Abstract
We analyze the evolution of health insurer costs in Massachusetts between 2010 and 2012, paying particular attention to changes in the composition of enrollees. This was a period in which Health Maintenance Organizations (HMOs) increasingly used physician cost control incentives but Preferred Provider Organizations (PPOs) did not. We show that cost growth and its components cannot be understood without accounting for (1) consumers’ switching between plans, and (2) differences in cost characteristics between new entrants and those leaving the market. New entrants are markedly less costly than those leaving (and their costs fall after their entering year), so cost growth of continuing enrollees in a plan is significantly higher than average per-member cost growth. Relatively high-cost HMO members switch to PPOs while low-cost PPO members switch to HMOs, so the impact of cost control incentives on HMO costs is likely different from their impact on market-wide insurer costs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
We examine the factors that lead to changes in the medical costs of commercial insurers in Massachusetts between 2010 and 2012. We focus on the impact on costs of compositional changes in the population of enrollees.
The path of medical care costs in Massachusetts has been a topic of substantial policy interest since the Coakley Reports (2010, 2011, 2013) documented high price dispersion across hospitals. Some hospitals were paid prices that were twice as high as others for particular procedures. The state passed a major cost-containment law in 2012 that encouraged payment and delivery reforms with the goal of slowing cost growth below a target of the GDP growth rate.
In the wake of this reform, measuring cost growth has received increased attention, with state agencies issuing regular reports on cost trends: overall, and by insurer and market segment. The state also tracks insurers’ adoption of non-fee-for-service, “global” payment mechanisms that share risk with providers to encourage cost reductions—similar to the “shared savings” arrangements that are used by Accountable Care Organizations (ACOs). The use of global payments by major insurers in Massachusetts more than doubled between 2009 and 2012, and evidence has been presented that they have reduced costs in at least one insurer (Song et al. 2012, 2014). This issue is also of national interest due to the similarity of these payment arrangements to the shared savings programs that are used by ACOs.
We use the Massachusetts All-Payer Claims Database (APCD) to analyze the evolution of health care costs from 2010 to 2012. We focus on tracking changes in average costs per member per month in the three largest commercial insurers, which together cover 78% of the state’s commercial insurance market. We summarize cost increases for this population—both overall, and by plan—and then consider the possible determinants of these changes.
The results highlight the importance of accounting for changes in the composition of enrollees across years when analyzing the factors that lead to cost trends in the market as a whole and differences in trends across plans. Unlike in many other industries, costs in health care are determined by the interaction of the health care system with the types of consumers in the market: e.g., with respect to their health needs and illness severity. When sicker consumers differentially leave the market or switch into certain plans, this affects the analysis of cost trends and the comparison of those trends across plans.
For example, for the HMO plans of Blue Cross Blue Shield of Massachusetts (henceforth referred to as Blue Cross)—the largest insurer in our data—real costs per member per month fell by $3.73 between 2011 and 2012. In contrast, the costs of Blue Cross HMO customers who stayed in the plan over the period increased by $16.45. The $20 difference represents a 6% point increase in measured cost growth (as a share of Blue Cross’s average costs in 2011). This example illustrates a finding that emerges consistently in our data across insurers, plans, and years. Cost growth for stayers is much higher than for the full population, and this difference persists after controlling for observable changes in age, gender, and severity of diagnoses.
At one level, the importance of accounting for sample composition in analyzing costs is obvious. There is a long tradition in health insurance of studying “adverse selection”: the propensity of certain plans to attract consumers with attributes that make those consumers more costly (see Breyer et al. (2011) for a review). There is also widespread awareness that population aging will lead to health care cost growth. The most sophisticated methodologies allow a portion of cost changes to arise from changes in observable severity measures: notably, age and disease prevalence (e.g., Dunn et al. 2017). There is another literature that focuses on decomposing cost growth into changes in the prices versus quantities of medical services.Footnote 1 However none of these literatures have integrated the impact of compositional change into their analysis of the factors that lead to health care cost growth.
Our main analysis is based on a risk-adjusted decomposition of cost growth for enrollees in the state’s top three commercial health insurers’ plans.Footnote 2 The decomposition accounts for the fact that costs can increase either because of changes in the observable characteristics of the population—e.g., getting older or sicker—or because of cost increases for a given age and sickness level. We present a formal decomposition of cost changes into: (1) changes in the age-gender composition of the population, (2) changes in detailed measures of the population’s severity of diagnoses (conditional on age and gender), and (3) changes in costs for a given age-gender-severity group.
