Abstract
A clustering of metabolic abnormalities such as dyslipidemia, hypertension, and diabetes mellitus, all of which are major risk factors for cardiovascular disease (CVD), occurs more often than by chance. Numerous epidemiological studies, as well as basic researches, have revealed that visceral fat accumulation is closely involved in this risk clustering. This morbid condition is now well recognized as the metabolic syndrome. The concept of the metabolic syndrome, i.e., the involvement of visceral adiposity in the clustering of CVD risk factors, implies that an effective CVD risk reduction will be accomplished by an intervention to reduce visceral fat deposits. The primary strategy of the intervention is lifestyle modification, which can be put into practice in healthcare fields, without necessity of medical treatment. Now that CVD is a leading global health burden, the metabolic syndrome attracts increasing attention in the world. To take global action against the syndrome, several working groups developed its internationally unified diagnostic criteria. Most recently, the International Diabetes Federation (IDF) and the American Heart Association/National Heart, Lung, and Blood Institute (AHA/NHLBI) jointly proposed the criteria, although some cautions will be needed in their practical use. In this review, we mainly focus on the findings observed in clinical and epidemiological studies, to discuss a practical strategy of the management of the metabolic syndrome in healthcare fields.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction: history of metabolic syndrome
In the last century, cardiovascular disease (CVD) was identified as a leading cause of morbidity and mortality in developed countries, and numerous epidemiological studies were launched in search of its contributing factors. Consequently, metabolic abnormalities such as dyslipidemia, hypertension, and diabetes mellitus were revealed to be major risk factors of CVD [1, 2]. Importantly, as was long suggested [3], these metabolic abnormalities often coexisted, especially in the individuals with abdominal obesity.
Subsequent epidemiological researches, assessing fat distribution in the body by the use of computed tomography, demonstrated that intra-abdominal visceral fat accumulation, rather than subcutaneous fat accumulation, is closely linked with a clustering of metabolic abnormalities in human [4–6]. In addition, basic researches found that adipose tissue secretes various bioactive substances, i.e., adipocytokines, such as adiponectin, which are closely involved in the homeostasis of various metabolisms, and that visceral adiposity disturbs their secretion and increases CVD risk [7–11]. On the basis of these findings, this clinically morbid condition, i.e., a clustering of metabolic abnormalities linked with visceral adiposity, has been established as a syndrome, which is now well recognized as the metabolic syndrome.
In the current century, CVD is still a leading global health burden and its prevention remains a key issue in the world. The concept of the metabolic syndrome, i.e., the involvement of abdominal obesity in a clustering of CVD risk factors, implies that an effective CVD risk reduction can be accomplished through an intervention to reduce visceral fat deposits. In addition, the metabolic syndrome is at the same time a risk factor for future development of type 2 diabetes mellitus, another key healthcare burden in the world [12]. An intervention to the metabolic syndrome is therefore expected to be also beneficial against diabetes pandemic. The metabolic syndrome now attracts increasing attention in both developed and developing countries.
2 From abdominal obesity, via metabolic abnormalities, to CVD
Ever since the etiological involvement of visceral adiposity in metabolic abnormalities was first demonstrated in human by evaluating abdominal visceral fat area with computed tomography [13], some novel imaging techniques for quantifying visceral fat deposits have been developed and have strengthened their etiological significance in human [14–16]. In addition, the establishment of commercial-based kits to measure circulating adipocytokines levels in recent years has enabled their measurement in larger clinical and epidemiological studies and has helped confirm the etiological importance of adipocytokines in human [17–20]. It is now no doubt that visceral fat accumulation and its associated phenomenon, dysregulated secretion of adipocytokines, are closely linked with a clustering of metabolic abnormalities [21, 22]. However, it is also known that metabolic abnormalities are multifactorial and are not derived solely from abdominal obesity. It has long remained to be clarified to what extent abdominal obesity exactly contributes to a clustering of metabolic abnormalities in vivo in human.
We recently addressed this issue by performing the structural equation modeling (SEM) analysis, with the use of a data of 1,989 Japanese employees [23]. In this study, we developed a multiple indicator multiple cause (MIMIC) model according to the concept of the metabolic syndrome. In brief, a latent variable named “risk clustering” was introduced in the model, to express a morbid change in the body leading to a clustering of metabolic abnormalities. We investigated to what extent the measurements of visceral fat area and circulating adiponectin levels would explain this morbid condition named “risk clustering.” The following clinically measurable parameters were set as the phenotypes of, i.e., the indicators of, the “risk clustering”: systolic blood pressure, glucose, high-density lipoprotein cholesterol, triglycerides, uric acid, and alanine aminotransferase levels. Consequently, as shown in Fig. 1, the squared multiple correlation R 2 of the “risk clustering” was calculated to be as much as 0.73, indicating that the measurements of visceral fat area and adiponectin levels explained 73 % of the variance in the risk clustering [23]. These findings support that abdominal obesity was considerably involved in a clustering of metabolic abnormalities in vivo in human.
The concept of the metabolic syndrome [23]. Impact of visceral fat accumulation and adiponectin on a clustering of metabolic abnormalities was investigated by the use of the structural equation modeling (SEM) analysis. Data are standardized regression weights (along arrows) and the squared multiple correlations R 2. An ellipse represents a latent variable, whereas rectangles and circles represent observed variables and error variables, respectively. The R 2 of the risk clustering was as much as 0.73, indicating that the measurements of VFA and adiponectin levels explained 73 % of the variance in the risk clustering. The R 2 between the risk clustering and metabolic parameters were ranged from 0.14 to 0.54, indicating that when the morbid condition of the risk clustering was developed in the body, these metabolic parameters reflect it within the range from 14 to 54 %. Log(x) represents log-transformed x, whereas e1 to e8 represent error variables. Adpn, adiponectin; ALT, alanine aminotransferase; HDL-C, high-density lipoprotein cholesterol; PG, plasma glucose; SBP, systolic blood pressure; TG, triglycerides; UA, uric acid; VFA, visceral fat area evaluated by the bioelectrical impedance method. (From Takahara M, Katakami N, Kaneto H, Noguchi M, Shimomura I. Contribution of Visceral Fat Accumulation and Adiponectin to the Clustering of Metabolic Abnormalities in a Japanese Population. J Atheroscler Thromb. 2014;21(6):543–53, with permission of the Japan Atherosclerosis Society)
In addition to the impact of abdominal obesity on the prevalence of metabolic abnormalities, its impact on CVD incidence has been investigated by a substantial number of epidemiological studies. These studies have reported that subjects with abdominal obesity at baseline had an increased risk of the future incidence of CVD [24–26]. On the other hand, the impact of abdominal obesity on future CVD risk is attenuated after adjustment for hypertension, dyslipidemia and diabetes mellitus [27], indicating that abdominal obesity increases CVD risk mainly via its associated metabolic abnormalities. These findings would reflect the pathophysiology of the metabolic syndrome, i.e., the stream from visceral adiposity, via metabolic abnormalities, to future CVD risk.
