Abstract
In recent years, almost all countries around the world face budget cuts in health spending, which force public and private hospitals in these countries to use their resources effectively and to provide more efficient health care. In this context, the present study evaluates hospital efficiency across 29 OECD countries between 2000 and 2010 and investigates the determinants affecting hospitals’ activities. In the first stage of the two-stage performance analysis, efficiency scores of the hospitals were measured by data envelopment analysis (DEA) while, in the second stage, Panel Tobit Analysis was used to identify the environmental factors that affect the efficiency scores obtained in the first stage. The paper also explores the changes in the factor efficiency compared to the previous years by decomposition through the Malmquist Productivity Index. In the first stage, it was found that the efficiency scores achieved after 2000 began to decline in 2004 and reached their lowest levels between 2009 and 2010. The highest slack values were found in the figures regarding tomography, MR, and nurses, respectively. In the second stage, due to the censored nature of the dependent variable obtained by DEA, in order to achieve consistent and unbiased estimators, the use of Panel Tobit Analysis was proposed. Estimations showed that, among the environmental factors that secondarily affect hospital efficiency, income, education and number of private hospitals affect efficiency in a positive way, while the effects of public and private health expenses and the number of public hospitals on such efficiency was negative.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
It is an inevitable phenomenon for organizations to perform performance assessment and, thus, to define more effective and efficient processes so as to increase their competitive advantages by ensuring continuity. Public and private hospitals both should make the health services they provide to society, as well as the use of the resources, more effective and more efficient. Particularly, the global financial and economic crises that occurred in recent years caused the countries to decrease their spendings on health care. Though health spending varies among nations, the average health expenditure per capita across the OECD countries increased by 4.1 % p.a. between 2000 and 2009, while this rate dropped by 0.2 % between 2009 and 2011. From 2009 to 2011, out of 34 OECD countries 11 countries decreased their health spendings (OECD 2013). This caused the countries to use the resources assigned to health sector in more effective ways. The challenge of providing health care without compromising on quality, even improving it by using their resources in more effective ways, made the governments to pursue the matter more rigorously.
In the light of the foregoing aspects, evaluation, improvement and analysis of health care performance provided by country at international levels, as well as discussing its shortages to ensure its efficiency and finally to level up hospital efficiency to advanced levels are all great importance. Traditional data envelopment analysis (DEA) is a commonly used technique by a decision making unit (DMU) in the calculation of relative overall efficiency. However, with this technique, only those variables that directly affect hospital efficiency can be taken into account and interpreted, whereas in the evaluation of health care performance of a country, some elements specific to that country such as economic and social elements also play a secondary role. Therefore, by using a two-stage analysis, it is important to examine the environmental variables that affect the overall hospital efficiency obtained by DEA during stage I in the second stage by using econometric models. However, because the efficiency scores obtained through the DEA model have a censored structure, parametric estimations of ordinary least square (OLS) regression to be used in the second stage will be biased and inconsistent. Efficiency analysis has become more extensive by examining the cross-section data by the years, and the use of Panel Tobit Analysis instead of traditional panel in the second stage will ensure that consistent and unbiased estimators are obtained.
Examining the hospital efficiency of countries by a one-stage analysis would be insufficient, and addressing just 1 year—as previous studies did—would limit our vision of the overall course. The aim of this study in which 10 years of data (2000–2010) regarding 29 OECD countries was used, is to thoroughly investigate hospital efficiency by using a two-stage performance rating. In the first stage of the study, assuming constant returns to scale (CRS), the hospital technical efficiency scores for each year and each country were obtained using DEA. The countries were ranked according to their efficiency in the health care sector so that efficient and inefficient countries be identified. Also, the changes in the individual efficiency of the countries for each year over a ten-year period were evaluated by the Malmquist Index, by which the total factor efficiency was decomposed. In the second stage of the study, since the dependent variable obtained by DEA has a censored structure, in order to obtain consistent and unbiased estimators Panel Tobit Analysis was proposed instead of traditional analysis. Also, which country-specific social and economic factors affected hospital efficiency were identified. As far as the others of the present studies are consulted, this research is among the first attempts to investigate the health care performances across OECD countries in such an extensive way.
The rest of the paper is organized as follows. The first section provides the literature reviews on the studies of hospital efficiency. This section is followed by the next section constituting the descriptions on data sets and variables used in the study. Then, the two-stage analysis and the methods used in each stage are explained. Following the detailed results and discussions of the analyses comes the final section, which consists of a summary of the contributions, conclusions and limitations of the study.
2 Literature Review
Achieving a high score of efficiency in performance assessment is a principal aim for any business, and this also applies to hospitals. Most studies evaluating hospital efficiency have employed a one-stage efficiency analysis, using DEA. Mobley and Magnussen (1998), Steinmann et al. (2004), Bhat (2005), Spinks and Hollingsworth (2009), Alexander et al. (2003), Sherman (1984), Grosskopf et al. (2006), Puig-Junoy (1998) and Retzlaff-Roberts et al. (2004) are among such studies. Puig-Junoy (1998) and Retzlaff-Roberts et al. (2004) are specifically among those that compare health care performance across OECD countries using DEA.
