Abstract
D-dimer levels are increased in patients with acute pulmonary embolism (PE). However, D-dimer levels are also increased in patients with community-acquired pneumonia (CAP). The aim of this prospective cohort study was to examine the incidence and clinical features of patients preliminarily diagnosed with CAP and with increased D-dimer levels, and who finally were diagnosed with PE. Patients diagnosed with CAP and hospitalized in the Respiratory Department of the Tenth People’s Hospital Affiliated to Tongji University between May 2011 and May 2013 were enrolled. D-dimer levels were measured routinely after admission. For patients with increased D-dimer levels, those suspected with PE underwent computed tomography pulmonary angiography (CTPA). A total of 2387 patients with CAP was included: 724 (30.3 %) had increased D-dimer levels (median of 0.91 mg/L). CTPA was performed for 139 of the 724 patients (median D-dimer levels of 1.99 mg/L). Among the 139 patients, 80 were diagnosed with PE, and 59 without PE; D-dimer levels were 2.83 and 1.41 mg/L, respectively (p < 0.05). Multivariate analysis showed that age, coronary heart disease, chronic obstructive pulmonary disease (COPD), lower limb varicosity, chest pain, shortness of breath, hemoptysis, fever, and increased levels of troponin I were independent risk factors for PE. Presentation of PE and CAP are similar. Nevertheless, these results indicated that for hospitalized patients with CAP and elevated D-dimer levels, PE should be considered for those >60 years; with CHD, COPD, or lower limb varicosity; with chest pain, shortness of breath, hemoptysis, increased troponin I, or low fever.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pulmonary embolism (PE) is a group of diseases or clinical symptoms characterized by a mechanical obstruction of the pulmonary artery system. In fact, PE refers to pulmonary thromboembolism (PTE) in most cases, which is caused by the blockage of the pulmonary artery by a blood clot from the venous system or right ventricle [1–4]. PE usually leads to pulmonary dysfunction or respiratory insufficiency. As the clinical presentations of PE are not specific, this disease is easily misdiagnosed or missed [1–4]. The mortality rate of PE is as high as 25–30 % if not treated; however, timely diagnosis and treatment reduce the mortality rate to 2–8 % [1–4]. Therefore, timely diagnosis is paramount to improve patients’ outcomes.
Currently, diagnosing PE mainly depends on computed tomography pulmonary angiography (CTPA); pulmonary artery obstruction index (PAOI) could also be used to quantitatively evaluate the severity of PE [1–4]. However, the complexity and high medical costs of these methods limit their widespread application. Therefore, clinical evaluation models and serum biomarkers are used for the early screening of PE [5]. Previous studies have shown that ruling out PE according to Wells score and D-dimer levels could substantially reduce the misdiagnosis rate of PE [6]. The sensitivity of using D-dimer in diagnosing acute PE is as high as 92–100 %, but the specificity is relatively low (40–43 %) [6, 7]. Several factors including operation, trauma, tumor, pregnancy, infectious diseases, peripheral vascular diseases, and advanced age could increase D-dimer levels.
Infections generally involve the activation of the inflammatory and coagulation systems. Therefore, D-dimer levels also reflect the severity of inflammation. Community-acquired pneumonia (CAP) is a common infectious disease. The mortality rate of CAP is about 5.6 % [8]. D-dimer levels are significantly higher in patients who die from critical CAP compared with surviving ones [9–11]. However, D-dimer levels of 0–4 mg/L are not specific and could reflect either CAP or PE [12].
Therefore, the aim of the present prospective cohort study was to examine the incidence and clinical features of patients preliminarily diagnosed with CAP and with increased D-dimer levels, and who finally were diagnosed with PE. CTPA was used as the gold standard to diagnose PE. Results of the present study could provide some clues for the early identification of patients at high risk of suffering from PE, hence improving the outcomes.
