Abstract
Platelet reactivity, an important factor in hemostasis and chronic disease, has widespread inter-individual variability with a substantial genetic contribution. Previously, our group performed a genome-wide association study of platelet reactivity identifying single nucleotide polymorphisms (SNPs) associated with ADP- and epinephrine- induced aggregation, including SNPs in MRVI1, PIK3CG, JMJD1C, and PEAR1, among others. Here, we assessed the association of these previously identified SNPs with ADP-, thrombin-, and shear- induced platelet aggregation. Additionally, we sought to expand the association of these SNPs with blood cell counts and hemostatic factors. To accomplish this, we examined the association of 12 SNPs with seven platelet reactivity and various hematological measures in 1300 middle-aged men in the Caerphilly Prospective Study. Nine of the examined SNPs showed at least suggestive association with platelet reactivity. The strongest associations were with rs12566888 in PEAR1 to ADP-induced (p = 1.51 × 10−7) and thrombin-induced (p = 1.91 × 10−6) reactivity in platelet rich plasma. Our results indicate PEAR1 functions in a relatively agonist independent manner, possibly through subsequent intracellular propagation of platelet activation. rs10761741 in JMJD1C showed suggestive association with ADP-induced reactivity (p = 1.35 × 10−3), but its strongest associations were with platelet-related cell counts (p = 1.30 × 10−9). These associations indicate variation in JMJD1C influences pathways that modulate platelet development as well as those that affect reactivity. Associations with other blood cell counts and hemostatic factors were generally weaker among the tested SNPs, indicating a specificity of these SNPs’ function to platelets. Future genome-wide analyses will further assess association of these genes and identify new genes important to platelet biology.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Platelet reactivity and aggregation are important aspects of hemostasis and wound healing, as well as common therapeutic targets in primary and secondary prevention of cardiovascular disease [1]. Several endogenous agonists, including epinephrine, ADP, and thrombin, among other activators, cause platelet aggregation. These reactive mechanisms serve as initial steps in thrombosis and clotting that allow for injury healing and repair. Differences in platelet reactivity among individuals have substantial effects on thrombotic function and clinical use of anti-platelet agents. Inter-individual variability in platelet reactivity does have a substantial genetic component, with heritability estimates ranging from 40–60 % [2].
Despite this considerable genetic influence, relatively few genome-wide genetic scans have been conducted on platelet reactivity traits in cohort studies, possibly due to logistical and technical difficulties of accurately collecting such data [2]. Our group conducted the largest genome-wide association study (GWAS) on ADP- and epinephrine- induced reactivity in platelet-rich plasma (PRP) and collagen lag time [3]. There, we identified and replicated novel associations with single nucleotide polymorphisms (SNPs) in or near MRVI1, SHH, PIK3CG and JMJD1C, as well as strengthened prior associations of SNPs in or near ADRA2A, PEAR1 and GP6 [3]. There were also several loci with suggestive associations, including some with responses to two or more agonists in the same direction of effect (e.g., ADAMTS2, RGS18, and SVIL). The relevance of these associated genes to platelet function in subsequent animal and cellular models reinforced the utility of human genetics in identifying genes important to platelet reactivity. For example, PEAR1 is involved in sustaining αIIβ3 activation following agonist recognition and in attenuating megakaryopoiesis [4, 5]. Additionally, variants in SVIL were associated with human shear-dependent platelet function. SVIL knockout mice had larger platelets and enhanced thrombus formation under high-shear conditions [6]. Based on these human genetic and subsequent functional studies, we hypothesized that additional assessment of our previously identified SNPs with a variety of agonists and related traits may extend SNP associations and highlight candidates for future functional studies.
To accomplish this, we used data from the Caerphilly Prospective Study (CaPs), a population sample of approximately 3000 middle aged men from Caerphilly, South Wales. Started in 1979, the primary intent of the study was to identify risk factors for ischemic heart disease [7]. During two of the five phases, platelet reactivity measures in PRP and/or whole blood were collected for ADP, thrombin, and shear stress. We selected 12 promising SNPs from our prior platelet reactivity GWAS and genotyped these in CaPs to assess whether these SNPs were associated with platelet reactivity to several agonists in an independent cohort [3]. Additionally, platelet count (PLT) and mean platelet volume (MPV) as well as other blood cell count and hemostatic factors were collected. We further examined whether these platelet reactivity SNPs were associated with these blood cell counts and hemostatic factors.