We first perform this decomposition for the actual enrollees in each insurer-plan type for each year from 2010 to 2012. We distinguish between Health Maintenance Organization (HMO)-type plans and Preferred Provider Organization (PPO)-type plans: we note that insurers used global or “alternative” payment arrangements almost exclusively in their HMO-type plans.Footnote 3 Our method is similar to those used in past papers that decompose cost growth, though it does not attempt to distinguish between cost changes that are due to changes in prices versus quantities of services. While we use a rich set of controls for illness severity and demographics, the method cannot directly account for changes in unobserved severity. Thus, our initial decomposition—like the standard methods in the literature—can be affected by changes in sample composition related to unobserved severity. For example, if consumers who switch out of HMOs and into PPOs are relatively sick in a way that our observables do not control for, a cost decomposition that does not control for compositional changes will generate a cost growth for the HMO that is lower than the actual cost growth for consumers who remained with the HMO in both years, and cost growth for the PPO that is higher than the actual cost growth for those who were in the PPO in both years.
This paper does not address causal issues such as the incentive to switch plans or the analysis of factors that lead to cost growth. Rather we focus on analyzing how the differences in costs—among “stayers” (those who remain in the data and do not switch plans between each pair of years), “switchers” (those who change plans between each pair of years), entrants into commercial insurance, and those who exit from commercial insurance—affect cost decompositions: in general, and by plan type. We find that compositional effects on overall cost growth are large. We also find an effect on the differences in cost growth across plans, though this effect is smaller. Our initial decomposition, which does not control for compositional changes, uses a relatively rich set of controls. We expect compositional effects to be even more notable in cost growth analysis that uses less detailed data.
Our initial decomposition finds several patterns. First, real health care costs per member-month are essentially flat over the 2-year period (after adjusting for inflation). After accounting for population aging and a small increase in severity, costs actually decline in most plans. We see differential trends across insurers and plans in this cost component. Blue Cross HMO and Tufts HMO—the plans with the greatest use of alternative payment arrangements—have negative cost growth, consistent with physicians’ responding to cost-control incentives. HMOs have consistently slower (or more negative) cost growth than do the PPOs that are offered by the same insurers.
As noted the initial decomposition does not adequately control for differences in the costs of stayers, switchers, entrants and those who exit. Moreover we show that higher-cost enrollees are more likely to exit the sample of people who are covered by the top three commercial insurers: e.g., by aging onto Medicare. Costs for “exiters” in their final year in the sample are typically 40–50% higher than for stayers in the same plans, and this difference varies across plans. Further, while new enrollees into the sample are more expensive in their first year, their costs decline over time so that in their second year they are typically about 10% less expensive than stayers. In addition, we show that even among people remaining in the sample over time, plan switching has an important effect on costs across plans. Switching of low-cost enrollees into HMO plans—i.e., “favorable selection” into HMOs—helps reduce their cost growth, particularly for the HMOs that first introduce global payments.
We repeat the risk-adjusted cost growth decomposition for the sample of “stayers”: enrollees who remain in the same plan between each pair of years.Footnote 4 We find much larger cost increases for this sample. This occurs partly because a fixed panel of people uniformly grows older over time—while the full population of commercial enrollees continually loses its oldest members to Medicare. Even conditional on age and severity, however, cost growth is consistently positive for the stayer population. We still find that HMOs have slower cost growth than do PPOs that are offered by the same insurer, although the gap is narrower than in the full sample. Both switching and entry patterns make it clear that HMOs benefit from attracting lower-cost consumers over the period we study. The differences across HMOs are in line with prior research: Earlier adopters of global payments tend to have lower cost growth than do other HMOs.
Though we make no attempt to attach a causal interpretation to our results, they are important for other reasons: First, we point out the potential for changes in the composition of consumers to affect the measurement of health care cost growth—particularly for market segments such as commercial insurance. Accurately measuring cost growth is important for assessing the impact of institutional change such as those instituted in Massachusetts and those due to the Affordable Care Act. Second, we contribute to the literature that studies the introduction of physician cost control incentives, and global payments in particular (e.g., Song et al. 2012, 2014). We provide evidence that HMOs that adopted global payments may have benefited from attracting lower-cost consumers disproportionately. Of course this may provide an additional incentive to adopt global payments, beyond any direct effect on costs for a fixed enrollee population, and be partially responsible for the diffusion of global payments. The analysis of these issues, however, is beyond the scope of this paper.
The paper proceeds as follows. Section 2 introduces the data, and Sect. 3 summarizes overall cost trends. Section 4 compares cost trends across plans with the use of several cost decompositions. The final section concludes.
