Abstract
Strokes can have a catastrophic impact on patients’ health-related quality of life (HRQoL). In addition to warfarin, two novel oral anticoagulants, i.e., dabigatran and rivaroxaban, have been approved to prevent strokes. This study aimed to use direct measures to elicit patient-reported utilities (i.e., preferences) for anticoagulant-related outcomes. A cross-sectional survey was administered to 100 patients taking warfarin in an anticoagulation clinic. Utilities for six long-term and four short-term anticoagulant-related health states were elicited by the visual analogue scale (VAS) and standard gamble (SG) methods. Health states with the highest SG-derived mean utility values were “well on rivaroxaban” (mean ± SD = 0.90 ± 0.15), “well on warfarin” (0.86 ± 0.17), and “well on dabigatran” (0.83 ± 0.18). Approximately half of the patients considered major ischemic stroke (−1.57 ± 6.77) and intracranial hemorrhage (−1.99 ± 6.98) to be worse than death. The percentages of patients who considered a particular health state worse than death ranged from 0 to 55 % among various health states assessed. The VAS had similar findings. Good logical consistency was observed in both VAS- and SG-derived utility values. Ischemic stroke and intracranial hemorrhage had a significant impact on patients’ HRQoL. Greater variation in patients’ preferences was observed for more severely impaired health states, indicating the need for individualized medical decision-making. In this study, both long-term and short-term health states were included in the utility assessment. The findings of this study can be used in cost-utility analysis of future anticoagulation therapies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Stroke remains the second leading cause of global mortality and accounts for approximately 10 % of all-cause mortality, leading to more than 6 million deaths at present and projected 8 million deaths per year in 2030 [1, 2]. Approximately 50 % of stroke survivors have life-long moderate and/or severe post-stroke disabilities that greatly impair their health-related quality of life (HRQoL) [2]. Therefore, stroke prophylaxis is crucial, especially in patients with atrial fibrillation (AF) and venous thromboembolism (VTE) [e.g., deep vein thrombosis (DVT)] who are at an increased risk of stroke [3, 4].
Oral anticoagulation therapies have been commonly used to prevent strokes, and warfarin has been the cornerstone for more than half a century [5]. Recently, several novel oral anticoagulants, e.g., dabigatran, rivaroxaban, apixaban, and edoxaban have been approved to prevent strokes in patients with AF or VTE in several countries. Studies have shown that patients on anticoagulation therapies may experience different levels of impaired outcomes, such as recurrent stroke and bleeding [6]. Some of these outcomes are associated with long-term physical disabilities that greatly impair patients’ HRQoL. Therefore, in addition to clinical outcomes, it is also important to assess patients’ preferences (i.e., utilities) for various health states related to anticoagulation therapies, which can provide insight into patient-perceived impact of stroke prophylaxis on their HRQoL.
Commonly used direct methods to assess patients’ utilities include rating scale, time trade-off (TTO) and standard gamble (SG) [7]. The rating scale method, e.g., the visual analogue scale (VAS), is easy to understand and administer. It is often used prior to other utility measures as a complement to familiarize patients with health states under evaluation. The TTO elicits patients’ utilities by assessing the amount of time in a perfect health state that is equivalent to a period of time in a poor health state. This method is often used to assist decision-making that involves trade-offs between longevity and quality of life. The SG, based on the axioms of expected utility theory (EUT) [8], elicits patients’ utilities by assessing how much risk they are willing to take to avoid staying in a poor heath state. This method has been advocated by some researchers because healthcare decisions (e.g., choices of stroke prophylactic therapies) often involve patients’ attitudes towards risks and uncertainties, which can be captured by the SG [9, 10].
Most previous utility studies focused only on warfarin treatment, and did not assess utilities for outcomes related to dabigatran or rivaroxaban [10, 11]. This study aimed to use the VAS and SG to elicit patients’ utilities for both long-term and short-term outcomes related to stroke prophylaxis using warfarin and the two novel oral anticoagulants that were available in the U.S. when this study was conducted, i.e., dabigatran and rivaroxaban.
Methods
Patient recruitment
A cross-sectional survey was administered to patients taking warfarin in an anticoagulation clinic (ACC) of a tertiary hospital from August to November in 2012. Prior to survey administration, two interviewers were trained to standardize the administration process and data collection procedure. Potentially eligible patients were identified by referral from the ACC pharmacists. To be eligible, participants had to be age 21 or older, on warfarin, able to comprehend English or Chinese, and able to understand the VAS and SG. Respondents who consented to participate were interviewed face-to-face in either English or Chinese depending on their language preference. The study was approved by the Singhealth Institution Review Board.
Data collection
A questionnaire was developed specifically for this study, which was composed of questions on patients’ socio-demographics (e.g., age, ethnicity, etc.) and clinical characteristics (e.g., duration of taking warfarin), as well as health state description cards, a VAS, and SG chance boards. In addition, patients’ international normalized ratio (INR) values in the past 3 months prior to the survey administration were retrieved from hospital databases.