Patients and methods
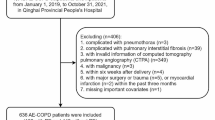
Study design and patients
This was a prospective cohort study of patients newly admitted to the Respiratory Department of the Tenth People’s Hospital Affiliated to Tongji University and diagnosed with CAP between May 2011 and May 2013. D-dimer levels were routinely examined. Patients with increased D-dimer levels with suspected PE underwent CTPA to clarify the presence of PE.
Inclusion criteria were (1) hospitalized patients with CAP newly admitted after May 2011; (2) increased D-dimer levels (>0.55 mg/L); and (3) chest pain, hemoptysis, and dyspnea that could not be alleviated by anti-inflammatory treatments. Exclusion criteria were (1) diagnosed with PE or deep venous thrombosis at admission; or (2) CTPA could not be performed due to the patient’s condition.
The study was approved by the ethical committee of the Tenth People’s Hospital Affiliated to Tongji University, and each participant provided a written informed consent.
Diagnostic criteria
CAP was diagnosed according to the diagnostic criteria described in the Guidelines of Diagnosis and Treatment of CAP issued by the Respiratory Society of the Chinese Medical Association. Patients were diagnosed with CAP in the presence of chest X-ray showing patchy or flake-like infiltrates or interstitial changes, with or without pleural effusion, and with at least one of the following four items (1) newly developed cough or expectoration, or aggravation of pre-existing respiratory diseases and with purulent sputum; with or without chest pain; (2) fever; (3) signs of lung consolidation and/or moist rale; and (4) WBC >10 × 109/L or <4 × 109/L, with or without nuclear left shift.
CTPA was used as the gold standard for the diagnosis of PE. The diagnosis of PE was performed according to direct and indirect signs. The direct signs were: partial filling defect or obstruction of the lumen, floating sign, saddle sign, irregular vascular wall, and thrombus calcification. The indirect signs were: uneven distribution of the pulmonary vessels, mosaic sign caused by uneven perfusion of the pulmonary parenchyma, signs of pulmonary infarction, signs of pulmonary hypertension including enlargement of the main pulmonary artery, and enlargement of the right ventricle.
The two major criteria for the diagnosis of acute PE were filling defect and complete obstruction (abrupt rupture) of the branches of the pulmonary artery. Other commonly found signs included partial obstruction or stenosis of the pulmonary artery branches, enlargement of the proximal lumen and narrowing of the distal lumen, and continuous retention of the contrast agent in the proximal artery at the late phase of angiography (venous phase).
Study procedures
Patients meeting the diagnostic criteria of CAP and the criteria for hospitalization were enrolled. D-dimer levels were measured routinely after admission. Patients with increased D-dimer levels were included as suspicious PE patients, and CTPA was performed. Patients were categorized into the PE and non-PE groups according to the CTPA results. PAOI (%) was calculated for the patients in the PE group.
D-dimer levels
Fasting venous blood (1.8 mL) was collected into sodium citrate anticoagulant tubes, and mixed immediately by reversing. Centrifugation at 2500 rpm for 10 min was performed 0.5 h later to separate plasma. A Symex CA-700 automatic blood coagulation analyzer was used; kits, standards, and quality control substances were provided by Siemens Healthcare Diagnostic Products GmbH (Erlangen, Germany). Immunoturbidimetry was used for the measurement of D-dimer levels. The normal range of D-dimer levels was 0–0.55 mg/L.
CTPA
A 64-detector row spiral CT (Lightspeed V, GE Healthcare, Waukesha, WI, USA) was used for CTPA. Patients were placed on the examination table in the supine position. CTPA covered the area from 1.5 cm above the aortic arch to the level of the diaphragm, with collimation of 1.25 mm and screw pitch of 1.0–1.5. Nonionic iodine solution (Ultravist, iodine concentration of 300 g/L) was used as the contrast agent (100–150 mL injected at 3.5–4.0 mL/s). Two experienced radiologists reviewed the images. PAOI was used to evaluate the severity of PE [13] according to: PAOI (%) = Σ(n × d)/40 × 100 %, where “n” indicates the number of arteries affected by embolism each side of the lung was divided into 10 pulmonary segments, each segment containing 10 segmental artery. Three arteries are in the upper right and left lobes each, two in the right middle lobe, two in the left lingular lobe, and five each in the lower left and right lobes. All emboli were scored 1. The score varied from 1 (obstruction of one segmental artery) to 20 (obstruction of the bilateral pulmonary arteries) and D refers to the severity of the embolism (1 indicating partial obstruction, and 2 indicating complete obstruction). The results are displayed as a percentage to reflect the decrease of the pulmonary vascular bed.