In addition to DEA in the analysis of hospital efficiency, there are other studies that how employed parametric or non-parametric methods. For example, Varabyova and Schreyögg (2013) obtained hospital efficiency scores through DEA and stochastic frontier analysis (SFA). Using two outputs and four inputs, their study investigated nine DEA models, six of them being input-oriented and the remaining three being output-oriented, and three SFA models, later to focus on the correlation between the results. In this comparison performed for 2007, it was found that there are closer results between those of output-oriented DEA models and those of SFA models, when compared to input-oriented models. Afonso and Aubyn (2005), on the other hand, have used two different non-parametric methods, Free Disposable Hull (FDH) and DEA, in the estimation of hospital efficiency scores. Hollingsworth and Wildman (2003) found that using only one method to estimate countries’ health care performances by the The World Health Organization (WHO) was a restricted effort in the report for the year 2000, and, instead, they reevaluated the efficiency of 191 countries by panel data, DEA, Malmquist, and SFA methods, using the data provided by the WHO.
In order to examine the efficiency changes by years in the one-stage efficiency measurement, Malmquist Productivity Index (MPI) is used in addition to DEA. Sahin et al. (2011) analyzed the effects of health transformation program on hospitals in Turkey between 2005 and 2008 by using DEA and Malmquist Index. For the period between 2002 and 2006, Chowdhury et al. (2014) have analyzed the performance of the hospitals in Ontario, and Chu (2011) did the same for the performance of Chinese hospitals using DEA and MPI. Weng et al. (2009) in their study of comparing the performances of hospitals, proposed a Panel-based extended DEA. They tested the validity of their proposed model with MPI.
Another group of studies that measures efficiency is that using a two-stage analysis. Such studies use the efficiency scores obtained through DEA in an econometric model in the second stage.
There are some other studies that employ OLS regression in the second stage of a two-stage analysis. Medin et al. (2011), in a study where they compared hospital efficiency, performed an international efficiency comparison among four Nordic countries and used DEA in the first stage and, then, OLS regression analysis in the second. Pelone et al. (2012), measured the technical efficiency of general practice across 20 regions of Italy first by using DEA, and then identified the contextual variables that affect such efficiency using regression analysis. Similarly, Gok and Sezen (2013) have obtained the efficiency scores of hospitals in Turkey by DEA in the first stage and analyzed the effects of such efficiency and structural quality on the satisfaction of the patients by regression analysis in the second stage using hospital efficiency as an explanatory variable.
Nevertheless, since the dependent variable consisting of the efficiency scores obtained through DEA is censored data, it makes the estimations done by OLS regression analysis both biased and inconsistent. Therefore, it’s better to have the estimations done by Tobit or truncated regression. Mitropoulos et al. (2013), the author who obtained the efficiency scores of Greek hospitals by DEA in the first stage, analyzed the effects of operational environment on hospital efficiency by truncated regression in the second stage. Nedelea and Fanin (2013), in their study on cost-effectiveness in US hospitals, used DEA in the first stage, and truncated regression in the second stage, using environmental variables as explanatory variables. Puig-Junoy (2000) used DEA in the first stage of his study on efficiency across 94 Catalan intensive care hospitals, and log regression in the second stage.
Moran and Jacobs (2013) is one of those studies that compare the efficiency of 32 OECD countries in terms of the health care provided to mental patients by employing a two-stage DEA method. For 2010, the efficiency of the countries was obtained through DEA in the first stage, and then the relation of environmental variables such as alcohol consumption, income, education, unemployment, etc. with the efficiency was identified by using Tobit regression analysis. Also in the study, countries were divided in clusters as efficient and inefficient using cluster analysis. Ancarani et al. (2009) investigated the effects of managerial perspectives on the efficiency of hospital wards’ in Italian hospitals. Adapting a two-stage approach, the author used DEA in the first stage, and Tobit regression in the second. Hu et al. (2012) in the first stage of their study where they investigated the effects of health insurance reform on the efficiency of Chinese hospitals, obtained the efficiency scores through DEA, and analyzed the relationship between the efficiency and the environmental variables by Tobit regression. Afonso and Aubyn (2011) measured the hospital efficiency across 21 OECD countries for 2005 by DEA, and then analyzed the relation between efficiency and environmental variables by Tobit regression. Similarly, Chilingerian (1995) evaluated the efficiency of 36 physicians working in the same hospital by using DEA in the first stage, and by Tobit regression in the second stage.
The second stage model that has been preferred by some studies doing health care performance comparison over a number of years is panel data analysis. Kjekshus and Hagen (2007) one of such studies, have measured, by a two-stage approach, if the alignment of 17 hospitals in Norway increased the efficiency. Evaluation the period between 1992 and 2000, the authors had obtained the hospital efficiency by DEA, and in the second stage they tested the effect of the unification on the efficiency by panel data analysis. Biorn et al. (2003) in their study of the Norwegian hospital sector, have analyzed the effects of a cost-based accounting system on hospital efficiency during 1992–2000 by employing the DEA method in the first and Panel regression in the second stage. Similarly, Kittelsen et al. (2008) have used the DEA in the first stage and a fixed effect model in the second stage to determine whether or not the centralization reform of the hospitals in Norway has any positive effect on the efficiency of the hospitals.
However, since the efficiency scores obtained in the first stage has a censored nature, Tobit Panel Analysis is required in the second stage instead of panel data analysis. Chen et al. (2005) have obtained the efficiency scores of Californian hospitals by DEA and by subtracting these scores from 1, they found the inefficiency scores for each hospital. In the second stage, they used Panel Tobit method to analyze the relationship between inefficiency scores and variables such as organization structure, management, demographics, and competition.