Materials and methods
Study sample and approval
CaPs is comprised of unrelated men of European ancestry from Caerphilly, South Wales as previously described [7]. All phenotypes examined presently were collected during Phase 2 or Phase 3 of the study, while genomic DNA was collected in Phase 4. Informed consent was obtained from all participants. Ethical approval for genetic studies in CaPs was granted by the South East Wales Research Ethics Committee (05/WSE02/131) and the Institutional Review Board at the National Hearth Lung and Blood Institute.
Platelet function measures in CaPs
ADP- and thrombin-induced reactivity in PRP
In Phase 2, platelet reactivity in PRP to ADP and thrombin was measured by light transmission aggregation (LTA). Fasting venous blood samples were collected into 0.13 M sodium citrate tubes, and PRP isolated by protocols previously described [8, 9]. Aggregation was measured in duplicate in PRP adjusted to 300,000 platelet/uL in autologous platelet poor plasma. The extent of optical density change to 0.725 μM/L ADP in the primary and secondary response wave, as well as the primary response wave to 0.056 unit/mL thrombin (Sigma Chemical Corp., Poole, UK), was measured in a Rubel-Renaud coaguloaggregometer [8].
ADP-induced reactivity in whole blood
In Phase 3, ADP-induced reactivity was determined in whole blood by impedance measures as previously described [10, 11]. In brief, fasting venous blood samples were collected in plastic syringes containing 0.13 M sodium citrate at pH 7.4. Sealed samples were left 30 min. All impedance testing was completed between 30 min and 120 min. The minimal concentration of ADP to produce a 1.5 Ω change in impedance within 2.5 min in a Chronolog 560 Aggregometer (Havertown, PA), was determined by testing 19 serially increasing concentrations of ADP (from 0.1 to 21.5 μM/L) (Sigma Chemical Corp., Poole, UK). The minimal ADP dose required to produce a 21.5 Ω impedance change was measured similarly.
Shear-induced platelet reactivity in whole blood
Retention of platelets after induction of shear stress filtration was measured in Phase 3 as previously described [12]. Briefly, within 5 min of a fasting venous blood draw, heparinized blood was forced at 40 mmHg through a 13 mm diameter filter with fibers ranging from 0.1–3.4 μM. Blood drops passing through filters were measured electronically over time. PLT was measured with a Sysmex K1000 analyzer (Kobe, Japan) in separate pre-filtration and post-blockage samples. Blockage was defined as ≤1 blood drop in 5 s. Pre- and post-blockage PLT were used to calculate the absolute and relative retention values. Four samples were eliminated for having higher post-blockage PLT, and two were eliminated for missing either a pre- or post-PLT .
Other hematological and hemostatic factor measures
Fasting, citrated blood plasma from was stored at −70 °C for assays conducted at the University of Glasgow. Cell counts were obtained on blood samples from Phase 2 (Couter S+, Coulter Corporation, Miami, FL) and Phase 3 (Technicon HI, Bayer, Newbury, UK). These included PLT, MPV, white blood cell (WBC) count, red blood cell (RBC) count, hemoglobin, hematocrit, mean corpuscular volume (MCV), mean corpuscular hemoglobin (MCH), neutrophil, lymphocyte, monocyte, eosinophil, basophil, and leukocyte counts. Hemostatic factors included Clauss fibrinogen [13], von Willebrand Factor antigen [14], tissue plasminogen activator antigen [15], plasminogen-activator inhibitor [15], and fibrin D-dimer with both original ELISA assay [15] and Gold assay [16] as previously described.
SNP selection and genotyping
Twelve SNPs were selected primarily on the basis of our prior GWAS results. Eight were selected for having at least suggestive results (p < 5 × 10−5) for associations with ADP- and epinephrine-induced platelet reactivity [3]. We included these because we reasoned they were more likely to influence platelet aggregation in an agonist independent manner, particularly as the overlap between agonists in the prior and current studies was incomplete. These eight SNPs were rs11144351 (PIP5K1B), rs12359150 (CUBN), rs12566888 (PEAR1), rs16876805 (ATP6V0D2), rs2479008 (GMDS), rs4128880 (RGS18), rs467053 (ADAMTS2), and rs7940646 (MRVI1). Since platelet reactivity to epinephrine was not measured in CaPs, two additional ADP-only associated SNPs, rs2363910 in SHH and rs9996294 in RAPGEF2, were also selected. Two epinephrine-only associated loci rs10761741 in JMJD1C and rs342286 in PIK3CG were selected because both have demonstrated pleiotropy with PLT and/or MPV [17]. The selected SNPs and rationale for inclusion are summarized in Table 1 [3]. SNPs were genotyped on genomic DNA stored at LGC Genomics, Inc. (Teddington, UK) using KASP™ genotyping technology. SNP probe information is available in Supplemental Table 1, and SNPviewer (LGC Genomics, Inc., Teddington, UK) was used to review cluster genotype calling.