Data collection
The following information was recorded in detail: (1) general characteristics (sex and age); (2) comorbidities [coronary heart disease (CHD), hypertension, chronic obstructive pulmonary disease (COPD), diabetes, hyperlipidemia, tumor, lower limb varicosity, and history of recent forced rest (bedridden for more than 2 days within the past 2 weeks)]; (3) clinical presentations [chest pain, hemoptysis, shortness of breath, chest tightness, fever (temperature >38.5 °C)], syncope, and lower limb swelling; and (4) laboratory results [D-dimer, C-reactive protein (CRP), blood pH, partial oxygen pressure (PO2), partial carbon dioxide pressure (PCO2), troponin I (TnI), brain nutriaretic peptide (BNP), and fibrinogen (FIB)]. The last laboratory results before CTPA were used in the present study.
Statistical analyses
Since a small sample size could affect statistical power, the following data were stratified into dichotomous variables: age (≤60 years and >60 years), CRP [normal (0–10 mg/L) and increased], pH [normal (7.35–7.45), acidosis (<7.35), and alkalosis (>7.45)], PO2 [normal (80–100 mmHg) and hypoxia (<80 mmHg)], PCO2 [normal (35–45 mmHg), decreased (<35 mmHg), and increased (>45 mmHg)], TnI [normal (0–0.014 ng/mL) and increased (>0.014 ng/mL)], BNP [normal (0–179 pg/mL) and increased (>179 pg/mL)], FIB [normal (2–4 g/L), decreased (<2 g/L), and increased (>4 g/L)], and D-dimer [normal (0–0.55 mg/L) and increased (>0.55 mg/L)].
SPSS 19.0 (IBM, Armonk, NY, USA) was used for the statistical analyses. Non-normally distributed continuous data are presented as median and were analyzed using non-parametric tests. Correlation between D-dimer levels and PAOI was evaluated using the Pearson correlation analysis. Univariate analyses were performed using the Pearson χ 2 test to obtain odds ratios (OR) and 95 % confidence intervals (CI). For the multivariate analysis, PE was the dependent variable and all potential risk factors (stratified as above) were used as independent variables. The backward (likelihood ratio) logistic regression was performed to identify the independent risk factors for PE, as well as the corresponding OR and 95 % CI. The significance level to enter the multivariate analysis was p < 0.05 for the variables to enter the regression. Two-sided p values <0.05 were considered significant.
Results
Characteristics of the patients
A total of 2387 hospitalized CAP patients were enrolled, among which 724 (30.3 %) displayed increased D-dimer levels. Three hundred and eighty-nine (53.7 %) of the 724 patients were males, and 335 (46.3 %) were females. CTPA was performed for 139 patients [66 males (47.48 %) and 73 females (52.52 %), age range of 22–87 years], according to our clinical experience and the criteria described above. Eighty patients [40 males (50 %) and 40 females (50 %), median age of 72 years] were diagnosed with PE. Fifty-nine patients [26 males (44.1 %) and 33 females (55.9 %), median age of 69 years] were in the non-PE group (Table 1).
D-dimer levels in the PE and non-PE groups
For the 724 CAP patients with increased D-dimer levels, the median level was 0.91 mg/L. For the 139 patients suspected with PE and who underwent CTPA examination, the median level was 1.99 mg/L. For the 80 patients with PE, the median level was 2.83 mg/L. For the 59 patients in the non-PE group, the median level was 1.41 mg/L. The distribution of D-dimer levels was significantly higher in the PE group compared with the non-PE group (Fig. 1).