2 Data
We use the Massachusetts All-Payer Claims Database (APCD) that is maintained by the state’s Center for Health Information and Analysis (CHIA). This is the most comprehensive available dataset on statewide health care use; it contains enrollment and claims data from all private health insurers. We use APCD version 2.0, which contains data from 2009 to 2012. It is one of the first available datasets in a larger group of state-level APCDs (ongoing in over 30 states) that give researchers unparalleled ability to analyze system-wide health care costs—including among privately insured populations. The claims data include patient diagnoses, procedures, provider and insurer identifiers, and actual prices that were paid for all medical services rendered.
We focus our analysis on the commercially insured population, which excludes government-sponsored programs such as Medicare and Medicaid. We limit attention to primary insurance products and to medical spending (excluding pharmacy and dental claims). We exclude individuals who live outside of Massachusetts or a neighboring state (NH, CT or RI) and individuals who were observed for less than 2 months. We further limit the sample to include just the three largest insurers: Blue Cross Blue Shield of MA (Blue Cross), Harvard Pilgrim Health Care (Harvard Pilgrim), and Tufts Health Plan. Each of these offers both HMO and PPO plans. Together, these three insurers constitute 78% of the commercial insurance market. The final dataset includes 2.7 million members per month in 2010 and then decreases somewhat over time (Table 1).
The primary variable considered in our analysis is insurers’ medical cost per member-month, adjusted for inflation into 2009 dollars using the CPI for New England states.Footnote 5 Our objective is to document and understand the sources of changes in this variable over time.
We construct two additional sets of variables as inputs into the decomposition of cost changes: The first set categorizes individuals into “risk groups” based on mutually exclusive combinations of age group, gender, and diagnosis severity. For age, we use 13 groupings (0–1, 2–24, 5 year groups from 25 to 74, and \(75+\)). We use the Johns Hopkins Adjusted Clinical Groups (ACG) risk-adjustment software to define severity groups. The software categorizes each enrollee into one of 93 ACG cells—intended to capture groups with similar expected spending—based on their demographics and diagnoses. Definitions of these groups are provided in Appendix Table 8.Footnote 6
We use the concurrent year of claims to define the ACG for each enrollee-year since the use of prior years would require restricting the sample to those continuously enrolled. We then form risk groups that are defined as the 1140 unique combinations of age, gender, and ACG categories. To address issues with small cell sizes, we eliminate cells with fewer than 30 member-months in any year and assign these enrollees to residual risk groups that are defined only by age and gender. These residual groups include just 0.06% of member-months.
The second set of variables categorizes types of insurance plans. We focus on distinguishing between enrollees in Health Maintenance Organizations (HMOs) and similar contracts (Point of Service (POS) plans and Exclusive Provider Organizations (EPOs)) versus Preferred Provider Organizations (PPOs) and indemnity plans. (For the remainder of the paper, we refer to the first set of plan types collectively as “HMOs” and the second as “PPOs.”) We address the problem that some consumers are enrolled in multiple products by assigning consumers to the plan in which they were enrolled for the majority of the months of a year (with ties assigned to PPOs). In our final sample, 71% of people are enrolled in HMOs, and 29% are enrolled in PPOs.
3 Industry Cost Trends
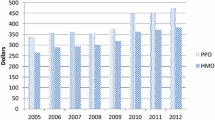
We begin by assessing aggregate cost changes in Massachusetts over time. Table 1 sets out, for each year 2010–2012, average spending (insurer plus patient contribution) per member per month, and the percent change in spending between years. We also provide data for 2009 for Harvard Pilgrim and Tufts; Blue Cross is excluded for this year because a data anomaly prevented the linking of its claims and enrollment file for a subset of its members. The number of enrollees in the full sample declined from 2.7 million to 2.6 million over the 3 years that we consider—probably due in part to an aging population shifting onto Medicare. Average inflation-adjusted spending per member per month increased by about 0.1% per year from 2010 to 2012.
These figures differ from those published in a 2014 report by CHIA and Massachusetts’ Health Policy Commission (CHIA 2014). That report considered the three largest commercial insurers and documented a 2.9% annual growth in medical claims-based spending. However, we adjust for inflation, while they report nominal dollar increases. This distinction explains almost the entire difference between these figures. We conclude that the growth rate in inflation-adjusted per member per month spending was a little less than the growth in the growth of U.S. real GDP per capita during this period (which was about 1.4%), and so quite low by historical standards.
4 Cost Decompositions
The cost growth rates in Table 1 differ across insurers. For example, Blue Cross costs fell in both years between 2010 and 2012 (by just under 1% in each year), while Harvard Pilgrim’s costs fell by around 2% between 2009 and 2011 but rose (by 6%) from 2011 to 2012. These differences are particularly interesting because—as noted—insurers were differentially expanding their use of alternative payment mechanisms for physicians during this time. Blue Cross HMO introduced its Alternative Quality Contract in 2009, under which several large provider organizations shifted to global payments.Footnote 7 Other insurers followed. However, Blue Cross continued to be the leader in adopting alternative payments.