In this study, we used the DEA method in the first stage to obtain the efficiency scores, and in the second stage we used an econometric modeling approach to analyze the relationship between efficiency scores and country-specific socio-economic variables. Covering a 10-year period research across the OECD countries, this study has employed Panel Tobit Analysis in the second stage. Also, we analyzed the changes over years by decomposing them, using Malmquist Index.
3 Data and Variables
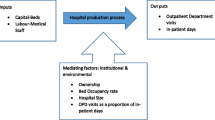
In this study, an available data set was used concerning 29 OECD countries for the period of 2000–2010. Completed as a two-stage performance evaluation study, DEA and Panel Tobit were used in the first and second stages, respectively. Further, the MPI values were computed for the panel data. DEA and Malmquist analyses were performed on five inputs and two outputs. These variables consist of controllable items that can directly affect health care services provided by a hospital. In the model, discharge rate and infant survival rate were used as health outcome measures. Improvement on countries’ health systems were denoted by increases in these variables. Five inputs were used as health care resources for production of health. These variables are health care equipment (beds, MRI, CI) and health workforce employed in hospitals (nurses, physicians) that provide more efficient health care services. In the Panel Tobit Analysis, at the second stage, environmental variables that affect hospital efficiency indirectly were used as independent variables. Such environmental variables are secondary (or indirect) variables including country-specific factors thought to impact health care performance in countries. In the identification of variables, the OECD reports published annually under the title of “Health At a Glance” (2012, 2013) (OECD 2012, 2013) as well as studies measuring hospital efficiency (Varabyova and Schreyögg 2013; Chowdhury et al. 2014; Afonso and Aubyn 2011; Greene 2004, b; Self and Grabowki 2003; Berger and Messer 2002) were used. The variables used in the models are presented along with their definitions in Table 1.
The data used in this study was taken from the World Data Bank, Eurostat, OECD statistics and the National Health System of Spain databases (The World Bank 2014; Eurostat 2014; OECD 2014; National Health System of Spain 2014). Figures for many of the variables we used in this study only covered up to 2010 in aforementioned institutional reports of 2014. Due to this limitation, this study could be done until 2010. The missing values for some countries going back 2 or 3 years were filled in by linear interpolation. Chile, Norway, Poland, Slovenia, and Sweden, due to the absence of variables were not included in the analyses. In the end, the size of the sample was limited to 29 OECD countries.
4 Methodology
4.1 Data Envelopment Analysis (DEA)
Data envelopment analysis (DEA), a non-parametric method, was first proposed by Farrell (1957) and then improved by Charnes et al. (1978) and Banker et al. (1984) thereby finding a larger application field. DEA is a mathematical programming method to measure the relative efficiency of decision-making units, using multiple inputs and outputs (Erdoğan and Samut 2013). In the efficiency measurement by DEA, there are two presumptions, variable return to scale (VRS) and constant returns to scale (CRS). In the studies on hospitals’ performance, the CCR model (Charnes, Cooper, and Rhodes) (Charnes et al. 1978) is preferred in that it gives better results. The reason for choosing CRS model in the analysis of hospital efficiency is because there is no restricting scale or effect on the relation of inputs and outputs (Gök and Sezen 2013). One common aim of all health care organizations is to provide high quality services using their resources, such as beds, personnel, etc. in the most minimal way. This shows that CCR input-oriented models are suitable to be used in the evaluation studies on the performance of a hospital (Weng et al. 2009). The controllability of inputs compared to outputs also requires the use of input-oriented DEA model in this study. An input-oriented DEA–CRS model that gives an efficiency score for n number of DMUs by using m outputs and s inputs is presented below:
subject to
In the model, DMUj gives outputs to yri by consuming an amount of input in xji. The weights of the outputs and inputs in the formula are shown in µr and vj, respectively. All inputs, outputs and all weights are considered as >0, and to obtain technical efficiency scores for n DMU, the program would be run n times (Cooper et al. 2011; Witte and Marques 2010). The obtained technical efficiency scores will take a value between 0 and 1, and if TE = 1, it means that DMU is technically efficient and that it produces on the production frontier. Scale efficiency, a component of technical efficiency, is the proportion of CRS to VRS, and if it is equal to 1, this means that the DMU is scale-efficient.
4.2 Malmquist Productivity Index (MI)
Malmquist Productivity Index (MI), a DEA-based non-parametric efficiency index, was first found by Malmquist (1953) and improved by Caves et al. (1982), Farë et al. (Färe and Grosskopf 1992, Färe et al. 1994). MI is a frontier analysis that measures the changes in total factor productivity and enables the evaluation of DMUs by years. The total factor productivity change (tfpch) is divided into two parts: technical change (techch) and technical efficiency change (effch) (Lovell 2003). Efficiency change is the measurement of effects of capturing best production fronts for both periods. Technical change gives the degree of progress arising from the innovations occurred between two periods (Ray 2004). Efficiency change is obtained by multiplying pure efficiency (pech), which measures managerial efficiency, with scale efficiency (sech), which measures whether DMUs are in fact working in an appropriate scale for them.
The distance functions are addressed in both ways, input- and output-oriented. The Malmquist TFP change index \(M_{h}^{t + 1}\) is expressed as follows, where \(x_{h}^{t} = \left( {X_{1ht} ,X_{2ht} , \ldots } \right)\) is the input vector, and \(y_{h}^{t} = \left( {Y_{1ht} ,Y_{2ht} , \ldots } \right)\) is the output vector that can be produced from the input vector (Färe and Grosskopf 1992):
If the computed TFP change index takes a value >1, then it is evident that TFP is increased from t until t + 1 period; and if it is <1, then TFP is decreased for the same duration.
