Abstract
The pursuit of longevity, which during the Renaissance era was limited to longing for miraculous ways of rejuvenation, such as bathing in the fountain of youth, took a scientific turn in 1889 with the publication of Brown-Sequard’s self-experiments with an extract of animal testes, which apparently improved his vitality, physical strength and cognition. This extract, marketed then as the "Elixir of Life", was sold for decades throughout Europe and North America. However, recent replication of Brown-Sequard’s experiments demonstrated that such an extract only contains homeopathic concentrations of testosterone that are insufficient to exert any biological effect. Thus, the birth of Andrology began with a placebo effect. Over the past few decades, the quest for compounds that might lead to rejuvenation has regained traction, with testosterone being at the forefront. Though clinical practice guidelines advocate testosterone therapy in men with organic hypogonadism—the only indication approved by the Food and Drug Administration—testosterone continues to be marketed as a wonder drug with rejuvenating effects on sexual function, vitality, and a host of other unproven benefits. Additionally, the epidemic of obesity and diabetes, conditions associated with low testosterone, has further brought testosterone into the limelight. Although the number of testosterone prescriptions written have increased several-fold in the past two decades, carefully conducted randomized trials suggest modest benefits of testosterone therapy. At the same time, safety concerns, particularly in older men, remain valid.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
Throughout history, humanity has searched for ways of rejuvenation and to extend healthy lifespan. While in the 1500 s, imagery of magical places, such as the Fountain of Youth (Fig. 1), kept the dreams of achieving eternal youth alive, the late 1800s saw the dawn of scientific quest for antiaging products, especially after the widely publicized report of Brown-Sequard’s experiments [1]. In his report published in the Lancet in 1889, the 72-year-old physician-scientist described the effects of subcutaneous self-administration over two weeks of an aqueous extract derived from the testicles of dogs and guinea pigs. He reported significant improvements in his strength, endurance, and cognition. The presumed benefits of Brown-Séquard’s "Elixir of Life" were widely advertised throughout Europe and North America, where this magic potion was commercially sold for decades (Fig. 2). Brown-Séquard’s experiments even provided an impetus for “organotherapy”; a ‘science’ of therapy with extracts derived from various animal organs, which were used to treat several diseases and to counter the effects of aging [2]. Though the ‘science of organotherapy’ led to successful treatment of hypothyroidism (with thyroid extracts), diabetes (with pancreatic extracts) and dwarfism (with pituitary extracts), this was not the case with sex steroids. Indeed, recent replication of Brown-Séquard’s published methods demonstrated that his ‘elixir’ likely contained 112 ng/mL (388 nmol/L) of unesterified testosterone, which is equivalent to administration of 186 ng/day [3]. This is in stark contrast to testicular secretion of ~ 6 mg/day of testosterone by healthy adult men [4]. Indeed, the Endocrine Society’s clinical practice guidelines on male hypogonadism recommend treatment with 5–10 mg of testosterone daily [5]. In addition to the homeopathic concentrations of testosterone in Brown Sequard’s magic potion, the half-life of unesterified testosterone is only limited to ~ 30 min [6]. Thus, the birth of Andrology started with a placebo effect.
A Portrait of Brown-Séquard, c.1880. B A magazine advertisement publicizing extracts of animal organs, including Brown-Sequard’s testicular extract, known as “Brown-Séquard’s Elixir” or “Elixir of Life”. Reproduced with permission from Rengachary et al. [7]. C A satirical cartoon of Brown-Séquard’s “Elixir or Life”, published in 1896 in the weekly magazine “Judge"
2 Anabolic androgenic steroids: use, misuse and abuse
As this paper focuses on medicalization of testosterone, we will first highlight various terms that have been associated with the use of testosterone (and other androgens) to provide some context on how commercialization of testosterone has impacted its use in various segments of the population.
Use
The use of Anabolic Androgenic Steroids (AAS) implies taking prescription androgens (mainly testosterone) for medical conditions. An example is the treatment of hypogonadal men with organic disease of the hypothalamus, the pituitary or the testes. Testosterone therapy, at physiologic dose, is indicated to induce or maintain secondary sexual characteristics. This is the only indication currently approved by the Food and Drug Administration (FDA). Additionally, clinical practice guidelines on male hypogonadism also advocate use of testosterone therapy in men with organic (classic) androgen deficiency.
Misuse
The misuse constitutes systematic prescribing of AAS for unproven medical indications in men who do not have organic androgen deficiency. This includes prescribing androgens to primarily treat obesity, diabetes, impaired cognition, male infertility or to reverse aging.