Table 2 shows the share of commercial HMO members under these alternative payment mechanisms starting in 2012, the first year for which comprehensive data are available (CHIA 2015). By 2012, Blue Cross HMO had the highest share under alternative payments (at about 80%), followed by Tufts (at 54%) and then Harvard Pilgrim (at 38%). By contrast, based on the same data source, PPO plans almost never used these payment arrangements during our data period.
Our next step is a cost decomposition to investigate the sources of variation in cost growth across insurer-plan type combinations.
4.1 Cost Decomposition Method
Categorizing patients with the ACG grouper enables us to compare patients in the same “risk group”—with the same severity of reported diagnoses and in the same age-gender group—and ask how their costs differ by insurer and over time. Define the average per-enrollee cost in severity (ACG) group g and age-gender group a at time t to be \(C_{a,g,t}\). Then if \(s_{a,g,t}\) is the share of members at time t who are in group (a, g), the per-enrollee cost to the insurer can be written \(C_{t}=\sum _{a,g}C_{a,g,t}s_{a,g,t}\).
We decompose the cost changes for stayers over time into portions that are attributable to: (1) changes in the cost of treating a given severity and age-gender group; (2) changes that are due to differences in the distribution of enrollees across severities conditional on age and gender; and (3) changes that are due to age and/or gender. The intuition is that any differential selection (on observed severity and age) should affect parts (2) and (3), which leaves (1) as a clean measure of cost growth for a group of enrollees with fixed severity.Footnote 8
More formally we note that, since \(\frac{s_{a,g,t}}{s_{a,t}}\) is the fraction of people within group a that belong to classification g, we can write the cost change over time as:
The first term of the decomposition measures the contribution of changes in cost per group; the third measures the contribution of changes in the age-gender distribution; and the second measures changes in the distribution across severity groups conditional on age and gender.
4.2 Cost Decomposition for the Full Sample
The results of the cost decomposition for the full sample from 2010 to 2012 are reported in Table 3. The column labeled “Total $ Change” lists the average change in spending per member per month for the relevant sample across years. The remaining columns of Table 3 decompose this change into our three components.
There are sizable differences in cost changes across insurers. The total cost change from 2010 to 2012 is negative for Blue Cross HMO and PPO plans and for Tufts HMO; it is positive for Harvard Pilgrim HMO and PPO and for Tufts PPO. The cost reductions for Blue Cross and Tufts stem from the cost component of the decomposition: This is negative for all Blue Cross and Tufts plans over the 2-year period (ranging from − $12.83 for Blue Cross HMO to − $1.47 for Blue Cross PPO) while it is positive for Harvard Pilgrim’s plans ($2.85 for the HMO and $11.49 for the PPO). The other components of the cost decomposition are largely consistent in sign across plans, although their magnitudes differ. All plans except Blue Cross PPO have a shift in enrollment towards higher-cost severities given age (term 2 of the decomposition), and all have a shift towards older age groups, both of which tend to increase costs in this time period.
For Blue Cross, the shift in shares across severity groups given a is positive for the HMO and negative for the PPO ($2.27 compared to − $3.45). A naive interpretation of this finding is that it could imply upcoding in the HMO by physicians who have an incentive to increase the number and severity of diagnoses that are listed in the patient’s record, even if there is no change in actual patient severity.Footnote 9 The difference in the ‘shift in shares’ components between Blue Cross’s HMO and its PPO implies that the difference between the HMO and PPO growth rates of total costs greatly underestimates the difference in costs conditional on severity, gender, and age (which is over $11 per member per month). However, there are other explanations for this difference besides upcoding, and we shall see that the results change substantially with the sample that is considered in later analyses.
For every insurer in the table, the cost component is more negative for the insurer’s HMO than for its PPO. This finding—together with the fact that the largest reductions in the cost component are achieved in Blue Cross HMO and Tufts HMO, which are the plans with the earliest implementation of global payment arrangements—is consistent with physicians responding to the incentives that are generated by alternative payment mechanisms. However, part of the difference that we see in the indices in Table 3 is attributable to: (1) consumers’ switching plans (possibly in response to the changes in plan characteristics such as global capitation); and (2) differences in the numbers of entrants and exiters and the costs of these two groups. The next two sections separate the contribution of these phenomena to our cost measures.
