Abstract
Purpose
Even treated chronic inflammatory demyelinating polyradiculoneuropathy (CIDP) continues to pose a significant burden in patients’ everyday functioning and may continuously affect their quality of life (QoL). The aims of our prospective study were to analyze health-related QoL in CIDP patients during a 1-year follow-up period in real-life settings and to compare QoL changes with changes in disability and with patient impression of change.
Methods
The study comprised 59 patients diagnosed with CIDP. SF-36 questionnaire was applied in order to evaluate patients’ QoL. Inflammatory neuropathy cause and treatment (INCAT) disability scale was used to assess patients’ functionality. The second question from the SF-36 questionnaire was used as an estimation of the patient impression of change (PIC) after 1 year.
Results
SF-36 scores did not change over time in the group as a whole. According to INCAT disability scores, worsening was registered in 24 (40%) patients and improvement in 8 (14%). Fifteen (25%) patients reported worsening and the same number reported improvement, according to PIC. Concordant results on INCAT and PIC were registered in 49% of patients. Pooled SF-36 scores moderately correlated with pooled INCAT disability scores (rho = − 0.27 to − 0.59, p < 0.01). One-year changes of SF-36 scores did not differ when compared to different INCAT outcomes (worsening, stable, improvement). On the other hand, significant changes of SF-36 scores in different outcome groups according to PIC (worsening, stable, improvement) were noted (p < 0.01).
Conclusion
INCAT, PIC, and SF-36 are complementary outcome measures that provide neurologists with useful items of information. We propose complementary use of these scales in CIDP patients in everyday clinical practice in order to detect worsening of the disease and/or of related symptoms on time.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic inflammatory demyelinating polyradiculoneuropathy (CIDP) is an autoimmune neuropathy which is characterized by progressive, stepwise, or recurrent symmetric proximal and distal weakness, sensory dysfunction, and absent or reduced tendon reflexes of all extremities, developing over the period of at least 2 months [1]. Although different therapeutic modalities are currently available for this chronic disorder, it seems that even previously treated CIDP continues to impose a significant burden on patients’ everyday functioning and may continuously affect their quality of life (QoL).
Health-related QoL is generally considered to reflect the impact of disease and treatment on disability and daily functioning; it has also been considered to reflect the impact of perceived health on an individual’s ability to live a fulfilling life [2]. In most of the previous studies, QoL in CIDP patients was assessed using generic questionnaires and QoL was found to be expectedly reduced in these patients [3, 4]. It was further noted that QoL in CIDP patients could be affected in both physical and mental domains, although it was more influenced by the patients’ physical status [3, 5,6,7,8]. Various non-physical factors such as fatigue, neuropathic pain, anxiety, and depression may also affect patients’ QoL [2, 9,10,11]. Nevertheless, in the majority of the previous studies comprising CIDP patients, QoL was evaluated only in a single time frame. Apart from the results of clinical trials [12], there are still no data about the longitudinal analysis of QoL in CIDP during the disease course in real-life settings.
The aim of our prospective study was to analyze the change in disability and quality of life in CIDP patients during a 1-year follow-up period in real-life settings and to compare different outcome measures.
Materials and methods
The patients who fulfilled the EFNS/PNS diagnostic criteria for CIDP were included in this research (EFNS/PNS Guidelines) [1]. CIDP variants were also evaluated in accordance with the EFNS/PNS criteria. Fifty-nine patients who came for their regular outpatient check-ups were assessed at baseline and then again at 1-year follow-up. None of these patients was newly diagnosed and drug naïve. All of them had been previously treated or were being treated while the study was conducted. The study was approved by the Ethical Committee of the Faculty of Medicine, University of Belgrade. All the patients signed an informed consent in order to participate in the study.
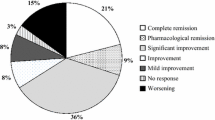
Sociodemographic and diagnostic data were collected from the patients’ medical records and from the patients themselves at the time of initial testing and retesting. We also analyzed the presence of significant comorbid disorders such as diabetes mellitus and monoclonal gammopathy of undetermined significance (MGUS) (excluding the patients with IgM), as well as each patient’s therapeutic modality and response to treatment. The Medical Research Council sum scale (MRC-SS) was used to estimate the muscle strength [13]. According to the INCAT (Inflammatory Neuropathy Cause and Treatment) disability score, we evaluated the patients’ functionality degree [14]. An increase in at least one point on the adjusted INCAT disability scale was considered to be an impairment, whereas a decrease in at least one point on the adjusted INCAT disability scale was thought to be an improvement.