Abuse
The abuse of AAS constitutes their use for non-medical purposes. In this context, androgens are often used in supraphysiologic doses to either achieve performance enhancement (competitive sports) or image enhancement. For these purposes, AAS are usually procured illicitly from compounding pharmacies, fitness centers or even veterinary clinics.
3 Promotion of ‘ideal male body’ image by the media
Although more than a century has passed since the birth of organotherapy, the quest for rejuvenation not only persists, but has gained momentum in recent years. Indeed, modern society places a high value in youthful appearance, with social media constantly promoting an idealized body image of a youthful and muscular man. Since the 1980s, mass media has emphasized on muscularity as an essential element of the ideal male body. Hollywood characters like “Rambo” and “Conan the Barbarian”, starring actors who were professional bodybuilders, started a trend of shirtless heroes with increasingly muscular physiques. This trend has since become the standard, as evident in most Hollywood action movies. Even more concerning is the fact that this ‘standard’ has now permeated to the ‘average Joe’, including teenagers and pre-teen boys. Indeed, even the action toy figures have become progressively more muscular through the years. For example, when G.I. Joe was first introduced in 1964, it had dimensions proportional to that of an average-built man. By 1998, the “G.I. Joe Extreme” had proportions that would parallel a bodybuilder (Fig. 3) [8, 9]. This degree of muscular hypertrophy is generally not achievable merely with resistance training unless supplemented by anabolic agents. Thus, the youth who see these images are drawn towards pharmaceutical agents to achieve the goal of this ideal physique. Not surprisingly, AAS abuse (not necessarily for performance-enhancement, but for image-enhancement) has become a major public health concern [10]. In the United States, questionnaire-based studies have estimated a lifetime prevalence of AAS abuse of up to 15% [11], with 98% of these abusers being men [12]. The lifetime prevalence of AAS use is even higher among gay and bisexual men (21%), as well as among ethnic minorities (25%) [13]. It is estimated that 3–4 million men between age 13 and 50 years in the United States have used AAS [10], and testosterone remains the most abused anabolic agent [14,15,16]. In summary, the role of mass media in promoting this male body image is not inconsequential when it comes to medicalization of testosterone therapy.
Evolution of action toy figures. The original GI Joe Land Adventurer from 1964 (top left panel, black arrow) and G.I. Joe Extreme, 1998 (bottom left panel, white arrow). The top right panel shows the evolution of physique of action toys Luke Skywalker and Hans Solo from 1978 and 1998. The bottom right panel shows other action toys. Adapted with permission from Pope et al. [9]
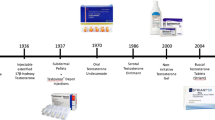
4 Influence of advertising on testosterone prescriptions
Although testosterone has been abused since the 1950s by both elite and amateur athletes for its ergogenic effects, the past two decades have seen an exponential growth in its use as a medicine. In the United States, testosterone prescriptions increased up to threefold between 2001 to 2011 [17, 18], while globally, testosterone sales increased by 12-fold, increasing testosterone market from $150 million to $1.8 billion (Fig. 4) [19]. This increase was largely driven by intense media campaigns. From 2010 to2013, advertisements of topical testosterone products accounted for 13% of all ads on prime time television news broadcasts on major networks in the United States [20]. Quarterly spending on physicians and consumer-targeted marketing increased from $5 million in 2009 to $65 million in 2013, with substantial resources directed towards direct-to-consumer advertising (DTCA) [21].This strategy proved to be quite effective; a study evaluating claims database for exposure to DTCA from the largest market areas in the United States estimated that each additional exposure to a testosterone promoting television advertisement resulted in 14 new orders for testosterone test and 5 new testosterone prescriptions per million men exposed [22]. Interestingly, 2 of these 5 new prescriptions were written without even testing for low testosterone. This is a classic vicious cycle of DTCA: patients respond to DTCA and in turn, physicians respond to patients' requests for prescriptions.
Testosterone use in various countries between 2000 to 2011. Reproduced with permission from Handelsman [19]
Although the United States and New Zealand are the only industrialized countries in which DTCA of prescription drugs is legal, in other parts of the world, manufacturers are allowed to run disease-awareness campaigns without mentioning brand name [23]. This regulatory loophole is quite advantageous for the manufacturers as while educating the public on symptoms of low testosterone, the generic name of the product is mentioned in a subtle way in such advertisements.