3 Intervention to abdominal obesity for CVD risk reduction
Given that visceral adiposity is the upstream of CVD risk, it is expected that CVD risk can be reduced through an intervention on visceral fat accumulation. Indeed, longitudinal studies including ours demonstrated that in subjects who received health promotion programs, visceral fat reduction was significantly associated with the improvement of metabolic profiles as well as circulating adipocytokine levels [28–32]. In addition, our 4-year observational study demonstrated that in subjects with visceral fat accumulation at baseline, those who succeeded in visceral fat reduction had a significantly lower incidence of CVD, compared to those with visceral fat deposits unchanged or increased [33]. These observations indicate that visceral fat reduction is a practical strategy for CVD risk reduction.
The primary strategy of visceral fat reduction is lifestyle modification [34, 35], which is in accordance to the conventional treatment strategy for obesity [36]. Indeed, previous studies have confirmed that lifestyle modification programs, including both improved dietary habits and increased physical activity levels, reduce not only body weight but also visceral fat deposits [37–39] (Table 1). However, this does not mean that every participant in the intervention programs achieves and maintains successful visceral fat reduction. Some participants will fail to achieve visceral fat loss, or will regain visceral fat deposit over time after a temporary reduction. For these subjects, pharmacotherapy, and sometimes bariatric surgery, may be considered as an adjunct to lifestyle intervention to help achieve targeted visceral fat reduction and health goals, as guidelines recommend for the management of overweight and obesity [36]. To date, some anti-obesity medications [40–44] and bariatric surgery [45–48] are reported to be beneficial not only for weight loss but also for visceral fat reduction, leading to the amelioration of metabolic abnormalities. In addition, bariatric surgery, but not anti-obesity medication, has been shown to reduce cardiovascular mortality in obese subjects [49, 50]. Nonetheless, it should be noted that these beneficial effects of anti-obesity medications and bariatric surgeries on visceral adiposity have been usually assessed as secondary outcomes in clinical trials which were primarily targeted at weight reduction in obese subjects. Their study designs such as inclusion criteria, outcome setting, and sample size calculation were not primarily for the assessment of visceral fat reduction in subjects with abdominal obesity. In addition, these medical options always accompany potential risks of adverse effects and costs; careful consideration therefore should be given to whether the potential benefits will be over the potential risks [49, 50].
Compared to these medical options as adjuncts to lifestyle modification, lifestyle modification itself is a foundational strategy for visceral fat reduction, regardless of combination of these medical options. What is important is that lifestyle modification programs can be put into practice even in healthcare fields, without necessity of medical treatment. This is in distinct contrast to anti-obesity medications and bariatric surgery. Carrying out the programs in healthcare fields means that a larger number of subjects with abdominal obesity are expected to be targeted and to benefit by the programs. It is true that there are so far few well-designed randomized controlled trials investigating the effects of these programs in subjects with abdominal obesity rather than general obesity. However, recent observational or single-arm studies including ours suggest that health promotion programs which are based on the concept of the metabolic syndrome and in which visceral adiposity heavily weigh will bring the reduction of visceral fat deposits and the improvement of various metabolic profiles in healthcare practice, seemingly without remarkable adverse effects [51, 52] (Table 1). Future well-designed trials will be needed to accurately assess their beneficial effects and potential risks as well as their cost performance, although existing statements by authorities already recommend lifestyle modification as a key strategy for dealing with the metabolic syndrome [34, 35].
4 Diagnosis of metabolic syndrome
The metabolic syndrome is now a worldwide public health concern, and there are urgent needs to take global action against the syndrome. To identify individuals with the metabolic syndrome, or its high risk population in the world, the establishment of its valid diagnostic criteria unified across ethnicity and country is critical. To this end, several working groups have made an effort to establish such diagnostic tools. Most recently, the International Diabetes Federation (IDF) and the American Heart Association/National Heart, Lung, and Blood Institute (AHA/NHLBI) collaborated and delivered a joint statement on unified diagnostic criteria of the metabolic syndrome [53]. However, some cautions will be need in their practical use.
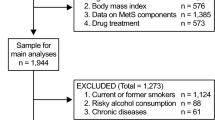
According to the criteria, the metabolic syndrome can be diagnosed when subjects have three or more of the following five components: abdominal obesity, elevated triglycerides levels, reduced high-density lipoprotein cholesterol levels, elevated blood pressure, and elevated fasting glucose levels. In other words, in the criteria, abdominal obesity was not treated as an obligatory component required in the diagnosis. That was in contrast to other criteria previously proposed such as the prior version of the IDF criteria [35] and those proposed in Japan [34], which positioned abdominal obesity as an obligatory component of the diagnosis. Consequently, the current joint criteria by the IDF and the AHA/NHLBI mean that some subjects diagnosed as the metabolic syndrome may have metabolic abnormalities without abdominal obesity. Indeed, we confirmed in a Japanese population that a substantial number of subjects who had three or more metabolic abnormalities and could be diagnosed as the metabolic syndrome according to their criteria were free from abdominal obesity (Fig. 2) [54]. As discussed above, in subjects who have metabolic abnormalities as well as abdominal obesity, a strategy of targeting visceral fat reduction is expected to be beneficial. On the other hand, in subjects with metabolic abnormalities but without abdominal obesity, such a strategy will not be so effective, since visceral fat accumulation is unlikely the origin of their metabolic abnormalities. Their metabolic abnormalities may be coincidently overlapped and medical intervention to respective independent etiologies may be required [21]. It would be worth emphasizing in healthcare practice that the metabolic syndrome diagnosed by their joint criteria is composed of two different pathogeneses which may require different management strategies.