Health state selection and descriptions
Six long-term and four short-term health states were selected based on their relevance to the oral anticoagulation therapies for the prophylaxis of stroke. The long-term health states included “well on warfarin”, “well on dabigatran”, “well on rivaroxaban”, major ischemic stroke, minor ischemic stroke and intracranial hemorrhage (ICH). Patients were told to assume that long-term health states would continue for the rest of their lives. The short-term health states included transient ischemic attack (TIA), major extracranial hemorrhage (ECH), minor ECH and myocardial infarction (MI). Patients were told that they would return to their good health after staying in a short-term health state for a pre-determined period. Perfect health and immediate death were used as anchoring health states.
The descriptions of health states (details described in Appendix 1 in supplementary material) included the common and important attributes of the health states assessed and were developed based on preference assessment guidelines [12, 13], medical textbooks, published literature and expert opinions (i.e., two researchers with Ph.D. degrees in pharmacy, two physicians with master’s degrees in medicine, a clinical pharmacist with a master’s degree in pharmacy and a Ph.D. candidate in pharmacy). The description for each health state consisted of one to six bullet points that described the health state’s important attributes, such as patients’ physical mobility in the health state. The descriptions were presented on cards in a neutral manner to reduce framing bias [14]. Each description card was numerically labeled on its reverse side to avoid potential labeling bias, as it was found that labels could have a significant impact on patients’ responses [15, 16].
Utility elicitation
Utilities for health states were elicited based on the procedures recommended by standard guidelines [7, 13, 14, 17]. The VAS followed by the SG was used to elicit utility values. The VAS is a vertical percentile scale anchored with 100 (most desirable health state) on the top and 0 (least desirable health state) at the bottom [7, 13, 14], with a higher value indicating higher desirability for a health state. In the SG method, chance boards were used as visual aids to elicit patients’ preferences. Details of utility elicitation were described in Appendix 2 in supplementary material.
Logical consistency
The logical consistency of SG- and VAS-derived utility values were assessed, i.e., whether the order of utility values corresponded to the levels of morbidities associated with each health state. It was hypothesized a priori that (1) the mean utility values of “well on warfarin”, “well on dabigatran” and “well on rivaroxaban” were higher than those of other long-term health states; (2) the mean utility values of major ischemic stroke and ICH were lower than those of minor ischemic stroke and TIA; and (3) the mean utility value of major ECH was lower than that of minor ECH.
Statistical analysis
Descriptive statistics were used to describe patients’ demographic and clinical characteristics, and their utility values. Utility values below zero were kept either as negative values or rounded up to zero for comparison with previous studies [9–11, 18]. Pearson χ 2 test and independent sample t test were used to compare the demographic and clinical characteristics of respondents and non-respondents, where appropriate. Wilcoxon signed-rank test was used to compare the utility values elicited by the SG and VAS and to assess the logical consistency of the SG-derived utility values. The logical consistency of the VAS-derived utility values was assessed by the paired-sample t test. All analyses were performed using SPSS version 19.0. The level of significance was set at probability p < 0.05.
Results
Patient characteristics
A total of 186 patients were approached, and 100 patients agreed to participate in the survey and completed the questionnaire, giving a response rate of 53.8 % (Table 1). Respondents had a mean ± SD age of 53.3 ± 12.7 years and had been taking warfarin for a mean ± SD duration of 7.8 ± 7.4 years. More than half of the respondents were male (58.0 %), Chinese (62.0 %), married (71.0 %), spoke English (66.0 %), and had completed secondary education (79.0 %). The most common indications for warfarin were AF and DVT (64.0 %). Compared with respondents, non-respondents were older (p = 0.005) and more likely to have AF (p = 0.01). The most common reasons for non-participation were lack of time (53.3 %), unable to understand the VAS or SG (16.3 %), and no interest (9.3 %).
Utility elicitation
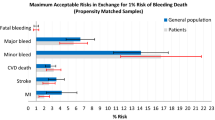
The mean ± SD utility values for all health states are presented in Table 2. Good logical consistency was found for the SG- and VAS-derived utility values. All three groups of a priori hypotheses were confirmed (all p < 0.001). Greater variation in utility values was observed among the health states with lower mean utility values. The SG-derived mean utilities were higher than the VAS-derived mean utilities for most health states. The health states with the highest SG-derived mean utility values were “well on rivaroxaban” (mean ± SD = 0.90 ± 0.15), “well on warfarin” (0.86 ± 0.17) and “well on dabigatran” (0.83 ± 0.18) whereas those with the lowest SG-derived mean utility values were major ischemic stroke (−1.57 ± 6.77) and ICH (−1.99 ± 6.98). The mean utilities of the four short-term health states ranged from 0.40 to 0.65. The VAS-derived mean utility values had similar rankings.
