Abstract
Computed tomographic pulmonary angiography (CTPA) has a high sensitivity for diagnosing filling defects in subsegmental pulmonary arteries. The adoption of CTPA as the prefered diagnostic modality for the diagnosis of pulmonary embolism (PE) has led to an increased rate of PE diagnosis. However, the case fatality rate is lower and the mortality rate of PE has remained unchanged despite this rise in PE diagnosis suggesting that the disease is of lesser severity. There continues to be clinical equipoise on whether patients diagnosed with isolated subsegmental PE (SSPE) require anticoagulation or can be managed conservatively if the presence of deep vein thrombosis (DVT) has been excluded. Recent recommendations from the European Society of Cardiology suggest an individualized approach for the management of patients with newly diagnosed SSPE based on the risk/benefit ratio of anticoagulation and the presence of lower limb DVT. Prospective data evaluating the safety and efficacy of management strategies for SSPE is needed in order to determine the optimal management of these patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Pulmonary embolism (PE) is a common disease causing significant morbidity and mortality in the United States [1]. For decades clinicians have been taught that untreated PE has a high mortality rate and is associated with a high risk of recurrent venous thromboembolism (VTE) [2, 3]. The recent increasing availability of computed tomography has led to a significant increase of its use to diagnose many medical conditions including PE. The increasing adoption of multi-detector computed tomographic pulmonary angiography (CTPA) as the dominant test of PE diagnosis has improved the sensitivity of diagnosis of PE by allowing better imaging of smaller subsegmental vessels of the lung. This has led to a rise in the overall incidence of PE diagnosis (including PE isolated to the subsegmental pulmonary arteries) without an associated increase in mortality suggesting that the current diagnoses of PE may represent a more heterogeneous or less severe disease with a lower case fatality rate [4, 5]. Therefore, the clinical significance of PE’s isolated to the subsegmental pulmonary arteries (SSPE) is unclear and continues to be an area of debate.
Increasing use of CTPA leads to rising rates of SSPE
Ventilation-perfusion (V/Q) lung scanning was the non-invasive imaging procedure of choice in patients with suspected PE for decades. However, the majority of patients with suspected PE undergoing a V/Q scan have a non-diagnostic examination (low or intermediate probability V/Q scan results). More recently, advancements in CTPA have allowed this modality to become the modality of choice for the diagnosis of PE. The ease in interpretation with fewer non diagnostic scans, the ability to detect other diagnoses explaining the symptoms that prompted the investigation and their often easier availability than V/Q imaging has led to CTPA being increasingly used for PE diagnosis over time [6, 7]. Surveys of emergency physicians have demonstrated that CTPA is the preferred first line modality for the diagnosis of PE [8]. This increase in the use of CTPA for PE diagnosis coincides with increased reported rates of SSPE diagnosis. A recent cohort study of post-operative cancer patients has reported that the increased use of CTPA led to an rise in the rates of SSPE diagnosis (5.4 %; 95 % CI 4.1–6.7) without a change in the rates of central or fatal PE over time [6]. Furthermore, as advances in CTPA technology improve, the rates of SSPE diagnosis are likely to rise even further. Earlier studies used primarily 4-detector CTPA and had an isolated SSPE diagnosis rate of 5 %. Newer studies with more detectors CTPA has led to a progressive increase in the diagnosis of SSPE from this prior rate to a rate closer to 9 % of all PE [4]. A cohort study using 64-detector CTPA reported a rate of SSPE among patients with confirmed PE as high as 12 % [9]. A concern is that with increasing advancements in technology, reported rates of SSPE will become an increasing proportion of PE diagnoses increasing the importance of addressing this important knowledge gap and determining whether these isolated SSPE are clinically important and relevant. Finally, this rise in PE diagnosis has occurred despite a push towards higher in-hospital deep vein thrombosis (DVT) thromboprophylaxis compliance and a lack of evidence that the risk factors for VTE have increased concurrent to the rate of diagnosis which makes it seem improbable that the increase in diagnosis of PE is related to a change in the population and points more toward the role of CTPA imaging [10].
Are SSPE clinically important?