5 Age-related low testosterone: is it a big public health problem?
Despite the marked increase in the number of testosterone prescriptions written, the syndromic prevalence of age-related low testosterone is miniscule. Two decades ago, data from the Baltimore Longitudinal Study on Aging showed that the numerical prevalence of low testosterone [defined as total testosterone < 325 ng/dL (11.3 nmol/L) or free testosterone index < 2.5th percentile] was as high as 68% in men in their 70 s and an astronomical 91% in men 80 years and older. However, this report did not assess presence of specific signs and symptoms of androgen deficiency [24]. A decade later, data from the European Male Aging Study (EMAS), in which the investigators carefully assessed candidate symptoms that are associated with androgen deficiency, found that the syndromic prevalence of hypogonadism in men aged 40–79 years was only 2.1% [25] (Fig. 5A).
A Schematic representation of the prevalence of syndromic androgen deficiency in men participating in the EMAS. Among 2966 men evaluated, only 63 (2.1%) had low testosterone concentration along with specific symptoms of androgen deficiency. Data from Wu et al. [25]. EMAS, European Male Aging Study. B Schematic representation of the yield of men with syndromic androgen deficiency during the screening process in the Ttrials. Among 51,085 men who underwent telephone-screening, only 931 men had specific symptoms and low testosterone concentrations (790 randomized; not depicted in image). Data from Cauley et al. [26]. TTrials, Testosterone Trials
Further evidence regarding the low syndromic prevalence of age-related low testosterone comes from the screening data of the Testosterone Trials (TTrials), a coordinated set of trials that assessed the efficacy of one year of testosterone therapy in men 65 years or older with age-related low testosterone and symptoms of androgen deficiency [27]. Eligibility criteria included an average of two total testosterone concentrations < 275 ng/dL and decreased vitality, sexual dysfunction or physical dysfunction [26]. Recruitment in the TTrials was challenging, of the 51,085 men who were screened only 931 men (1.8%) met eligibility criteria for randomization [26] (Fig. 5B). These statistics indicate that only a slim minority of older men meet subjective, objective and biochemical criteria of androgen deficiency. Despite careful selection of men who were thought to benefit the most from testosterone therapy, only modest improvements in sexual function and mood were noted in the testosterone group, while no improvements were seen in the vitality and physical function in men who reported fatigue and mobility limitation at the time of enrollment. Despite modest efficacy of testosterone in aging men and the fact that guidelines recommend treatment of men with organic hypogonadism, a large fraction of men are still prescribed testosterone for age and obesity-related low testosterone. In fact, a substantial number of men who were started on testosterone therapy have baseline serum testosterone concentrations within the normal range, and astonishingly, testosterone levels are not even checked in many men before a testosterone prescription was written [28]. The medicalization of testosterone has permeated in the scientific community to such an extent that biochemical diagnosis is not even made in many men who present with symptoms suggestive of androgen deficiency.
6 Large market, modest benefits
As mentioned above, the benefits of testosterone therapy in the TTrials were modest. Testosterone therapy improved overall sexual activity, libido and erectile function [27]. The increase in total testosterone concentrations were associated with improvements in sexual activity [29]. However, improvements in erectile function were modest and of lower magnitude compared to that seen with phosphodiesterase-5 inhibitors [30, 31]. Testosterone treatment also improved mood and depressive symptoms [27]. Though bone density also improved in men participating in the Bone Trial of the TTrials who were randomized to testosterone [32], the magnitude of increase was lower than seen with most other FDA-approved bone-specific agents [33]. Furthermore, the clinical benefit of this increase in bone density remains unclear as anti-fracture efficacy of testosterone therapy is unknown, while FDA-approved bone-specific agents (bisphosphonates, denosumab, Romosozumab, etc.) have demonstrated anti-fracture efficacy. For this reason, Endocrine Society guidelines for male osteoporosis suggest that men who are at high risk for fracture should be treated with an agent with proven anti-fracture efficacy, even if testosterone is prescribed for symptoms of androgen deficiency [34]. Similarly, though testosterone treatment was associated with an increase in hemoglobin levels in anemic men participating in the Anemia Trial of the Ttrials [35, 36], testosterone therapy is not considered a first-line treatment for unexplained anemia nor it can be recommended as such until long-term safety of testosterone is established [36].
Previous mechanistic studies had shown that testosterone improves motivation and energy [37]. Indeed, in the EMAS, men with low testosterone were more likely to report fatigue [25]. Similarly, men undergoing androgen deprivation therapy (ADT) for prostate cancer experience more fatigue compared with men who only undergo prostatectomy [38]. Based on these data, it was simply assumed by lay public and in some quarters of the scientific community, that testosterone therapy improves vitality. However, in the Vitality Trial of the TTrials, testosterone treatment was not superior to placebo in improving fatigue as assessed by FACIT-F questionnaire [27]. While it is conceivable that the currently available instruments may not be capturing the effects of testosterone treatment on fatigue, the current evidence does not support prescribing testosterone to improve energy levels in men with age-related low testosterone.
