Abstract
The implementation of regulation in the health care sector is often motivated by assuring a minimum level of quality, but there is little understanding of the cost of this regulation. This paper explores the cost of regulation in the nursing home industry. Using panel data on the same nursing homes from 1999 to 2004, this paper examines how financial performance is impacted by regulations that increased the minimum number of nurses that provide direct care to residents. While nursing homes attempt to increase revenues and mitigate the cost of responding to more stringent regulation, various measures of profitability show nursing homes are worse off financially. In fact, more stringent staffing regulations cause some nursing homes to lose money providing services.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
In many instances the consumer is less informed than the firm selling a product. If the asymmetry in the information between the consumer and firm is great enough, the firm can use this informational advantage to exploit the consumer, often by lowering unobservable dimensions of quality. Mechanisms such as guarantees or warranties exist to protect consumers, but in the health care sector warranties and guarantees are not feasible because an ineffective product could result in permanent injury or death. This leaves regulation as the usual mechanism employed to assure quality in the health care sector. While regulation attempts to assure quality, it also can increase the cost of producing care.
In the nursing home (NH) industry, a regulatory mechanism implemented to assure quality is the minimum direct care staffing (MDCS) regulation. Direct care is provided by nurses and empirical evidence suggests that higher nurse staffing levels could lead to higher quality of care (Konetzka et al. 2008; Lin 2014). MDCS regulations are a form of input regulation that dictates the minimum levels of nurse staff a NH must employ per resident, hopefully ensuring a minimum level of quality. More stringent MDCS regulations are found to increase nurse staffing levels (Mueller et al. 2006; Kim et al. 2009; Park and Stearns 2009; Bowblis 2011a), decrease non-nurse staffing levels (Thomas et al. 2010; Bowblis and Hyer 2013), and impact the quality of care provided at NHs (Park and Stearns 2009; Bowblis 2011a; Grabowski et al. 2011; Tong 2011).
Nurses are the largest cost of providing care, so any regulation that increases the number of nurses also affects costs. While numerous studies examine the impact of more stringent MDCS regulations on staffing and quality, NH financial performance has not been examined. A few studies examine characteristics associated with better financial performance, such as quality of care (Weech-Maldonado et al. 2003), ownership (Weech-Maldonado et al. 2012), racial composition (Chisholm et al. 2013), and private equity ownership (Cadigan et al. 2014), but to my knowledge, none have examined how NH financial performance is impacted by more stringent regulations.
This paper is the first to examine if NH financial performance is impacted by more stringent MDCS regulations. Moreover, this paper makes a broader impact on economics by increasing our understanding of how more stringent regulation can affect financial performance in health care industries. In addition, much of the NH literature on financial performance uses cross-sectional statistical techniques, which can lead to biased results if there are unobserved differences across NHs that are correlated with financial performance. This paper uses Medicare Cost Reports from 1999 through 2004 to construct a panel of NHs that can account for this unobserved heterogeneity.
The next section of the paper provides a background on NH staffing and presents a conceptual model of staffing regulation. Section 3 outlines the data used and the empirical strategy. Section 4 presents the results while the last section concludes.
2 A conceptual model of nursing home staffing regulation
Nursing homes generally employ two types of nurse staff. The first type is a licensed nurse, which includes licensed practical nurses (LPNs) and registered nurses (RNs). Licensed nurses are of high skill, high cost, and require training and education at vocational schools or traditional universities. While licensed nurses provide direct care to residents, they also have administrative duties. The second type of nurse staff is certified nurse aides (CNAs). CNAs are only required to have 80 h of training, are paid wages slightly above minimum wage, and provide most of the direct care to residents.
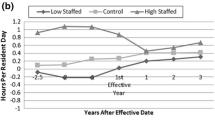
In order to ensure quality, states have regulations on the minimum number of licensed nurses (i.e. licensed nurse regulations) and all nurses providing direct care to residents (i.e. MDCS regulations). Licensed nurse regulations dictate that at least one or more licensed nurses be on duty at specific times during the day. In contrast, MDCS regulations dictate the minimum number of hours per resident a nurse must be available to provide direct care. Therefore, more nurses with direct care responsibilities are required as the number of residents in a NH increase. Between 1999 and 2004, 14 states enacted or strengthened their MDCS regulations (Bowblis 2011a), and these MDCS regulations are the focus of this paper.