4.3 Tobit Panel Analysis
In the regression models, where the change range of the dependent variable is somehow restricted, the variables that take values in a limited range are defined as “censored” or “truncated” data. If the observations outside of a certain range are excluded systematically from sample and completely lost, then they are called “truncated” data, and if the observations do not have any information on the dependent variable, but at least the independent variables could be observed, then they are called “censored” data (Davidson and MacKinnon 2003). If the observations resulted from the analysis of DEA are >1, then they would not be excluded from the sample as it was the with the truncated data. However, they cannot take their own values either and, thus, they are censored to 1 (Chilingerian 1995). In this context, since the dependent variable consisting of efficiency scores from the DEA is limited to [0,1] and that the independent variables that correspond to 1 can be observed, it has a censored structure.
Estimating a model with a censored dependent variable by the OLS method leads to biased and inconsistent results in parametric estimations (Greene 2003). Furthermore, DEA scores having a relative efficiency index, rather than an absolute index, and the correlation between the efficiency scores make the OLS regression invalid (Atkinson and Wilson 1995). For the foregoing reasons, Tobit regression, one of limited dependent variable models that takes a censored structure into account, is used in the present study.
For parameter estimations, the Maximum Likelihood Estimation (MLE) method is used in the Tobit model. Since the parameters obtained through MLE are non-linear, the predictions of the estimations are performed by iterations. Also, since it requires less time and fewer iterations as an iteration method, thus offering other advantages, the Newton–Raphson method has been utilised here (Jamil 2013).
Panel data means the observed data of N different sections at T different times, i.e. combination of cross-section data and time data. In this context, the basic formula of Panel Tobit used in this study is expressed as follows:
where subscript \(i\) defines the country and subscript \(t\) defines the time. \(\chi_{it}\) is the explanatory variable in the dimension of 1 × k and \(\beta\) is the parameter vector on the dimension of k × 1 (Baltagi 2008).
The error term in panel data application is generally defined as follows:
where \(\lambda_{i}\) is the unobservable individual effects and \(u_{it}\) is the unobservable individual and random effects. Individual effects are addressed in two different ways as follows:
If \(\lambda_{i}\) is assumed fixed for each individual, then it is referred to as a “Fixed Effect” estimator; or if it is considered to be picked up randomly from a probabilistic distribution, then it should be referred to as a “Random Effect” estimator (Thomas 2007).
Nevertheless, since the Tobit model is non-linear, using fixed effects in Panel Tobit Analysis would increase the αi as N is increased, thus causing incidental parameter problems and resulting in biased outcomes (Fernandez-Val and Weidner 2013). It has been emphasized that there is a problem related to the distribution of disturbance variance estimator with the fixed effect Tobit models beyond the incidental parameters problem (Greene 2004, b). Therefore, it would be more appropriate to use a random effect estimation for Panel Tobit.
The results of DEA and Malmquist in this study were obtained through WIN4DEAP (Coelli 1996) the results of Panel Tobit were obtained using LIMDEP and Eviews 7 programs.
5 Results and Discussion
This study investigates hospital efficiency at international level. The productivity structure across 29 OECD countries for 2000–2010 was investigated through a two-stage analysis. In the first stage of the study, DEA was used while, in the second stage, Panel Tobit Analysis was applied. Also, Malmquist Productivity Index values were computed for the panel data. While efficiency scores of DMUs were measured by DEA, evaluation of total factor productivity change by years was obtained by MI. Besides, by decomposing the total factor productivity, opportunity of a detailed analysis was provided. The results concerning the DEA model, MI, and the Panel Tobit appear in the following.
5.1 Results of DEA Model
The input-oriented DEA analysis across 29 OECD countries was conducted under CRS assumption. The hospital efficiency scores of the countries for 2000–2010 were obtained using 2 outputs and 5 inputs. Table 2 shows the technical efficiency scores for each country and descriptive statistics. When considering the average technical efficiency scores of the countries by years, it is seen that the increase achieved in efficiency scores began to decrease in 2004. Again, these scores declined substantially in 2009 and 2010, with values at 0.842 and 0.819, respectively. A basic reason for this can be the cuts in health spending across OECD countries, particularly between 2009 and 2011, due to the financial crisis (OECD 2013). Assessing the distribution of the countries based on the efficiency score ratings, it can be observed that the number of fully efficient countries reached 12 in 2004 but, afterward, the number dropped and finally totalled only 6 in 2010. The rate of the countries that have efficiency scores above the average in 2000 and 2001 was approximately 52 % and 59 %, respectively, and it even reached 65.5 % in 2003; yet, it began to decrease in later years, and finally in 2010 only 37.9 % of the countries had an efficiency score above the average.
The countries that were fully efficient during this 10-year period are Mexico, Turkey, and the United Kingdom. Moran and Jacobs (2013) also reached the conclusion, in their study on hospital efficiency for 2010, that Turkey and Mexico were efficient. From the perspective of our study, the main reason for this is that both Turkey and Mexico had the minimum length-of-stay values. Though it has an under-average efficiency score for all the years, Japan also has the maximum length of stay value. The OECD indicates that this is because Japan has a health care service payment structure that encourages the patients to stay in hospital for longer times (OECD 2013). Beside Japan, Iceland, France and Belgium have under-average efficiency scores for all the years.