Similar to fatigue, it has been assumed for quite some time that testosterone therapy improves physical function. Though testosterone replacement consistently improves muscle mass and muscle strength, its efficacy in improving physical function remains inconsistent [39,40,41]. In the Physical Function Trial of the TTrials, men randomized to testosterone did not demonstrate an increase in the distance walked during the 6-min walk test (even though these men were carefully selected and met both subjective and objective criteria of mobility limitation) [27]. Thus, the current evidence does not support testosterone therapy to improve physical function in older men with mobility limitations.
7 New trends and the risk of testosterone misuse
Current estimates suggest that ~ 40% of the adult population in the United States is obese [42, 43]. Considering that obesity is associated with low serum concentrations of sex hormone-binding globulin (SHBG) [44], the principle binding protein of sex steroids [45], a large number of men are being diagnosed with low testosterone levels that are obesity-related. This is a problem of clinical chemistry and does not necessarily imply an androgen deficient state given that free testosterone levels are generally normal in these men. Symptoms of fatigue in these men might be indicative of underlying, undiagnosed obstructive sleep apnea. Though in men who have severe obesity free testosterone levels do decline, this is still a "functional" state and not organic androgen deficiency as weight loss results in restoration of endogenous serum testosterone concentrations [46, 47]. Thus, unless clinicians recognize the impact of obesity of testosterone concentrations, many men might be considered candidates for testosterone therapy; the desire to achieve ideal male body could create a “perfect storm” of over prescription of testosterone in obese men. Indeed, analyses of testosterone prescribing patterns in the Veterans Affairs (VA) system revealed that obesity was one of the stronger predictors for receiving a testosterone prescription [48]. Yet, current evidence from randomized trials in obese men show modest, and transient, benefits of testosterone therapy on weight loss and metabolic health [49,50,51].
Similar to obesity, diabetes is a highly prevalent condition and is associated with low testosterone levels [52, 53]. Previous studies of testosterone therapy in men with diabetes had not shown a significant treatment benefit on metabolic parameters. However, a recent large, randomized trial suggested an improvement in metabolic outcomes and a reduced risk of developing diabetes after 2 years of treatment with testosterone compared to placebo, when combined with lifestyle intervention [54]. Though these data are encouraging, physical activity, metformin and GLP-1 agonists might be preferrable in such patients, specially considering their cardiovascular benefit. In sum, there remains a concern that these new data may lead to an increase in testosterone prescription in men with prediabetes.
8 Safety concerns
While the benefits of testosterone therapy in select men with age-related, low testosterone levels remain modest at best, the safety of testosterone therapy continues to stir debate, particularly regarding the potential risk of cardiovascular and prostate disease [55,56,57,58]. Some observational studies have suggested increased cardiovascular risk, including myocardial infarction, stroke and venous thromboembolism [59,60,61], while limited data from randomized trials have shown increased cardiovascular events in older men randomized to testosterone [39] (Fig. 6A). In 2013, in response to a petition by a citizen's interest group and due to conflicting results from various studies, the FDA conducted an extensive review of the literature and issued updated testosterone labeling that included warning of a possible increased risk of stroke and myocardial infarction, and of limitation of use in men with “age-related hypogonadism” [62]. Cardiovascular safety of testosterone therapy garnered more attention with the publication of the Cardiovascular Trial of the TTrials that showed a greater increase in the volume of noncalcified plaque in men treated with testosterone compared with men who received placebo [63] (Fig. 6B).