Whenever states implement more stringent staffing regulations, NHs that are subject to the constraint must pay for the cost of hiring additional nurses and this will negatively impact financial performance. In order to keep financial performance at similar levels of profitability without changing the type of residents served, NHs can respond by decreasing costs or increasing revenues. However, the ability to reduce costs or increase revenues are constrained by the regulatory and economic structure of the industry.
There are multiple ways to decrease costs in response to more stringent regulation. One way is to change the composition of nurse staffing. Licensed nurses are paid higher wages than CNAs, and NHs are known to use a greater proportion of CNAs when MDCS regulations become more stringent (Park and Stearns 2009; Bowblis 2011a). This change in composition could be due to only hiring CNAs, and in some cases may include a direct substitution of licensed staff with CNAs. The ability to engage in this substitution is constrained by licensed nurse regulations. In some cases this substitution cannot occur because many NHs are already bound by licensed nurse regulatory constraints.
A second way to reduce costs is for NHs to reduce the use of non-nurse staff (Thomas et al. 2010; Bowblis and Hyer 2013). However, non-nurse workers are often in occupations that have lower wage rates than nurses, such as housekeepers and food service staff, limiting savings that may occur by using fewer non-nurse staffing inputs. Further, a profit maximizing NH may already have non-nurse staffing levels at efficient levels and any cuts to non-nurse staff may result in increased regulatory scrutiny or penalties. For example, inadequate non-nurse staffing to provide proper food service and sanitation may result in a monetary fine during a NH’s annual state regulatory review. Given these binding constraints, NHs are limited in how they can reduce costs, though some cost cutting may be possible.
As costs are increased, NHs can only maintain the same level of income and profitability by seeking additional revenues, which is difficult. NHs receive revenues from the Medicare and Medicaid programs, as well as private pay residents. In the case of Medicare and Medicaid, reimbursement rates are set by the government. For Medicare, reimbursement rates are set nationally and do not vary with more stringent MDCS regulations. State Medicaid programs will attempt to offset the financial cost of more stringent MDCS regulations by increasing reimbursement rates (Tilly et al. 2003), but industry trade associations argue that Medicaid reimburses at rates below the cost of care (Eljay 2011). Therefore, any increase in reimbursement is not likely to cover the full cost of care for Medicaid residents, let alone all residents.
This leaves private pay patients as the last revenue source. Private pay residents are individuals that pay for care out of their own pocket or through long-term care insurance plans. While NHs may attempt to increase private pay prices in response to more stringent regulation, there is little reason to believe that prices can be increased to offset the entire cost of hiring additional nurse staff. First, all NHs are expected to increase staffing levels and the relative competitive advantage of any given NH is likely to remain unchanged. Second, the market is relatively competitive and there are a limited number of private pay residents. This reduces the ability of NHs to increase private pay prices. Third, any increases would need to cover the costs of providing care to all residents. Private pay residents only account for 24 % of resident days in the data used in this study. Finally, higher prices make these residents deplete their assets faster and residents will then need to be converted to Medicaid.
It is expected that more stringent MDCS regulations should result in NHs seeking additional revenues. These higher revenues are not expected to be able to offset the entire costs of hiring additional nurse staff, resulting in lower profits. Furthermore, the effect is likely to vary with facility payer-mix. Medicaid attempts to offset some of the cost of MDCS regulations by increasing Medicaid reimbursement rates while Medicare and private pay rates are more constrained. Therefore, NHs that have a greater reliance on Medicare and private pay residents (i.e. low Medicaid dependence) are likely to see a larger negative impact to profits. It should be noted that some NHs may have staffing levels that satisfy more stringent MDCS regulations even before the regulations are enacted. These NHs are not required to change staffing levels and henceforth, mitigate the average financial impact on the NH industry.