All the patients filled in the Serbian version of the SF-36 questionnaire, as the measure of health-related QoL [15]. This is a generic instrument which measures eight health domains: physical functioning (PF), role physical (RP), bodily pain (BP), general health (GH), vitality (VT), social functioning (SF), role emotional (RE) and mental health (MH). These scales are summarized in two main composite scores: physical composite score (PCS) and mental composite score (MCS), followed by the total SF-36 score. All these scores fit in the range of 0 to 100 points, where higher scores reflect a better QoL. We used question #2 from the SF-36 questionnaire as an estimation of the patients’ impression of change (PIC) compared to 1 year before. The patients could describe their QoL as much better, somewhat better, about the same, somewhat worse and much worse. For the purpose of this study, the patients were divided into three groups: disease worsening (somewhat worse and worse), stable disease (about the same) or disease improvement (somewhat better and better).
Descriptive statistics were used to characterize the study population. Comparison of the INCAT and SF-36 scores between two time points was assessed using the Wilcoxon signed-rank test. Concordance between INCAT status and PIC was analyzed through kappa statistics, for the entire group and for the subgroups of treated and non-treated patients. We correlated pooled SF-36 scores with pooled INCAT scores using Spearman’s rho (pooled scores are scores for each patient at each time point). The changes of SF-36 scores between three different outcome groups were compared using the Kruskal–Wallis test. The significance level was set at < 0.05.
Results
Main sociodemographic and clinical characteristics of investigated CIDP patients are presented in Tables 1 and 2. Men accounted for 63% of our cohort. Typical CIDP variant was present in 63% of the patients. About 86% of the patients fulfilled the definite EFNS/PNS nerve conduction studies (NCS) criteria. Diabetes mellitus was present in 19% and IgG or IgA paraproteinemia were found in 12% of our patients. Only 42% of the patients received the treatment during a 1-year study period. More than half of the patients had supposedly a non-active disease with or without symptoms.
After a year, mean INCAT disability score for the entire group worsened (1.5 ± 1.9 vs 2.2 ± 1.9, p < 0.01) (Table 2). However, when it comes to the individual patients’ INCAT, deterioration was registered in 24 (40%) patients, stable state in 27 (46%) patients and improvement in eight (14%) patients (Table 3). It is important to mention that 35% of the patients without therapy experienced disease worsening which suggests that their disease was not completely inactive. On the other hand, CIDP worsening was detected in 48% of the patients on therapy and in the majority of cases the reason was steroid dose tapering, but it was also due to the IVIg dosage reduction or an increase in the treatment interval.
When the entire group is concerned, neither the SF-36 total score nor its sub-scores changed over a 1-year period (Table 4). According to PIC, 15 (25%) patients reported worsening, 29 (49%) patients were in a stable state, and 15 (25%) patients had an improvement. Completely the same pattern of changes on INCAT and PIC was found in 29 (49%) patients. A completely different pattern of changes (i.e., improvement on one scale and worsening on the other) was registered in only two (3.4%) patients. Improved INCAT with no change on PIC was found in five (8.5%) patients and worsened INCAT with no change on PIC in 10 (16.9%) CIDP patients. The main noticed discrepancy was that the patients reported their subjective state (PIC) to be better than the one assessed by objective scale (INCAT), which occurred in 35% of cases in the non-treated group and in 40% of cases in the treated group. Cohen’s kappa was as follows: 0.20 (95%CI 0.01–0.39) for the whole group; 0.21 (95%CI − 0.05–0.48) for non-treated group; and 0.18 (95%CI − 0.10–0.47) for treated group. These values suggest only a slight to fare agreement between the two measures [16].
Pooled SF-36 score moderately correlated with pooled INCAT disability scores (rho = − 0.27 to rho = − 0.59, p < 0.01) (Table 5); however, somewhat stronger correlations were noted for physical than for mental domains. The changes of SF-36 scores in different outcome groups according to the INCAT disability scale are presented in Table 6. No differences in the changes of SF-36 scores were observed across these three groups when all the patients were included, when only patients without therapy were included or when only patients on therapy were taken into consideration (results not shown).
The changes of all SF-36 scores in different outcome groups according to PIC are presented in Table 7. Significant changes were noted in PF, GH, VT, and MH domains, as well as in PCS, MCS and the total SF-36 score. The majority of these score changes were different in the worsening group compared to the stable (and improvement) groups.