When the SG was used, 50 and 55 % of the respondents perceived major ischemic stroke and ICH, respectively, to be worse than death. Around 14 % of the respondents perceived major ECH and MI to be worse than death. When the VAS was used, similar results were found.
Discussion
In this study, both the VAS and SG showed good logical consistency, indicating that they were comprehensible measures. Compared to the VAS, the SG elicited higher mean utility values for most health states. This could be because the SG involved risks so that a number of risk-averse respondents were more likely to stay in a health state under evaluation instead of taking the risk of death [19]. As the prophylaxis of stroke involves risks of therapeutic failure and adverse effects, and the SG is based on the axioms of EUT [8], it might be a better measure of utility for anticoagulant-related outcomes than the VAS.
Consistent with previous studies [10, 11, 18], it was found that more than half of the respondents considered major ischemic stroke and ICH to be worse than death, indicating patients’ fear of strokes because of their severe impairment of patients’ HRQoL. In addition, consistent with previous studies [9–11, 18, 20], considerable variation in utilities for major ischemic stroke and ICH was observed. One explanation could be the individual difference in attitudes towards gambling between staying in severely impaired health states and using treatments that involve risks, emphasizing the need for individualized medical decision-making. Moreover, in this study, the mean utility value of warfarin was close to that of dabigatran. Similar finding was reported in a recent study, where there was no difference in HRQoL between patients who had been taking warfarin and those taking dabigatran for 12 months [21].
The SG-derived mean utilities for major and minor ischemic strokes in our study were similar to those reported in previous studies, which found that, when negative utility values were rounded up to zero, the mean utility value for minor stroke was 0.64 and those for major stroke ranged from 0.19 to 0.26, in patients at risk of stroke [10, 18]. Other studies, however, have reported different utility values for major and minor strokes [11, 20]. The variation could be the result of different measures used [19] or differences in health state descriptions. For example, while our study made use of different levels of speaking deficits to describe major and minor ischemic stokes, previous studies that did not include inability to speak as a post-stroke disability found higher mean utility values for major (ranging from 0.34 to 0.45) and minor (0.81) strokes [18, 20]. This is consistent with a previous study, which evaluated the impact of speech impairment on utility and found that the mean utility for major stroke reduced from 0.34 to 0.26 after speech deficits were considered [18]. Indeed, speech problems are common in stroke survivors [22, 23], and they can significantly impair patients’ communication and quality of life. Therefore, it is crucial to include speech deficits in the descriptions of post-stroke health states. In addition, the variation could be due to varying proportions of stroke survivors in study populations surveyed. For example, stroke survivors accounted for 25–50 % of participants in two previous studies [9, 18] whereas the respondents in our study were mostly patients who were at risk of but had not experienced strokes. It has been found that stroke survivors have adapted to stroke-related health states and are more likely to have higher utilities than non-stroke survivors [24].
This study has several strengths. First, utilities for novel oral anticoagulants were assessed, which may contribute to filling a gap in the literature, as previous studies mostly evaluated utilities for warfarin only [10, 11]. Second, utilities for short-term health states were evaluated using the cascading approach as it is inappropriate to evaluate these health states directly on the 0 (immediate death) to 1 (perfect health) scale [7, 13, 14]. Procedures for the cascading approach were described in details in our study, which may assist future studies that aim to evaluate utilities for short-term health states. Moreover, most previous studies focused on patient-reported utilities for major and minor strokes, and only one study evaluated utility for a short-term health state, i.e., major bleeding [10]. Our study evaluated the utilities for both long-term and short-term health states that are crucial outcomes in patients at risk of stroke. The findings of our study can provide useful information for future cost-utility analysis of anticoagulants, which may not only help patients and physicians make better decisions in clinical settings, but may also assist policy-makers in optimizing healthcare resource allocation.
This study has a few limitations. First, selection bias may exist because the patients with cognitive impairment (e.g., major stroke survivors) were excluded from the survey. As patients with post-stroke disabilities are more likely to be accustomed to their current health states and give higher utility values to severely impaired health states [24], exclusion of these patients may have underestimated utilities. Second, a number of participants in this study were already on warfarin, and may have been accustomed to the treatment, leading to inflated utilities for warfarin. Patients new to taking warfarin may have lower utilities for warfarin and higher utilities for dabigatran and rivaroxaban. Third, patients taking dabigatran or rivaroxaban were not surveyed and they may have different preferences from those participated in this study.
In conclusion, ischemic stroke and ICH can severely impact patients’ HRQoL, with a large number of patients considering them worse than death. Proportions of patients considering other health states worse than death ranged from 0 to 14 %. Greater variation in patients’ preferences was observed for more severely impaired health states, indicating the need for individualized medical decision-making. The findings of this study may assist medical decision making and can be used in future cost-utility analysis of anticoagulation therapies.