Waist circumference in subjects with three or more metabolic abnormalities [54]. Data are the distribution of waist circumference in Japanese male (A) and female (B) employees, who had three or more of the following four components: hypertriglyceridemia, decreased HDL cholesterol level, raised blood pressure, and elevated fasting glucose level. These subjects therefore could be diagnosed as the metabolic syndrome according to the current joint criteria by the IDF and the AHA/NHLBI [53]. They accounted for 58 % of males and 71 % of females with the metabolic syndrome. Note that the cutoff points of waist circumference for detecting abdominal obesity in Japanese males and females are proposed to be 85 cm and 90 cm, respectively [34]. (From Takahara M, Kaneto H, Shimomura I. High prevalence of normal waist circumference in Japanese employees with a cluster of metabolic abnormalities. J Atheroscler Thromb. 2013;20(3):310–2, with permission of the Japan Atherosclerosis Society)
It should be also noted that the diagnostic criteria of the metabolic syndrome is not a tool to predict future absolute cardiometabolic risk [53]. It is true that patients with the metabolic syndrome have an increased risk for future development of CVD and type 2 diabetes mellitus [55, 56]. However, the diagnostic criteria were not developed for the primary purpose of predicting these risks. They does not contain many of the factors that determine these absolute risks, such as age, sex, cigarette smoking, and total or low-density lipoprotein cholesterol levels for CVD [57–61], and age, sex, and family history of diabetes mellitus for type 2 diabetes mellitus [62–65]. The risk assessment based on such diagnostic criteria are therefore at risk of inaccuracy and might be misleading. The risk for future development of CVD and type 2 diabetes mellitus should be estimated rather by the risk prediction tools developed for the purposes [66–70].
5 Identification of abdominal obesity
Epidemiological studies have demonstrated that cardiometabolic risks is increased in an almost linear fasion as visceral fat is accumulated [71]. This relationship indicates that waist circumference, a relevant index of visceral fat accumulation [72], has no clear threshold above which cardiometabolic risks would increase sharply. Nonetheless, to act against abdominal obesity in healthcare practice, a cutoff point of waist circumference needs to be determined as the action level.
In the current joint criteria of the metabolic syndrome by the IDF and AHA/ NHLBI, adhering to the prior version of the IDF criteria, proposed different cutoff points in different populations and ethnic groups [53, 35]. This sensible idea was based on the recognition that different ethnic groups had different relationships of waist circumference to cardiometabolic risks, partly due to the interethnic difference in body shape, and partly due to that in susceptibility to cardiometabolic risks [35, 73–78]. Based on this idea, they proposed ethnic-specific cutoff points of waist circumference, which were originally derived from previous studies performed in individual ethnic groups [35, 53]. The process for proposing ethnic-specific cutoff points would be apparently logical. However, it should be noted that these cutoff points in different ethnic groups were originally derived from studies separately performed through different statistical procedures based on different working hypotheses. The current joint criteria just diverted and reproduced these values, ignoring their difference in statistical procedures.
For example, Western countries derived their cutoff points of waist circumference from its correlation with body mass index [79–81]. The cutoff points were set to be the values corresponding to 25 or 30 kg/m2 of body mass index, well established cutoff points of body mass index for detecting general adiposity. General adiposity is involved not only in metabolic abnormalities but also in other unfavorable health problems, e.g., osteoarthritis. This statistical approach would enable to detect general adiposity including abdominal adiposity by waist circumference as a substitute for body mass index.
In contrast, some Asian countries attempted to develop their cutoff points by the use of the receiver operating characteristic (ROC) curve for detecting a clustering of metabolic abnormalities [82–85]. Importantly, metabolic abnormalities cannot be assessed without sphygmomanometer or blood sampling. The assessment may be difficult in some healthcare fields. The ROC curve-derived cutoff points of waist circumference will fit the purpose of predicting the presence of undiagnosed metabolic abnormalities in these fields.
On the other hand, in Japan, the cutoff points was set to correspond to the absolute risk of the presence of metabolic abnormalities; subjects with waist circumference above the cutoff points are likely to have more than one metabolic abnormality [34]. These cutoff points are assumed to be used in the environment where metabolic abnormalities can be directly assessed by sphygmomanometer and blood sampling. When subjects are found to have metabolic abnormalities, it can be judged by using the cutoff points whether their metabolic abnormalities come from visceral fat accumulation or not.
As thus far seen, the currently prosed ethnic-specific cutoff points of waist circumference were based on various working hypotheses and were derived from various statistical approaches. Different statistical procedures themselves can cause the generation of different cutoff points, as we illustrated elsewhere using a data of a Japanese population (Table 2) [71]. It is also noteworthy that the cutoff points are dependent on age of the population. Analyses in different age-groups provide different cutoff points, irrespective of statistical procedures, as shown in Table 2. Furthermore, when the cutoff points are derived from the ROC-curve analysis, they are also influenced by the distribution of waist circumference in the population. For example, in our simulated Japanese populations, a right or left shift of the distribution by 5 cm resulted in an increment or decrement of the cutoff point by around 5 cm, respectively [71]. These findings indicate that both different statistical approaches and different population attributes such as age and waist circumference distribution could generate different optimal cutoff points of waist circumference, even in a same ethnic group. Practically in healthcare settings, action should be taken on the basis of the proper cutoff points of waist circumference for its definite purpose.
6 Deeper understanding of metabolic syndrome
It is now well recognized that an excessive amount of intra-abdominal visceral adipose deposition is closely involved in a clustering of metabolic abnormalities, whereas subcutaneous adipose deposition in contrast demonstrates if any weaker associations with these CVD risk factors [15, 16, 86, 87]. Visceral fat accumulation is no doubt a key feature of the metabolic syndrome. Nonetheless, the following two points, apparently conflicting, would be also worth mentioning for a deeper understanding of the metabolic syndrome.
