment rate was statistically lower in the cohort with a diagnosed VTE, which may partially explain the lower adherence rate in this group. Nevertheless, the absolute difference was only 8 % (77.2 % in the VTE group and 85.5 % in the control group), and it is out of proportion to the 25 % adherence rate difference (54 % vs. 79.2 %). This suggests that there are other factors that contributed to decreased compliance in the VTE arm.
To improve adherence to guidelines, some institutions have developed electronic risk assessment tools and automated system alerts that prompt physicians regarding lapses in VTE prophylaxis. The Brigham and Women’s Hospital completed a prospective study utilizing such a system and demonstrated successfully, an increase in clinician use of thromboprophylaxis, with a subsequent 41 % decline in overall VTE rates at 90-days [17]. This demonstrates that coupling electronic alerts directly with electronic orders for VTE prophylaxis has the potential to decrease VTE rates.
Timeliness of VTE prophylaxis
To our knowledge, there are no studies evaluating the time from patient presentation to VTE prophylaxis delivery in those who subsequently developed a VTE. Although our study found no difference between the two arms, we found that the absolute time in both arms was well in excess of 24 h. While there are no specific recommendations on timeliness in the ACCP guidelines, VTE prophylaxis within 24 h post-operatively is a core measure for the Surgical Care Improvement Project (SCIP) [18]. Thus, efforts to reduce delays in timely delivery of VTE prophylaxis are imperative.
Subset analysis by risk group
Subset data analysis by risk group found little disparity in practice patterns regarding VTE prophylaxis. The adherence rates between all the subgroups were not appreciably different except for the cardiothoracic group (7.7 % in the thrombosis group and 46.2 % in the control group). The VTE risk assessment rate was excellent in both arms within the cardiothoracic surgical patients (12/13 in both), and the median age of both arms was 68 years, which is nominally younger than the composite median age of 69 years.
Subset analysis also revealed that the high bleeding risk group did not have a difference in VTE adherence rates between the arms. More prominently, because this group relied on mechanical prophylaxis for adherence, it also had a high rate of “intention to prophylax”, meaning a high rate of undocumented SCD’s. This highlights the improvements needed to increase the documentation rate.
Limitations
Although our investigation employed a rigorously designed case-control study, it is limited by its retrospective and single-center nature, and the application rate of mechanical prophylaxis was dependent on documentation. Thus, it is highly likely that a portion of patients with undocumented mechanical prophylaxis were actually receiving SCD’s. Cases for the thrombosis arm were identified from medical records indicating development of VTE during a patient’s admission or patients who were readmitted with VTE within 30 days of discharge. It is therefore possible that we may not have detected all hospital-acquired VTE cases between 2007 and 2011, as some of these patients could have been diagnosed and treated at other institutions. Despite meticulous review of VTE risk factors in each VTE and control case to enable accurate assignment of VTE risk categories, there is a possibility that a patients admitted under the same service would fall under a different VTE risk category.
Future
At our institution, the documentation system for SCD application has been simplified, streamlined and is now electronic. Subsequent to this study, mechanical prophylaxis documentation rates have risen markedly. In addition, the admission order sets containing initial thromboprophylaxis orders, previously in paper format, are now electronic. These electronic order-sets have incorporated a similar automated risk scoring system to the one described by Kucher et al., thus simplifying the risk assessment process [19]. An automated alert system is also in the process of being implemented, which may further increase adherence rates [19, 20]. Finally, a prospective study after the implementation of all the above changes will be performed to measure improvements in VTE prophylaxis adherence. We believe that the increasing use of novel oral anticoagulants (NOAC’s) will also have a significant impact on the outcomes.
Conclusions
Low adherence to ACCP guidelines for VTE prophylaxis correlated with an increase in hospital acquired VTE events. The decreased adherence may be linked to a lower VTE risk assessment rate, and other barriers including incorrect identification of contraindications to pharmacologic prophylaxis, and poor documentation of mechanical prophylaxis. There was no difference in SCD documentation rate and timeliness to administration of initial thromboprophylaxis between the two groups.
