Abstract
Purpose
To summarize the current evidence regarding the effectiveness of intradialytic exercise (IDE) on the health-related quality of life (HRQOL) of patients undergoing maintenance haemodialysis.
Methods
Five English databases (PubMed, EMBASE, Cochrane Library, Web of Science, and ScienceDirect) and four Chinese databases (VIP, WAN FANG, CNKI, CBM) were comprehensively searched from their inception to 18 March 2021. This study was reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement. Two independent reviewers selected the papers and extracted the details of each study therein. Only randomized controlled trials were included. The risk of bias tool version 2.0 was used to evaluate the risk of bias of the included studies. A random-effects meta-analysis was conducted to pool the effect size.
Results
Thirty-three eligible studies with 1481 participants were included. For the generic HRQOL, assessed by the Medical Outcomes Study Short-Form survey, IDE significantly improved most domains and the physical component summary compared with the control group. Furthermore, aerobic exercise alone significantly improved more domains compared to resistance exercise, combined aerobic and resistance exercise, and other types of exercise. Regarding the kidney-specific HRQOL, IDE improved three of eleven domains, including the symptom/problem list, the effect of kidney disease, and the quality of social interaction. No significant effect was found on other domains of kidney-specific HRQOL.
Conclusion
Intradialytic exercise could benefit patients undergoing haemodialysis in improving most domains of generic HRQOL, but the effect on most domains of kidney-specific HRQOL is insufficient.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Plain English summary
The number of end-stage renal disease patients who need maintenance haemodialysis has risen significantly in recent years. The health-related quality of life is lower in this population. Many types of exercise during dialysis sessions may improve the health-related quality of life in patients undergoing haemodialysis. However, the effect of different types of exercise on domain-level of health-related quality of life lacks, especially on kidney disease-related domains. In this study, we have explored the impact of different kinds of exercise during dialysis on the detail of the health-related quality of life via the synthesis of high-quality clinical trials. This study indicated that aerobic exercise alone improved more part of health-related quality of life compared to resistance exercise, combined aerobic and resistance exercise, and other types of exercise. Exercise during dialysis could benefit patients undergoing haemodialysis in improving most generic health-related quality of life. Still, the effect on most aspects of kidney-specific health-related quality of life is insufficient.
Introduction
Maintenance haemodialysis (MHD) is the predominant form of renal replacement therapy (RRT) for end-stage renal disease (ESRD) patients [1]. The prevalence of ESRD has risen significantly in recent years [2]. It is estimated that the number of ERSD patients who need RRT will increase from 2.618 million in 2010 to 5.439 million in 2030 globally and that the most growth will occur in Asia [2]. In China alone, 553,000 patients underwent MHD in 2015 [3].
While improvements in the treatment of ESRD patients have prolonged their life expectancy, the burden of MHD remains substantial. MHD requires patients to commit to at least two to four-hour treatment sessions three times weekly, leading to challenges for patients in terms of scheduling, travel flexibility, and the possibility of holding certain jobs that do not allow for breaks during the day [4]. Furthermore, patients undergoing MHD suffer from a series of symptom clusters (e.g., dry skin, muscle soreness, dry mouth, etc.) and economic burdens, leading to more inferior health-related quality of life (HRQOL) compared with their healthy counterparts [4, 5].
Physical exercise, including intradialytic exercise (IDE) and out-of-clinical exercise, for MHD patients may improve physical activity and HRQOL [6]. IDE has been considered the ideal method of physical exercise for MHD patients since it is performed under the supervision of healthcare staff and is safer precisely because of the monitoring from medical professionals [6].
According to the World Health Organization, quality of life (QOL) is subjective and multi-dimensional, including in relation to physical, psychological, social relationships, level of independence, and spirituality [7]. HRQOL refers to the aspects of QOL that are affected by health [8]. Although there is no uniform definition of HRQOL, it is widely accepted as including physical, psychological, and social domains [9, 10]. Patient-reported outcomes, usually in the form of questionnaire responses, are commonly used to measure HRQOL [7, 10, 11]. Generic and disease-specific HRQOL measurements are widely used to measure HRQOL among patients with ESRD [9]. Specifically, the most common assessment tools for generic and disease-specific HRQOL for ERSD patients are the Medical Outcomes Study Short-Form (SF-36) survey and the Kidney Disease Quality of Life (KDQOL) questionnaire, respectively [9]. The Kidney Disease Quality of Life Short-Form (KDQOL-SF) includes the generic (SF-36) and eleven kidney-specific domains of HRQOL (e.g., the symptom/problems list (SPL), the effect of kidney disease (EKD), the burden of kidney disease (BKD), etc.), which could comprehensively reflect the HRQOL of MHD patients [11]. A shorter version of the KDQOL-SF, the Kidney Disease Quality of Life-36 (KDQOL-36), also includes generic and kidney-specific aspects of HRQOL [12].
The HRQOL of patients undergoing MHD is significantly lower than that of the general population in the physical component summary (PCS), the mental component summary (MCS) and eight domains assessed using the SF-36 [5]. Impaired HRQOL in patients undergoing MHD was associated with adverse outcomes, such as higher rates of mortality and hospitalization [13]. With every 10-point decline in different components of HRQOL, the adjusted relative risk of mortality increased by 1.13 times for the MCS, 1.25 times for the PCS, and 1.11 times for the kidney disease component summary [13].
IDE may benefit physical functioning and improve the HRQOL of MHD patients [6, 14]. It includes aerobic exercise, resistance exercise, combined aerobic and resistance exercise, and other types of exercise [6]. Published studies have shown that IDE can improve dialysis efficiency, aerobic capacity (VO2peak), physical capacity, muscle strength, and HRQOL in this population [15,16,17,18].