Statistical analyses
Most traits were normally distributed, but appropriate data transformations were applied when non-normal as noted in the Results. We only adjusted for age in our models as CaPs is entirely comprised of men. We performed analyses in all subjects as well as in a subset of participants not taking anti-platelet medication (e.g., aspirin and dipyridamole) and with greater than 8 h since last food eaten (Supplemental Table 2). Subjects with a genotyping rate less than 80 % were also excluded (n = 37). One SNP, rs16876805 in ATP6V0D2, was excluded due to its rare minor allele frequency (MAF = 0.009). The sample size for each phenotype is in Supplemental Table 2. SNPs were tested for association with quantitative measures of platelet reactivity using PLINK [18]. We tested 11 SNPs for association with 7 distinct platelet aggregation measures in our primary analyses. Therefore, we used Bonferroni correction for multiple testing: 0.05/(7 SNPs × 11 phenotypes) = 6.49 × 10−4. Bonferroni correction is overly conservative, as these SNPs have prior GWAS associations with our primary outcome and the phenotypes are correlated. We also present associations with p < 0.01 in the main text and full results for additive models in the supplement (Supplemental Tables 3–8). We also performed two separate secondary analyses: (1) platelet-related cell count (PLT/MPV) and (2) non-platelet cell count and hemostatic factors. Associations with p < 0.01 in these secondary analyses are reported.
Results
Genotype quality was high for all SNPs with an average call rate of 98.1 %. Allele frequencies in CaPs ranged from rare (rs16876805, 0.9 % MAF) to common (rs4128880, 47.0 % MAF), and were similar to reference European ancestry allele frequencies (Table 1). Demographics for subjects included in analyses are summarized in Supplemental Table 9.
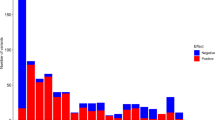
Nine of eleven tested SNPs showed at least marginal associations with platelet reactivity (p < 0.05) (Supplemental Table 10). The strongest associations were with rs12566888 in PEAR1. The T allele was associated with reduced primary aggregation to ADP (β = −2.29, p = 9.98 × 10−5), secondary aggregation to ADP (β = −0.13, p = 1.51 × 10−7), and aggregation to thrombin (β = −2.07, p = 1.91 × 10−6) (Table 2). In addition, several other SNPs showed suggestive associations with platelet reactivity traits. The G allele of rs10761741 in JMJD1C showed evidence of association with increased ADP dose necessary to incur both a 1.5 Ω impedance (β = 0.44, p = 1.35 × 10−3) and 21.5 Ω impedance (β = 0.42, p = 8.52 × 10−3) change (Table 2). These results indicate that the G allele of rs10761741in JMJD1C were associated with decreased platelet reactivity. SNPs in SHH (β = −0.06, p = 6.65 × 10−3), RGS18 (β = −0.04, p = 4.35 × 10−3), and MRVI1 (β = 11.01, p = 5.04 × 10−3) were suggestively associated with secondary aggregation to ADP (Table 2).
Next, we examined whether these 11 SNPs with prior relationships with platelet aggregation were also associated with platelet-related cell count measures, other blood cell counts, and hemostatic factors. Two SNPs, rs10761741 in JMJD1C and rs342286 in PIK3CG, showed associations with PLT and/or MPV (Table 3). In both phases, the G allele of rs10761741 was associated with decreased PLT (Phase 2: β = −9.37, p = 3.50 × 10−5; Phase 3: β = −8.71 p = 9.05 × 10−5) and increased MPV (Phase 2: β = 1.17, p = 5.07 × 10−3; Phase 3: β = 2.25 p = 1.30 × 10−9) (Table 3). Similarly, rs342286 in PIK3CG associated with increased MPV (Phase 2: β = 1.39 p = 9.43 × 10−4; Phase 3: β = 1.09 p = 3.46 × 10−3) (Table 3). However, no other SNP, including rs12566888 in PEAR1, showed evidence of association with PLT or MPV (p > 0.05).