PAOI in the PE group
Sixteen (20 %), 48 (60 %), and six (7.5 %) patients were with PAOI of 1–10 %, 10–30 %, and >60 %, respectively (Fig. 2). Figure 3 shows that there was no significant correlation between D-dimer levels and PAOI (r = 0.131, p = 0.245).
Univariate analyses of the risk factors for PE
As shown in Table 2, there was no significant correlation between sex and PE. However, age >60 years was a possible risk factor for PE in patients with CAP and increased D-dimer levels (p = 0.021). A total of 87.1 % of the patients were with comorbidities including CHD, hypertension, COPD, tumor, lower limb varicosity, hyperlipidemia, and recently being bedridden. Having three or more comorbidities was a possible risk factor for PE (p < 0.05, OR 2.53–3.54). The incidence of PE was 76.0 % for patients with more than three comorbidities (Table 2). Chest pain, shortness of breath, hemoptysis, and fever were possible risk factors for the development of PE (p < 0.05). The incidence rate of PE was 69.1 % for patients with shortness of breath. No significant correlation was found between chest tightness, syncope, or lower limb swelling and the development of PE (p > 0.05) (Table 2). Increased TnI, decreased PO2, and increased CRP were possible risk factors for the development of PE (p < 0.05). The incidence rate of PE was 69.0, 66.3, and 70.2 % for the patients with increased TnI, decreased PO2, and increased CRP, respectively (Table 2).
Multivariate analysis of the risk factors for PE
As the number of comorbidities was calculated by adding the number of comorbidities, this factor was excluded because it was a covariate. Therefore, the multivariate logistic regression was performed with the other 24 variables as the independent variables, and PE as the dependent variable. The dichotomous variables were directly included into the regression model, while quantitative data were stratified and then included in the model. After 21 iterations, 11 variables and 1 constant term were obtained for the regression equation (Table 3). These 11 variables included age, CND, COPD, hyperlipidemia, lower limb varicosity, chest pain, shortness of breath, hemoptysis, chest tightness, fever, and TnI levels (Table 3).
Discussion
D-dimer is widely used for the preliminary screening of PE. The incidence of embolus in the main pulmonary artery increases significantly when the level of D-dimer increases to >4 mg/L [14]. Previous studies have reported that for patients with PE and D-dimer levels ≥4.2 mg/L, the overall mortality rate and the incidence of life-threatening PE or hemorrhage events within 15 days were significantly higher [15]. However, the use of D-dimer is limited as it is a non-specific biomarker. Milbrandt et al. [16] studied 900 patients with CAP and increased D-dimer levels, and found that the levels of D-dimer were increased (>5 mg/L) in patients with severe pneumonia, while patients with D-dimer levels <0.5 mg/L had better prognoses. These findings showed that increased D-dimer levels could be found in both CAP and PE. It is important to early identify patients with PE among the patients with CAP and increased D-dimer levels in order to improve their outcomes.
In the present study, 2378 hospitalized CAP patients were studied. Seven hundred and twenty-four (30.3 %) patients were with increased D-dimer levels. CTPA was performed for 139 patients with suspicion of PE, and finally diagnosed 80 patients with PE (80/2387, 3.35 %). These 80 patients had significantly higher D-dimer levels (median of 2.83 mg/L) than those in the non-PE group (median of 1.41 g/L). Multivariate analysis showed that age, CHD, COPD, lower limb varicosity, chest pain, shortness of breath, hemoptysis, fever, and increased level of TNI were independent risk factors for PE.