Evidence about the effects of different types of IDE on the HRQOL domains remains wanting, especially for kidney-specific HRQOL. For HRQOL in MHD patients, domain-level analyses have been found to be more sensitive and specific than component-level analyses, given that changes in some component summaries of HRQOL did not translate into changes in the corresponding domains [11, 19]. Although most published clinical trials reported on the effectiveness of IDE on HRQOL in both the domain and component levels for MHD patients, most meta-analyses have focused on the PCS and MCS [20,21,22,23,24]. To date, only one meta-analysis has reported on the effectiveness of combined aerobic and resistance exercise on eight generic domains of HRQOL (measured by SF-36), with the results showing that combined aerobic and resistance exercise could significantly improve physical functioning (PF) and vitality (VT) [25]. Therefore, the effectiveness of IDE on the domain level of generic HRQOL needs to be explored.
Furthermore, the results of the existing systematic review on the effectiveness of IDE on the HRQOL of MHD patients are inconsistent [20, 22]. Some published meta-analyses indicated that IDE could improve the PCS or MCS [21,22,23]. However, other meta-analysis results demonstrated that the effect of IDE on the PCS and MCS of the same population was unobvious [20, 24]. Different results on the effectiveness of IDE on HRQOL will create confusion among healthcare providers and patients in terms of reliability. In addition, it has been reported that most KDQOL domains (e.g., SPL, EKD, BKD, etc.) are independently and significantly associated with death and hospitalization [13]. To the best of our knowledge, no published meta-analysis has explored the effectiveness of IDE on kidney-specific HRQOL. Moreover, the published meta-analysis pooled different types of IDE together, and no one could distinguish which modality of IDE is more efficacious [22, 23]. Therefore, this systematic review is necessary as it explores the effects of different types of IDE on the domain-level HRQOL of MHD patients.
To update the evidence about the effectiveness of IDE on HRQOL and supplement previous meta-analyses, the current meta-analysis aimed to synthesize all the eligible randomized controlled trials (RCTs) and systematically analyse the effects of IDE on generic and kidney-specific HRQOL, with specific objectives to assess the effectiveness of different types of IDE on specific domains and component summaries of HRQOL.
Materials and methods
This systematic review and meta-analysis was conducted following the Cochrane Handbook for Systematic Reviews of Interventions [26] and reported according to the principles of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [27]. The protocol of this study was registered on the PROSPERO website (ID: CRD42020219799).
Search strategy and data selection
Five English electronic databases (PubMed, EMBASE, Cochrane Library, Web of Science, and Science Direct) and four Chinese electronic databases (CNKI: China National Knowledge Infrastructure; CBM: Chinese BioMedical Literature Database; WAN FANG: WAN FANG Data; and VIP: VIP Chinese Science and Technology Journal Database) were searched from their inception to 18 March 2021. Keywords and their synonyms were used with a combination of Boolean notations. The keywords included ‘chronic kidney disease’, ‘end-stage renal disease’, ‘hemodialysis’, ‘haemodialysis’, ‘dialysis’, ‘exercise’, ‘physical training’, ‘aerobic exercise’, ‘resistance exercise’, ‘quality of life’, ‘health-related quality of life’, ‘patient-reported outcome’, ‘randomized controlled trial’, and their related terms. The search strategy for PubMed is shown in Appendix 1, and similar methods were applied to other electronic databases.
The populations included in this study were adult patients (≥ 18 years old) diagnosed with ESRD who have undergone regular MHD for at least three months. All forms of IDE performed during the haemodialysis were included. The comparison interventions included usual care, sham exercise, and no exercise. The outcome of this study was HRQOL. The assessment tools of HRQOL included the SF-36, SF-12, KDQOL-SF, KDQOL-36, etc. Only RCTs published in English and Chinese were included.
The references searched from the nine databases were imported to EndNote X9. Two independent reviewers screened the titles and abstracts after removing duplicates. The full texts were then carefully evaluated according to the inclusion criteria defined by the two independent reviewers. Disagreements regarding the included studies were resolved through discussion or arbitration involving the senior author.
Risk of bias assessment
Two reviewers independently evaluated the risk of bias of the included studies according to the Risk of Bias tool 2.0 (RoB 2.0) from Cochrane Collaboration [28]. Disagreements were resolved by discussion between the two reviewers or in collaboration with the senior reviewer. RoB 2.0 assesses the risk of six domains: randomization process, deviations from the intended interventions, missing outcome data, measurement of the outcome, selection of the reported result, and overall. Each domain of the risk of bias can be assessed as low risk, high risk, or some concerns [28].
Data extraction
Two reviewers developed a structured data extraction table, which was pilot-tested on ten randomly selected papers. The table included basic information (first author, title, keywords, setting, funding, journal, publication year, and publication language), participant information (inclusion and exclusion criteria, socio-demographic, dialysis vintage), and study details (sample size, time and duration of implementation, the length of the study, outcomes, and follow-up). Disagreements between the two reviewers were resolved by discussion or consultation with the senior author.
Meta-analysis
The standardized mean difference (SMD) with 95% confidence intervals (CI) of changes was calculated as the effect measures [26]. An SMD of 0.2 was considered a small effect size, 0.5 a medium effect size, and 0.8 a large effect size [26]. The heterogeneity of the included data was assessed by I2 statistics, with I2 > 50% signifying the existence of heterogeneity and I2 ≤ 50% signifying the absence of heterogeneity [29]. The random-effects analysis model was used to calculate the effect. A subgroup analysis was conducted to explore the impact of different IDE types on HRQOL [26]. The statistical significance level was 0.05. RevMan 5.3 was used for the data analysis. Sensitivity analyses were conducted by excluding studies with a high risk of bias.
Results
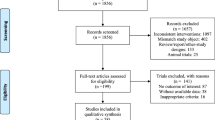
After an initial search of nine electronic databases, 2784 records were identified. After eliminating duplicates, the titles and abstracts of 2170 papers were screened, and 2042 irrelevant papers were excluded. The full text of a total of 128 papers was screened. Finally, 33 papers were included in the systematic review and meta-analysis [15,16,17,18, 30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58] (see Fig. 1).