4.3 Contributions of Entry and Exit
We begin by considering the contribution of entrants and exiters to cost growth in each plan. Table 4 investigates the differences between the full sample and the set of enrollees who enter and exit the sample, separately by insurer and plan type.Footnote 10 We provide cost statistics on entrants (those entering commercial insurance) and exiters (those moving out of the sample, e.g., into Medicare, Medicaid, or uninsurance, or by dying) in comparison to those for “stayers”, defined as enrollees neither entering, exiting, nor switching plans from 2011 to 2012. Enrollees switching plans but remaining in the sample are excluded from this table. We limit attention to Blue Cross and Harvard Pilgrim for brevity; numbers for Tufts are qualitatively similar.
Exiters from every plan have higher costs than do either stayers or entrants. For example, the average 2011 cost of Blue Cross HMO stayers was $300.71 (standard error $1.40), compared to an average of $388.18 (S.E. $4.76) for exiters in 2012 and $433.44 (S.E. $6.07) for exiters in 2011. The magnitudes differ across insurers and plan types, but the pattern persists.
Two additional facts are clear from this table: First, new entrants to the sample have higher costs in the first year than in their second year in the plan; this is consistent with pent-up demand for medical care being satisfied in year one. For example, for Blue Cross HMO 2011 entrants, the figures are $331.29 (S.E. $7.22) and $282.41 (S.E. $3.92) in 2011 and 2012 respectively. Conversely, exiters have particularly high costs in their last year in the data. For example, exiters from Blue Cross HMO in 2012 have 2011 costs of $388.18 (S.E. $4.76) and 2012 costs of $428.38 (S.E. $7.94). We conclude that the low overall cost growth rate is generated in part by lower-cost enrollees entering and more-expensive enrollees leaving the sample over time.Footnote 11
Next we turn to the contribution of individuals who switched plans to differential cost growth among plans, and then return to the cost growth of ‘stayers’ (those who were in the same plan in two consecutive years).
4.4 Differential Switching Across Plans
We now assess the role of consumer switching between the three carriers in the data. Plan switching is common in our sample: 12% of enrollees switch plans between 2011 and 2012. This is larger than the fraction who switch that is usually found in this literature.Footnote 12 However, this is a period in which there are changes in the characteristics of plans (and possibly also in the plans offered), and consumers may be more sensitive to these changes than to the premium changes that have been the focus of the prior switching literature. In addition, most of the literature focuses on switching that is made by consumers among a given set of options, while our switching number may also capture employers’ choices to change the menu of plans that are available to their workers. 16% of Blue Cross HMO and Tufts HMO enrollees switch plans at the end of 2011; these two plans account for about half the sample. Switching often takes place between plans within the same carrier. For example, over half of switchers from Blue Cross HMO move to Blue Cross PPO, while the rest move across carriers.
Cross-plan switchers will affect plan cost trends if switchers have different costs from non-switchers. In our sample, switchers from HMO to PPO plans tend to be high-cost, and switchers from PPO to HMO plans tend to be low-cost. Table 5 provides examples for Blue Cross HMO and Harvard Pilgrim PPO. Stayers in the Blue Cross HMO have 2011 costs of $300.71 on average (SE $1.40). In contrast, switchers from other PPOs to Blue Cross HMO have average 2011 costs of $252.82 (SE $19.14), while switchers from Blue Cross HMO to another PPO have average costs of $340.90 (SE $7.08). Approximately the reverse pattern exists for Harvard Pilgrim PPO. In particular, the enrollees who switch away to HMOs have significantly lower 2011 costs than those who stay in the plan.
These switching patterns are consistent with older and sicker enrollees’ moving away from HMOs, which use alternative payment arrangements, to PPOs, which do not. (However, of course there are other important differences between HMOs and PPOs.) We next consider the overall magnitude of the selection effects across different insurers.
4.5 The Impact of Entry, Exit and Switching on Cost Growth
Table 6 assesses how much the 2011–2012 cost growth changes when we remove exiters and entrants and/or switchers. We note that the change in costs from year t to year \(t+1\) in a plan, \(C_{t+1}-C_{t}\), can be written as a combination of cost changes for stayers, a contribution of exiters out of \(C_{t}\), a contribution of entrants into \(C_{t+1}\) and a contribution of plan switchers.Footnote 13 The table reports the change in average per member per month costs, by plan, (1) for stayers only; (2) for stayers plus entrants and exiters; (3) for stayers plus switchers; and (4) for the full sample. The difference in cost growth between the full sample and stayers can be interpreted as a measure of how much switching, entry and exit affect a plan’s average costs. The difference between the full sample and \(\hbox {stayers} + \hbox {entrants}/\hbox {exiters}\) can be interpreted as a measure of how much plan switching affects costs.