The severity of PE directly affects the prognosis of the patients. A previous study has shown that PAOI, which is correlated with arterial blood gas distribution, could be used to evaluate the severity of PE [17]. Another study has shown that PAOI was inversely correlated with PaO2; PAOI higher than 60 % reflects more severe damages to the pulmonary ventilation function [18]. In the present study, prospective observation of the CAP patients who were eventually diagnosed with PE by CTPA was performed, and 7.5 % of the 80 PE patients were with PAOI higher than 60 % (reflecting severe disease). Delayed treatment for such patients due to misdiagnosis could result in adverse events or even sudden death. Most (80 %) of the patients were with PAOI lower than 30 %, suggesting that they were with relatively mild disease, and could achieve good prognosis after treatments.
Wiener et al. [19] have shown that the incidence of PE was increased dramatically when CTPA was used in PE diagnosis (by 81 %), while the mortality rate of PE did not decrease substantially. This suggests that the use of CTPA reveals a great number of asymptomatic, non-life threatening emboli that have no clinical significance, while the incidence of anti-coagulation-related complications is increased greatly (by 71 %). These results suggest that the high diagnostic sensitivity of CTPA could induce over-diagnosis and over-treatment of PE.
Previous studies [20] have shown that several factors including smoking, hypertension, diabetes, hyperlipidemia, cardiac dysfunction, and COPD are risk factors for PE and deep venous thrombosis. The findings of the present study showed that CHD, COPD, hypertension, tumor, hyperlipidemia, lower limb varicosity, and a recent history of being bedridden were independent risk factors for PE in patients preliminarily diagnosed with CAP, in accordance with previous studies. The present study did not find the correlation between diabetes and PE; however, as only a relatively small number of patients was included, the features of the individual patients could affect the evaluation of the risk factors substantially, and thus could mask the effects of diabetes.
In the present study, 77.5 % of the patients were aged >60 years, among which 87.1 % had comorbidities. The results showed that age >60 was an independent factor for PE (OR 11.6). Previous studies have shown that the in-hospital mortality rate in aged patients was 10-fold of the rate in young patients [21]. All the patients selected in the present study were hospitalized CAP patients. Among patients who met the criteria for hospitalization, there were many patients being older than 60 years and with comorbidities. The number of comorbidities was also shown to be an independent risk factor for PE, suggesting that the presence of any three comorbidities in a single patient could increase the risk of developing PE by 3.5 folds compared with patients with less than three comorbidities. The mechanisms for this observation could be related to the damages to the vascular epithelial cells, blood flow stasis, hyper-coagulation status, and fibrinolytic dysfunction. However, studies on these mechanisms are lacking. Lower limb varicosity, being bedridden, and lower limb venous dysfunction are closely associated with deep venous thrombosis and PE [22, 23]. In the present study, we also found that a recent history of being bedridden was an independent factor for the development of PE.
The clinical symptoms and signs of PE are generally non-specific, which is also the major causes of misdiagnosis of PE. Chest pain, dyspnea, and hemoptysis have been acknowledged as the triad signs of PE; however, recent studies have shown that only 20 % of the PE patients display all three signs simultaneously [24], and that this proportion is even lower in Chinese patients (5 %) [21]. The findings of the present study showed that chest pain, hemoptysis, shortness of breath, and fever were risk factors for PE. However, these symptoms could also been found in pneumonia, suggesting that CAP and PE share some common signs. Rutschman et al. [25] performed a study in patients with COPD and PE, and found that PE patients were with higher frequency of chest pain and syncope, while the frequency of cough was much lower.
The present study also showed that fever was an independent risk factor for PE. Multivariate regression showed that the OR of fever was 0.001, suggesting that fever is a protective factor and indicating that patients with temperature >38.5 °C should be considered as CAP rather than PE, which was in accordance with previous findings [26].
Compared with pneumonia, PE could directly obstruct the pulmonary artery to induce pulmonary circulation disorders and respiratory dysfunctions, thus syncope and even shock could be observed. Indeed, acute right ventricular dysfunction could affect the filling of the left ventricle, and thus reduce the cardiac output, which consequently reduces the blood supply to cerebral arteries. In addition, PE aggravates the cardiac load, which could result in instable hemodynamics and arrhythmia, and thus induce syncope. Finally, PE could induce vascular vasovagal reflex and thus induce neurocardiogenic syncope.