Associations with non-platelet blood cell count and hemostatic factors were generally weak. The most intriguing associations were rs9996294 in RAPGEF2 and rs342286 in PIK3CG with RBC-related traits (Table 4). These included nominal associations of (1) rs9996294 with RBC (β = −6.04, p = 9.97 × 10−3), hemoglobin (β = −2.49, p = 5.12 × 10−4), hematocrit (β = −6.90, p = 1.07 × 10−3), and D-dimer (β = 0.38, p = 7.40 × 10−3) and (2) rs342286 with RBC (β = −4.65, p = 3.54 × 10−3) and hemoglobin (β = −1.25, p = 9.30 × 10−3).
Discussion
In this investigation, our primary goal was to assess the associations of 12 SNPs identified by GWAS with a variety of platelet reactivity measures in the independently ascertained CaPs. We further implicate rs12566888 in PEAR1 with ADP-induced platelet reactivity and expand its association to thrombin-induced platelet reactivity. We also provide suggestive evidence for association of 8 other SNPs, including rs10761741 in JMJD1C, rs2363910 in SHH, rs4128880 in RGS18, and rs7940646 in MRVI1. A majority of the platelet reactivity associated SNPs were not associated with platelet-related cell count traits. Of the SNPs examined, only rs10761741 in JMJD1C and rs342286 in PIK3CG showed association with PLT and/or MPV. Associations with non-platelet blood cell counts and hemostatic factors were fewer and weaker. Nonetheless, rs9996294 in RAPGEF2 and rs342286 in PIK3CG had suggestive associations with RBC-related traits. The lack of associations of platelet reactivity implicated SNPs with other blood cell and hemostatic factors suggest divergent pathways for platelet reactivity from other blood cell and hemostatic factor traits.
The strongest associations with platelet aggregation in this study were with rs12566888 in PEAR1. In our previous GWAS, PEAR1 influenced platelet aggregation to both ADP and epinephrine [3]. There, the T allele of intronic rs12566888 was associated with reduced reactivity to both ADP and epinephrine. Here, we replicate the association of the T allele with reduced aggregation to ADP and extend it to reduced aggregation to thrombin. Our studies in conjunction with others have now observed associations of PEAR1 with platelet reactivity to epinephrine, ADP, thrombin, and collagen [3, 19]. Its associations with multiple agonists indicate PEAR1 functions in the intracellular propagation of general platelet activation as opposed to the recognition and downstream signaling of specific agonists. Platelet activation increases expression of PEAR1 and its phosphorylation at the cell surface. This phosphorylation of PEAR1 yields a signaling cascade that activates αIIbβ3 and allows it to bind to fibrinogen [5]. Despite a number of genetic studies implicating different PEAR1 variants [3, 19–23], rs12566888 has been the strongest and most consistently associated variant. It also has been associated with aspirin, clopidogrel/prasugel, and dual anti-platelet responses, as well as sticky platelet syndrome and fetal loss [22, 24–26]. These findings indicate PEAR1 plays an agonist independent role in platelet reactivity and suggest it as a valuable therapeutic target.
We also observed suggestive association of rs10761741 in JMJD1C with ADP-induced platelet reactivity. The G allele was associated with a higher ADP dose necessary to induce impedance changes, indicating reduced reactivity. The T allele of rs10761741, the alternative allele to G, was associated with increased reactivity to epinephrine but not ADP, at a genome-wide significant level, in our previous study [3]. In conjunction with these previous results, our study indicates that the G allele of rs10761741 in JMJD1C is associated with decreased platelet reactivity to ADP and epinephrine. However, our strongest associations of rs10761741 were with MPV and PLT as previously seen with this SNP and others in JMJD1C [17, 27, 28]. The G allele of rs10761741 was associated with increased MPV and decreased PLT, as well as decreased platelet reactivity. Associations with PLT/MPV and aggregation suggest that JMJD1C functions in pathways that influence the platelet development as well as their reactivity to various agonists. JMJD1C encodes a histone demethylase expressed and functional in pluripotent and multipotent cells including human bone marrow [29–31]. Its development functions, possibly through interactions with androgen receptor, are thought to modulate gene expression [32]. Identification of transcriptional targets and temporal relationships of JMJD1C within platelet development and activation will be necessary to disentangle causal pathways and to what extent they are shared between these processes.