We draw two conclusions from the table: First, as expected, cost increases in all plans are much greater for stayers than for the full sample, and most of the difference is accounted for by exiters and entrants. For example, costs per member per month for the full sample in Blue Cross HMO fell by $3.95 from 2011 to 2012, while the equivalent change for stayers was an increase of $15.86. Adding back entrants and exiters brings cost growth down to − $3.03, very close to the change for the full sample.
Second, a comparison of rows 1 and 3 of the table shows that differential switching helps explain the differences in cost growth across plans in the full sample. Row 3 includes the sample of plan switchers and the stayers sample, while row 1 contains just stayers. Removing switchers tends to increase cost growth for HMOs (e.g. an increase from $7.96 to $15.86 for Blue Cross HMO) while it reduces cost growth for PPOs (e.g. a reduction from $16.81 to $12.43 for Blue Cross PPO): this reduces the disparity in growth rates among types of plans. The increase in cost growth is larger for Blue Cross HMO and for Tufts HMO, the two plans with the greatest use of alternative payment arrangements in 2012, though Harvard Pilgrim HMO also has a sizeable increase.Footnote 14
4.6 Cost Decomposition for Stayers
The previous analyses indicate the importance of compositional changes (caused by entry, exit and plan switching) for cost growth. We now repeat the original cost decomposition for the sample of enrollees who stay with a plan from year to year (stayers).
The results of this cost decomposition for 2010–2012 are provided in Table 7. As before, the column labeled “Total $ Change” lists the average change in spending per member per month for the relevant sample across years; it corresponds to the “Stayers” row of Table 6. The results look quite different from Table 3. Cost growth from 2010 to 2012 is much higher in every plan for the sample of stayers than for the full sample: a difference that is driven largely by the high cost of exiters. For example, for Blue Cross HMO, the total cost change for the full sample (Table 3) is − $6.51; for stayers it is $29.20. There are sizable differences across insurers: the equivalent figures for Harvard Pilgrim’s PPO are $21.89 and $56.38.
The remaining columns of Table 7 decompose these changes into our three components, which sum to the numbers in the “Total $ Change” column. Nearly every component is larger (more positive) here than it was in the full sample. For all but one plan and year, there is an annual cost increase of $6–$10 per enrollee per month that is due to the aging of the population of stayers. A second source of cost increases is an increase in the proportion of stayers who are in higher-cost severity groups conditional on age and gender (term 2 of the cost decomposition). The magnitude of this component is quite comparable across insurers, generating a $15–$20 cost increase over the 2 years. There is no longer any evidence of upcoding in Blue Cross HMO: The shift in shares across severity groups given age and gender is now essentially the same for Blue Cross HMO as for its PPO. We infer that the difference between the HMO and the PPO plans in the full sample that was analyzed in Sect. 4.2 and Table 3 was caused by differential switching and entry or exit from the sample rather than upcoding.
The cost component of the decomposition—which in the full sample was negative for all plans except Harvard Pilgrim—is now positive for all plans when summed over 2010–2012. That is, costs—conditional on severity group and age—are increasing for stayers in every plan. The increases are smaller for HMOs than for PPOs. For example, for Blue Cross, the HMO cost component for 2010–2012 is $0.65, while that for the PPO is $2.03. For Harvard Pilgrim the equivalent figures are $10.32 and $19.52 for the HMO and PPO respectively. The HMO with the highest growth in the cost component ($10.32 between 2010 and 2012) is Harvard Pilgrim: the insurer with the latest and lowest-share application of global payments of all HMOs.
While all of these findings are consistent with the physician incentives that are generated by global payments having a negative impact on cost growth, we cannot draw causal conclusions because the group of stayers is a selected sample that endogenously chose to enroll in particular types of plans. Unobserved changes in health conditions of stayers in HMOs are likely to be different from those in PPOs, which implies many reasons why their cost changes should be different beyond the differences in physician incentives. Note also that, for Blue Cross, the difference between its HMO and PPO is much smaller than in the full sample.Footnote 15 This is consistent with the finding above that switching of higher-cost enrollees from HMOs to PPOs was one cause of the lower HMO cost growth in the full sample. Removing switchers brings HMO cost growth closer to that for PPOs.
5 Conclusion
This paper presents data on cost changes in the three largest commercial insurers in Massachusetts from 2010 to 2012: a period when all three HMO plans expanded global payment arrangements for their physicians. There are large differences in cost growth across insurers and plan types. To understand population cost changes over time, we need to consider changes for different sub-populations—entrants, exiters, plan switchers, and stayers—and how the separate sub-populations affect this growth. Our results indicate that accounting for exiters, entrants and switchers is essential to understanding cost growth and differential cost growth across plans.