Characteristics of included studies
Thirty-three RCTs involving 1481 participants were included (Table 1). Five studies were published in Chinese and 28 in English. All studies reported that their rate of compliance ranged from 61% [53] to 100% [18, 30, 31, 51].
Fourteen studies included aerobic exercise, most of which involved pedaling a fixed cycle ergometer during haemodialysis. Thirteen studies utilized resistance exercise, which included leg exercise performed with ankle weights, dumbbells, elastic bands, or training machines. Nine studies included combined aerobic and resistance exercise, and four of those studies compared aerobic exercise, resistance exercise, or combined aerobic and resistance exercise with the interventions in the control group. Three studies included other types of exercise, which involves resistance exercise combined with virtual reality [40], inspiratory muscle training [33], and supine gymnastics [48]. The interventions in the control group generally involved usual care.
Outcomes measured
The outcomes were assessed using the following instruments: SF-36 (21 studies), KDQOL-SF (7 studies), KDQOL-36 (3 studies), SF-12 (1 study), and RAND-36 (1 study). Three studies did not report data on HRQOL, but we obtained the data from the authors via email [32, 39, 49].
Results of risk of bias assessment
The included studies had some concerns (N = 16) to high risk (N = 17) of bias. The risk of bias of the included studies is shown in Fig. 2.
Generic HRQOL assessed by SF-36 and SF-12
The pooled effect showed that IDE improved the PCS and most of the domains of generic HRQOL. A subgroup analysis showed that aerobic exercise effectively improved more domains of generic HRQOL, followed by resistance exercise, other types of exercise, and combined aerobic and resistance exercise. The results also showed that all four types of IDE could significantly increase PF but could not relieve bodily pain (BP). See Table 2 and Appendix 2.
Nineteen studies, which included 861 participants, assessed the effectiveness of IDE on the PCS and MCS compared to the control group. The pooled analysis showed that IDE had a significant positive effect on the PCS (SMD = 0.40, 95% CI 0.22, 0.58, I2 = 36%) but not on the MCS (SMD = 0.19, 95% CI − 0.01, 0.38, I2 = 47%). A subgroup analysis showed that all types of IDE improved PCS, but only resistance exercise had a positive effect on the MCS. Twenty-one studies assessed the effectiveness of IDE on PF. The pooled results showed that IDE had a statistically positive effect on PF (SMD = 0.58, 95% CI 0.36, 0.80, I2 = 61%). A subgroup analysis showed that all types of IDE significantly improved PF. Seventeen studies assessed the effectiveness of IDE on role physical (RP). The pooled results indicated that IDE significantly affected RP (SMD = 0.61, 95% CI 0.21, 1.02, I2 = 86%). A subgroup analysis showed that aerobic exercise and other types of exercise positively affected RP. Eighteen studies assessed the effectiveness of IDE on BP. The pooled results revealed that IDE did not significantly relieve BP (SMD = 0.13, 95% CI − 0.02, 0.28, I2 = 12%). A subgroup analysis revealed that no IDE type could positively affect BP. Eighteen studies assessed the effectiveness of IDE on general health (GH). The pooled results indicated that IDE positively affected GH (SMD = 0.56, 95% CI 0.32, 0.80, I2 = 61%). A subgroup analysis revealed that aerobic exercise and other types of exercise positively affected GH. Eighteen studies assessed the effectiveness of IDE on VT. The pooled analysis showed that IDE positively affected VT (SMD = 0.61, 95% CI 0.41, 0.81, I2 = 48%). A subgroup analysis showed that aerobic exercise and resistance exercise positively affected VT. Eighteen studies assessed the effectiveness of IDE on social functioning (SF), role emotional (RE), and mental health (MH). The pooled analysis showed that IDE had a significantly positive effect on SF (SMD = 0.39, 95% CI 0.08, 0.70, I2 = 77%), RE (SMD = 0.47, 95% CI 0.09, 0.86, I2 = 85%), and MH (SMD = 0.27, 95% CI 0.04, 0.49, I2 = 57%). A subgroup analysis revealed that aerobic exercise could significantly improve SF; resistance exercise could significantly improve MH; and combined aerobic and resistance exercise could significantly improve RE (Table 2, Forest plots, see Appendix 2).
Kidney-specific HRQOL
The meta-analysis included eight studies reporting on 11 domains of kidney-specific HRQOL. Because of the limited number of studies on some domains, subgroup analyses were conducted only in terms of SPL, EKD, and BKD. The pooled effect showed that IDE could ameliorate SPL (SMD = 0.38, 95% CI 0.05, 0.71, I2 = 65%), EKD (SMD = 0.41, 95% CI 0.03, 0.79, I2 = 73%), and the quality of social interaction (SMD = 0.28, 95% CI 0.04, 0.51, I2 = 0%). However, according to the subgroup analyses, none of these four types of IDE could effectively improve SPL, EKD, and BKD. Furthermore, the positive impact of IDE on the other eight domains of kidney-specific HRQOL was not significant (Table 3, Forest plots, see Appendix 2).
Sensitivity analysis
Sensitivity analyses were conducted to examine the influence of the results on studies judged as having a high risk of bias by their removal from the total pooled effect. No significant difference was found in most of the total results except for SF, RE, and EKD, for which the results from the sensitivity analyses were insignificant (P > 0.05).
Discussion
The findings of this study indicate that IDE could ameliorate both generic and kidney-specific HRQOL. Specifically, we found that IDE could improve the PCS and most domains of HRQOL, including PF, RP, GH, VT, SF, RE, and MH on the SF-36; SPL, EKD, and the quality of social interaction regarding KDQOL. The subgroup analysis showed that aerobic exercise could improve more domains of generic HRQOL compared to other types of IDE. However, we need to be cautious when interpreting the study results due to the moderate-to-high risk of bias for the included studies.