First, ample evidence has indicated that visceral fat accumulation is not only a cause of the pathophysiology but also is a marker of a morbid condition in which dysfunctional adipose tissue is unable to appropriately store the energy excess, resulting in non-physiological fat deposition in non-adipose tissues, e.g., the liver, the skeletal muscle, the pancreas, and the heart [88, 89]. Such morbid fat deposition in undesirable sites, called ectopic fat deposition, has been revealed to play an important role in the pathophysiology of the metabolic syndrome, along with an excessive visceral fat deposition [90–100]. The comparable importance of ectopic fat deposition may be partly supported by a series of recent clinical trials in patients with abdominal obesity, which reported that surgical removal of visceral fat by omentectomy brings a limited, or no obvious improvement in metabolic profiles in human [101–106]. Nonetheless, the emphasis on visceral fat accumulation as an origin of various metabolic abnormalities would make sense in healthcare practice, because waist circumference, as its relevant index [72], is a simple and familiar barometer with reality to general population and is expected to easily receive popular attention. Furthermore, practically in healthcare fields, visceral fat reduction through lifestyle modification programs is actually accompanied by ectopic fat reduction, which brings a successful improvement of metabolic profiles [107–109]. The chief focus on waist circumference is likely a practical strategy in healthcare fields. Waist circumference will therefore continue to be a purposeful index in healthcare practice.
Second, although associated metabolic abnormalities, i.e., elevated blood pressure, lipid abnormalities, and hyperglycemia, are often equally treated without any weighting in discussing the metabolic syndrome, the involvement of visceral adiposity considerably varies among these metabolic abnormalities, as suggested by a broad range of R 2 of metabolic parameters in Fig. 1. Indeed, as shown in Table 3, despite significant associations of waist circumference with all kinds of metabolic abnormalities, the impacts of waist circumference quite differed among the metabolic abnormalities. The impact was the strongest on lipid abnormalities, followed by elevated blood pressure and hyperglycemia. Importantly, the difference in the impact on metabolic abnormalities was observed not only regarding waist circumference at baseline, but also regarding the change of waist circumference from baseline. Practically in healthcare settings, these findings suggest that visceral fat reduction would bring different beneficial effects among metabolic abnormalities. The presence of lipid abnormalities would be the most sensitive to the change of waist circumference, whereas that of hyperglycemia would be the least. It implies that patients who had a clustering of all the three metabolic abnormalities as well as visceral adiposity in the past and have succeeded in visceral fat reduction might most likely get rid of lipid abnormalities. On the other hand, patients who were free from any metabolic abnormality in the past and have gained waist circumference might be more likely subject to lipid abnormalities than to hyperglycemia. The understanding of these associations would be of healthcare importance to appropriately interpret the change of the risk accumulation along with the change of waist circumference.
7 Conclusions
Visceral fat accumulation is importantly involved in the clustering of metabolic abnormalities, leading to an increase of future CVD risk. The concept is now well recognized as the metabolic syndrome. The introduction of this concept to healthcare settings would be beneficial for public CVD risk reduction.
References
Kannel WB, Dawber TR, Kagan A, Revotskie N, Stokes 3rd J. Factors of risk in the development of coronary heart disease–six year follow-up experience. The Framingham study. Ann Intern Med. 1961;55:33–50.
Stamler J, Wentworth D, Neaton JD. Is relationship between serum cholesterol and risk of premature death from coronary heart disease continuous and graded? Findings in 356,222 primary screenees of the Multiple Risk Factor Intervention Trial (MRFIT). JAMA. 1986;256(20):2823–8.
Vague J. La differenciation sexuelle, feateur determinant des formes de l’obesite. Presse Med. 1947;55:339–40.
Fujioka S, Matsuzawa Y, Tokunaga K, Tarui S. Contribution of intra-abdominal fat accumulation to the impairment of glucose and lipid metabolism in human obesity. Metabolism. 1987;36(1):54–9.
Kanai H, Matsuzawa Y, Kotani K, Keno Y, Kobatake T, Nagai Y, et al. Close correlation of intra-abdominal fat accumulation to hypertension in obese women. Hypertension. 1990;16(5):484–90.
Nakamura T, Tokunaga K, Shimomura I, Nishida M, Yoshida S, Kotani K, et al. Contribution of visceral fat accumulation to the development of coronary artery disease in non-obese men. Atherosclerosis. 1994;107(2):239–46.
Hotamisligil GS, Shargill NS, Spiegelman BM. Adipose expression of tumor necrosis factor-alpha: direct role in obesity-linked insulin resistance. Science. 1993;259(5091):87–91.
Zhang Y, Proenca R, Maffei M, Barone M, Leopold L, Friedman JM. Positional cloning of the mouse obese gene and its human homologue. Nature. 1994;372(6505):425–32. doi:10.1038/372425a0.
Maeda K, Okubo K, Shimomura I, Funahashi T, Matsuzawa Y, Matsubara K. cDNA cloning and expression of a novel adipose specific collagen-like factor, apM1 (AdiPose Most abundant Gene transcript 1). Biochem Biophys Res Commun. 1996;221(2):286–9. doi:10.1006/bbrc.1996.0587.
Shimomura I, Funahashi T, Takahashi M, Maeda K, Kotani K, Nakamura T, et al. Enhanced expression of PAI-1 in visceral fat: possible contributor to vascular disease in obesity. Nat Med. 1996;2(7):800–3.
Matsumoto S, Kishida K, Shimomura I, Maeda N, Nagaretani H, Matsuda M, et al. Increased plasma HB-EGF associated with obesity and coronary artery disease. Biochem Biophys Res Commun. 2002;292(3):781–6. doi:10.1006/bbrc.2002.6720.
World Health Organization. 2008–2013 action plan for the global strategy for the prevention and control of noncommunicable diseases : prevent and control cardiovascular diseases, cancers, chronic respiratory diseases and diabetes. Geneva: WHO Press; 2008.
Tokunaga K, Matsuzawa Y, Ishikawa K, Tarui S. A novel technique for the determination of body fat by computed tomography. Int J Obes. 1983;7(5):437–45.
Anderson PJ, Chan JC, Chan YL, Tomlinson B, Young RP, Lee ZS, et al. Visceral fat and cardiovascular risk factors in Chinese NIDDM patients. Diabetes Care. 1997;20(12):1854–8.
Fox CS, Massaro JM, Hoffmann U, Pou KM, Maurovich-Horvat P, Liu CY, et al. Abdominal visceral and subcutaneous adipose tissue compartments: association with metabolic risk factors in the Framingham heart study. Circulation. 2007;116(1):39–48. doi:10.1161/CIRCULATIONAHA.106.675355.
Liu J, Fox CS, Hickson DA, May WD, Hairston KG, Carr JJ, et al. Impact of abdominal visceral and subcutaneous adipose tissue on cardiometabolic risk factors: the Jackson heart study. J Clin Endocrinol Metab. 2010;95(12):5419–26. doi:10.1210/jc.2010-1378.