We show that HMOs—which use global payments during the time period of study—have slower cost growth than PPOs, which do not. Some of the difference is accounted for by healthier enrollees’ switching into HMOs and sicker enrollees’ switching out of them. After removing plan switchers, entrants, and exiters from the sample, we see substantially higher cost growth for all plans. Growth in costs conditional on severity group, age, and gender is now positive in every case. But the finding of higher cost growth for PPOs than HMOs remains. Insurers whose HMOs use more global payments have lower cost growth than other insurers’ HMOs.
The endogenous selection of enrollees into the “stayer” population in HMOs means that we cannot make causal statements about the impact of global payments on costs. However, our results do raise the possibility that HMOs’ expansion of global payments was connected to their attracting healthier enrollees to switch to their plans. This would be an additional incentive—beyond any direct cost effect—to adopt global payments.
Our ability to draw strong conclusions is limited by the possibility of other confounding effects and limited data. It would be helpful to test whether switching patterns into and out of HMOs changed when global payments were introduced in 2009–2010, but we do not have reliable data on insurers before this period.
Further research is needed to study the introduction of global payments in the context of larger changes in market structures and integration between hospitals and physicians—all of which are likely to have affected costs. We are engaged in ongoing work towards this end to evaluate the relationship of physician incentives to changes in market structure, prices, and referrals.
Notes
As we describe in Sect. 2, we limit the sample to enrollees in the “big three” insurers—Blue Cross, Harvard Pilgrim, and Tufts—for data quality reasons. These three insurers cover more than three-fourths of commercial enrollees.
Alternative payments technically encompass a broader set of non-fee-for-service payment mechanisms, including limited budgets and bundled payments for episodes of care. However, in practice, global payments comprised 97% of alternative payment schemes in Massachusetts. We therefore use these terms interchangeably.
The stayer sample for 2011–2012 includes enrollees who enter in 2010.
Medical costs do not include prescription drug or dental costs, since not all plans cover these benefits. In cases where physicians are paid using alternative payment arrangements, our data contain the fee-for-service component of the payment rather than later reconciliations with respect to shared savings.
The ACG grouper software begins by aggregating individual patient ICD-9 codes into 32 Aggregate Diagnosis Groups (ADGs) based on duration and severity of the condition, diagnostic certainty, types of health care services likely to be used, and the degree to which specialty care is likely to be required. See the Johns Hopkins ACG Software System Technical Reference Guide, Version 10.0, December 2011. The software then uses a clearly defined algorithm to place individuals into 93 discrete ACG categories based on their assigned ADGs, age and gender. These categories are listed in the Appendix with their associated Resource Utilization Bands, which are assigned based on expected spending required for each category.
Seven provider organizations agreed to use these contracts in 2009, followed by four more in 2010. At the same time, Blue Cross also introduced comprehensive support for participating physician groups, including regular provision of data on the care provided to patients by providers (e.g. hospitals) outside of the group, and organized sessions where the groups met to discuss best practices. See Chernew et al. (2011) for additional details.
Note, however, that the decomposition is an identity and the cost component is the part that we can not explain by our severity and age/gender groupings. Consequently, any error in the construction of those two components will be transmitted, with opposite sign, to our cost component.
Under the alternative payment arrangements that are frequently used by HMO plans in the data, a target for overall spending is established for each physician group based on the severity level of the group’s patients. Savings relative to this target—and in many cases excesses above the target—are shared between the insurer and the physician group. This introduces an incentive for the physician group to control costs, and potentially also to “upcode”: if physicians list a larger number of diagnoses on the patient’s record, this will result in a larger number of diagnoses per patient and a resulting movement of patients to ACGs that are coded as higher severity level. In turn this generates an increase in the group’s target spending level.
The analyses of entry, exit and switching use a slightly different data sample from the cost decompositions in Tables 3 and 7. For example we simplify by dropping enrollees who switch plans more than once. For this reason the aggregate cost numbers in Tables 1, 3 and 7 differ slightly from those in Tables 4, 5 and 6.
This is partly offset by the high cost growth of exiters in their last 2 years in-sample.
For example, this is a much larger switching percentage than that recorded in Handel (2013).
That is, \(C_{t+1}-C_{t} = \sum _{r} (s_{r,t+1}C_{r,t+1} - s_{r,t}C_{r,t}) \) where \(C_{r,t}\) = Average monthly cost of plan j’s enrollment who are in group r and \(s_{r,t}\) is the share of plan j’s enrollment (in member-months) who are in group r. Note that \(s_{r,t+1}=0\) for exiters/switchers out of the plan (before the start of \(t+1\)), so they only contribute to \(C_{r,t}\). Similarly, entrants/switchers in only contribute to \(C_{r,t+1}\).