Discussion
Since the longitudinal data on QoL in CIDP patients are still under-researched, especially in real-life settings, our study was conducted with the purpose of providing novel information on the course of the health-related QoL in these patients during a 1-year follow-up. We also wanted to correlate these changes with the changes in patients’ functionality and their impression of change.
In this study, two different patient-reported outcome measures were used: INCAT, which is somewhat more objective, and PIC being fully subjective. These two measures showed consistent results in 49% of cases, while in 3% of cases the results were completely opposite. Around 8% of patients improved on INCAT, but no changes were detected on PIC. The main discrepancy was that the patients reported their subjective state (PIC) to be better than the one assessed by objective scale (INCAT), which occurred in 35% of the cases from the non-treated group and in 40% of the cases from the treated group. Thus, although INCAT scale was able to detect improvement or worsening in functionality, this change might not necessarily be significant for the patient. This confirms once again that many factors apart from disability may affect a patient’s impression of his/her state of health, including pain, sleep disorders, fatigue, depression, anxiety etc. [3, 17, 18]. Subjective feeling of improvement or deterioration is not necessarily associated with a change in disability. Previous studies have already underlined the importance of non-physical life aspects for CIDP patients [9, 10]. PIC is able to detect other disease aspects which are not comprised by the INCAT scale, and therefore, PIC seems to be a good complementary outcome measure. However, one must note that it may be complicated for a patient to recall his/her health status as it was a year ago, since PIC compares the status of health in the moment of testing and 1 year before. On the other hand, INCAT can be easily marked at two time points by a neurologist, thus avoiding the problem of recollection. Our study confirmed that the patient's opinion is not totally reliable with respect to CIDP change and therefore it highlighted the importance of the use of more objective outcome measures in therapy monitoring, such as INCAT. If someone has improved based on the INCAT scale, but is still stable or even worsened based on PIC or another subjective measure, we believe he/she is not a candidate for immune therapy introduction or dose increment, but rather a candidate for additional symptomatic therapies that may improve pain, sleep impairment, fatigue, mood disorders etc. On the other hand, if someone has worsened based on the INCAT scale, but is still stable or even improved based on PIC or another subjective measure, we believe he/she might be a candidate for immune therapy introduction or dose increment with the aim of improving functionality, but only after consulting the patient and after estimating the risk benefit ratio.
In our study, cross sectional correlation between INCAT disability score and SF-36 score was moderate and somewhat stronger for physical domains. This was also reported in several previous papers [3, 5,6,7,8]. These findings might indicate that physical disability can be considered an important burden in patients’ daily activities. On the other hand, our longitudinal data showed that changes of SF-36 scores did not differ in different outcome groups according to the INCAT disability scale. In other words, worsening or improvement of functionality did not necessarily mean improvement in QoL as perceived by patients themselves. Indeed, Merkies et al. showed the correlation between SF-36 scores and physical disability, but only 20% of variance of PCS of SF-36 was explained using the INCAT measure [19]. Some of these additional factors that may explain the discrepancy were listed in the previous paragraph. Furthermore, the duration of disease and prolonged therapy may place an additional burden on patients. SF-36 seems to be an appropriate measure for assessing multidimensional aspects of CIDP influence on patients’ lives that can be missed when only INCAT is used.
Subjective worsening as measured by PIC was in correlation with the quality-of-life changes, including changes in PCS, MCS and total SF-36 score. Regarding the subdomains, the main differences were observed for PF, GH, VT, and MH suggesting that worsening in these domains was most important for patients’ subjective perception of disease worsening. Worsening of these four SF-36 scores in approximately 20 points might be a good signal of the degree of worsening important for a patient. PF domain comprises a number of important activities that are different compared to those comprised by the INCAT disability scale. GH domain contains questions regarding a patient’s subjective impression of their health status, so correlation with PIC is expected. Strong association of PIC with changes in the mental SF-36 domains (VT and MH) is of particular interest. VT score is actually a measure of fatigue and was usually used to confirm validity of different fatigue scales [18]. Once again, our results reflect the importance of fatigue in CIDP. In addition, the previous studies underlined the association between a higher level of fatigue and lower SF-36 scores, where the strongest correlation was noted in SF-36 physical domains [9]. Thus, it seems that severe fatigue is one of the most significant predictors of a worse SF-36 score in patients with CIDP and, therefore, it should be adequately treated in order to improve patients’ QoL [3, 11, 20]. Considering a previous report on fatigue in different neuromuscular diseases, fatigue can be improved by treating the underlying condition only to a minor degree [21]. Many other items, that are related to and impact fatigue but are not specific to the disease in question, are known and include age, gender, pain, obstructive sleep apnea, poor sleep, hypersomnolence, depression, anxiety, personality type, use of different medications and life experiences [21]. Some of these factors can be modified and can improve the level of fatigue. Finally, we showed a clear influence of MH scale on patients’ impression of worsening. MH comprises questions on patients’ emotional state, including anxiety and depression symptoms. It means that a change in emotional status, not always related to CIDP itself, may influence patients’ subjective impression of CIDP worsening. These patients are usually not candidates for retreatment if objective CIDP measures are stable.