A Cardiovascular events in the testosterone in older men with mobility limitation trial. The Kaplan–Meier plot shows divergence of the curves weeks after randomization. Adapted from Gagliano-Jucá and Basaria [64]. B Change in the volume of various components of the coronary artery atherosclerotic plaques in the Cardiovascular Trial of the Ttrials. Adapted from Gagliano-Jucá and Basaria [64]
Contrary to the studies discussed above, other observational studies do not report an association between testosterone therapy and cardiovascular risk [65,66,67]. In fact, some studies have even suggested a reduced cardiovascular risk with testosterone treatment [68,69,70]. The reason behind these conflicting data is likely the fact that no published randomized trial was adequately powered to assess cardiovascular events. In addition to the advisory and updated testosterone labeling, the FDA also issued a guidance “… requiring manufacturers of approved testosterone products to conduct a well-designed clinical trial to more clearly address the question of whether an increased risk of heart attack or stroke exists among users of these products”. The Testosterone Replacement therapy for Assessment of long-term Vascular Events and efficacy ResponSE in hypogonadal men (TRAVERSE) study was designed in response to this FDA guidance to determine the effects of testosterone treatment on the incidence of major adverse CV events (MACE) in middle-aged and older men with hypogonadism with or at high risk for CV disease. The TRAVERSE trial is currently ongoing [71], and will randomize ~ 6,000 men aged 45–80 years with serum total testosterone level < 300 ng/dL (10.4 nmol/L) and at high risk of cardiovascular disease (primary prevention) or with known history of cardiovascular disease (secondary prevention), to receive testosterone gel or placebo gel for 5 years. The trial will also evaluate the impact of testosterone treatment on the incidence of high-grade prostate cancer [71]. Until the results of the TRAVERSE trial become available, risks of cardiovascular and prostate disease remain unclear, and require an open discussion with patients before testosterone therapy is started.
9 Conclusion
In a society that is constantly in quest for the fountain of youth, testosterone has found its spot on the center stage. In addition to the increase in longevity (and resulting interest in age-related low testosterone), which has substantially increased the market for testosterone products, the prevalence of obesity and diabetes has also increased to epidemic proportions. This, together with promotion of hypermuscular male body image, has created a perfect storm that has escalated both misuse and abuse of testosterone. In older men, benefits of testosterone therapy are modest while safety issues remain unresolved. Though there will always be room for more rigorously conducted studies to assess benefits and risks of testosterone therapy, there is a greater need to educate the general public regarding the benefits and potential harm of testosterone treatment, and to highlight the fact that testosterone is a medicine that is indicated in men with organic androgen deficiency, and that it is NOT an Elixir of Life.
References
Brown-Séquard C. Note on the effects produced on man by subcutaneous injections of a liquid obtained from the testicles of animals. The Lancet. 1889;134(3438):105–7.
Borell M. Organotherapy, british physiology, and discovery of the internal secretions. J Hist Biol. 1976;9(2):235–68.
Cussons AJ, Bhagat CI, Fletcher SJ, Walsh JP. Brown-Sequard revisited: a lesson from history on the placebo effect of androgen treatment. Med J Aust. 2002;177(11–12):678–9.
Vermeulen A, Rubens R, Verdonck L. Testosterone secretion and metabolism in male senescence. J Clin Endocrinol Metab. 1972;34(4):730–5.
Bhasin S, Brito JP, Cunningham GR, Hayes FJ, Hodis HN, Matsumoto AM, et al. Testosterone therapy in men with hypogonadism: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2018;103(5):1715–44.
Veldhuis JD, Keenan DM, Liu PY, Takahashi PY. Kinetics of removal of intravenous testosterone pulses in normal men. Eur J Endocrinol. 2010;162(4):787–94.
Rengachary SS, Colen C, Guthikonda M. Charles-Edouard Brown-Sequard: an eccentric genius. Neurosurgery. 2008;62(4):954–64; discussion 64.
Kanayama G, Pope HG Jr. History and epidemiology of anabolic androgens in athletes and non-athletes. Mol Cell Endocrinol. 2018;464:4–13.
Pope HG Jr, Olivardia R, Gruber A, Borowiecki J. Evolving ideals of male body image as seen through action toys. Int J Eat Disord. 1999;26(1):65–72.
Pope HG Jr, Wood RI, Rogol A, Nyberg F, Bowers L, Bhasin S. Adverse health consequences of performance-enhancing drugs: an Endocrine Society scientific statement. Endocr Rev. 2014;35(3):341–75.
Sagoe D, Molde H, Andreassen CS, Torsheim T, Pallesen S. The global epidemiology of anabolic-androgenic steroid use: a meta-analysis and meta-regression analysis. Ann Epidemiol. 2014;24(5):383–98.
Pope HG Jr, Kanayama G, Athey A, Ryan E, Hudson JI, Baggish A. The lifetime prevalence of anabolic-androgenic steroid use and dependence in Americans: current best estimates. Am J Addict. 2014;23(4):371–7.
Blashill AJ, Safren SA. Sexual orientation and anabolic-androgenic steroids in U.S. adolescent boys. Pediatrics. 2014;133(3):469–75.
de Ronde W, Smit DL. Anabolic androgenic steroid abuse in young males. Endocr Connect. 2020;9(4):R102–11.