References
Heit JA, Melton LJ 3rd, Lohse CM et al (2001) Incidence of venous thromboembolism in hospitalized patients vs community residents. Mayo Clin Proc 76:1102–1110
Anderson FA Jr, Zayaruzny M, Heit JA et al (2007) Estimated annual numbers of US acute-care hospital patients at risk for venous thromboembolism. Am J Hematol 82:777–782
Ruppert A, Steinle, Lees M (2011) Economic burden of venous thromboembolism: a systematic review. J Med Econ 14:65–74
MacDougall DA, Feliu AL, Boccuzzi SJ et al (2006) Econonimc burden of deep vein thrombosis, pulmonary embolism, and post-thrombotic syndrome. Am J Health Syst Pharm 63(20 Suppl 6):S5–S15
Guanella R, Ducruet T, Johri M et al (2011) Economic burden and cost determinants of deep vein thrombosis during 2 years following diagnosis: a prospective evaluation. J Thromb Haemost 9:2397–2405
Guyatt GH, Akl EL, Crowther M et al (2012) Executive summary: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. CHEST 141(2 Suppl):7S–47S
Languasco A, Galante M, Marín J et al (2011) Adherence to local guidelines for venous thromboprophylaxis: a cross-sectional study of medical inpatients in Argentina. Thromb J 15(9):18
Kahn SR, Panju A, Geerts W, CURVE study investigators (2007) Multicenter evaluation of the use of venous thromboembolism prophylaxis in acutely ill medical patients in Canada. Thromb Res 119(2):145–155
Tapson VF, Decousus H, Pini M et al (2007) Venous thromboembolism prophylaxis in acutely ill hospitalized medical patients: findings from the International Medical Prevention Registry on Venous Thromboembolism. CHEST 132:936–945
Cohen AT, Victor FT, Jean-Francois B et al (2008) Venous thromboembolism risk and prophylaxis in the acute hospital care setting (ENDORSE study): a multinational cross-sectional study. The Lancet 371:387–394
Anderson FA Jr, Spencer FA (2003) Risk factors for venous thromboembolism. Circulation 107:I9–I16
Geerts WH, Bergqvist D, Pineo GF et al (2008) Prevention of Venous Thromboembolism: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest 133(6_suppl):381S–453S
Kakkar AK, Cimminiello C, Goldhaber SZ, LIFENOX Investigators (2011) Low-molecular-weight heparin and mortality in acutely ill medical patients. N Engl J Med 365(26):2463–2472
Schleyer AM, Schreuder AB, Jarman KM et al (2011) Adherence to guideline-directed venous thromboembolism prophylaxis among medical and surgical inpatients at 33 academic medical centers in the United States. Am J Med Qual 26(3):174–180
Cook D, Tkaczyk A, Lutz K et al (2009) Thromboprophylaxis for hospitalized medical patients: a multicenter qualitative study. J Hosp Med 4(5):269–275
Daniel D, Maund C, Butler K (2010) Community hospital participation in a pilot project for venous thromboembolism quality measures: learning, collaboration, and early improvement. Jt Comm J Qual Patient Saf 36(7):301–309
Piazza G, Goldhaber SZ (2009) Computerized decision support for the cardiovascular clinician: applications for venous thromboembolism prevention and beyond. Circulation 120(12):1133–1137
Bratzler DW, Hunt DR (2006) The surgical infection prevention and surgical care improvement projects: national initiatives to improve outcomes for patients having surgery. Clin Infect Dis 43:322–330
Kucher N, Koo S, Quiroz R et al (2005) Electronic alerts to prevent venous thromboembolism among hospitalized patients. N Engl J Med 352(10):969–977
Fiumara K, Piovella C, Hurwitz S et al (2010) Multi-screen electronic alerts to augment venous thromboembolism prophylaxis. Thromb Haemost 103(2):312–317
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Rights and permissions
About this article
Cite this article
Suh, J., Desai, A., Desai, A. et al. Adherence to thromboprophylaxis guidelines in elderly patients with hospital acquired venous thromboembolism: a case control study. J Thromb Thrombolysis 43, 172–178 (2017). https://doi.org/10.1007/s11239-016-1432-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-016-1432-6