The clinical impact of a SSPE diagnosis is unknown [4, 5, 11]. The increased incidence of SSPE with CTPA has been associated with a lower severity of illness and lower mortality of acute PE in the CTPA era [6, 12]. Similarly, a recent time trend analysis using the US Nationwide Inpatient Sample and Multiple Cause-of-Death databases showed that the introduction of CTPA to diagnose PE has led to an increased incidence of PE diagnosis but also to lower mortality and case fatality rates [13]. This improved outcome in PE patients diagnosed with CTPA might be due to an increased proportion of patients with isolated SSPE with unknown clinical significance. Furthermore, these intra-luminal filling defects in subsegmental pulmonary arteries may not represent true thrombus but could be imaging artifacts or other non-thrombotic material with uncertain clinical significance [11, 13]. The positive predictive value for SSPE detected by multi-detector CTPA has been previously reported to be only 25 % with a low inter-observer variability between radiologists (K: 0.38; 95 % CI 0.0–0.89) [14, 15]. Furthermore, a prior study also suggested that 11 % of SSPE diagnoses were deemed false positive when re-read by an experienced thoracic radiologist, reinforcing that all SSPE diagnosis should be reviewed by an experienced chest radiologist [16].
The clinical importance of SSPE remains debatable. SSPE were shown to be prevalent among patients with non-diagnostic V/Q scans. In the PIOPED study, 17 % of patients with a low probability V/Q scan had an isolated SSPE on pulmonary angiography [17]. Many prospective management cohort studies have demonstrated that patients with suspected PE and non-diagnostic V/Q scans can be safely managed without the use of anticoagulation provided there is negative compression ultrasonography of the lower extremities [16, 18, 19]. The rate of recurrent VTE in this group left untreated and managed with the above diagnostic strategy was 0.5 % (95 % CI 0.1–2.9 %) which is similar to the risk of recurrent VTE in patients with a negative pulmonary angiography (1.7 %; 95 % CI 1.0–2.7 %) [19, 20]. Therefore, many patients with suspected PE and non-diagnostic V/Q scans would presumably have been diagnosed with isolated SSPE if multi-detector CTPA were conducted and presumably these isolated SSPE don’t require anticoagulant treatment.
A randomized controlled trial comparing CTPA to V/Q scan for the management of patients with suspected PE has shown similar results [21]. CTPA resulted in a significantly greater number of PE diagnoses than did V/Q scans; hence, more patients diagnosed by CTPA were treated with anticoagulants. Despite this, the rate of VTE during the three-month follow-up period was similar in untreated patients (i.e. in whom PE was excluded) who were randomized to either diagnostic strategy suggesting that the additional cases of PE detected by CTPA were clinically unimportant.
A recent post hoc analysis combining data from two cohort studies showed that the risks of recurrent VTE were similar for patients with SSPE or more proximal PE receiving anticoagulation suggesting that SSPE might be clinically important [22]. However, the patients did not undergo lower limb ultrasonography so the number of patients studied that had undetected DVT and thus a higher risk of recurrent VTE is unknown [22]. This high risk of recurrent VTE is also discriptant with lower rates reported (1 %) in other studies suggesting that the risk of anticoagulation may exceed the benefits [23, 24]. A recent systematic review of the literature assessing the risk/benefit of anticoagulation in patients with SSPE reported a low rate of recurrent VTE (0 %) in patients left untreated while the risk of major bleeding episodes was 7 % when anticoagulated [24]. Concurrent DVT is an important predictor of recurrent VTE and therefore, imaging for DVT is an important component of the management of SSPE left untreated [25].
The current ACCP Chest guidelines from 2012 do not differentiate between isolated SSPE versus more proximal PE [26]. More recent guidelines such as those by the European Society of Cardiology take a more individualized stance regarding patients with SSPE and suggests that there may be a role for lower limb ultrasonography to rule out a DVT (which requires treatment) and that in a patient with isolated SSPE and negative leg ultrasonography, an individualized decision about anticoagulant therapy needs to be taken after careful assessment of the risk/benefit ratio [27]. Therefore, serial ultrasonography of the lower extremities might be a reasonable alternative to anticoagulation in low risk patients.