3 Methods
3.1 Data
Two primary data sources on NHs are used in this study. The first source is the Medicare Cost Reports (MCRs) for free-standing NHs. MCRs are submitted annually by all Medicare-certified facilities and contain itemized financial and utilization information at the facility level. MCRs from the lower 48 states with at least 360 days in the reporting period from fiscal years 1999 through 2004 are utilized. This is a period when multiple states enacted a number of changes in MDCS regulations. The MCRs are merged with a second data source, the Online Survey, Certification, and Reporting (OSCAR) system, using a common provider identification number. OSCAR surveys are conducted by state inspection teams on an annual basis, and include information regarding the facility structure, resident case-mix, and staffing resources. OSCAR surveys within the fiscal year of the MCR are utilized. If an OSCAR survey is not conducted in the fiscal year, the closest OSCAR survey within 60 days of the fiscal year is utilized. The merged data results in a panel with a unit of observation of a NH-fiscal year.
Three state-level regulatory variables are also merged into the data. The key variable of interest is the MDCS regulation in the state. This variable reflects the minimum number of hours per resident day (HPRD) of direct care nurses required under state law. The second set of regulatory variables identify each time a state changed a licensed nurse regulation. Data on both type of regulations are obtained from Bowblis (2011a). Because states may change staffing requirements midyear, the requirement effective at the end of the fiscal year of each observation is utilized. Third, to capture the fact that some states increased Medicaid reimbursement to offset some of the additional cost of staffing requirements (Tilly et al. 2003), average Medicaid reimbursement rates in each state are obtained from Grabowski et al. (2004a, b, 2008).
3.2 Dependent variables
The dependent variables are measures of financial performance for revenues and profits constructed from Worksheet G-3 of the MCRs. The financial performance measures utilized include patient revenues, patient costs, patient profits, patient profit margin, and total operating profit margin. In the case of patient profit margins, an indicator for negative profit margins is also used as a dependent variable.
Patient revenue is the total money collected by the NH for general inpatient routine care services net of any contractual allowances or discounts (Line 3). Patient profits is the net income from service to patients (Line 5) after operating expenses are deducted from patient revenues. Patient costs is calculated as the difference between patient revenues and patient profits. To standardize these three measures across NHs of varying sizes, each measure is divided by the number of certified beds reported in the MCRs.
Profit margins are percentages that reflect the profitability of each NH. Patient profit margins capture the profitability of providing care to patients and are constructed from patient revenues and income. Total operating profit margins measure the profitability of the entire operation (including non-patient care). For this study, total operating profit margins are calculated excluding any income from donations and investments. Examples of items included in operating profits, but not patient profits are television/telephone services, laundry and linen services, meals and medical items sold to persons other than patients, vending machines, and gift/flower/coffee shops. Total operating margin is defined as total net income (Line 32) minus any income from donations (Line 7) and investments (Line 8) divided by total revenues (patient revenues plus all non-donation and non-investment income).
While the MCRs are subject to audit, the data is known to have outliers. Some of the past literature has handled this issue by examining dichotomous variables (Bowblis 2011b; Cadigan et al. 2014), but in this study the purpose is to examine the actual financial performance associated with MDCS regulations. To address outliers, the analysis uses MCRs that have positive patient revenues, which excludes 288 observations. Among the remaining observations, outliers are handled by winsoring the data to exclude observations from the extreme 1 % right and left tails of the distribution. To keep the observations consistent across all regressions, winsoring is based off the patient profit margin variable. Winsoring based on other dependent variables did not significantly change the results. The resulting analytical sample consists of 63,012 nursing home-fiscal year observations for 13,318 unique NHs.
3.3 Empirical specification
To determine how MDCS regulations impact the financial performance of NHs, a few concerns need to be addressed in the regression model. First, MDCS regulations may be changed in states where NHs are more profitable. Using data from 1999, states that changed regulations over the study period are found to have profit levels and profit margins statistically indistinguishable from states that did not change regulations. To err on the side of caution, MDCS regulations are included in the model with a time lag though results are also presented using contemporaneous measures. Second, the impact of increasing MDCS regulations on financial performance is likely to be a function of the physical structure and other time-invariant characteristics of the NH. While some of these factors are observable, many are not. Therefore, the model needs to account for NH specific heterogeneity that can be correlated with other variables. And finally, changes in regulations affect all NHs within the state, creating a correlation in the error term within the state. To account for this, standard errors are clustered at the state level. This results in the following fixed effect linear panel regression model:
where \(\textit{FP}_{ist} \) is a measure of financial performance for nursing home \(i\) located in state \(s\) during fiscal year \(t\), \(\textit{MDCS}_{st-1} \) is the MDCS regulation in HPRD effective the prior fiscal year, \(R_{st} \) reflects other state regulatory variables, \(X_{ist} \) is a set of time-varying NH control variables, \(\delta _i \) is NH specific heterogeneity treated as a fixed effect, and \(\varepsilon _{ist} \) is an error term.