Several laboratory parameters including D-dimer, homocysteine, BNP, and TnI have already been used in the early diagnosis, risk assessment, and treatment efficacy evaluation of PE [1–4]. The findings of the present study showed that CRP, PO2, and TnI were risk factors for PE. As an important marker for infection, CRP was found to be an independent risk factor for PE in the present study (incidence 70.2 %, OR 2.257). To our knowledge, this is the first study reporting an association between CRP and PE, and further studies are needed to verify this association. Decreased PO2 was also found to be an independent risk factor for PE (OR 2.4). The major mechanism for inducing PE is that pulmonary ischemia could result in increased ventilation/perfusion ratio and thus reduced PO2; however, such mechanisms need to be further investigated in patients preliminarily diagnosed with CAP. TnI is generally used as a biomarker for myocardial damages and plays an important role in diagnosing, risk stratification, treatment efficacy evaluation, and prognosis prediction of acute coronary syndromes [27]. In patients with PE, the occlusion of the pulmonary vascular bed will increase the pulmonary arterial pressure, the right ventricular afterload, and the tension of the right ventricular wall, which will result in relatively insufficient blood supply of the myocardium of the right ventricle and increase the oxygen consumption of the myocardium of the right ventricle, consequently inducing right ventricular ischemia. In addition, the dilation of the right ventricle will result in a left-shift of the interventricular septum, which will reduce the volume and ejection of the left ventricle, consequently resulting in insufficient blood supply for myocardium to aggravate myocardial damages. Increased TnI levels are associated with the mortality rate of PE, and has been regarded as an independent predictor for adverse events [28]. In the present study, we also found that TnI was an independent risk factor for PE; the risk of developing PE was increased to 2.66-fold.
There are several limitations to the present study. The sample size was small, and the use of some cut off points (e.g. 60 years for age) could have resulted in some subgroups being small. Some patients died in a short-term due to fast progression of their disease, or did not undergo CTPA examination due to other reasons, and could not be included. In addition, because of its high cost, CTPA was performed only in patients with a high suspicion of PE, and it is possible that some patients were missed. Some patients died from CAP before measuring D-dimer levels, probably underestimating PE incidence. Finally, some patients have been initially misdiagnosed as CAP while they really had PE, and other patients had both CAP and PE, leading to a delayed diagnosis. However, the misdiagnosis rate was not assessed in the present study. Further studies are warranted to verify our findings.
All the patients included in the present study were preliminarily diagnosed with CAP and with increased D-dimer levels. On one hand, PE patients could be misdiagnosed with CAP due to atypical presentation; on the other hand, patients with severe pneumonia could also develop systemic coagulation-fibrinolytic system disorders, which will add to the pre-existing risk factors for PE and thus finally cause PE. Further studies are needed to clarify the exact mechanisms. Nevertheless, the present study proposes a useful strategy for detecting PE using D-dimer screening. When combined with the symptoms, it allows the identification of the patients who are most likely to have PE. The use of this approach could reduce the use of unnecessary and expensive diagnostic testing, and might reduce the cost of diagnosis.
In conclusion, for hospitalized patients with CAP and elevated D-dimer levels, PE should be considered for those >60 years; with CHD, COPD, or lower limb varicosity; with chest pain, shortness of breath, hemoptysis, increased TNI, or low fever.