In line with published meta-analyses, the current meta-analysis found that IDE improved the PCS in MHD patients but not the MCS [22]. Nonetheless, the effect of IDE on the PCS and MCS in patients undergoing MHD was inconclusive, which may have been due to differences in inclusion criteria. For instance, Huang et al. [23] and Salhab et al. [21] found that IDE could improve the MCS in MHD patients. However, Huang et al. [23] included seven studies, and one exercise was conducted pre-dialysis [59], while Salhab et al. [21] included five studies, of which the design of one study was a non-RCT [60]. We are more confident with our results because the number of studies included in this meta-analysis was larger than in any similar published meta-analysis, and all included studies were RCTs [20, 21, 23, 24]. Therefore, when we interpret the effects of varied meta-analyses, we should consider the reliability of the evidence and the scope of the application.
This meta-analysis indicated that the PCS and its related domains (PF, RP) were more likely to improve than the MCS and its associated domains (RE and MH) via IDE. All types of IDE could improve PF with medium effect sizes, and two kinds of IDE could improve RP with medium-to-large effect sizes. For the domains with more significant correlations with the MCS, only one type of IDE could improve one domain, with a small-to-medium effect size (combined aerobic and resistance exercise for RE; resistance exercise for MH; aerobic exercise for SF). The results of this meta-analysis were consistent with those of the SF-36 measurement model, indicating that domains with higher loadings on the PCS (PF, RP) could more easily be improved by interventions that change physical capacity [19], and IDE could significantly improve physical capacity (e.g., 6-min walk test, sit-to-stand 30, and grip strength) [14, 20]. However, domains with higher loadings on the MCS (RE, MH) responded most to interventions targeting MH rather than physical capacity [19]. Nevertheless, strategies to improve MH for MHD patients need to be explored, given that lower MH was a predictor of death and hospitalization for this population [13].
It should be noted that there is no evidence that IDE can relieve BP. It has been reported that pain is prevalent in 50% to 82% of MHD patients and that up to 75% of patients are treated ineffectively [61]. Musculoskeletal pain is the most common symptom of chronic pain syndromes in patients with ESRD [62]. Although exercise has been recommended as the first-line conservative management to control BP for MHD patients [61], the results of this meta-analysis showed that no IDE could relieve BP. This suggests that IDE has a limited effect on BP, or the assessment tool (SF-36) for BP may not be the best way to measure the impact of IDE on BP in this population. Further intervention studies should include a more specific instruments to measure musculoskeletal pain among patients with ESRD.
The results of this study indicate that aerobic exercise could ameliorate five of eight domains of generic HRQOL, with medium-to-large effect sizes. Several explanations may help us understand why aerobic exercise has a more noticeable effect than other forms of IDE for improving HRQOL. First, aerobic exercise requires less supervision or fewer reminders from healthcare providers than other forms of IDE [6]. Second, aerobic exercise can be easily conducted and may achieve higher compliance [6]. Third, the published meta-analysis showed that aerobic exercise had greater success at improving the aerobic and physical capacities of MHD patients [14]. Therefore, aerobic exercise may be the most preferred type of IDE for improving HRQOL in MHD patients.
Integrating the findings regarding kidney-specific HRQOL, a small-to-medium effect size improvement was observed for three domains. However, subgroup analysis for these domains showed no significant improvement in any of the four types of IDE. IDE could improve the dialytic effect and aerobic capacity, which would reduce the adverse impact of ESRD, improve SPL, and reduce EKD [14, 22]. In addition, the quality of social interaction in the KDQOL-SF was assessed by three items reflecting the interaction of MHD patients with those around them [11]. During the implementation of IDE, MHD patients need to interact with the healthcare provider, which may help them better interact with others and improve the quality of their social interaction.
The results of this meta-analysis indicate that some domains of kidney-specific HRQOL could not be enhanced by IDE, including BKD, work status, cognitive function, sleep, social support, dialysis staff encouragement, patients satisfaction, and sexual function. Therefore, we should consider improving the above domains of kidney-specific HRQOL to help MHD patients attain happiness in life.
Implications for practice and research
This systematic review identified the positive effect of IDE on the domains of HRQOL in MHD patients. The study results will help MHD patients, healthcare providers, and policymakers understand that IDE does have beneficial effects on HRQOL. Aerobic exercise could improve more domains of HRQOL compared to other types of IDE, and aerobic exercise could be easily conducted during dialysis [6]. Thus, we recommend aerobic exercise in more MHD patients in clinical practice. In addition, patients undergoing MHD who wish to improve their physical capacity are highly recommended to conduct IDE, for IDE could significantly increase physical performance and its related domains of HRQOL [14, 23]. In the meantime, strategies to improve the MCS and its related domains, BP, and kidney-specific HRQOL, in MHD patients need to be explored. These components and domains of HRQOL were key indicators in the death and hospitalization of this population [13].
Several aspects could be studied to improve the understanding of the effect of IDE on HRQOL in MHD patients. Since IDE is an effective way to enhance most domains of HRQOL for patients undergoing MHD, it may play a positive role in improving survival rates and decreasing hospitalization rates [13]. This hypothesis calls for further verification in future clinical trials. In addition, there is a need to explore the various effects of different levels of intensity, frequency, duration, as well as the type of IDE for the different domains of HRQOL [14]. In the meantime, considering the increased risk of bias if clinical trials fail in participant blinding, the methodology of clinical trials needs to be improved [28]. Lastly, although IDE implementation will benefit MHD patients, it also needs time, equipment, and human resources [6]. Therefore, a cost-effectiveness analysis for IDE is required.
Strengths and limitations
This study provides a comprehensive review and meta-analysis of the effectiveness of IDE on MHD patients in terms of the various domains of HRQOL. Moreover, the results from the subgroup analyses help in understanding the different effects of IDE on HRQOL in MHD patients. Additionally, compared with the existing meta-analysis focusing only on the PCS and MCS, the analysis of eight domains of generic HRQOL in this review provided a deeper understanding of the effect of IDE on MHD patients. Furthermore, this meta-analysis explored the effects of IDE on kidney-specific HRQOL, which was not discussed in the published meta-analysis. Finally, a comprehensive search strategy and rigorous criteria were set to select RCTs for evaluation, thereby increasing the reliability of the conclusions of this study.