Bonnecaze AK, O’Connor T, Aloi JA. Characteristics and attitudes of men using Anabolic Androgenic Steroids (AAS): A survey of 2385 Men. Am J Mens Health. 2020;14(6):1557988320966536.
Mullen C, Whalley BJ, Schifano F, Baker JS. Anabolic androgenic steroid abuse in the United Kingdom: An update. Br J Pharmacol. 2020;177(10):2180–98.
Baillargeon J, Urban RJ, Ottenbacher KJ, Pierson KS, Goodwin JS. Trends in androgen prescribing in the United States, 2001 to 2011. JAMA Intern Med. 2013;173(15):1465–6.
Bandari J, Ayyash OM, Emery SL, Wessel CB, Davies BJ. Marketing and testosterone treatment in the USA: a systematic review. Eur Urol Focus. 2017;3(4–5):395–402.
Handelsman DJ. Global trends in testosterone prescribing, 2000–2011: expanding the spectrum of prescription drug misuse. Med J Aust. 2013;199(8):548–51.
Koo K, Yap RL. Trends in urological direct-to-consumer advertising during prime-time television news programs. Urology Practice. 2017;4(1):7–13.
Mintzes B. The marketing of testosterone treatments for age-related low testosterone or “Low T.” Curr Opin Endocrinol Diabetes Obes. 2018;25(3):224–30.
Layton JB, Kim Y, Alexander GC, Emery SL. Association between direct-to-consumer advertising and testosterone testing and initiation in the United States, 2009–2013. JAMA. 2017;317(11):1159–66.
Leonardo Alves T, Martins de Freitas AF, van Eijk ME, Mantel-Teeuwisse AK. Compliance of disease awareness campaigns in printed Dutch media with national and international regulatory guidelines. PLoS One. 2014;9(9):e106599.
Harman SM, Metter EJ, Tobin JD, Pearson J, Blackman MR, Baltimore Longitudinal Study of A. Longitudinal effects of aging on serum total and free testosterone levels in healthy men. Baltimore Longitudinal Study of Aging. J Clin Endocrinol Metab. 2001;86(2):724–31.
Wu FC, Tajar A, Beynon JM, Pye SR, Silman AJ, Finn JD, et al. Identification of late-onset hypogonadism in middle-aged and elderly men. N Engl J Med. 2010;363(2):123–35.
Cauley JA, Fluharty L, Ellenberg SS, Gill TM, Ensrud KE, Barrett-Connor E, et al. Recruitment and screening for the testosterone trials. J Gerontol A Biol Sci Med Sci. 2015;70(9):1105–11.
Snyder PJ, Bhasin S, Cunningham GR, Matsumoto AM, Stephens-Shields AJ, Cauley JA, et al. Effects of testosterone treatment in older men. N Engl J Med. 2016;374(7):611–24.
Jasuja GK, Bhasin S, Rose AJ. Patterns of testosterone prescription overuse. Curr Opin Endocrinol Diabetes Obes. 2017;24(3):240–5.
Cunningham GR, Stephens-Shields AJ, Rosen RC, Wang C, Bhasin S, Matsumoto AM, et al. Testosterone treatment and sexual function in older men with low testosterone levels. J Clin Endocrinol Metab. 2016;101(8):3096–104.
Qaseem A, Snow V, Denberg TD, Casey DE Jr, Forciea MA, Owens DK, et al. Hormonal testing and pharmacologic treatment of erectile dysfunction: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2009;151(9):639–49.
Spitzer M, Huang G, Basaria S, Travison TG, Bhasin S. Risks and benefits of testosterone therapy in older men. Nat Rev Endocrinol. 2013;9(7):414–24.
Snyder PJ, Kopperdahl DL, Stephens-Shields AJ, Ellenberg SS, Cauley JA, Ensrud KE, et al. Effect of testosterone treatment on volumetric bone density and strength in older men with low testosterone: A controlled clinical trial. JAMA Intern Med. 2017;177(4):471–9.
Snyder PJ, Bhasin S, Cunningham GR, Matsumoto AM, Stephens-Shields AJ, Cauley JA, et al. Lessons from the testosterone trials. Endocr Rev. 2018;39(3):369–86.
Watts NB, Adler RA, Bilezikian JP, Drake MT, Eastell R, Orwoll ES, et al. Osteoporosis in men: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2012;97(6):1802–22.
Roy CN, Snyder PJ, Stephens-Shields AJ, Artz AS, Bhasin S, Cohen HJ, et al. Association of testosterone levels with anemia in older men: A controlled clinical trial. JAMA Intern Med. 2017;177(4):480–90.