The above model specification assumes that the financial impact of more stringent MDCS regulations are the same for all NHs. As noted earlier, NHs that are less reliant on Medicaid are more likely to see larger negative impacts on profits. To test this hypothesis, Eq. (1) is appended to include an interaction term between the MDCS regulation variable and an indicator signifying low reliance on Medicaid. Low reliance on Medicaid is defined as being in the lowest 25th percentile of percentage of residents on Medicaid during the study period, and observations that meet this criteria are identified with the indicator variable \(\textit{LMCAID}_{ist} .\) The resulting empirical specifications becomes:
where the coefficient \(\pi \) captures the average difference in financial performance for NHs that have low reliance on Medicaid, and the coefficients \(\alpha \) and \(\theta \) capture the effects of the regulations. In particular, \(\alpha \) reports the effect of regulation for the baseline group (more reliant on Medicaid) while \(\alpha +\theta \) reports the effect of regulation for the group with low reliance on Medicaid. The coefficient \(\theta \) determines if the effect is different for the two groups.
3.4 Control variables
The summary statistics for select time-varying regulatory variables and NH control variables that may impact financial performance are reported in Panel B of Table 1. The first set of these variables include other state regulatory policies, including Medicaid reimbursement rates and indicators of licensed nurse regulation changes. Higher Medicaid reimbursement rates should result in higher revenues and potentially higher profitability if the rates are above the cost of care. The average Medicaid reimbursement rate during the study is $116.32 per resident day. Additionally, some states also changed their licensed nurse regulations during the study period. These changes could impact financial performance and are captured by including a set of indicators that identify whether the state is in a period after a licensed nurse staff regulation was changed. There are a total of five indicator variables that reflect licensed staff changes in four states (Arkansas, Delaware—twice, Florida, and Ohio). Similar to the MDCS regulations, these licensed nurse regulation changes are measured with a one period lag.
The second set of controls account for the structure and type of residents in the NH. NH structure includes measures of ownership (i.e. for-profit, not-for-profit, government) and if the NH is part of a chain. These variables capture differences in NH motivation for profit as well as managerial and physical structure that may influence efficiency. The majority of NHs observed are for-profit (73.4 %) and part of a chain (60.9 %). Payer-mix and occupancy rates are also included. Each revenue source has difference reimbursement and cost per day, while higher occupancy rates spread fixed costs over more residents. The average NH is 87.6 % occupied with the majority (64.8 %) of residents having the cost of services paid for by Medicaid. Finally, NHs that have residents with greater physical and mental needs are likely to have higher costs. To capture differences in the needs of these residents, case-mix of the NH is measured using a physical acuity index (Cowles 2002) and measures of the percentage of residents with various mental conditions.
Nurse staffing levels should be highly correlated with the MDCS regulation variable and therefore are excluded the regressions. However as a robustness check, regressions are performed that included the level of nurse staffing in the NH during that fiscal year. These regressions are robust to those reported in the next section.
4 Results
Table 1 (Panel A) reports the summary statistics for the measures of financial performance. The average amount of patient revenue per bed is $48,589 with an average patient cost per bed equaling $49,813. Since costs are higher than revenues, the patient profit per bed is negative (\(-\)$1,224). This is expected during this period because the Prospective Payment System was introduced and phased-in from 1998 to 2002 for Medicare patients receiving care in NHs. This reimbursement system significantly reduced Medicare reimbursement rates and as a result, a number of the large for-profit chains declared bankruptcy (Dummit 2000). These financial losses are reflected in patient profit margins. The average patient profit margin is \(-\)2.77 %, with 56.3 % of NHs having negative patient profit margins. When all operating revenues and expenses are included, the average NH experienced a negative operating profit margin of \(-\)0.59 %.