Generally, the other SNPs did not associate with blood cell counts or hemostatic traits. rs12566888 in PEAR1 notably did not show associations with any cell count or hemostatic trait (p > 0.05). The specificity of PEAR1 associations with platelet aggregation indicates PEAR1 functions primarily in a platelet’s ability to respond to agonists and injury. The only other SNP to show association with MPV was rs342286 in PIK3CG. rs342286 was also marginally associated with various RBC traits, indicating PIK3CG influences function of multiple blood cell traits as suggested in animal models [33–35]. Also marginally associated with RBC traits was rs9996294 in RAPGEF2. Mouse knockouts of Rapgef2 suggest the essentiality of the gene for embryonic RBC development but not adult hematopoiesis [36]. These developmental effects of RAPGEF2 on hematopoiesis may have life-long effects on RBC-related traits that we marginally detected here. However, the general lack of associations of platelet reactivity SNPs with other hematological traits suggests that many platelet aggregation loci generally function in a platelet specific manner. This specificity implies that continued investigation of platelet aggregation genes should be examined in future cohort studies of larger sample size as well as animal and cellular models. To this end, we plan to perform a GWAS of platelet reactivity in CaPs to identify novel genetic elements that influence platelet function.
The findings of this study are subject to several limitations. First, although our aim was to further examine the strongest associations of our previous GWAS, the platelet aggregation measures of the two investigations were not identical. Both studies did have reactivity measures in response to ADP, although study doses and equipment varied. We could not, however, specifically query epinephrine-induced aggregation associations previously observed. Additionally, differences in agonist dosages and methods of measurements may explain why we are unable to replicate some previous findings. Second, our ability to detect common variant associations was limited by sample size, although CaPs is among the largest cohort studies with collected platelet aggregation. Increased sample size and meta-analysis with other cohort studies will further increase statistical power. Third, CaPs is comprised entirely of men from a local community in South Wales. These genetic associations should eventually be extended to more diverse cohorts and populations.
In this investigation, we confirm the association of rs12566888 in PEAR1 with platelet aggregation to ADP and extend it to reactivity to thrombin. Our associations along with others indicate that PEAR1’s role in platelet reactivity is relatively agonist independent. Nine of the eleven SNPs examined showed at least suggestive association with platelet reactivity measures. We observed associations of rs10761741 in JMJD1C with PLT and MPV as well as provide marginal support for its association with ADP-induced platelet reactivity. These results further confirm the role of these genes in platelet aggregation. Our associations also indicate that there are shared and unique pathways governing platelet-related cell count and platelet reactivity. Further interrogation of these pathways by identifying more associated genetic factors through increased sample size and genomic coverage and by modeling these factors in animal and cellular models will help determine to what extent these pathways are shared.
Abbreviations
- SNP:
-
Single nucleotide polymorphism
- GWAS:
-
Genome-wide association study
- PRP:
-
Platelet rich plasma
- CaPs:
-
Caerphilly Prospective Study in men
- PLT:
-
Platelet count
- MPV:
-
Mean platelet volume
- LTA:
-
Light transmission aggregometry
- WBC:
-
White blood cell
- RBC:
-
Red blood cell
- MCV:
-
Mean corpuscular volume
- MCH:
-
Mean corpuscular hemoglobin
- MAF:
-
Minor allele frequency
References