Shahani S, Braga-Basaria M, Maggio M, Basaria S. Androgens and erythropoiesis: past and present. J Endocrinol Invest. 2009;32(8):704–16.
Zitzmann M. Testosterone, mood, behaviour and quality of life. Andrology. 2020;8(6):1598–605.
Shahinian VB, Kuo YF, Freeman JL, Goodwin JS. Risk of the “androgen deprivation syndrome” in men receiving androgen deprivation for prostate cancer. Arch Intern Med. 2006;166(4):465–71.
Basaria S, Coviello AD, Travison TG, Storer TW, Farwell WR, Jette AM, et al. Adverse events associated with testosterone administration. N Engl J Med. 2010;363(2):109–22.
Bhasin S, Apovian CM, Travison TG, Pencina K, Moore LL, Huang G, et al. Effect of protein intake on lean body mass in functionally limited older men: a randomized clinical trial. JAMA Intern Med. 2018;178(4):530–41.
Basaria S, Harman SM, Travison TG, Hodis H, Tsitouras P, Budoff M, et al. Effects of testosterone administration for 3 years on subclinical atherosclerosis progression in older men with low or low-normal testosterone levels: a randomized clinical trial. JAMA. 2015;314(6):570–81.
Ellison-Barnes A, Johnson S, Gudzune K. Trends in obesity prevalence among adults aged 18 through 25 years, 1976–2018. JAMA. 2021;326(20):2073–4.
Liu B, Du Y, Wu Y, Snetselaar LG, Wallace RB, Bao W. Trends in obesity and adiposity measures by race or ethnicity among adults in the United States 2011–18: population based study. BMJ. 2021;372: n365.
Goudswaard LJ, Bell JA, Hughes DA, Corbin LJ, Walter K, Davey Smith G, et al. Effects of adiposity on the human plasma proteome: observational and Mendelian randomisation estimates. Int J Obes (Lond). 2021;45(10):2221–9.
Goldman AL, Bhasin S, Wu FCW, Krishna M, Matsumoto AM, Jasuja R. A reappraisal of testosterone’s binding in circulation: physiological and clinical implications. Endocr Rev. 2017;38(4):302–24.
Dhindsa S, Miller MG, McWhirter CL, Mager DE, Ghanim H, Chaudhuri A, et al. Testosterone concentrations in diabetic and nondiabetic obese men. Diabetes Care. 2010;33(6):1186–92.
Grossmann M, Matsumoto AM. A perspective on middle-aged and older men with functional hypogonadism: focus on holistic management. J Clin Endocrinol Metab. 2017;102(3):1067–75.
Jasuja GK, Bhasin S, Reisman JI, Hanlon JT, Miller DR, Morreale AP, et al. Who gets testosterone? patient characteristics associated with testosterone prescribing in the veteran affairs system: a cross-sectional Study. J Gen Intern Med. 2017;32(3):304–11.
Ng Tang Fui M, Prendergast LA, Dupuis P, Raval M, Strauss BJ, Zajac JD, et al. Effects of testosterone treatment on body fat and lean mass in obese men on a hypocaloric diet: a randomised controlled trial. BMC Med. 2016;14(1):153.
Mangolim AS, Brito LAR, Nunes-Nogueira VDS. Effectiveness of testosterone replacement in men with obesity: a systematic review and meta-analysis. Eur J Endocrinol. 2021;186(1):123–35.
Ng Tang Fui M, Hoermann R, Zajac JD, Grossmann M. The effects of testosterone on body composition in obese men are not sustained after cessation of testosterone treatment. Clin Endocrinol (Oxf). 2017;87(4):336–43.
Ding EL, Song Y, Malik VS, Liu S. Sex differences of endogenous sex hormones and risk of type 2 diabetes: a systematic review and meta-analysis. JAMA. 2006;295(11):1288–99.
Pitteloud N, Mootha VK, Dwyer AA, Hardin M, Lee H, Eriksson KF, et al. Relationship between testosterone levels, insulin sensitivity, and mitochondrial function in men. Diabetes Care. 2005;28(7):1636–42.
Wittert G, Bracken K, Robledo KP, Grossmann M, Yeap BB, Handelsman DJ, et al. Testosterone treatment to prevent or revert type 2 diabetes in men enrolled in a lifestyle programme (T4DM): a randomised, double-blind, placebo-controlled, 2-year, phase 3b trial. Lancet Diabetes Endocrinol. 2021;9(1):32–45.
Gagliano-Juca T, Basaria S. Testosterone replacement therapy and cardiovascular risk. Nat Rev Cardiol. 2019;16(9):555–74.