Arita Y, Kihara S, Ouchi N, Takahashi M, Maeda K, Miyagawa J, et al. Paradoxical decrease of an adipose-specific protein, adiponectin, in obesity. Biochem Biophys Res Commun. 1999;257(1):79–83.
Ryo M, Nakamura T, Kihara S, Kumada M, Shibazaki S, Takahashi M, et al. Adiponectin as a biomarker of the metabolic syndrome. Circ J. 2004;68(11):975–81.
Nishimura A, Sawai T. Determination of adiponectin in serum using a latex particle-enhanced turbidimetric immunoassay with an automated analyzer. Clin Chim Acta. 2006;371(1–2):163–8. doi:10.1016/j.cca.2006.03.008.
Ai M, Otokozawa S, Asztalos BF, White CC, Cupples LA, Nakajima K, et al. Adiponectin: an independent risk factor for coronary heart disease in men in the Framingham offspring study. Atherosclerosis. 2011;217(2):543–8. doi:10.1016/j.atherosclerosis.2011.05.035.
Matsuzawa Y, Funahashi T, Nakamura T. The concept of metabolic syndrome: contribution of visceral fat accumulation and its molecular mechanism. J Atheroscler Thromb. 2011;18(8):629–39.
Matsuzawa Y, Funahashi T, Kihara S, Shimomura I. Adiponectin and metabolic syndrome. Arterioscler Thromb Vasc Biol. 2004;24(1):29–33. doi:10.1161/01.ATV.0000099786.99623.EF.
Takahara M, Katakami N, Kaneto H, Noguchi M, Shimomura I. Contribution of visceral fat accumulation and Adiponectin to the clustering of metabolic abnormalities in a Japanese population. J Atheroscler Thromb. 2014;21(6):543–53.
de Koning L, Merchant AT, Pogue J, Anand SS. Waist circumference and waist-to-hip ratio as predictors of cardiovascular events: meta-regression analysis of prospective studies. Eur Heart J. 2007;28(7):850–6. doi:10.1093/eurheartj/ehm026.
Browning LM, Hsieh SD, Ashwell M. A systematic review of waist-to-height ratio as a screening tool for the prediction of cardiovascular disease and diabetes: 0.5 could be a suitable global boundary value. Nutr Res Rev. 2010;23(2):247–69. doi:10.1017/S0954422410000144.
Czernichow S, Kengne AP, Stamatakis E, Hamer M, Batty GD. Body mass index, waist circumference and waist-hip ratio: which is the better discriminator of cardiovascular disease mortality risk?: evidence from an individual-participant meta-analysis of 82 864 participants from nine cohort studies. Obes Rev. 2011;12(9):680–7. doi:10.1111/j.1467-789X.2011.00879.x.
Wormser D, Kaptoge S, Di Angelantonio E, Wood AM, Pennells L, Thompson A, et al. Separate and combined associations of body-mass index and abdominal adiposity with cardiovascular disease: collaborative analysis of 58 prospective studies. Lancet. 2011;377(9771):1085–95. doi:10.1016/S0140-6736(11)60105-0.
Okauchi Y, Nishizawa H, Funahashi T, Ogawa T, Noguchi M, Ryo M, et al. Reduction of visceral fat is associated with decrease in the number of metabolic risk factors in Japanese men. Diabetes Care. 2007;30(9):2392–4. doi:10.2337/dc07-0218.
Okauchi Y, Kishida K, Funahashi T, Noguchi M, Ogawa T, Ryo M, et al. Changes in serum adiponectin concentrations correlate with changes in BMI, waist circumference, and estimated visceral fat area in middle-aged general population. Diabetes Care. 2009;32(10):e122. doi:10.2337/dc09-1130.
Borel AL, Nazare JA, Smith J, Almeras N, Tremblay A, Bergeron J, et al. Visceral and not subcutaneous abdominal adiposity reduction drives the benefits of a 1-year lifestyle modification program. Obesity (Silver Spring). 2012;20(6):1223–33. doi:10.1038/oby.2011.396.
Borel AL, Nazare JA, Smith J, Almeras N, Tremblay A, Bergeron J, et al. Improvement in insulin sensitivity following a 1-year lifestyle intervention program in viscerally obese men: contribution of abdominal adiposity. Metabolism. 2012;61(2):262–72. doi:10.1016/j.metabol.2011.06.024.
Pelletier-Beaumont E, Arsenault BJ, Almeras N, Bergeron J, Tremblay A, Poirier P, et al. Normalization of visceral adiposity is required to normalize plasma apolipoprotein B levels in response to a healthy eating/physical activity lifestyle modification program in viscerally obese men. Atherosclerosis. 2012;221(2):577–82. doi:10.1016/j.atherosclerosis.2012.01.023.
Okauchi Y, Kishida K, Funahashi T, Noguchi M, Morita S, Ogawa T, et al. 4-year follow-up of cardiovascular events and changes in visceral fat accumulation after health promotion program in the Amagasaki visceral fat study. Atherosclerosis. 2010;212(2):698–700. doi:10.1016/j.atherosclerosis.2010.06.011.
The Examination Committee of Criteria for the Metabolic Syndrome in Japan. Definition and diagnostic criteria of the metabolic syndrome. J Japan Soc Intern Med. 2005;94:794–809 (in Japanese).
Alberti KG, Zimmet P, Shaw J. Metabolic syndrome–a new world-wide definition. A consensus statement from the international diabetes federation. Diabet Med. 2006;23(5):469–80. doi:10.1111/j.1464-5491.2006.01858.x.
Jensen MD, Ryan DH, Apovian CM, Ard JD, Comuzzie AG, Donato KA, et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American college of cardiology/American heart association task force on practice guidelines and the obesity society. Circulation. 2014;129(25 Suppl 2):S102–38. doi:10.1161/01.cir.0000437739.71477.ee.
Sacks FM, Bray GA, Carey VJ, Smith SR, Ryan DH, Anton SD, et al. Comparison of weight-loss diets with different compositions of fat, protein, and carbohydrates. N Engl J Med. 2009;360(9):859–73. doi:10.1056/NEJMoa0804748.
Vissers D, Hens W, Taeymans J, Baeyens JP, Poortmans J, Van Gaal L. The effect of exercise on visceral adipose tissue in overweight adults: a systematic review and meta-analysis. PLoS One. 2013;8(2):e56415. doi:10.1371/journal.pone.0056415.