In the full sample, Blue Cross HMO experienced a cost reduction of $12.83, while the PPO had a cost reduction of $1.47.
References
Aizcorbe, A., & Nestoriak, N. (2011). Changing mix of medical care services: Stylized facts and implications for price indexes. Journal of Health Economics, 30(3), 568–574.
Breyer, F., Bundorf, M. K., & Pauly, M. (2011). Health care spending risk, health insurance, and payment to health plans. Handbook of Health Economics, 2, 691–762.
Bundorf, M. K., Royalty, A., & Baker, L. C. (2009). Health care cost growth among the privately insured. Health Affairs, 28(5), 1294–1304.
Center for Health Information and Analysis (CHIA). (2014). Massachusetts commercial medical care spending: Findings from the all-payer claims database. Available at http://www.mass.gov/anf/docs/hpc/apcd-almanac-chartbook.pdf. Accessed 3 January 2017.
Center for Health Information and Analysis (CHIA). (2015). Annual report on the performance of the Massachusetts health care system: Data book. Available at http://www.chiamass.gov/assets/2015-annual-report/2015-Annual-Report-Data-Books.zip. Accessed 3 January 2017.
Chernew, M. E., Mechanic, R., Landon, B. E., & Safran, D. (2011). Private-payer innovation in Massachusetts: The ‘alternative quality contract’. Health Affairs, 30(1), 51–61.
Cutler, D. M., McClellan, M., Newhouse, J. P., & Remler, D. (1998). Are medical prices declining? Evidence from heart attack treatments. Quarterly Journal of Economics, 113, 991–1024.
Cutler, D. M., McClellan, M., Newhouse, J. P., & Remler, D. (2001). Pricing heart attack treatments. In D. Cutler, E. Berndt (Eds.) Medical care output and productivity (pp. 305–362). Chicago: University of Chicago Press.
Dunn, A., Liebman, E., & Shapiro, A. H. (2017). Decomposing medical-care expenditure growth. NBER Working Paper 23117.
Handel, B. (2013). Adverse selection and inertia in health insurance markets: When nudging hurts. American Economic Review, 103(7), 2643–2682.
Herrera, C., Gaynor, M., Newman, D., Town, R. J., & Parente, S. T. (2013). Trends underlying employer-sponsored health insurance growth for Americans younger than age sixty-five. Health Affairs, 32(10), 1715–1722.
Johns Hopkins ACG Software System Technical Reference Guide, Version 10.0. (2011).
Office of Attorney General Martha Coakley. (2010). Examination of health care cost trends and cost drivers. Retrieved from http://www.mass.gov/ago/docs/healthcare/2010-hcctd.pdf. Accessed 3 January 2017.
Office of Attorney General Martha Coakley. (2011). Examination of health care cost trends and cost drivers. Retrieved from http://www.mass.gov/ago/docs/healthcare/2011-hcctd.pdf. Accessed 3 January 2017.
Office of Attorney General Martha Coakley. (2013). Examination of health care cost trends and cost drivers. Retrieved from http://www.mass.gov/ago/docs/healthcare/2013-hcctd.pdf. Accessed 3 January 2017.
Song, Z., Rose, S., Safran, D. G., Landon, B. E., Day, M. P., & Chernew, M. E. (2014). Changes in health care spending and quality 4 years into global payment. New England Journal of Medicine, 371(18), 1704–1714.
Song, Z., Safran, D. G., Landon, B. E., Landrum, M. B., He, Y., Mechanic, R. E., et al. (2012). The ‘alternative quality contract’, based on a global budget, lowered medical spending and improved quality. Health Affairs, 31(8), 1885–1894.
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors gratefully acknowledge funding support for this work through a grant from the Commonwealth Fund. We also acknowledge financial support from a pilot Grant under NIH Grant P01AG005842 via the National Bureau of Economic Research. Shepard gratefully acknowledges Ph.D. and post-doctoral funding support from the National Institute on Aging Grant No. T32-AG000186 (via the National Bureau of Economic Research).
Appendix
Appendix
See Table 8.
Rights and permissions
About this article
Cite this article
Ho, K., Pakes, A. & Shepard, M. The Evolution of Health Insurer Costs in Massachusetts, 2010–2012. Rev Ind Organ 53, 117–137 (2018). https://doi.org/10.1007/s11151-018-9623-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11151-018-9623-2