Hennekens CH, Dyken ML, Fuster V (1997) Aspirin as a therapeutic agent in cardiovascular disease: a statement for healthcare professionals from the American Heart Association. Circulation 96:2751–2753
Johnson AD (2011) The genetics of common variation affecting platelet development, function and pharmaceutical targeting. J Thromb Haemost 9(Suppl 1):246–257
Johnson AD, Yanek LR, Chen MH, Faraday N, Larson MG, Tofler G, Lin SJ, Kraja AT, Province MA, Yang Q, Becker DM, O’Donnell CJ, Becker LC (2010) Genome-wide meta-analyses identifies seven loci associated with platelet aggregation in response to agonists. Nat Genet 42:608–613
Kauskot A, Vandenbriele C, Louwette S, Gijsbers R, Tousseyn T, Freson K, Verhamme P, Hoylaerts MF (2013) PEAR1 attenuates megakaryopoiesis via control of the PI3K/PTEN pathway. Blood 121:5208–5217
Kauskot A, Di MM, Loyen S, Freson K, Verhamme P, Hoylaerts MF (2012) A novel mechanism of sustained platelet alphaIIbbeta3 activation via PEAR1. Blood 119:4056–4065
Edelstein LC, Luna EJ, Gibson IB, Bray M, Jin Y, Kondkar A, Nagalla S, Hadjout-Rabi N, Smith TC, Covarrubias D, Jones SN, Ahmad F, Stolla M, Kong X, Fang Z, Bergmeier W, Shaw C, Leal SM, Bray PF (2012) Human genome-wide association and mouse knockout approaches identify platelet supervillin as an inhibitor of thrombus formation under shear stress. Circulation 125:2762–2771
The Caerphilly and Speedwell Collaborative Group (1984) Caerphilly and Speedwell collaborative heart disease studies. The Caerphilly and Speedwell Collaborative Group. J Epidemiol Community Health 38:259–262
Elwood PC, Renaud S, Sharp DS, Beswick AD, O’Brien JR, Yarnell JW (1991) Ischemic heart disease and platelet aggregation. The Caerphilly Collaborative Heart Disease Study. Circulation 83:38–44
Renaud S, Godsey F, Dumont E, Thevenon C, Ortchanian E, Martin JL (1986) Influence of long-term diet modification on platelet function and composition in Moselle farmers. Am J Clin Nutr 43:136–150
Sharp DS, Ben-Shlomo Y, Beswick AD, Andrew ME, Elwood PC (2005) Platelet aggregation in whole blood is a paradoxical predictor of ischaemic stroke: Caerphilly Prospective Study revisited. Platelets 16:320–328
Elwood PC, Beswick AD, Sharp DS, Yarnell JW, Rogers S, Renaud S (1990) Whole blood impedance platelet aggregometry and ischemic heart disease. The Caerphilly Collaborative Heart Disease Study. Arteriosclerosis 10:1032–1036
Beswick AD, O’Brien JR, Limb ES, Yarnell JW, Elwood PC (1994) Shear-induced filter blockage. A population based appraisal of a method for the assessment of platelet, white cell and von Willebrand factor interactions. Platelets 5:186–192
Sweetnam PM, Yarnell JW, Lowe GD, Baker IA, O’Brien JR, Rumley A, Etherington MD, Whitehead PJ, Elwood PC (1998) The relative power of heat-precipitation nephelometric and clottable (Clauss) fibrinogen in the prediction of ischaemic heart disease: the Caerphilly and Speedwell studies. Br J Haematol 100:582–588
Rumley A, Lowe GD, Sweetnam PM, Yarnell JW, Ford RP (1999) Factor VIII, von Willebrand factor and the risk of major ischaemic heart disease in the Caerphilly Heart Study. Br J Haematol 105:110–116
Lowe GD, Yarnell JW, Sweetnam PM, Rumley A, Thomas HF, Elwood PC (1998) Fibrin D-dimer, tissue plasminogen activator, plasminogen activator inhibitor, and the risk of major ischaemic heart disease in the Caerphilly Study. Thromb Haemost 79:129–133
Lowe GD, Rumley A, Sweetnam PM, Yarnell JW, Rumley J (2001) Fibrin D-dimer, markers of coagulation activation and the risk of major ischaemic heart disease in the caerphilly study. Thromb Haemost 86:822–827