Nazare JA, Smith J, Borel AL, Almeras N, Tremblay A, Bergeron J, et al. Changes in both global diet quality and physical activity level synergistically reduce visceral adiposity in men with features of metabolic syndrome. J Nutr. 2013;143(7):1074–83. doi:10.3945/jn.113.175273.
Chilton M, Dunkley A, Carter P, Davies MJ, Khunti K, Gray LJ. The effect of antiobesity drugs on waist circumference: a mixed treatment comparison. Diabetes Obes Metab. 2014;16(3):237–47. doi:10.1111/dom.12198.
Chan EW, He Y, Chui CS, Wong AY, Lau WC, Wong IC. Efficacy and safety of lorcaserin in obese adults: a meta-analysis of 1-year randomized controlled trials (RCTs) and narrative review on short-term RCTs. Obes Rev. 2013;14(5):383–92. doi:10.1111/obr.12015.
Viner RM, Hsia Y, Tomsic T, Wong IC. Efficacy and safety of anti-obesity drugs in children and adolescents: systematic review and meta-analysis. Obes Rev. 2010;11(8):593–602. doi:10.1111/j.1467-789X.2009.00651.x.
Padwal R, Li SK, Lau DC. Long-term pharmacotherapy for obesity and overweight. Cochrane Database Syst Rev. 2004;3, CD004094. doi:10.1002/14651858.CD004094.pub2.
Padwal RS, Majumdar SR. Drug treatments for obesity: orlistat, sibutramine, and rimonabant. Lancet. 2007;369(9555):71–7. doi:10.1016/S0140-6736(07)60033-6.
Kim MK, Kim W, Kwon HS, Baek KH, Kim EK, Song KH. Effects of bariatric surgery on metabolic and nutritional parameters in severely obese Korean patients with type 2 diabetes: a prospective 2-year follow up. J Diabetes Investig. 2014;5(2):221–7. doi:10.1111/jdi.12137.
Bradley D, Conte C, Mittendorfer B, Eagon JC, Varela JE, Fabbrini E, et al. Gastric bypass and banding equally improve insulin sensitivity and beta cell function. J Clin Invest. 2012;122(12):4667–74. doi:10.1172/JCI64895.
Olbers T, Bjorkman S, Lindroos A, Maleckas A, Lonn L, Sjostrom L, et al. Body composition, dietary intake, and energy expenditure after laparoscopic Roux-en-Y gastric bypass and laparoscopic vertical banded gastroplasty: a randomized clinical trial. Ann Surg. 2006;244(5):715–22. doi:10.1097/01.sla.0000218085.25902.f8.
Miller GD, Carr JJ, Fernandez AZ. Regional fat changes following weight reduction from laparoscopic Roux-en-Y gastric bypass surgery. Diabetes Obes Metab. 2011;13(2):189–92. doi:10.1111/j.1463-1326.2010.01338.x.
Adams TD, Gress RE, Smith SC, Halverson RC, Simper SC, Rosamond WD, et al. Long-term mortality after gastric bypass surgery. N Engl J Med. 2007;357(8):753–61. doi:10.1056/NEJMoa066603.
Yanovski SZ, Yanovski JA. Long-term drug treatment for obesity: a systematic and clinical review. JAMA. 2014;311(1):74–86. doi:10.1001/jama.2013.281361.
Ryo M, Nakamura T, Funahashi T, Noguchi M, Kishida K, Okauchi Y, et al. Health education “Hokenshido” program reduced metabolic syndrome in the Amagasaki visceral fat study. Three-year follow-up study of 3,174 Japanese employees. Intern Med. 2011;50(16):1643–8.
Muramoto A, Yamamoto N, Nakamura M, Koike G, Numata T, Tamakoshi A, et al. Effect of intensive lifestyle intervention programs on metabolic syndrome and obesity: how much weight reduction is needed to improve metabolic comorbidities? J Jpn Soc Study Obes. 2010;16(3):182–7 (in Japanese).
Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, et al. Harmonizing the metabolic syndrome: a joint interim statement of the international diabetes federation task force on epidemiology and prevention; national heart, lung, and blood institute; American heart association; world heart federation; international atherosclerosis society; and international association for the study of obesity. Circulation. 2009;120(16):1640–5. doi:10.1161/CIRCULATIONAHA.109.192644.
Takahara M, Kaneto H, Shimomura I. High prevalence of normal waist circumference in Japanese employees with a cluster of metabolic abnormalities. J Atheroscler Thromb. 2013;20(3):310–2.
Mottillo S, Filion KB, Genest J, Joseph L, Pilote L, Poirier P, et al. The metabolic syndrome and cardiovascular risk a systematic review and meta-analysis. J Am Coll Cardiol. 2010;56(14):1113–32. doi:10.1016/j.jacc.2010.05.034.
Shin JA, Lee JH, Lim SY, Ha HS, Kwon HS, Park YM, et al. Metabolic syndrome as a predictor of type 2 diabetes, and its clinical interpretations and usefulness. J Diabetes Investig. 2013;4(4):334–43. doi:10.1111/jdi.12075.
Wilson PW, D”Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97(18):1837–47.
Chambless LE, Folsom AR, Sharrett AR, Sorlie P, Couper D, Szklo M, et al. Coronary heart disease risk prediction in the Atherosclerosis Risk in Communities (ARIC) study. J Clin Epidemiol. 2003;56(9):880–90.
Assmann G, Cullen P, Schulte H. Simple scoring scheme for calculating the risk of acute coronary events based on the 10-year follow-up of the prospective cardiovascular Munster (PROCAM) study. Circulation. 2002;105(3):310–5.
Hippisley-Cox J, Coupland C, Vinogradova Y, Robson J, May M, Brindle P. Derivation and validation of QRISK, a new cardiovascular disease risk score for the United Kingdom: prospective open cohort study. BMJ. 2007;335(7611):136. doi:10.1136/bmj.39261.471806.55.
Conroy RM, Pyorala K, Fitzgerald AP, Sans S, Menotti A, De Backer G, et al. Estimation of ten-year risk of fatal cardiovascular disease in Europe: the SCORE project. Eur Heart J. 2003;24(11):987–1003.
Hippisley-Cox J, Coupland C, Robson J, Sheikh A, Brindle P. Predicting risk of type 2 diabetes in England and Wales: prospective derivation and validation of QDScore. BMJ. 2009;338:b880. doi:10.1136/bmj.b880.