References
Konstantinides SV, Torbicki A, Agnelli G et al. (2014) ESC guidelines on the diagnosis and management of acute pulmonary embolism. Eur Heart J 35(43):3033–3069, 3069a–3069k. doi:10.1093/eurheartj/ehu283
Jaff MR, McMurtry MS, Archer SL et al (2011) Management of massive and submassive pulmonary embolism, iliofemoral deep vein thrombosis, and chronic thromboembolic pulmonary hypertension: a scientific statement from the American Heart Association. Circulation 123(16):1788–1830. doi:10.1161/CIR.0b013e318214914f
Goldhaber SZ, Bounameaux H (2012) Pulmonary embolism and deep vein thrombosis. Lancet 379(9828):1835–1846. doi:10.1016/S0140-6736(11)61904-1
Busse LW, Vourlekis JS (2014) Submassive pulmonary embolism. Crit Care Clin 30(3):447–473. doi:10.1016/j.ccc.2014.03.006
Huang W, Anderson FA, Spencer FA, Gallus A, Goldberg RJ (2013) Risk-assessment models for predicting venous thromboembolism among hospitalized non-surgical patients: a systematic review. J Thromb Thrombolysis 35(1):67–80. doi:10.1007/s11239-012-0780-0
Righini M, Van Es J, Den Exter PL et al (2014) Age-adjusted D-dimer cutoff levels to rule out pulmonary embolism: the ADJUST-PE study. JAMA 311(11):1117–1124. doi:10.1001/jama.2014.2135
Stein PD, Hull RD, Patel KC, Olson RE, Ghali WA, Brant R, Biel RK, Bharadia V, Kalra NK (2004) D-dimer for the exclusion of acute venous thrombosis and pulmonary embolism: a systematic review. Ann Intern Med 140(8):589–602
Yu H, Rubin J, Dunning S, Li S, Sato R (2012) Clinical and economic burden of community-acquired pneumonia in the Medicare fee-for-service population. J Am Geriatr Soc 60(11):2137–2143. doi:10.1111/j.1532-5415.2012.04208.x
Snijders D, Schoorl M, Schoorl M, Bartels PC, van der Werf TS, Boersma WG (2012) D-dimer levels in assessing severity and clinical outcome in patients with community-acquired pneumonia. A secondary analysis of a randomised clinical trial. Eur J Intern Med 23(5):436–441. doi:10.1016/j.ejim.2011.10.019
Salluh JI, Rabello LS, Rosolem MM, Soares M, Bozza FA, Verdeal JC, Mello GW, Castro Faria Neto HC, Lapa ESJR, Bozza PT (2011) The impact of coagulation parameters on the outcomes of patients with severe community-acquired pneumonia requiring intensive care unit admission. J Crit Care 26(5):496–501. doi:10.1016/j.jcrc.2011.02.001
Jolobe OM (2013) Elevated D-dimer levels signify overlap between community-acquired pneumonia and pulmonary embolism. Eur J Intern Med 24(2):e18. doi:10.1016/j.ejim.2012.07.008
Karalezl A, Hasanoglu HC, Kaya S, Babaoglu E, Acikgoz ZC, Kanbay A (2009) Cut-off value of D-dimer in pulmonary thromboembolism and pneumonia. Turk J Med Sci 39:387–392
Qanadli SD, El Hajjam M, Vieillard-Baron A, Joseph T, Mesurolle B, Oliva VL, Barre O, Bruckert F, Dubourg O, Lacombe P (2001) New CT index to quantify arterial obstruction in pulmonary embolism: comparison with angiographic index and echocardiography. AJR Am J Roentgenol 176(6):1415–1420. doi:10.2214/ajr.176.6.1761415
Hochuli M, Duewell S, Frauchiger B (2007) Quantitative d-dimer levels and the extent of venous thromboembolism in CT angiography and lower limb ultrasonography. Vasa 36(4):267–274. doi:10.1024/0301-1526.36.4.267
Lobo JL, Zorrilla V, Aizpuru F, Grau E, Jimenez D, Palareti G, Monreal M, Investigators R (2009) D-dimer levels and 15-day outcome in acute pulmonary embolism. Findings from the RIETE Registry. J Thromb Haemost 7(11):1795–1801. doi:10.1111/j.1538-7836.2009.03576.x
Milbrandt EB, Reade MC, Lee M, Shook SL, Angus DC, Kong L, Carter M, Yealy DM, Kellum JA, Gen IMSI (2009) Prevalence and significance of coagulation abnormalities in community-acquired pneumonia. Mol Med 15(11–12):438–445. doi:10.2119/molmed.2009.00091