Gieger C, Radhakrishnan A, Cvejic A, Tang W, Porcu E, Pistis G, Serbanovic-Canic J, Elling U, Goodall AH, Labrune Y, Lopez LM, Magi R, Meacham S, Okada Y, Pirastu N, Sorice R, Teumer A, Voss K, Zhang W, Ramirez-Solis R, Bis JC, Ellinghaus D, Gogele M, Hottenga JJ, Langenberg C, Kovacs P, O’Reilly PF, Shin SY, Esko T, Hartiala J, Kanoni S, Murgia F, Parsa A, Stephens J, van der Harst P, Ellen van der Schoot C, Allayee H, Attwood A, Balkau B, Bastardot F, Basu S, Baumeister SE, Biino G, Bomba L, Bonnefond A, Cambien F, Chambers JC, Cucca F, D’Adamo P, Davies G, de Boer RA, de Geus EJ, Doring A, Elliott P, Erdmann J, Evans DM, Falchi M, Feng W, Folsom AR, Frazer IH, Gibson QD, Glazer NL, Hammond C, Hartikainen AL, Heckbert SR, Hengstenberg C, Hersch M, Illig T, Loos RJ, Jolley J, Khaw KT, Kuhnel B, Kyrtsonis MC, Lagou V, Lloyd-Jones H, Lumley T, Mangino M, Maschio A, Mateo Leach I, McKnight B, Memari Y, Mitchell BD, Montgomery GW, Nakamura Y, Nauck M, Navis G, Nothlings U, Nolte IM, Porteous DJ, Pouta A, Pramstaller PP, Pullat J, Ring SM, Rotter JI, Ruggiero D, Ruokonen A, Sala C, Samani NJ, Sambrook J, Schlessinger D, Schreiber S, Schunkert H, Scott J, Smith NL, Snieder H, Starr JM, Stumvoll M, Takahashi A, Tang WH, Taylor K, Tenesa A, Lay TS, Tonjes A, Uda M, Ulivi S, van Veldhuisen DJ, Visscher PM, Volker U, Wichmann HE, Wiggins KL, Willemsen G, Yang TP, Hua ZJ, Zitting P, Bradley JR, Dedoussis GV, Gasparini P, Hazen SL, Metspalu A, Pirastu M, Shuldiner AR, van Joost PL, Zwaginga JJ, Boomsma DI, Deary IJ, Franke A, Froguel P, Ganesh SK, Jarvelin MR, Martin NG, Meisinger C, Psaty BM, Spector TD, Wareham NJ, Akkerman JW, Ciullo M, Deloukas P, Greinacher A, Jupe S, Kamatani N, Khadake J, Kooner JS, Penninger J, Prokopenko I, Stemple D, Toniolo D, Wernisch L, Sanna S, Hicks AA, Rendon A, Ferreira MA, Ouwehand WH, Soranzo N (2011) New gene functions in megakaryopoiesis and platelet formation. Nature 480:201–208
Purcell S, Neale B, Todd-Brown K, Thomas L, Ferreira MA, Bender D, Maller J, Sklar P, de Bakker PI, Daly MJ, Sham PC (2007) PLINK: a tool set for whole-genome association and population-based linkage analyses. Am J Hum Genet 81:559–575
Qayyum R, Becker LC, Becker DM, Faraday N, Yanek LR, Leal SM, Shaw C, Mathias R, Suktitipat B, Bray PF (2015) Genome-wide association study of platelet aggregation in African Americans. BMC Genet 16:58
Jones CI, Bray S, Garner SF, Stephens J, de Bono B, Angenent WG, Bentley D, Burns P, Coffey A, Deloukas P, Earthrowl M, Farndale RW, Hoylaerts MF, Koch K, Rankin A, Rice CM, Rogers J, Samani NJ, Steward M, Walker A, Watkins NA, Akkerman JW, Dudbridge F, Goodall AH, Ouwehand WH (2009) A functional genomics approach reveals novel quantitative trait loci associated with platelet signaling pathways. Blood 114:1405–1416
Kim Y, Suktitipat B, Yanek LR, Faraday N, Wilson AF, Becker DM, Becker LC, Mathias RA (2013) Targeted deep resequencing identifies coding variants in the PEAR1 gene that play a role in platelet aggregation. PLoS One 8:e64179
Lewis JP, Ryan K, O’Connell JR, Horenstein RB, Damcott CM, Gibson Q, Pollin TI, Mitchell BD, Beitelshees AL, Pakzy R, Tanner K, Parsa A, Tantry US, Bliden KP, Post WS, Faraday N, Herzog W, Gong Y, Pepine CJ, Johnson JA, Gurbel PA, Shuldiner AR (2013) Genetic variation in PEAR1 is associated with platelet aggregation and cardiovascular outcomes. Circ Cardiovasc Genet 6:184–192
Faraday N, Yanek LR, Yang XP, Mathias R, Herrera-Galeano JE, Suktitipat B, Qayyum R, Johnson AD, Chen MH, Tofler GH, Ruczinski I, Friedman AD, Gylfason A, Thorsteinsdottir U, Bray PF, O’Donnell CJ, Becker DM, Becker LC (2011) Identification of a specific intronic PEAR1 gene variant associated with greater platelet aggregability and protein expression. Blood 118:3367–3375
Wurtz M, Nissen PH, Grove EL, Kristensen SD, Hvas AM (2014) Genetic determinants of on-aspirin platelet reactivity: focus on the influence of PEAR1. PLoS One 9:e111816
Xiang Q, Cui Y, Zhao X, Zhao N (2013) Identification of PEAR1 SNPs and their influences on the variation in prasugrel pharmacodynamics. Pharmacogenomics 14:1179–1189
Sokol J, Biringer K, Skerenova M, Stasko J, Kubisz P, Danko J (2015) Different models of inheritance in selected genes in patients with sticky platelet syndrome and fetal loss. Semin Thromb Hemost 41:330–335