Some limitations of this review should not be neglected. Only Chinese and English articles were included in this study, which might have missed studies published in other languages. Additionally, the included RCTs had some methodological weaknesses. Due to the characteristics of exercise intervention trials, most of the included RCTs were unable to implement the blinded participant method, which may affect the validity of the results. Furthermore, every IDE may vary in the training process, frequency, duration, and intensity, leading to heterogeneity. The limitations mentioned above should be considered when interpreting the findings of this study.
Conclusion
IDE can improve most generic and some kidney-specific HRQOL in MHD patients, but different forms of IDE may have varied effects. The results of this study show that aerobic exercise may be more effective improvement of HRQOL. IDE can more easily enhance the PCS and PF but not the MCS and BP. More well-designed RCTs comparing the effect and safety of different IDE types on HRQOL need to be conducted.
Data availability
All data generated or analyzed during this study are included in this published article and its supplementary information files.
Code availability
Not applicable.
References
Collaboration, G. B. D. C. K. D. (2020). Global, regional, and national burden of chronic kidney disease, 1990–2017: A systematic analysis for the global burden of disease study 2017. Lancet, 395(10225), 709–733. https://doi.org/10.1016/S0140-6736(20)30045-3
Liyanage, T., Ninomiya, T., Jha, V., Neal, B., Patrice, H. M., Okpechi, I., Zhao, M. H., Lv, J., Garg, A. X., Knight, J., Rodgers, A., Gallagher, M., Kotwal, S., Cass, A., & Perkovic, V. (2015). Worldwide access to treatment for end-stage kidney disease: A systematic review. Lancet, 385(9981), 1975–1982. https://doi.org/10.1016/S0140-6736(14)61601-9
Wang, F., Yang, C., Long, J., Zhao, X., Tang, W., Zhang, D., Bai, K., Su, Z., Gao, B., Chu, H., Wang, J., Sun, X., Wang, S., Zuo, L., Wang, Y., Yu, F., Wang, H., Zhang, L., & Zhao, M. H. (2019). Executive summary for the 2015 annual data report of the China kidney disease network (CK-NET). Kidney International, 95(3), 501–505. https://doi.org/10.1016/j.kint.2018.11.011
Eckert, K., Motemaden, L., & Alves, M. (2018). Effect of hemodialysis compared with conservative management on quality of life in older adults with end-stage renal disease: Systematic review. Journal of Hospice and Palliative Nursing, 20(3), 279–285. https://doi.org/10.1097/NJH.0000000000000444
Legrand, K., Speyer, E., Stengel, B., Frimat, L., Ngueyon Sime, W., Massy, Z. A., Fouque, D., Laville, M., Combe, C., Jacquelinet, C., Durand, A. C., Edet, S., Gentile, S., Briancon, S., & Ayav, C. (2020). Perceived health and quality of life in patients with CKD, including those with kidney failure: Findings from national surveys in france. American Journal of Kidney Diseases, 75(6), 868–878. https://doi.org/10.1053/j.ajkd.2019.08.026
Fang, H. Y., Burrows, B. T., King, A. C., & Wilund, K. R. (2020). A comparison of intradialytic versus out-of-clinic exercise training programs for hemodialysis patients. Blood Purification, 49(1–2), 151–157. https://doi.org/10.1159/000503772
GROUP, W. (1995). The world health organization quality of life assessment (WHOQOL): Position paper from the world health organization. Social Science and Medicine, 41(10), 1403–1409. https://doi.org/10.1016/0277-9536(95)00112-k
Karimi, M., & Brazier, J. (2016). Health, health-related quality of life, and quality of life: What is the difference? PharmacoEconomics, 34(7), 645–649. https://doi.org/10.1007/s40273-016-0389-9
Valderrabano, F., Jofre, R., & Lopez-Gomez, J. M. (2001). Quality of life in end-stage renal disease patients. American Journal of Kidney Diseases, 38(3), 443–464. https://doi.org/10.1053/ajkd.2001.26824
Ware, J. E., Jr., & Sherbourne, C. D. (1992). The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Medical Care, 30(6), 473–483.