An investigation into the input slacks of these countries revealed that there were slacks in the variables of beds, nurses, and MRI for Belgium; in the variable of nurses for France; in nurses, MRI, and CT for Iceland; and in beds, nurses, and CT variables for Japan for all years. It’s been found that physicians were used efficiently and that there are no capacity excesses in any of these countries.
Table 3 shows the input slacks averages for each year. In general, the highest slack values are on the CT, MRI and Nurses, respectively. In 2010, it can be seen that CT should be decreased by 6.492 averagely, MRI by 2.513, and Nurses by 2.707 units. Also, it is determined that in 2009, 14 countries and, in 2010, 18 countries have a CT excess. Again in 2009 and 2010, there was MRI excess in about 28 % of the countries. This tells us that most of the OECD countries have a slack capacity in their medical technology inputs. As for the health workforce, physicians work in full capacity, while nurses have a serious capacity excess. In 2009, there was a nurse slack in 15 countries out of 29 countries, and in 2010 this figure increased to 19 countries. In order to provide a more effective health service, inputs should be used in a more effective way to obtain better outputs. Therefore, it is important in terms of health performance to use that slack capacity, particularly in these three inputs.
5.2 Results of Malmquist Index
In this study, the 10-year productivity scores of these OECD countries were computed using input-oriented MI TFP. The analysis results of the tfpch, techch, effch, pech and sech for the countries are given in the Table 4. In the 10-year period under investigation, the general average tfpch of the countries was found at 0.978. Of this, 1.3 % resulted from decrease in technology, and 0.9 % from a decline in technical efficiency. During this period, 22 out of 29 countries have had an average tfpch value under 1.
The highest efficiency increase was scored in Greece by 2 %, owing to its efficiency score increase in the technological progress. Technical efficiency in Greece had decreased by 2.5 %, while its technological efficiency increased by 4.5 %. The country that has seen the biggest decrease in its efficiency during this 10-year period is Ireland. Hospital efficiency in this country decreased averagely by 11.9 %, while its technical efficiency decreased by 2.3 %, and its technological efficiency decreased by 9.9 %. The decrease in Ireland’s technical efficiency was entirely due to scale inefficiency. Greece needs to provide services in an appropriate scale, using optimal inputs. Pure efficiency in Ireland was constant, indicating that the source of such inefficiency was not managerial.
When considering the changes in the average factor productivity against the years, it is seen that there was either a slight decrease or non at all in each year (Table 5). The biggest decrease rate in the total factor productivity was seen in 2000–2001, decreasing by 6.2 % in 2001 compared to its previous year. The reason for this decrease was the decline in the technical efficiency by 7.7 % in 2001. This shows us that, in general terms, the countries did not make any progress in terms of technology. Similarly, the decrease in the countries total productivity still resulted from the lack of technological progress in 2001 and 2002. In 2009 and 2010, technological progress finally began to increase but, this time, technical efficiency dropped. The reason for the decrease by 0.9 % in the total productivity rate was the decrease in technical efficiency by 4.8, 4.5 % of which was caused by scale efficiency. This shows that the countries, in general, did not work in a scale fit to their capacities by 2009.
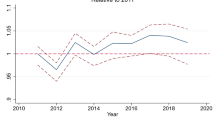
Figure 1 is a visual representation of the annual average tfpch, effch, and techch for 2000–2010. Even though no increase was found in the change of tfpch overall, it can be seen that its decrease was slowing until 2004–2005. Had this trend been able to continue by 2005, then health productivity across OECD countries would have taken a positive turn. However, we see that productivity began to decrease again in the upcoming years. The biggest share in the increase showed by total factor productivity until 2005 was mostly coming from the increase in techch. We see that efforts were made to slow the decline in technological progress until 2005. However, by 2010 efficiency did not change compared to 2009.
5.3 Results of Panel Tobit
Assuming the efficiency scores obtained from the DEA as dependent variables, Panel Tobit Analysis was applied in the second stage of the study to examine the socio-economic environmental variables affecting the efficiency. The estimation results of the Panel Tobit Random Effects model are shown in Table 6. Three models were estimated by Panel Tobit Analysis. By including the number of the private hospitals into the first model a second model was obtained and, by including life expectancy into this model, a third model was formed. In these models, a positive and statistically significant relation was found between GDP and efficiency, and also in all the three models a statistically significant and positive relation was seen between education and efficiency. Namely, as the income and education levels increase, so does efficiency. This finding supports the hypothesis of “Wealthier is Healthier”, which means that more educated and economically viable individuals live in healthier states (Self and Grabowki 2003; Pritchett and Summers 1996).
Regardless of public or private sector, there is a significant and negative relationship between health spending and efficiency. However, public health spending affects efficiency in a more negative way in comparison to private health spending. Berger and Messer (2002) correlated the increase in public health spending rate within the total health spending with higher mortality rates, suggesting that public spending not only affects the health outcomes but also reflects demographic factors, such as income level, age structure and health behavior of the population. There are some findings that show, particularly for OECD countries, that health spending does not increase efficiency, decreasing it instead (Afonso and Aubyn 2005; Berger and Messer 2002; Evans et al. 2000). In those studies, it was emphasized that an increase in life expectancy causes the number of aged people to increase drastically, resulting in an increase in health spending across the OECD countries. Since health spending also reflects the age structure of the population, an increase in those aged over 65 also increases the mortality rate in the country, while decreasing efficiency.