As outlined in the conceptual framework, it is expected that NHs will attempt to increase revenues, but will be unable to offset the higher costs of the regulation, resulting in lower profits after an increase in MDCS regulations. Table 2 reports the results of estimating Eq. (1) for the financial performance measures of patient revenue per bed (Panel A), patient cost per bed (Panel B), patient profit per bed (Panel C), patient profit margin (Panel D), if the NH has a negative patient profit margins (Panel E), and total operating profit margin (Panel E). In the first column, the regression controls for regulatory variables, year indicators, and NH fixed effects. The second column contains all controls in Column (1), but also controls for time-varying NH control variables (i.e., ownership, chain, payer-mix, occupancy rates, and case-mix). The final column has all the same controls as Column (2), but uses the contemporaneous MDCS regulation in HPRD instead of a one period lag. These model specifications are identified at the bottom of the table.
For all dependent variables, the inclusion of time-varying NH control variables does not significantly change the effect sizes of the MDCS regulation variable. Furthermore, regressions that use a contemporaneous measure of the MDCS regulation find effects in a similar direction and statistical significance as using a one period lag. Because the results are robust across specifications, the discussion of the results will focus on the specification that includes NH control variables (Column 2).
The effect of a one HPRD increase in the MDCS regulations is found to be associated with increases in the amount of patient revenue per bed (Panel A) and the patient cost per bed (Panel B), though the effects are not statistically significant. In contrast, a similar increase in the MDCS regulation reduces patient profits per bed by $611. This implies that while patient revenues or patient costs do not significantly change, the average NH is made worse off in terms of lower patient profits per bed. This loss in profits is also evident when examining profit margins. Patient profit margins are found to decrease by 1.3 percentage points for every one HPRD increase in the MDCS regulation (Panel D). This forces an additional 4.6 % of NHs to go from having a positive to a negative patient profit margins (Panel E). Finally, the effect of more stringent regulation impacts overall profitability as total operating profit margins are also found to decrease (Panel F).
As a placebo test, staffing regulations were entered as leads of the MDCS regulations (i.e., \(MDCS_{st+1} \) or \(MDCS_{st+2} )\). These use of these alternative specifications found that MDCS regulations do not impact profitability. For example, the effect of a one HPRD increase in the MDCS regulation reduced patient profit per bed by $123, patient profit margins by \(-\)0.3 %, and operating profit margin is 0.1 % when using a one year lead. None of these results are statistically significant at conventional levels and suggest that empirical strategy passes standard placebo tests.
To test if the effect of MDCS regulations vary with exposure to Medicaid, the results for Eq. (2) are reported in Table 3. The first row of the Table reports how the dependent variable changes in response to a one HPRD increase in the MDCS regulation for all NHs (\(\alpha \) in Eq. 2). The second row reports the additional effect of this change for low Medicaid dependent NHs (\(\theta )\). Therefore, the first row reports the effect for highly Medicaid dependent NHs and the sum of the coefficient estimates of the first and second rows are the effect for low Medicaid dependent NHs. Finally, the third row reports the average difference in the dependent variable for low and high Medicaid dependent NHs (\(\pi )\).
Patient revenues per bed are not found to be statistically impacted by MDCS regulations, consistent with NHs not being able to increase Medicare reimbursement rates or private pay prices. Patient costs per bed are found to vary with Medicaid dependence. A low Medicaid dependent NH has $1,867 higher patient costs per bed for a one HPRD increase in the MDCS regulation compared to $1,035 for a high Medicaid dependence NH. These costs directly translate into lower profits, with low Medicaid dependent NHs having lower patient profits per bed of $796 compared to $569 for high Medicaid dependent NHs. This differentiated effect by Medicaid dependence is also found in terms of worse patient profit margins (\(-\)1.4 vs. \(-\)1.2 % for low versus high dependence), more NHs experiencing negative profit margins (5.5 vs. 4.4 percentage points), and worse total operating profit margins (\(-\)1.8 vs. \(-\)1.5 %).