Santella C, Renoux C, Yin H, Yu OHY, Azoulay L. Testosterone replacement therapy and the risk of prostate cancer in men with late-onset hypogonadism. Am J Epidemiol. 2019;188(9):1666–73.
Loeb S, Folkvaljon Y, Damber JE, Alukal J, Lambe M, Stattin P. Testosterone replacement therapy and risk of favorable and aggressive prostate cancer. J Clin Oncol. 2017;35(13):1430–6.
Walsh TJ, Shores MM, Krakauer CA, Forsberg CW, Fox AE, Moore KP, et al. Testosterone treatment and the risk of aggressive prostate cancer in men with low testosterone levels. PLoS ONE. 2018;13(6): e0199194.
Finkle WD, Greenland S, Ridgeway GK, Adams JL, Frasco MA, Cook MB, et al. Increased risk of non-fatal myocardial infarction following testosterone therapy prescription in men. PLoS ONE. 2014;9(1): e85805.
Vigen R, O’Donnell CI, Baron AE, Grunwald GK, Maddox TM, Bradley SM, et al. Association of testosterone therapy with mortality, myocardial infarction, and stroke in men with low testosterone levels. JAMA. 2013;310(17):1829–36.
Martinez C, Suissa S, Rietbrock S, Katholing A, Freedman B, Cohen AT, et al. Testosterone treatment and risk of venous thromboembolism: population based case-control study. BMJ. 2016;355: i5968.
Food and Drug Administration (FDA). Center for drug evaluation and research. Minutes of the Joint Meeting of the Bone, Reproductive and Urologic Drugs Advisory Committee and the Drug Safety and Risk Management Advisory Committee. 2014.
Budoff MJ, Ellenberg SS, Lewis CE, Mohler ER 3rd, Wenger NK, Bhasin S, et al. Testosterone treatment and coronary artery plaque volume in older men with low testosterone. JAMA. 2017;317(7):708–16.
Gagliano-Juca T, Basaria S. Trials of testosterone replacement reporting cardiovascular adverse events. Asian J Androl. 2018;20(2):131–7.
Li H, Benoit K, Wang W, Motsko S. Association between use of exogenous testosterone therapy and risk of venous thrombotic events among exogenous testosterone treated and untreated men with hypogonadism. J Urol. 2016;195(4 Pt 1):1065–72.
Sharma R, Oni OA, Chen G, Sharma M, Dawn B, Sharma R, et al. Association between testosterone replacement therapy and the incidence of DVT and pulmonary embolism: a retrospective cohort study of the veterans administration database. Chest. 2016;150(3):563–71.
Shores MM, Walsh TJ, Korpak A, Krakauer C, Forsberg CW, Fox AE, et al. Association between testosterone treatment and risk of incident cardiovascular events among us male veterans with low testosterone levels and multiple medical comorbidities. J Am Heart Assoc. 2021;10(17): e020562.
Baillargeon J, Urban RJ, Kuo YF, Ottenbacher KJ, Raji MA, Du F, et al. Risk of myocardial infarction in older men receiving testosterone therapy. Ann Pharmacother. 2014;48(9):1138–44.
Sharma R, Oni OA, Gupta K, Chen G, Sharma M, Dawn B, et al. Normalization of testosterone level is associated with reduced incidence of myocardial infarction and mortality in men. Eur Heart J. 2015;36(40):2706–15.
Anderson JL, May HT, Lappe DL, Bair T, Le V, Carlquist JF, et al. Impact of testosterone replacement therapy on myocardial infarction, stroke, and death in men with low testosterone concentrations in an Integrated Health Care System. Am J Cardiol. 2016;117(5):794–9.
Bhasin S, Lincoff AM, Basaria S, Bauer DC, Boden WE, Cunningham GR, et al. Effects of long-term testosterone treatment on cardiovascular outcomes in men with hypogonadism: Rationale and design of the TRAVERSE study. Am Heart J. 2022;245:41–50.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical statement
No sources of funding, financial or non-financial interests are declared. Due to the nature of the article (review) no study-specific approval by the appropriate ethics committee for research involving humans and/or animals, neither informed consent if the research involved human participants, and a statement on welfare of animals if the research involved animals is provided.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gagliano-Jucá, T., Alvarez, M. & Basaria, S. The medicalization of testosterone: reinventing the elixir of life. Rev Endocr Metab Disord 23, 1275–1284 (2022). https://doi.org/10.1007/s11154-022-09751-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11154-022-09751-8