Doi Y, Ninomiya T, Hata J, Hirakawa Y, Mukai N, Iwase M, et al. Two risk score models for predicting incident Type 2 diabetes in Japan. Diabet Med. 2012;29(1):107–14. doi:10.1111/j.1464-5491.2011.03376.x.
Alssema M, Vistisen D, Heymans MW, Nijpels G, Glumer C, Zimmet PZ, et al. The evaluation of screening and early detection strategies for type 2 Diabetes and Impaired Glucose Tolerance (DETECT-2) update of the Finnish diabetes risk score for prediction of incident type 2 diabetes. Diabetologia. 2011;54(5):1004–12. doi:10.1007/s00125-010-1990-7.
Stern MP, Williams K, Haffner SM. Identification of persons at high risk for type 2 diabetes mellitus: do we need the oral glucose tolerance test? Ann Intern Med. 2002;136(8):575–81.
Wannamethee SG, Shaper AG, Lennon L, Morris RW. Metabolic syndrome vs Framingham risk score for prediction of coronary heart disease, stroke, and type 2 diabetes mellitus. Arch Intern Med. 2005;165(22):2644–50. doi:10.1001/archinte.165.22.2644.
McNeill AM, Rosamond WD, Girman CJ, Golden SH, Schmidt MI, East HE, et al. The metabolic syndrome and 11-year risk of incident cardiovascular disease in the atherosclerosis risk in communities study. Diabetes Care. 2005;28(2):385–90.
Wannamethee SG. The metabolic syndrome and cardiovascular risk in the British regional heart study. Int J Obes. 2008;32 Suppl 2:S25–9. doi:10.1038/ijo.2008.32.
Cameron AJ, Magliano DJ, Zimmet PZ, Welborn TA, Colagiuri S, Tonkin AM, et al. The metabolic syndrome as a tool for predicting future diabetes: the AusDiab study. J Intern Med. 2008;264(2):177–86. doi:10.1111/j.1365-2796.2008.01935.x.
Stern MP, Williams K, Gonzalez-Villalpando C, Hunt KJ, Haffner SM. Does the metabolic syndrome improve identification of individuals at risk of type 2 diabetes and/or cardiovascular disease? Diabetes Care. 2004;27(11):2676–81.
Takahara M, Katakami N, Kaneto H, Noguchi M, Shimomura I. Statistical reassessment of the association between waist circumference and clustering metabolic abnormalities in Japanese population. J Atheroscler Thromb. 2012;19(8):767–78.
Pouliot MC, Despres JP, Lemieux S, Moorjani S, Bouchard C, Tremblay A, et al. Waist circumference and abdominal sagittal diameter: best simple anthropometric indexes of abdominal visceral adipose tissue accumulation and related cardiovascular risk in men and women. Am J Cardiol. 1994;73(7):460–8.
Expert WHO. Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363(9403):157–63.
Despres JP, Couillard C, Gagnon J, Bergeron J, Leon AS, Rao DC, et al. Race, visceral adipose tissue, plasma lipids, and lipoprotein lipase activity in men and women: the Health, Risk Factors, Exercise Training, and Genetics (HERITAGE) family study. Arterioscler Thromb Vasc Biol. 2000;20(8):1932–8.
Tan CE, Ma S, Wai D, Chew SK, Tai ES. Can we apply the national cholesterol education program adult treatment panel definition of the metabolic syndrome to Asians? Diabetes Care. 2004;27(5):1182–6.
Lear SA, Toma M, Birmingham CL, Frohlich JJ. Modification of the relationship between simple anthropometric indices and risk factors by ethnic background. Metabolism. 2003;52(10):1295–301.
Kadowaki T, Sekikawa A, Murata K, Maegawa H, Takamiya T, Okamura T, et al. Japanese men have larger areas of visceral adipose tissue than Caucasian men in the same levels of waist circumference in a population-based study. Int J Obes. 2006;30(7):1163–5. doi:10.1038/sj.ijo.0803248.
Lovejoy JC, de la Bretonne JA, Klemperer M, Tulley R. Abdominal fat distribution and metabolic risk factors: effects of race. Metabolism. 1996;45(9):1119–24.
Balkau B, Charles MA. Comment on the provisional report from the WHO consultation. European GROUP for the Study of Insulin Resistance (EGIR). Diabet Med. 1999;16(5):442–3.
Executive summary of the third report of the national cholesterol education program (NCEP) Expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III). Jama. 2001;285(19):2486–97.
Lean ME, Han TS, Morrison CE. Waist circumference as a measure for indicating need for weight management. BMJ. 1995;311(6998):158–61.
Lin WY, Lee LT, Chen CY, Lo H, Hsia HH, Liu IL, et al. Optimal cut-off values for obesity: using simple anthropometric indices to predict cardiovascular risk factors in Taiwan. Int J Obes Relat Metab Disord. 2002;26(9):1232–8. doi:10.1038/sj.ijo.0802040.
Wildman RP, Gu D, Reynolds K, Duan X, He J. Appropriate body mass index and waist circumference cutoffs for categorization of overweight and central adiposity among Chinese adults. Am J Clin Nutr. 2004;80(5):1129–36.
Zhou BF. Predictive values of body mass index and waist circumference for risk factors of certain related diseases in Chinese adults–study on optimal cut-off points of body mass index and waist circumference in Chinese adults. Biomed Environ Sci. 2002;15(1):83–96.
Snehalatha C, Viswanathan V, Ramachandran A. Cutoff values for normal anthropometric variables in asian Indian adults. Diabetes Care. 2003;26(5):1380–4.
Hiuge-Shimizu A, Kishida K, Funahashi T, Ishizaka Y, Oka R, Okada M, et al. Absolute value of visceral fat area measured on computed tomography scans and obesity-related cardiovascular risk factors in large-scale Japanese general population (the VACATION-J study). Ann Med. 2012;44(1):82–92. doi:10.3109/07853890.2010.526138.
Oka R, Miura K, Sakurai M, Nakamura K, Yagi K, Miyamoto S, et al. Impacts of visceral adipose tissue and subcutaneous adipose tissue on metabolic risk factors in middle-aged Japanese. Obesity (Silver Spring). 2010;18(1):153–60. doi:10.1038/oby.2009.180.
Despres JP, Lemieux I. Abdominal obesity and metabolic syndrome. Nature. 2006;444(7121):881–7. doi:10.1038/nature05488.