5 Conclusion
While regulators are often interested in assuring the quality of an output, if quality is multi-dimensional or difficult to verify a mechanism that is often utilized is to regulate an input that is easier to verify, and is believed to have a relationship to output quality. In the NH industry, regulators are concerned with output quality, but given the complexity of patients’ needs and the multiple dimensions on which quality may be measured, a common method employed is to use minimum staffing regulations. These regulations are found to increase staffing levels and improve the quality of care provided to NH residents in a number of dimensions. Given the focus of policymakers and NH advocates on quality, MDCS regulations have been implemented without fully exploring the financial impacts. These regulations increase costs by forcing many NHs to hire additional nurses, and may lower quality in other dimensions, such as quality of life. For example, NHs substitute higher skilled nurses, such as RNs and LPNs, for lower skilled and less costly CNAs (Park and Stearns 2009; Bowblis 2011a), or NHs reduce staffing in areas not specifically related to nurse staffing, such as support staff (Thomas et al. 2010; Bowblis and Hyer 2013).
The cost of more stringent MDCS regulations depends on a number of factors, but most importantly the type of nurses hired and the total compensation package paid to those nurses. The Bureau of Labor Statistics reports for 2013 that median wage rate in NHs for CNAs are $11.54 and for RNs are $28.82. This implies that without reducing non-nurse staffing levels and ignoring non-wage compensation, a one HPRD increase in a MDCS regulation today would increase the annual cost of care per resident by $4,212 to $10,519 for a fully occupied NH. While it is expected NHs would attempt to increase patient revenues and decrease other costs in response to more stringent MDCS regulations, the changes in revenues and costs found in this study are in the predicted direction, though both results are not statistically significant. A naïve conclusion would be that regulation had no impact. However, profits per bed and profit margins are found to be lower, suggesting any potential increases in costs are not offset by increases in revenues. Furthermore, given the low levels of profitability in the industry, more stringent regulations moved more NHs into negative profitability.
Regulators and advocates for higher staffing standards need to consider the financial strength of the industry, and merely looking at costs does not fully illustrate the impact of regulation. Regulators need to consider a range of performance measures. In the short run, financial performance can have negative impacts on health care outcomes (Weech-Maldonado et al. 2003; Ly et al. 2011). In the longer run, NHs that cannot make a profit under more stringent regulations only have a few options. One is to change the mix of residents towards more profitable payers, such as Medicare. Another option is to close, something seen commonly after Medicare cut reimbursement rates as part of the implementation of the Prospective Payment System (Bowblis 2011b). Both of these options hurt access to care. It is also possible that more stringent regulations provide motivation for NHs to engage in activities that increase revenues from existing payment sources. For example, NHs could focus on admitting patients that have case-mixes that are more profitable (i.e., cream-skimming) or could engage in activities such as upcoding, a practice in which patients are provided additional services or are coded as sicker in order to increase revenues (Bowblis and Brunt 2014).
These results suggest the need to question the role of direct input regulation when output quality is the regulator’s targeted goal. Input regulation directly impacts firm costs, profitability, and as shown by other studies, the mix of inputs used by firm. Yet input regulation may have a questionable impact on measures of output quality. While some measures of quality may improve, other dimensions of quality may deteriorate or the firm may engage in behavior that decreases welfare. Though the setup of this paper cannot determine if input regulation is optimal compared to direct output regulation in the NH industry, more stringent regulation can impact the profitability of NHs, potentially leading to unintended consequences. This requires regulators to weigh the benefits and costs of mandating higher staffing levels.
References
Bowblis, J. R. (2011a). Staffing ratios and quality: An analysis of minimum direct care staffing requirements for nursing homes. Health Services Research, 46(5), 1495–1516.
Bowblis, J. R. (2011b). Ownership conversion and closure in the nursing home industry. Health Economics, 20(6), 631–644.
Bowblis, J. R., & Brunt, C. S. (2014). Medicare skilled nursing facility reimbursement and upcoding. Health Economics, 23(7), 821–840.