Hays, R. D., Kallich, J. D., Mapes, D. L., Coons, S. J., & Carter, W. B. (1994). Development of the kidney disease quality of life (KDQOL) instrument. Quality of Life Research, 3(5), 329–338. https://doi.org/10.1007/BF00451725
Tao, X., Chow, S. K., & Wong, F. K. (2014). Determining the validity and reliability of the Chinese version of the kidney disease quality of life questionnaire (KDQOL-36). BMC Nephrology, 15, 115. https://doi.org/10.1186/1471-2369-15-115
Mapes, D. L., Lopes, A. A., Satayathum, S., McCullough, K. P., Goodkin, D. A., Locatelli, F., Fukuhara, S., Young, E. W., Kurokawa, K., Saito, A., Bommer, J., Wolfe, R. A., Held, P. J., & Port, F. K. (2003). Health-related quality of life as a predictor of mortality and hospitalization: The dialysis outcomes and practice patterns study (DOPPS). Kidney International, 64(1), 339–349. https://doi.org/10.1046/j.1523-1755.2003.00072.x
Ferrari, F., Helal, L., Dipp, T., Soares, D., Soldatelli, Â., Mills, A. L., Paz, C., Tenório, M. C. C., Motta, M. T., Barcellos, F. C., & Stein, R. (2020). Intradialytic training in patients with end-stage renal disease: A systematic review and meta-analysis of randomized clinical trials assessing the effects of five different training interventions. Journal of Nephrology, 33(2), 251–266. https://doi.org/10.1007/s40620-019-00687-y
Cheema, B., Abas, H., Smith, B., O’Sullivan, A., Chan, M., Patwardhan, A., Kelly, J., Gillin, A., Pang, G., Lloyd, B., et al. (2007). Progressive exercise for anabolism in kidney disease (PEAK): A randomized, controlled trial of resistance training during hemodialysis. Journal of the American Society of Nephrology, 18(5), 1594–1601. https://doi.org/10.1681/ASN.2006121329
Ouzouni, S., Kouidi, E., Sioulis, A., Grekas, D., & Deligiannis, A. (2009). Effects of intradialytic exercise training on health-related quality of life indices in haemodialysis patients. Clinical Rehabilitation, 23(1), 53–63. https://doi.org/10.1177/0269215508096760
Segura-Orti, E., Kouidi, E., & Lison, J. F. (2009). Effect of resistance exercise during hemodialysis on physical function and quality of life: Randomized controlled trial. Clinical Nephrology, 71(5), 527–537. https://doi.org/10.5414/cnp71527
Dobsak, P., Homolka, P., Svojanovsky, J., Reichertova, A., Soucek, M., Novakova, M., Dusek, L., Vasku, J., Eicher, J. C., & Siegelova, J. (2012). Intra-dialytic electrostimulation of leg extensors may improve exercise tolerance and quality of life in hemodialyzed patients. Artificial Organs, 36(1), 71–78. https://doi.org/10.1111/j.1525-1594.2011.01302.x
Ware, J. E., Jr. (2000). SF-36 health survey update. Spine, 25(24), 3130–3139. https://doi.org/10.1097/00007632-200012150-00008
Zhang, F., Zhou, W. Q., Sun, Q. Z., Zhai, Y. Y., Zhang, Y., Su, H., & Wang, Z. C. (2019). Effects of intradialytic resistance exercises on physical performance, nutrient intake and quality of life among haemodialysis people: A systematic review and meta-analysis. Nursing Open. https://doi.org/10.1002/nop2.274
Salhab, N., Karavetian, M., Kooman, J., Fiaccadori, E., & El Khoury, C. F. (2019). Effects of intradialytic aerobic exercise on hemodialysis patients: A systematic review and meta-analysis. Journal of Nephrology, 32(4), 549–566. https://doi.org/10.1007/s40620-018-00565-z
Pu, J., Jiang, Z., Wu, W. H., Li, L., Zhang, L. L., Li, Y., Liu, Q., & Ou, S. T. (2019). Efficacy and safety of intradialytic exercise in haemodialysis patients: A systematic review and meta-analysis. British Medical Journal Open, 9(1), e020633. https://doi.org/10.1136/bmjopen-2017-020633
Huang, M., Lv, A. L., Wang, J., Xu, N., Ma, G. R., Zhai, Z. H., Zhang, B., Gao, J. L., & Ni, C. P. (2019). Exercise training and outcomes in hemodialysis patients: Systematic review and meta-analysis. American Journal of Nephrology, 50(4), 240–254. https://doi.org/10.1159/000502447
Young, H. M. L., March, D. S., Graham-Brown, M. P. M., Jones, A. W., Curtis, F., Grantham, C. S., Churchward, D. R., Highton, P., Smith, A. C., Singh, S. J., Bridle, C., & Burton, J. O. (2018). Effects of intradialytic cycling exercise on exercise capacity, quality of life, physical function and cardiovascular measures in adult haemodialysis patients: A systematic review and meta-analysis. Nephrology Dialysis Transplantation, 33(8), 1436–1445. https://doi.org/10.1093/ndt/gfy045
Neto, M. G., de Lacerda, F. F. R., Lopes, A. A., Martinez, B. P., & Saquetto, M. B. (2018). Intradialytic exercise training modalities on physical functioning and health-related quality of life in patients undergoing maintenance hemodialysis: Systematic review and meta-analysis. Clinical Rehabilitation, 32(9), 1189–1202. https://doi.org/10.1177/0269215518760380
Higgins, J. P. T., Thomas, J., Chandler, J., Cumpston, M., Li, T., Page, M. J., Welch, V. A., & Collaboration, C. (2019). Cochrane handbook for systematic reviews of interventions (2nd ed.). Wiley-Blackwell.
Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G., & Group P. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Journal of Clinical Epidemiology, 62(10), 1006–1012. https://doi.org/10.1016/j.jclinepi.2009.06.005
Sterne, J. A. C., Savovic, J., Page, M. J., Elbers, R. G., Blencowe, N. S., Boutron, I., Cates, C. J., Cheng, H. Y., Corbett, M. S., Eldridge, S. M., Emberson, J. R., Hernan, M. A., Hopewell, S., Hrobjartsson, A., Junqueira, D. R., Juni, P., Kirkham, J. J., Lasserson, T., Li, T., … Higgins, J. P. T. (2019). RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ, 366, l4898. https://doi.org/10.1136/bmj.14898
Higgins, J. P., & Thompson, S. G. (2002). Quantifying heterogeneity in a meta-analysis. Statistics in Medicine, 21(11), 1539–1558. https://doi.org/10.1002/sim.1186
Fathi, M., & Hejazi, K. (2021). The effect of six months aerobic exercise during dialysis on liver enzymes, cystatin c and quality of life of hemodialysis patients. The Journal of Sports Medicine and Physical Fitness. https://doi.org/10.23736/S0022-4707.21.11812-2
Zhao, J. R., Qi, Q. G., Xu, S. S., & Shi, D. Y. (2020). Combined aerobic resistance exercise improves dialysis adequacy and quality of life in patients on maintenance hemodialysis. Clinical Nephrology, 93(6), 275–282. https://doi.org/10.5414/cn110033
Zhang, F., Huang, L., Wang, W., Shen, Q., & Zhang, H. (2020). Effect of intradialytic progressive resistance exercise on physical fitness and quality of life in maintenance haemodialysis patients. Nursing Open, 7(6), 1945–1953. https://doi.org/10.1002/nop2.585
Yuenyongchaiwat, K., Namdang, P., Vasinsarunkul, P., Phongsukree, P., Chaturattanachaiyaporn, K., Pairojkittrakul, S., & Traitanon, O. (2020). Effectiveness of inspiratory muscle training on respiratory fitness and breathlessness in chronic renal failure: A randomized control trial. Physiotherapy Research International, 26, e1879. https://doi.org/10.1002/pri.1879
Young, H. M. L., March, D. S., Highton, P. J., Graham-Brown, M. P. M., Churchward, D. C., Grantham, C., Goodliffe, S., Jones, W., Cheung, M. M., Greenwood, S. A., Eborall, H. C., Conroy, S., Singh, S. J., Smith, A. C., & Burton, J. O. (2020). Exercise for people living with frailty and receiving haemodialysis: A mixed-methods randomised controlled feasibility study. British Medical Journal Open, 10(11), e041227. https://doi.org/10.1136/bmjopen-2020-041227
Valle, F. M., Valle Pinheiro, B., Almeida Barros, A. A., Ferreira Mendonça, W., de Oliveira, A. C., de Oliveira Werneck, G., de Paula, R. B., & Moura Reboredo, M. (2020). Effects of intradialytic resistance training on physical activity in daily life, muscle strength, physical capacity and quality of life in hemodialysis patients: A randomized clinical trial. Disability and Rehabilitation, 42(25), 3638–3644. https://doi.org/10.1080/09638288.2019.1606857
Lee, J. Y., Baek, S. H., Lee, Y. M., Cho, J. H., Kim, J. C., & Choi, S. W. (2020). The effect of a 12-week intradialytic exercise on patients’ blood indices, physical performance, and quality of life. Journal of Medical Imaging and Health Informatics, 10(6), 1429–1435. https://doi.org/10.1166/jmihi.2020.3066
Jamshidpour, B., Bahrpeyma, F., & Khatami, M.-R. (2020). The effect of aerobic and resistance exercise training on the health related quality of life, physical function, and muscle strength among hemodialysis patients with Type 2 diabetes. Journal of Bodywork and Movement Therapies, 24(2), 98–103. https://doi.org/10.1016/j.jbmt.2019.10.003
Huang, M., Lv, A. L., Wang, J., Zhang, B., Xu, N., Zhai, Z. H., Gao, J. L., Wang, Y., Li, T. Z., & Ni, C. P. (2020). The effect of intradialytic combined exercise on hemodialysis efficiency in end-stage renal disease patients: A randomized-controlled trial. International Urology and Nephrology, 52(5), 969–976. https://doi.org/10.1007/s11255-020-02459-1
Suhardjono, N., Umami, V., Tedjasukmana, D., & Setiati, S. (2019). The effect of intradialytic exercise twice a week on the physical capacity, inflammation, and nutritional status of dialysis patients: A randomized controlled trial. Hemodialysis International, 23(4), 486–493. https://doi.org/10.1111/hdi.12764
Maynard, L. G., de Menezes, D. L., Liao, N. S., de Jesus, E. M., Andrade, N. L. S., Santos, J. C. D., da Silva, W. M., Bastos, K. D., & Barreto, J. A. S. (2019). Effects of exercise training combined with virtual reality in functionality and health-related quality of life of patients on hemodialysis. Games for Health Journal, 8(5), 339–348. https://doi.org/10.1089/g4h.2018.0066
Lopes, L. C. C., Mota, J. F., Prestes, J., Schincaglia, R. M., Silva, D. M., Queiroz, N. P., Freitas, A., Lira, F. S., & Peixoto, M. D. G. (2019). Intradialytic resistance training improves functional capacity and lean mass gain in individuals on hemodialysis: A randomized pilot trial. Archives of Physical Medicine and Rehabilitation, 100(11), 2151–2158. https://doi.org/10.1016/j.apmr.2019.06.006
Hu, X., Yin, L., Zhang, H., Dong, Z., & Zhang, Y. (2019). Effects of multidisciplinary cooperating exercise on quality of life and micro-inflammatory state among patients undergoing Maintenance Hemodialysis. Chinese Nursing Management, 19(10), 1467–1471. https://doi.org/10.3969/j.issn.1672-1756.2019.10.008
Ye, F. (2018). Bicycle exercise in dialysis patients with maintenance hemodialysis hypotension effect of intervention study. Master Huzhou University.
Rosa, C. S. D. C., Nishimoto, D. Y., Souza, G. D. E., Ramirez, A. P., Carletti, C. O., Daibem, C. G. L., Sakkas, G. K., & Monteiro, H. L. (2018). Effect of continuous progressive resistance training during hemodialysis on body composition, physical function and quality of life in end-stage renal disease patients: A randomized controlled trial. Clinical Rehabilitation, 32(7), 899–908. https://doi.org/10.1177/0269215518760696
Dong, Z. (2018). Effects of intradialytic resistance exercise on maintenance hemodialysis patients with sarcopenia. Nanjing Medical University.
Liu, Y. (2017). The effects of resistant exercise on maintenance hemodialysis patients with intradialytic hypotension. Dalian Medical University.
Abreu, C. C., Cardozo, L. F. M. F., Stockler-Pinto, M. B., Esgalhado, M., Barboza, J. E., Frauches, R., & Mafra, D. (2017). Does resistance exercise performed during dialysis modulate Nrf2 and NF-kappa B in patients with chronic kidney disease? Life Sciences, 188, 192–197. https://doi.org/10.1016/j.lfs.2017.09.007
Xu, J. (2016). Effect of supine exercise on the quality of maintenance hemodialysis patients’ lives. Heilongjiang University of Chinese Medicine.