References
World Health Organization (2008) The top 10 causes of death. http://www.who.int/mediacentre/factsheets/fs310/en/index.html. Accessed 25 July 2013
World Health Organization (2004) The global burden of disease. http://www.who.int/healthinfo/global_burden_disease/2004_report_update/en/index.html. Accessed 25 July 2013
DE Singer, Albers GW, Dalen JE, Go AS, Halperin JL, Manning WJ (2004) Antithrombotic therapy in atrial fibrillation: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest 126:429S–456S
Sorensen HT, Horvath-Puho E, Pedersen L, Baron JA, Prandoni P (2007) Venous thromboembolism and subsequent hospitalisation due to acute arterial cardiovascular events: a 20-year cohort study. Lancet 370:1773–1779
Ansell J, Hirsh J, Poller L, Bussey H, Jacobson A, Hylek E (2004) The pharmacology and management of the vitamin K antagonists: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest 126:204S–233S
Baber U, Mastoris I, Mehran R (2014) Balancing ischaemia and bleeding risks with novel oral anticoagulants. Nat Rev Cardiol 11:693–703
Drummond MF (2005) Methods for the economic evaluation of health care programmes, 3rd edn. Oxford University Press, New York
von Neumann J, Morgenstern O (1944) Theory of games and economic behaviour, 1st edn. Princeton University Press, Princeton
Hallan S, Asberg A, Indredavik B, Wideroe TE (1999) Quality of life after cerebrovascular stroke: a systematic study of patients’ preferences for different functional outcomes. J Intern Med 246:309–316
Robinson A, Thomson R, Parkin D, Sudlow M, Eccles M (2001) How patients with atrial fibrillation value different health outcomes: a standard gamble study. J Health Serv Res Policy 6:92–98
Gage BF, Cardinalli AB, Owens DK (1996) The effect of stroke and stroke prophylaxis with aspirin or warfarin on quality of life. Arch Intern Med 156:1829–1836
Froberg DG, Kane RL (1989) Methodology for measuring health-state preferences–I: measurement strategies. J Clin Epidemiol 42:345–354
Furlong W, Feeny D, Torrance GW, Barr R, Horsman J (1990) Guide to design and development of health-state utility instrumentation. The McMaster University. http://www.chepa.org/Files/Working%20Papers/WP%2090-9.pdf. Accessed 3 Jan 2013
Torrance GW (1986) Measurement of health state utilities for economic appraisal: a review. J Health Econ 5:1–30
Brazier J, Ratcliffe J, Salomon JA, Tsuchiya A (2007) Measuring and valuing health benefits for economic evaluation, 1st edn. Oxford University Press, New York
Froberg DG, Kane RL (1989) Methodology for measuring health-state preferences–III: population and context effects. J Clin Epidemiol 42:585–592
Gudex C (1994) Standard gamble user manual: props and self-completion methods. The University of York. http://www.york.ac.uk/media/che/documents/papers/occasionalpapers/CHE%20Occasional%20Paper%2021.pdf. Accessed 3 Jan 2013
Samsa GP, Matchar DB, Goldstein L et al (1998) Utilities for major stroke: results from a survey of preferences among persons at increased risk for stroke. Am Heart J 136:703–713
Read JL, Quinn RJ, Berwick DM, Fineberg HV, Weinstein MC (1984) Preferences for health outcomes. Comparison of assessment methods. Med Decis Making 4:315–329
Shin AY, Porter PJ, Wallace MC, Naglie G (1997) Quality of life of stroke in younger individuals: utility assessment in patients with arteriovenous malformations. Stroke 28:2395–2399
Monz BU, Connolly SJ, Korhonen M et al (2013) Assessing the impact of dabigatran and warfarin on health-related quality of life: results from an RE-LY sub-study. Int J Cardiol 168:2540–2547
Chenaitia H, Lefevre O, Ho V et al (2013) Emergency medical service in the stroke chain of survival. Eur J Emerg Med 20:39–44
El Hachioui H, van de Sandt-Koenderman MW, Dippel DW, Koudstaal PJ, Visch-Brink EG (2011) A 3-year evolution of linguistic disorders in aphasia after stroke. Int J Rehabil Res 34:215–221
Post PN, Stiggelbout AM, Wakker PP (2001) The utility of health states after stroke: a systematic review of the literature. Stroke 32:1425–1429
Acknowledgments
We would like to acknowledge the National University of Singapore for providing us with a research Grant.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wang, Y., Xie, F., Kong, M.C. et al. Patient-reported health preferences of anticoagulant-related outcomes. J Thromb Thrombolysis 40, 268–273 (2015). https://doi.org/10.1007/s11239-015-1191-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-015-1191-9