Incidental cancer-associated SSPE
Incidental diagnosis of isolated SSPE in cancer patients is another area of controversy. Malignancy is a well documented risk factor for PE [28]. SSPE is a common finding on staging scans and will be reported in up to 4 % of scans done for staging among cancer patients [29, 30].
While again there is a paucity of data as to the optimal management, unlike isolated symptomatic SSPE in non-cancer patients, the clinical practice has been to treat the incidental cancer-associated SSPE due to the underlying heightened risk or recurrent VTE. A recent survey demonstrated that 84 % of the oncologists surveyed would treat a single incidental SSPE but with significant variation in clinical practice between oncologists, palliative care physicians and chest physicians [31]. Similarly, a recent systematic review of the literature pooling patient-level data reported that the risk of recurrent VTE in patients with incidental cancer-associated SSPE despite anticoagulation was similar to those with more proximal PE [32]. In this analysis, the risk of recurrent VTE was 55 % in incidentally diagnosed cancer-associated SSPE left untreated. However, other prior studies have reported no statistical significant difference in outcome in patients with symptomatic or incidental PE, more of which were SSPE [33]. Similarly, a cohort study has showed no overall survival difference in patients with incidental cancer-associated SSPE compared to those without PE [34]. Given the associated increased risk of major bleeding in this population, prospective research studies in this patient population are desperately needed to address this important knowledge gap.
SSPE: advancing the field
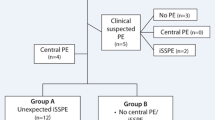
With conflicting studies and guidelines, there remains considerable clinical equipoise on the management of isolated symptomatic or incidental cancer-associated SSPE. Prospective studies providing safety data would be potentially practice changing if it could be shown that a group of patients being diagnosed with PE could be managed more conservatively without anticoagulation. This would allow these patients to avoid the inconvenience and known risks and complications of systematic anticoagulation [35]. The lack of good quality prospective evidence in this area can be demonstrated by the recent attempt by the Cochrane Collaboration Peripheral Vascular Disease Group to review the topic of SSPE treatment. They found no RCT data and therefore were unable to include any data in their study or make any meaningful practice suggestions [36]. Only one known prospective management cohort study is currently recruiting patients with isolated symptomatic SSPE and withholding anticoagulation in patients with no DVT on lower extremity ultrasonography (NCT01455818).
In conclusion, there is still considerable clinical controversy with regards to the management of patients with isolated SSPE (symptomatic or incidental) associated with significant clinical practice variation. The practice of withholding anticoagulation in SSPE with serial negative leg dopplers is currently being assessed with a prospective trial and can be considered in low risk non-cancer patients with no deep vein thrombosis on serial ultrasonography of the lower limbs, especially if the patient is at high risk of major bleeding episodes.
References
Anderson FA Jr, Wheeler HB, Goldberg RJ, Hosmer DW, Patwardhan NA, Jovanovic B, Forcier A, Dalen JE (1991) A population-based perspective of the hospital incidence and case-fatality rates of deep vein thrombosis and pulmonary embolism. The Worcester study. Arch Intern Med 151:933–938
Dismuke SE (1986) Pulmonary embolism as a cause of death. The changing mortality in hospitalized patients. JAMA 255:2039–2042
Dalen JE, Alpert JS (1975) Natural history of pulmonary embolism. Prog Cardiovasc Dis 17:259–270