Thompson, S., Klarenbach, S., Molzahn, A., Lloyd, A., Gabrys, I., Haykowsky, M., & Tonelli, M. (2016). Randomised factorial mixed method pilot study of aerobic and resistance exercise in haemodialysis patients: DIALY-SIZE! British Medical Journal Open, 6(9), e012085. https://doi.org/10.1136/bmjopen-2016-012085
Wu, Y. Y., He, Q., Yin, X. H., He, Q., Cao, S. S., & Ying, G. H. (2014). Effect of individualized exercise during maintenance haemodialysis on exercise capacity and health-related quality of life in patients with uraemia. Journal of International Medical Research, 42(3), 718–727. https://doi.org/10.1177/0300060513509037
Marchesan, M., Nunes, V. G. D. S., & Rombaldi, A. J. (2014). Physical training improves physical fitness and the quality of life of patients on hemodialysis. Revista Brasileira de Cineantropometria e Desempenho Humano. https://doi.org/10.5007/1980-0037.2014v16n3p334
Giannaki, C. D., Sakkas, G. K., Karatzaferi, C., Hadjigeorgiou, G. M., Lavdas, E., Kyriakides, T., Koutedakis, Y., & Stefanidis, I. (2013). Effect of exercise training and dopamine agonists in patients with uremic restless legs syndrome: A six-month randomized, partially double-blind, placebo-controlled comparative study. BMC Nephrology, 14, 194. https://doi.org/10.1186/1471-2369-14-194
Koh, K. P., Fassett, R. G., Sharman, J. E., Coombes, J. S., & Williams, A. D. (2010). Effect of intradialytic versus home-based aerobic exercise training on physical function and vascular parameters in hemodialysis patients: A randomized pilot study. American Journal of Kidney Diseases, 55(1), 88–99. https://doi.org/10.1053/j.ajkd.2009.09.025
Chen, J. L. T., Godfrey, S., Ng, T. T., Moorthi, R., Liangos, O., Ruthazer, R., Jaber, B. L., Levey, A. S., & Castaneda-Sceppa, C. (2010). Effect of intra-dialytic, low-intensity strength training on functional capacity in adult haemodialysis patients: A randomized pilot trial. Nephrology Dialysis Transplantation, 25(6), 1936–1943. https://doi.org/10.1093/ndt/gfp739
Johansen, K. L., Painter, P. L., Sakkas, G. K., Gordon, P., Doyle, J., & Shubert, T. (2006). Effects of resistance exercise training and nandrolone decanoate on body composition and muscle function among patients who receive hemodialysis: A randomized, controlled trial. Journal of the American Society of Nephrology, 17(8), 2307–2314. https://doi.org/10.1681/asn.2006010034
van Vilsteren, M. C. B. A., de Greef, M. H. G., & Huisman, R. M. (2005). The effects of a low-to-moderate intensity pre-conditioning exercise programme linked with exercise counselling for sedentary haemodialysis patients in The Netherlands: Results of a randomized clinical trial. Nephrology Dialysis Transplantation, 20(1), 141–146. https://doi.org/10.1093/ndt/gfh560
Parsons, T. L., Toffelmire, E. B., & King-VanVlack, C. E. (2004). The effect of an exercise program during hemodialysis on dialysis efficacy, blood pressure and quality of life in end-stage renal disease (ESRD) patients. Clinical Nephrology, 61(4), 261–274. https://doi.org/10.5414/cnp61261
Painter, P., Moore, G., Carlson, L., Paul, S., Myll, J., Phillips, W., & Haskell, W. (2002). Effects of exercise training plus normalization of hematocrit on exercise capacity and health-related quality of life. American Journal of Kidney Diseases, 39(2), 257–265. https://doi.org/10.1053/ajkd.2002.30544
Song, W. J., & Sohng, K. Y. (2012). Effects of progressive resistance training on body composition, physical fitness and quality of life of patients on hemodialysis. Journal of Korean Academy of Nursing, 42(7), 947–956. https://doi.org/10.4040/jkan.2012.42.7.947
Sakkas, G. K., Hadjigeorgiou, G. M., Karatzaferi, C., Maridaki, M. D., Giannaki, C. D., Mertens, P. R., Rountas, C., Vlychou, M., Liakopoulos, V., & Stefanidis, I. (2008). Intradialytic aerobic exercise training ameliorates symptoms of restless legs syndrome and improves functional capacity in patients on hemodialysis. Asaio Journal, 54(2), 185–190. https://doi.org/10.1097/MAT.0b013e3181641b07
Raina, R., Krishnappa, V., & Gupta, M. (2018). Management of pain in end-stage renal disease patients: Short review. Hemodialysis International, 22(3), 290–296. https://doi.org/10.1111/hdi.12622
Hsu, H. J., Yen, C. H., Hsu, K. H., Wu, I. W., Lee, C. C., Hung, M. J., Sun, C. Y., Chou, C. C., Chen, Y. C., Hsieh, M. F., Chen, C. Y., Hsu, C. Y., Tsai, C. J., & Wu, M. S. (2014). Factors associated with chronic musculoskeletal pain in patients with chronic kidney disease. BMC Nephrology, 15, 6. https://doi.org/10.1186/1471-2369-15-6
Acknowledgements
No acknowledgments.
Funding
This study did not receive any specific grant from funding agencies in public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
HH contributed to the conception and design, search, screening, data extraction, data analysis and interpretation, and manuscript writing. XL contributed to the search, screening, data extraction, data interpretation, and manuscript writing. PHC contributed to the data analysis and interpretation, manuscript revise. EPHC contributed to the conception and design, data analysis and interpretation, manuscript writing, and final approval of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
Ethical approval was not required for conducting this review.
Consent to participate
Informed consent was not required for conducting this review.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Hu, H., Liu, X., Chau, P.H. et al. Effects of intradialytic exercise on health-related quality of life in patients undergoing maintenance haemodialysis: a systematic review and meta-analysis. Qual Life Res 31, 1915–1932 (2022). https://doi.org/10.1007/s11136-021-03025-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-021-03025-7