Miranda PJ, DeFronzo RA, Califf RM, Guyton JR. Metabolic syndrome: definition, pathophysiology, and mechanisms. Am Heart J. 2005;149(1):33–45. doi:10.1016/j.ahj.2004.07.013.
Byrne CD, Targher G. Ectopic fat, insulin resistance, and nonalcoholic fatty liver disease: implications for cardiovascular disease. Arterioscler Thromb Vasc Biol. 2014;34(6):1155–61. doi:10.1161/ATVBAHA.114.303034.
Stefan N, Kantartzis K, Machann J, Schick F, Thamer C, Rittig K, et al. Identification and characterization of metabolically benign obesity in humans. Arch Intern Med. 2008;168(15):1609–16. doi:10.1001/archinte.168.15.1609.
Jacob S, Machann J, Rett K, Brechtel K, Volk A, Renn W, et al. Association of increased intramyocellular lipid content with insulin resistance in lean nondiabetic offspring of type 2 diabetic subjects. Diabetes. 1999;48(5):1113–9.
Yim JE, Heshka S, Albu J, Heymsfield S, Kuznia P, Harris T, et al. Intermuscular adipose tissue rivals visceral adipose tissue in independent associations with cardiovascular risk. Int J Obes. 2007;31(9):1400–5. doi:10.1038/sj.ijo.0803621.
Goodpaster BH, Thaete FL, Kelley DE. Thigh adipose tissue distribution is associated with insulin resistance in obesity and in type 2 diabetes mellitus. Am J Clin Nutr. 2000;71(4):885–92.
Toledo-Corral CM, Alderete TL, Hu HH, Nayak K, Esplana S, Liu T, et al. Ectopic fat deposition in prediabetic overweight and obese minority adolescents. J Clin Endocrinol Metab. 2013;98(3):1115–21. doi:10.1210/jc.2012-3806.
Wang CY, Ou HY, Chen MF, Chang TC, Chang CJ. Enigmatic ectopic fat: prevalence of nonalcoholic fatty pancreas disease and its associated factors in a Chinese population. J Am Heart Assoc. 2014;3(1):e000297. doi:10.1161/JAHA.113.000297.
Sacks HS, Fain JN. Human epicardial adipose tissue: a review. Am Heart J. 2007;153(6):907–17. doi:10.1016/j.ahj.2007.03.019.
Iacobellis G, Ribaudo MC, Assael F, Vecci E, Tiberti C, Zappaterreno A, et al. Echocardiographic epicardial adipose tissue is related to anthropometric and clinical parameters of metabolic syndrome: a new indicator of cardiovascular risk. J Clin Endocrinol Metab. 2003;88(11):5163–8. doi:10.1210/jc.2003-030698.
Iacobellis G, Leonetti F. Epicardial adipose tissue and insulin resistance in obese subjects. J Clin Endocrinol Metab. 2005;90(11):6300–2. doi:10.1210/jc.2005-1087.
Rabkin SW. The relationship between epicardial fat and indices of obesity and the metabolic syndrome: a systematic review and meta-analysis. Metab Syndr Relat Disord. 2014;12(1):31–42. doi:10.1089/met.2013.0107.
Csendes A, Maluenda F, Burgos AM. A prospective randomized study comparing patients with morbid obesity submitted to laparotomic gastric bypass with or without omentectomy. Obes Surg. 2009;19(4):490–4. doi:10.1007/s11695-008-9660-2.
Fabbrini E, Tamboli RA, Magkos F, Marks-Shulman PA, Eckhauser AW, Richards WO, et al. Surgical removal of omental fat does not improve insulin sensitivity and cardiovascular risk factors in obese adults. Gastroenterology. 2010;139(2):448–55. doi:10.1053/j.gastro.2010.04.056.
Herrera MF, Pantoja JP, Velazquez-Fernandez D, Cabiedes J, Aguilar-Salinas C, Garcia-Garcia E, et al. Potential additional effect of omentectomy on metabolic syndrome, acute-phase reactants, and inflammatory mediators in grade III obese patients undergoing laparoscopic Roux-en-Y gastric bypass: a randomized trial. Diabetes Care. 2010;33(7):1413–8. doi:10.2337/dc09-1833.
Dillard TH, Purnell JQ, Smith MD, Raum W, Hong D, Laut J, et al. Omentectomy added to Roux-en-Y gastric bypass surgery: a randomized, controlled trial. Surg Obes Relat Dis. 2013;9(2):269–75. doi:10.1016/j.soard.2011.09.027.
Tamboli RA, Hajri T, Jiang A, Marks-Shulman PA, Williams DB, Clements RH, et al. Reduction in inflammatory gene expression in skeletal muscle from Roux-en-Y gastric bypass patients randomized to omentectomy. PLoS One. 2011;6(12):e28577. doi:10.1371/journal.pone.0028577.
Lima MM, Pareja JC, Alegre SM, Geloneze SR, Kahn SE, Astiarraga BD, et al. Visceral fat resection in humans: effect on insulin sensitivity, beta-cell function, adipokines, and inflammatory markers. Obesity (Silver Spring). 2013;21(3):E182–9. doi:10.1002/oby.20030.
Schafer S, Kantartzis K, Machann J, Venter C, Niess A, Schick F, et al. Lifestyle intervention in individuals with normal versus impaired glucose tolerance. Eur J Clin Invest. 2007;37(7):535–43. doi:10.1111/j.1365-2362.2007.01820.x.
Bosy-Westphal A, Kossel E, Goele K, Blocker T, Lagerpusch M, Later W, et al. Association of pericardial fat with liver fat and insulin sensitivity after diet-induced weight loss in overweight women. Obesity (Silver Spring). 2010;18(11):2111–7. doi:10.1038/oby.2010.49.
Kim MK, Tanaka K, Kim MJ, Matuso T, Endo T, Tomita T, et al. Comparison of epicardial, abdominal and regional fat compartments in response to weight loss. Nutr Metab Cardiovasc Dis. 2009;19(11):760–6. doi:10.1016/j.numecd.2009.01.010.
Conflict of interest
None of the authors have conflict of interest to declare in relation with the content of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Takahara, M., Shimomura, I. Metabolic syndrome and lifestyle modification. Rev Endocr Metab Disord 15, 317–327 (2014). https://doi.org/10.1007/s11154-014-9294-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11154-014-9294-8