Qayyum R, Snively BM, Ziv E, Nalls MA, Liu Y, Tang W, Yanek LR, Lange L, Evans MK, Ganesh S, Austin MA, Lettre G, Becker DM, Zonderman AB, Singleton AB, Harris TB, Mohler ER, Logsdon BA, Kooperberg C, Folsom AR, Wilson JG, Becker LC, Reiner AP (2012) A meta-analysis and genome-wide association study of platelet count and mean platelet volume in African Americans. PLoS Genet 8:e1002491
Soranzo N, Spector TD, Mangino M, Kuhnel B, Rendon A, Teumer A, Willenborg C, Wright B, Chen L, Li M, Salo P, Voight BF, Burns P, Laskowski RA, Xue Y, Menzel S, Altshuler D, Bradley JR, Bumpstead S, Burnett MS, Devaney J, Doring A, Elosua R, Epstein SE, Erber W, Falchi M, Garner SF, Ghori MJ, Goodall AH, Gwilliam R, Hakonarson HH, Hall AS, Hammond N, Hengstenberg C, Illig T, Konig IR, Knouff CW, McPherson R, Melander O, Mooser V, Nauck M, Nieminen MS, O’Donnell CJ, Peltonen L, Potter SC, Prokisch H, Rader DJ, Rice CM, Roberts R, Salomaa V, Sambrook J, Schreiber S, Schunkert H, Schwartz SM, Serbanovic-Canic J, Sinisalo J, Siscovick DS, Stark K, Surakka I, Stephens J, Thompson JR, Volker U, Volzke H, Watkins NA, Wells GA, Wichmann HE, Van Heel DA, Tyler-Smith C, Thein SL, Kathiresan S, Perola M, Reilly MP, Stewart AF, Erdmann J, Samani NJ, Meisinger C, Greinacher A, Deloukas P, Ouwehand WH, Gieger C (2009) A genome-wide meta-analysis identifies 22 loci associated with eight hematological parameters in the HaemGen consortium. Nat Genet 41:1182–1190
Katoh M, Katoh M (2007) Comparative integromics on JMJD1C gene encoding histone demethylase: conserved POU5F1 binding site elucidating mechanism of JMJD1C expression in undifferentiated ES cells and diffuse-type gastric cancer. Int J Oncol 31:219–223
Sroczynska P, Cruickshank VA, Bukowski JP, Miyagi S, Bagger FO, Walfridsson J, Schuster MB, Porse B, Helin K (2014) shRNA screening identifies JMJD1C as being required for leukemia maintenance. Blood 123:1870–1882
Shakya A, Callister C, Goren A, Yosef N, Garg N, Khoddami V, Nix D, Regev A, Tantin D (2015) Pluripotency transcription factor Oct4 mediates stepwise nucleosome demethylation and depletion. Mol Cell Biol 35:1014–1025
Wolf SS, Patchev VK, Obendorf M (2007) A novel variant of the putative demethylase gene, s-JMJD1C, is a coactivator of the AR. Arch Biochem Biophys 460:56–66
Hirsch E, Bosco O, Tropel P, Laffargue M, Calvez R, Altruda F, Wymann M, Montrucchio G (2001) Resistance to thromboembolism in PI3Kgamma-deficient mice. FASEB J 15:2019–2021
Hirsch E, Lembo G, Montrucchio G, Rommel C, Costa C, Barberis L (2006) Signaling through PI3Kgamma: a common platform for leukocyte, platelet and cardiovascular stress sensing. Thromb Haemost 95:29–35
Lian L, Wang Y, Draznin J, Eslin D, Bennett JS, Poncz M, Wu D, Abrams CS (2005) The relative role of PLCbeta and PI3Kgamma in platelet activation. Blood 106:110–117
Satyanarayana A, Gudmundsson KO, Chen X, Coppola V, Tessarollo L, Keller JR, Hou SX (2010) RapGEF2 is essential for embryonic hematopoiesis but dispensable for adult hematopoiesis. Blood 116:2921–2931
Acknowledgments
The authors wish to acknowledge the subjects who volunteered their time and effort as well as the National Heart, Lung and Blood Institute Intramural Research Program funding to Dr. Chris J. O’Donnell for the support of SNP genotyping. The Caerphilly Prospective Study was undertaken by the former MRC Epidemiology Unit (South Wales) and was funded by the Medical Research Council of the United Kingdom. The Caerphilly DNA Bank was established by an MRC Grant (G9824960).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interests
The authors state that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Eicher, J.D., Xue, L., Ben-Shlomo, Y. et al. Replication and hematological characterization of human platelet reactivity genetic associations in men from the Caerphilly Prospective Study (CaPS). J Thromb Thrombolysis 41, 343–350 (2016). https://doi.org/10.1007/s11239-015-1290-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-015-1290-7