Bowblis, J. R., & Hyer, K. (2013). Nursing home staffing requirements and input substitution: Effects on housekeeping, food service and activities staff. Health Services Research, 48(4), 1539–1550.
Cadigan, R. O., Stevenson, D. G., Caudry, D. J., & Grabowski, D. C. (2014). Private investment purchase and nursing home financial health. Health Services Research, 50, 180–196.
Chisholm, L., Weech-Maldonado, R., Laberge, A., Lin, F.-C., & Hyer, K. (2013). Nursing home quality and financial performance: Does the racial composition of residents matter? Health Services Research, 48(6 part 1), 2060–2080.
Cowles, C. M. (2002). Nursing home statistical yearbook. Montgomery Village, MD: Cowles Research Group.
Dummit, L. A. (2000). Nursing homes: Aggregate medicare payments are adequate despite bankruptcies. Washington, DC: GAO.
Eljay, L. L. C. (2011). A report on shortfalls in medicaid funding for nursing home care. Washington, DC: American Health Care Association.
Grabowski, D. C., Angelelli, J. J., & Mor, V. (2004a). Medicaid payment and risk-adjusted nursing home quality. Health Affairs, 23(5), 243–252.
Grabowski, D. C., Feng, Z., Intrator, O., & Mor, V. (2004b). Recent trends in state nursing home payment policies. Health Affairs, W4, 363–373.
Grabowski, D. C., Feng, Z., Intrator, O., & Mor, V. (2008). Medicaid nursing home payment and the role of provider taxes. Medical Care Research and Review, 65(40), 514–527.
Grabowski, D. C., Bowblis, J. R., Lucas, J. A., & Crystal, S. (2011). Labor prices and the treatment of nursing home residents with dementia. International Journal of the Economics of Business, 18(2), 273–292.
Kim, H., Harrington, C., & Greene, W. H. (2009). Registered nurse staffing mix and quality of care in nursing homes: A longitudinal analysis. The Gerontologist, 49(1), 81–90.
Konetzka, R. T., Stearns, S. C., & Park, J. (2008). The staffing-outcome relationship in nursing homes. Health Services Research, 43(3), 1025–1042.
Lin, H. (2014). Revisiting the relationship between nurse staffing and quality in nursing homes: An instrumental variables approach. Journal of Health Economics, 37, 13–24.
Ly, D. P., Jha, A. K., & Epstein, A. M. (2011). The association between hospital Margins, quality of care, and closure or other changes in operating status. Journal of General Internal Medicine, 25(11), 1291–1296.
Mueller, C., Arling, G., Kane, R., Bershadsky, J., Holland, D., & Joy, A. (2006). Nursing home staffing standards: Their relationship to nurse staffing levels. The Gerontologist, 46(1), 74–80.
Park, J., & Stearns, S. C. (2009). Effects of state minimum staffing standards on nursing home staffing and quality of care. Health Services Research, 44(1), 56–78.
Thomas, K. S., Hyer, K., Andel, R., & Weech-Maldonado, R. (2010). The unintended consequences of staffing mandates in Florida nursing homes: Impacts on indirect-care staff. Medical Care Research and Review, 67(5), 555–573.
Tilly, J., Black, K., Ormond, B., & Harvell, J. (2003). States experiences with minimum nursing staff ratios for nursing facilities: Findings from case studies in eight states. Washington, DC: U.S. Department of Health and Human Services.
Tong, P. K. (2011). The effects of California minimum nurse staffing laws on nurse labor and patient mortality in skilled nursing facilities. Health Economics, 20(7), 802–816.
Weech-Maldonado, R., Neff, G., & Mor, V. (2003). The relationship between quality of care and financial performance in nursing homes. Journal of Health Care Finance, 29(3), 48–60.
Weech-Maldonado, R., Leberge, A., Pradhan, R., Johnson, C. E., Yang, Z., & Hyer, K. (2012). Nursing home financial performance: The role of ownership and chain affiliation. Health Care Management Review, 37(3), 235–245.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bowblis, J.R. The cost of regulation: More stringent staff regulations and nursing home financial performance. J Regul Econ 47, 325–338 (2015). https://doi.org/10.1007/s11149-015-9269-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11149-015-9269-z