Carrier M, Righini M, Wells PS, Perrier A, Anderson DR, Rodger MA, Pleasance S, Le GG (2010) Subsegmental pulmonary embolism diagnosed by computed tomography: incidence and clinical implications. A systematic review and meta-analysis of the management outcome studies. J Thromb Haemost 8:1716–1722
Carrier M, Righini M, Le GG (2012) Symptomatic subsegmental pulmonary embolism: what is the next step? J Thromb Haemost 10:1486–1490
Auer RC, Schulman AR, Tuorto S, Gonen M, Gonsalves J, Schwartz L, Ginsberg MS, Fong Y (2009) Use of helical CT is associated with an increased incidence of postoperative pulmonary emboli in cancer patients with no change in the number of fatal pulmonary emboli. J Am Coll Surg 208:871–878
Wittram C, Meehan MJ, Halpern EF, Shepard JA, McLoud TC, Thrall JH (2004) Trends in thoracic radiology over a decade at a large academic medical center. J Thorac Imaging 19:164–170
Weiss CR, Scatarige JC, Diette GB, Haponik EF, Merriman B, Fishman EK (2006) CT pulmonary angiography is the first-line imaging test for acute pulmonary embolism: a survey of US clinicians. Acad Radiol 13:434–446
Pesavento R, de Conti G, Minotto I, Filippi L, Mongiat M, de Faveri D, Maurizi F, Dalla VF, Piovella C, Pagnan A, Prandoni P (2011) The value of 64-detector row computed tomography for the exclusion of pulmonary embolism. Thromb Haemost 105:901–907
Burge AJ, Freeman KD, Klapper PJ, Haramati LB (2008) Increased diagnosis of pulmonary embolism without a corresponding decline in mortality during the CT era. Clin Radiol 63:381–386
Goodman LR (2005) Small pulmonary emboli: what do we know? Radiology 234:654–658
DeMonaco NA, Dang Q, Kapoor WN, Ragni MV (2008) Pulmonary embolism incidence is increasing with use of spiral computed tomography. Am J Med 121:611–617
Wiener RS, Schwartz LM, Woloshin S (2011) Time trends in pulmonary embolism in the United States: evidence of overdiagnosis. Arch Intern Med 171:831–837
Stein PD, Fowler SE, Goodman LR, Gottschalk A, Hales CA, Hull RD, Leeper KV, Popovich J Jr, Quinn DA, Sos TA, Sostman HD, Tapson VF, Wakefield TW, Weg JG, Woodard PK, for the PIOPED II Investigators (2006) Multidetector computed tomography for acute pulmonary embolism. N Engl J Med 354:2317–2327
Ghanima W, Nielssen BE, Holmen LO, Witwit A, Al-Ashtari A, Sandset PM (2007) Multidetector computed tomography (MDCT) in the diagnosis of pulmonary embolism: interobserver agreement among radiologists with varied levels of experience. Acta Radiol 48:165–170
Perrier A, Desmarais S, Miron MJ, de Moerloose P, Lepage R, Slosman D, Didier D, Unger PF, Patenaude JV, Bounameaux H (1999) Non-invasive diagnosis of venous thromboembolism in outpatients. Lancet 353:190–195
Stein PD, Henry JW (1997) Prevalence of acute pulmonary embolism in central and subsegmental pulmonary arteries and relation to probability interpretation of ventilation/perfusion lung scans. Chest 111:1246–1248
Perrier A, Bounameaux H, Morabia A, de Moerloose P, Slosman D, Didier D, Unger PF, Junod A (1996) Diagnosis of pulmonary embolism by a decision analysis-based strategy including clinical probability, D-dimer levels, and ultrasonography: a management study. Arch Intern Med 156:531–536
Salaun PY, Couturaud F, Duc-Pennec LE, Lacut K, Le Roux PY, Guillo P, Pennec PY, Cornily JC, Leroyer C, Le CG (2010) Non-invasive diagnosis of pulmonary embolism. Chest 139:1294–1298
van Beek EJ, Brouwerst EM, Song B, Stein PD, Oudkerk M (2001) Clinical validity of a normal pulmonary angiogram in patients with suspected pulmonary embolism—a critical review. Clin Radiol 56:838–842
Anderson DR, Kahn SR, Rodger MA, Kovacs MJ, Morris T, Hirsch A, Lang E, Stiell I, Kovacs G, Dreyer J, Dennie C, Cartier Y, Barnes D, Burton E, Pleasance S, Skedgel C, O’Rouke K, Wells PS (2007) Computed tomographic pulmonary angiography vs ventilation-perfusion lung scanning in patients with suspected pulmonary embolism: a randomized controlled trial. JAMA 298:2743–2753