Ji Y, Sun B, Juggessur-Mungur KS, Li Z, Zhang Z (2014) Correlation of D-dimer level with the radiological severity indexes of pulmonary embolism on computed tomography pulmonary angiography. Chin Med J (Engl) 127(11):2025–2029
Metafratzi ZM, Vassiliou MP, Maglaras GC, Katzioti FG, Constantopoulos SH, Katsaraki A, Efremidis SC (2006) Acute pulmonary embolism: correlation of CT pulmonary artery obstruction index with blood gas values. AJR Am J Roentgenol 186(1):213–219. doi:10.2214/AJR.04.1320
Wiener RS, Schwartz LM, Woloshin S (2011) Time trends in pulmonary embolism in the United States: evidence of overdiagnosis. Arch Intern Med 171(9):831–837. doi:10.1001/archinternmed.2011.178
Duan SC, Yang YH, Li XY, Liang XN, Guo RJ, Xie WM, Kuang TG, Dai HP, Wang C (2010) Prevalence of deep venous thrombosis in patients with acute exacerbation of chronic obstructive pulmonary disease. Chin Med J (Engl) 123(12):1510–1514
Castelli R, Bergamaschini L, Sailis P, Pantaleo G, Porro F (2009) The impact of an aging population on the diagnosis of pulmonary embolism: comparison of young and elderly patients. Clin Appl Thromb Hemost 15(1):65–72. doi:10.1177/1076029607308860
Ramzi DW, Leeper KV (2004) DVT and pulmonary embolism: part I. Diagnosis. Am Fam Physician 69(12):2829–2836
Zhu T, Martinez I, Emmerich J (2009) Venous thromboembolism: risk factors for recurrence. Arterioscler Thromb Vasc Biol 29(3):298–310. doi:10.1161/ATVBAHA.108.182428
Wells PS (2005) The role of qualitative D-dimer assays, clinical probability, and noninvasive imaging tests for the diagnosis of deep vein thrombosis and pulmonary embolism. Semin Vasc Med 5(4):340–350. doi:10.1055/s-2005-922479
Rutschmann OT, Cornuz J, Poletti PA, Bridevaux PO, Hugli OW, Qanadli SD, Perrier A (2007) Should pulmonary embolism be suspected in exacerbation of chronic obstructive pulmonary disease? Thorax 62(2):121–125. doi:10.1136/thx.2006.065557
Nucifora G, Badano L, Hysko F, Allocca G, Gianfagna P, Fioretti P (2007) Pulmonary embolism and fever: when should right-sided infective endocarditis be considered? Circulation 115(6):e173–176. doi:10.1161/CIRCULATIONAHA.106.674358
Nagarajan V, Hernandez AV, Tang WH (2012) Prognostic value of cardiac troponin in chronic stable heart failure: a systematic review. Heart 98(24):1778–1786. doi:10.1136/heartjnl-2012-301779
Bova C, Pesavento R, Marchiori A, Palla A, Enea I, Pengo V, Visona A, Noto A, Prandoni P, Group TS (2009) Risk stratification and outcomes in hemodynamically stable patients with acute pulmonary embolism: a prospective, multicentre, cohort study with three months of follow-up. J Thromb Haemost 7(6):938–944. doi:10.1111/j.1538-7836.2009.03345.x
Acknowledgments
This study was funded by the National Natural Science Foundation of China (Nos. 81172229, 81472180, 81100018). We thank Dr. Changbao Zhang (Department of Radiology, Shanghai Tenth People’s Hospital, China) for his help with CTPA.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the ethical committee of the Tenth People’s hospital Affiliated to Tongji University and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Yunfeng Zhang and Qixing Zhou have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Zhang, Y., Zhou, Q., Zou, Y. et al. Risk factors for pulmonary embolism in patients preliminarily diagnosed with community-acquired pneumonia: a prospective cohort study. J Thromb Thrombolysis 41, 619–627 (2016). https://doi.org/10.1007/s11239-015-1275-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-015-1275-6