Life expectancy at birth, reflecting average life expectancy, was found statistically insignificant. The number of private hospitals was statistically significant and positive, while the number of public hospitals was found statistically significant and negative. An increase in the number of public hospitals does not increase efficiency; rather, it decreases it. It is assumed that an excess in the number of public hospitals due to wrong assignment of the resources resulting from self- interested expense-preference behavior of public managers, as well as market failure resulting from the lack of competition in public hospitals, negatively affect efficiency (Mobley and Magnussen 1998). On the other hand, an increase in the number of private hospitals, where competition is intense, affects efficiency in a positive way.
6 Conclusion
This study carried out a two-stage performance assessment across 29 OECD countries for 2000–2010. In the first stage of the study, the efficiency scores of the hospitals measured by DEA. In the second stage the environmental factors affecting the efficiency scores obtained in the first stage were identified by Panel Tobit Analysis. The paper also examined the change in the total factor productivity compared to previous years by the decomposing the change, using Malmquist Productivity Index.
In the first stage of the study, the efficiency scores of the countries were obtained for each year, using two outputs and five inputs by DEA under the presumption of CRS. It was found that the efficiency scores achieved after 2000 began to decrease across the countries in 2004, and reached their lowest points in 2009 and 2010 by 0.842 and 0.819, respectively. The main reason for this drop is thought to be the cuts made by these countries in their health spendings between 2009 and 2011 due to the financial crisis. While Turkey, Mexico, and the United Kingdom were the most efficient countries during that 10-year period, Japan, Iceland, France, and Belgium had an efficiency score below the average level. The reason for this is, in general, the high slack values occurred in the numbers of tomography, MR, and nurses. It is concluded that these countries should remove the idle capacity formed on those input values in order to make these processes more efficient. As another input variable, physicians were found working in full capacity in almost every country. As for Malmquist total factor productivity, it was concluded that it did not increase on an annual basis during this 10-year period. The lack of technological progress in 2001 and 2002 was found to decrease in the later years but, this time, there was technical inefficiency.
In the second stage of the study, the socio-economic factors affecting the technical efficiency scores obtained by DEA were identified by Panel Tobit Analysis. It was proposed in the paper to use the Panel Tobit Analysis instead of traditional panel data analysis in order to obtain consistent and unbiased estimators since the dependent variable obtained by DEA has a censored structure.
As a result of the estimation, there was found a positive relation between GDP and education; also a positive relation between GDP and efficiency. It is concluded that countries with more educated and wealthy population have more efficient health systems. Also, a negative but statistically significant relation between health spending and efficiency existed. Public health spending was found to impact efficiency in a more negative way compared to private health spending. Due to the high rate of aged population in these OECD countries, this is thought to have affected efficiency negatively as a result of an increase in the care costs for the elderly, chronic diseases, and mortality rates.
It is observed that there is a statistically significant and negative relation between the number of public hospitals (as another environmental variable) and efficiency. Since public hospitals are not profit-oriented and do not work to improve their reputation, in short, due to a lack of competition they might affect efficiency in negative ways, thus leading to such results. A positive and statistically significant relation was found between the number of private hospitals and efficiency. Since an increase in this number also brings about competition, it affects efficiency in a positive way.
This study has been intended to not only contribute to the literature but also, to policy-making strategies. The authors have tried to provide suggestions on what variables should be focused on and how to have a more effective and efficient health system. A limitation of this study, in which a number of variables have been used, is the exclusion of some countries from the analysis due to lack of data.
7 Policy Recommendations
The study found that the GDP as well as education positively correlated with efficiency. The findings show that people with less education and lower income tend to have poorer efficient health systems so growth policies are important to foster health production. Also, increasing the level of education is of great importance because more educated people are more conscious about their health, and they make healthier life style choices. It is concluded that there is negative relation between the number of public hospitals and efficiency, but a positive relation was found between the number of private hospitals and efficiency. Since public and private health spending have negative impact on efficiency, policy recommendations should address the inefficiency in spending and improper allocation of resources. One of the major policy recommendation that emerges from the study is for policy makers to pay more attention to allocation of resources in public hospitals. Resource allocation should be increased or sanctioned based on the health outcome of the hospitals, rather than number of people treated by the hospitals. Since unlike private hospitals, there is no motivation created by competition in public hospitals, desired outcome can only be obtained by proper oversight by the policy makers. In OECD countries, a growing spending due to chronic illnesses such as cancer, diabetes, and depression, in addition to health threat caused by obesity and inactivity create a big burden on the budget. Training programs, guidelines, public spots, etc. should be prepared for better lifestyles, disease prevention and early diagnosis. Also, health workers should be trained or retrained to raise awareness and consciousness of the people.
References
Afonso, A., & Aubyn, M. (2005). Non-parametric approaches to education and health efficiency in OECD countries. Journal of Applied Economics, 8(2), 227–246.
Afonso, A., & Aubyn, M. (2011). Assessing health efficiency across countries with a two-step and bootstrap analysis. Applied Economics Letters, 18, 1427–1430.
Alexander, C. A., Busch, G., & Stringer, K. (2003). Implementing and interpreting a data envelopment analysis model to assess the efficiency of health systems in developing countries. IMA Journal of Management Mathematics, 14, 49–63.