den Exter PL, Van EJ, Klok FA, Kroft LJ, Kruip MJ, Kamphuisen PW, Buller HR, Huisman MV (2013) Risk profile and clinical outcome of symptomatic subsegmental acute pulmonary embolism. Blood 122:1144–1149
Donato AA, Khoche S, Santora J, Wagner B (2010) Clinical outcomes in patients with isolated subsegmental pulmonary emboli diagnosed by multidetector CT pulmonary angiography. Thromb Res 126:e266–e270
Stein PD, Goodman LR, Hull RD, Dalen JE, Matta F (2012) Diagnosis and management of isolated subsegmental pulmonary embolism: review and assessment of the options. Clin Appl Thromb Hemost 18:20–26
Raskob GE (2013) Importance of subsegmental pulmonary embolism. Blood 122:1094–1095
Kearon C, Akl EA, Comerota AJ, Prandoni P, Bounameaux H, Goldhaber SZ, Nelson ME, Wells PS, Gould MK, Dentali F, Crowther M, Kahn SR (2012) Antithrombotic therapy for VTE disease: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 141:e419S–e494S
Konstantinides SV, Torbicki A, Agnelli G, Danchin N, Fitzmaurice D, Galie N, Gibbs JS, Huisman MV, Humbert M, Kucher N, Lang I, Lankeit M, Lekakis J, Maack C, Mayer E, Meneveau N, Perrier A, Pruszczyk P, Rasmussen LH, Schindler TH, Svitil P, Vonk NA, Zamorano JL, Zompatori M (2014) 2014 ESC Guidelines on the diagnosis and management of acute pulmonary embolism: The Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology (ESC)Endorsed by the European Respiratory Society (ERS). Eur Heart J 35:3033–3073
Nordstrom M, Lindblad B, Anderson H, Bergqvist D, Kjellstrom T (1994) Deep venous thrombosis and occult malignancy: an epidemiological study. BMJ 308:891–894
Dentali F, Ageno W, Becattini C, Galli L, Gianni M, Riva N, Imberti D, Squizzato A, Venco A, Agnelli G (2010) Prevalence and clinical history of incidental, asymptomatic pulmonary embolism: a meta-analysis. Thromb Res 125:518–522
Gladish GW, Erasmus JJ (2010) Unsuspected pulmonary emboli in oncology patients undergoing routine computed tomography imaging. J Thorac Oncol 5:759–760
Lim WY, Bozas G, Noble S, Hart S, Maraveyas A (2014) Anticoagulating the subsegmental pulmonary embolism in cancer patients: a survey amongst different medical specialties. J Thromb Thrombolysis. doi:10.1007/s11239-014-1143-9
van der Hulle T, den Exter PL, Meyer G, Planquette B, Soler S, Monreal M et al. (2014) Risk of recurrent venous thromboembolism and major bleeding in cancer-associated incidental pulmonary embolism amongst treated and untreated patients: a pooled analysis of 926 patients. Blood 124(21):590
Shinagare AB, Okajima Y, Oxnard GR, Dipiro PJ, Johnson BE, Hatabu H, Nishino M (2012) Unsuspected pulmonary embolism in lung cancer patients: comparison of clinical characteristics and outcome with suspected pulmonary embolism. Lung Cancer 78:161–166
O’Connell C, Razavi P, Ghalichi M, Boyle S, Vasan S, Mark L, Caton A, Duddalwar V, Boswell W, Grabow K, Liebman HA (2011) Unsuspected pulmonary emboli adversely impact survival in patients with cancer undergoing routine staging multi-row detector computed tomography scanning. J Thromb Haemost 9:305–311
Wysowski DK, Nourjah P, Swartz L (2007) Bleeding complications with warfarin use: a prevalent adverse effect resulting in regulatory action. Arch Intern Med 167:1414–1419
Yoo HH, Queluz TH, El (2014) Anticoagulant treatment for subsegmental pulmonary embolism. Cochrane Database Syst Rev 4:CD010222
Acknowledgments
Dr. Carrier is a recipient of a New Investigator Award from the Heart and Stroke Foundation of Canada and holds a T2 Research Chair in Cancer and Thrombosis form the University of Ottawa.
Conflict of interest
No relevant conflict of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ikesaka, R., Carrier, M. Clinical significance and management of subsegmental pulmonary embolism. J Thromb Thrombolysis 39, 311–314 (2015). https://doi.org/10.1007/s11239-015-1169-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-015-1169-7