Ancarani, A., Di Maurob, C., & Giammancob, M. D. (2009). The impact of managerial and organizational aspects on hospital wards’ efficiency: Evidence from a case study. European Journal of Operational Research, 194, 280–293.
Atkinson, S. E., & Wilson, P. W. (1995). Comparing mean efficiency and productivity scores from small samples: A bootstrap methodology. The Journal of Productivity Analysis, 6, 137–152.
Baltagi, B. (2008). Econometric analysis of panel data (4th ed.). Hoboken: Wiley.
Banker, R. D., Charnes, A., & Cooper, W. W. (1984). Some models for estimating technical and scale inefficiencies in data envelopment analysis. Management Science, 30(9), 1078–1092.
Berger, M. C., & Messer, J. (2002). Public financing of health expenditures, insurance, and health outcomes. Applied Economics, 34(17), 2105–2113.
Bhat, V. N. (2005). Institutional arrangements and efficiency of health care delivery systems. European Journal of Health Economics, 50, 215–222.
Biorn, E., Hagen, T. P., Iversen, T., & Magnussen, J. (2003). The effect of activity-based financing on hospital efficiency: A panel data analysis of DEA efficiency scores 1992–2000. Health Care Management Science, 6, 271–283.
Caves, D. W., Christensen, L. R., & Diewert, W. E. (1982). The economic theory of index numbers and the measurement of input, output, and productivity. Econometrica, 50(6), 1393–1414.
Charnes, A., Cooper, W. W., & Rhodes, E. (1978). Measuring the efficiency of decision making units. European Journal of Operational Research, 2, 429–444.
Chen, A., Hwang, Y., & Shao, B. (2005). Measurement and sources of overall and input inefficiencies: Evidences and implications in hospital services. European Journal of Operational Research, 161, 447–468.
Chilingerian, J. A. (1995). Evaluating physician efficiency in hospitals: A multivariate analysis of best practices. European Journal of Operational Research, 80, 548–574.
Chowdhury, H., Zelenyuk, V., Laporte, A., & Wodchis, W. P. (2014). Analysis of productivity, efficiency and technological changes in hospital services in Ontario: How does case-mix matter? International Journal of Production Economics, 150, 74–82.
Chu, N. G. Y. (2011). The productive efficiency of Chinese hospitals. China Economic Review, 22, 428–439.
Coelli, T.J. (1996). A guide to DEAP version 2.0: A data envelopment analysis (computer) program. Center for Efficiency and Productive Analysis (CEPA) Department of Econometrics University of New England, Armidale, Australia.
Cooper, W. W., Seiford, L. M., & Zhu, J. (2003). Handbook on data envelopment analysis. International series in operations research and management science (2nd ed., Vol. 164). Norwell: Springer.
Davidson, R., & MacKinnon, J. (2003). Econometric theory and methods. Oxford: Oxford University Press.
Erdoğan, A. H., & Samut, P. K. (2013). Analysis of the efficiency determinants of Turkey’s agriculture sector by two-stage data envelopment analysis (DEA). Ege Academic Review, 13(1), 21–28.
Eurostat, European Commission. (2014). http://epp.eurostat.ec.europa.eu/portal/page/portal/statistics/themes. Accessed March 10, 2014.
Evans, D., Tandon, T., Murray, C. & Lauer, J. (2000). The comparative efficiency of national health systems in producing health: An analysis of 191 countries. GPE Discussion Paper No. 29, Geneva: WHO.
Färe, R., & Grosskopf, S. (1992). Malmquist productivity indexes and fisher ideal indexes. Economic Journal, 102(410), 158–160.
Färe, R., Grosskopf, S., Lindgren, B., & Roos, P. (1994). Productivity developments in Swedish hospitals: A malmquist output index approach. In A. Charnes, W. Cooper, A. Lewin, & L. Seiford (Eds.), data envelopment analysis: Theory, methodology and applications. Boston: Kluwer.
Farrell, M. J. (1957). The measurement of productive efficiency. Journal of the Royal Statistical Society, 120(3), 253–290.
Fernandez-Val, I., Weidner, M. (2013). Individual and time effects in nonlinear panel models with large N, T. http://arxiv.org/pdf/1311.7065v1.pdf. Accessed April 24, 2014.
Gok, M. S., & Sezen, B. (2013). Analyzing the ambiguous relationship between efficiency, quality and patient satisfaction in healthcare services: The case of public hospitals in Turkey. Health Policy, 111, 290–300.
Greene, W. (2003). Econometric analysis (5th ed.). New Jersey: Prentice Hall.
Greene, W. (2004a). Distinguishing between heterogeneity and inefficiency: Stochastic frontier analysis of the World Health Organization’s panel data on national health care systems. Health Economics, 13, 959–980.
Greene, W. (2004b). Fixed effects and bias due to the incidental parameters problem in the tobit model. Econometric Reviews, 23(2), 125–147.
Grosskopf, S., Self, S., & Zaim, O. (2006). Estimating the efficiency of the system of healthcare financing in achieving better health. Applied Economics, 38, 1477–1488.
Hollingsworth, B., & Wildman, J. (2003). The efficiency of health production: Re-estimating the WHO panel data using parametric and non-parametric approaches to provide additional information. Health Economics, 12, 493–504.
Hu, H. H., Qi, Q., & Yang, C. H. (2012). Analysis of hospital technical efficiency in China: Effect of health insurance reform. China Economic Review, 23, 865–877.
Jamil, N. (2013). A comparison of iterative methods for the solution of non-linear systems of equations. International Journal, 3(2), 119–130.
Kittelsen, S. A. C., Magnussen, J., Anthun, K. S., Häkkinen, U., Linna, M., Medin, E., Olsen, K. R., & Rehnberg, C. (2008). Hospital productivity and the Norwegian ownership reform—A Nordic comparative study (Vol. 10, pp. 1–25). HERO Working Paper, University of Oslo, Health Economics Research Programme.
Kjekshus, L., & Hagen, L. (2007). Do hospital mergers increase hospital efficiency? Evidence from a National Health Service country. Journal of Health Services Research and Policy, 12(4), 230–235.
Lovell, K. C. A. (2003). The decomposition of Malmquist productivity indexes. Journal of Productivity Analysis, 20, 437–458.
Malmquist, S. (1953). Index numbers and indifference surfaces. Trabajos de Estadistica, 4, 209–242.
Medin, E., Anthun, K. S., Hakkinen, U., Kittelsen, S. A. C., Linna, M., Magnussen, J., et al. (2011). Cost efficiency of university hospitals in the Nordic countries: A cross-country analysis. The European Journal of Health Economics, 12, 509–519.
Mitropoulos, P., Mitropoulos, I., & Sissouras, A. (2013). Managing for efficiency in health care: The case of Greek public hospitals. The European Journal of Health Economics, 14, 929–938.
Mobley, L. R., & Magnussen, J. (1998). An international comparison of hospital efficiency: Does institutional environment matter? Applied Economics, 30, 1089–1100.
Moran, V., & Jacobs, R. (2013). An international comparison of efficiency of inpatient mental health care systems. Health Policy, 112, 88–99.
National Health System of Spain. (2014). http://www.msssi.gob.es/organizacion/sns/docs/sns2012/SNS012__Ingles.pdf. Accessed March 10, 2014.
Nedelea, I. C., & Fanin, J. M. (2013). Analyzing cost efficiency of critical access hospitals. Journal of Policy Modeling, 35, 183–195.
OECD. (2012). Health at a glance: Europe 2012. Paris: OECD Publishing. doi:10.1787/9789264183896-en.
OECD. (2013). Health at a glance 2013: OECD indicators. Paris: OECD Publishing. doi:10.1787/health_glance-2013-en.
OECD. (2014). Stat Extracts. http://stats.oecd.org/. Accessed March 7, 2014.
Pelone, F., Kringos, D. S., Valerio, L., Romaniello, A., Lazzari, A., Ricciardi, W., & Giulio de Belvis, A. (2012). The measurement of the relative efficiency of general practice and the implications for policy makers. Health Policy, 107, 258–268.
Pritchett, L., & Summers, L. H. (1996). Wealthier is healthier. Journal of Human Resources, University of Wisconsin Press, 31(4), 841–868.
Puig-Junoy, J. (1998). Measuring health production performance in the OECD. Applied Economics Letters, 5, 255–259.
Puig-Junoy, J. (2000). Partitioning input cost efficiency into its allocative and technical components: An empirical DEA application to hospitals. Socio-Economic Planning Sciences, 34, 199–218.
Ray, S. C. (2004). Data envelopment analysis: Theory and techniques for economics and operations research. Cambridge: Cambridge University Press.
Retzlaff-Roberts, D., Chang, C. F., & Rubin, R. M. (2004). Technical efficiency in the use of health care resources: A comparison of OECD countries. Health Policy, 69, 55–72.
Sahin, I., Ozcan, Y. A., & Ozgen, H. (2011). Assessment of hospital efficiency under health transformation program in Turkey. Central European Journal of Operations Research (CEJOR), 19, 19–37.
Self, S., & Grabowki, R. (2003). How effective is public health expenditure in improving overall health? A cross-country analysis. Applied Economics, 35(7), 835–845.
Sherman, H. D. (1984). Hospital efficiency measurement and evaluation: Empirical test of a new technique. Medical Care, 22(10), 922–938.
Spinks, J., & Hollingsworth, B. (2009). Cross-country comparisons of technical efficiency of health production: A demonstration of pitfalls. Applied Economics, 41, 417–427.
Steinmann, L., Dittrich, G., Karmann, A., & Zweifel, P. (2004). Measuring and comparing the (in) efficiency of German and Swiss hospitals. The European Journal of Health Economics, 5, 216–226.
The World Bank. (2014). http://data.worldbank.org/indicator. Accessed March 10, 2014.
Thomas, A. (2007). Applied panel data econometrics http://www.cams.aub.edu.lb/events/docs/athomashandout.pdf. Accessed April 11, 2014.
Varabyova, Y., & Schreyögg, J. (2013). International comparisons of the technical of the hospital sector: Panel data analysis of OECD countries using parametric and non-parametric approaches. Health Policy, 112, 70–79.
Weng, S.-J., Wu, T., Blackhurst, J., & Mackulak, G. (2009). An extended DEA model for hospital performance evaluation and improvement. Health Service Outcomes Research Method, 9, 39–53.
Witte, K. D., & Marques, R. C. (2010). Designing performance incentives, an international benchmark study in the water sector. Central European Journal of Operations Research (CEJOR), 18, 189–220.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kaya Samut, P., Cafrı, R. Analysis of the Efficiency Determinants of Health Systems in OECD Countries by DEA and Panel Tobit. Soc Indic Res 129, 113–132 (2016). https://doi.org/10.1007/s11205-015-1094-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11205-015-1094-3