Conclusion
INCAT, PIC, and SF-36 are complementary outcome measures that provide neurologists with useful information. We propose the use of these scales in CIDP patients in everyday clinical practice with the aim of detecting worsening of the disease and/or of related symptoms on time.
Availability of data and materials
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
Change history
13 May 2021
A Correction to this paper has been published: https://doi.org/10.1007/s11136-021-02862-w
References
Van den Bergh, P. Y. K., Hadden, R. D. M., Bouche, P., Cornblath, D. R., Hahn, A., Illa, I., et al. (2010). European Federation of Neurological Societies/Peripheral Nerve Society Guideline on management of chronic inflammatory demyelinating polyradiculoneuropathy: Report of a joint task force of the European Federation of Neurological Societies and the Peripher. European Journal of Neurology, 17(3), 356–363.
Mayo, E. N. (2015). ISOQOL dictionary of quality of life and health outcomes measurement. International Society for Quality of Life Research.
Bozovic, I., Kacar, A., Peric, S., Nikolic, A., Bjelica, B., Cobeljic, M., et al. (2017). Quality of life predictors in patients with chronic inflammatory demyelinating polyradiculoneuropathy. Journal of Neurology, 264(12), 2481–2486.
Merkies, I. S., Schmitz, P. I., van der Meché, F. G., Samijn, J. P., van Doorn, P. A., & Inflammatory Neuropathy Cause and Treatment (INCAT) group. (2002). Quality of life complements traditional outcome measures in immune-mediated polyneuropathies. Neurology, 59(1), 84–91.
Harbo, T., Andersen, H., Overgaard, K., & Jakobsen, J. (2008). Muscle performance relates to physical function and quality of life in long-term chronic inflammatory demyelinating polyradiculoneuropathy. Journal of the Peripheral Nervous System, 13(3), 208–217.
Westblad, M. E., Forsberg, A., & Press, R. (2009). Disability and health status in patients with chronic inflammatory demyelinating polyneuropathy. Disability and Rehabilitation, 31(9), 720–725.
Erdmann, P. G., van Meeteren, N. L. U., Kalmijn, S., Wokke, J. H. J., Helders, P. J. M., & van den Berg, L. H. (2005). Functional health status of patients with chronic inflammatory neuropathies. Journal of the Peripheral Nervous System, 10(2), 181–189.
dos Santos, P. L., de Almeida-Ribeiro, G. A. N., Silva, D. M. D., Marques Junior, W., & Barreira, A. A. (2014). Chronic inflammatory demyelinating polyneuropathy: Quality of life, sociodemographic profile and physical complaints. Arquivos de Neuro-Psiquiatria, 72(3), 179–183.
Merkies, I. S. J., & Kieseier, B. C. (2016). Fatigue, pain, anxiety and depression in Guillain-Barré Syndrome and chronic inflammatory demyelinating polyradiculoneuropathy. European Neurology, 75(3–4), 199–206.
Goebel, A., Lecky, B., Smith, L. J., & Lunn, M. P. (2012). Pain intensity and distribution in chronic inflammatory demyelinating polyneuropathy. Muscle and Nerve, 46(2), 294–295.
Kacar, A., Bjelica, B., Bozovic, I., Peric, S., Nikolic, A., Cobeljic, M., et al. (2018). Neuromuscular disease-specific questionnaire to assess quality of life in patients with chronic inflammatory demyelinating polyradiculoneuropathy. Journal of the Peripheral Nervous System, 23(1), 11–16.
Merkies, I. S., Bril, V., Dalakas, M. C., Deng, C., Donofrio, P., Hanna, K., et al. (2009). Health-related quality-of-life improvements in CIDP with immune globulin IV 10%: The ICE Study. Neurology, 72(15), 1337–1344.
Kleyweg, R. P., van der Meché, F. G., & Schmitz, P. I. (1991). Interobserver agreement in the assessment of muscle strength and functional abilities in Guillain-Barré syndrome. Muscle and Nerve, 14(11), 1103–1109.
Breiner, A., Barnett, C., & Bril, V. (2014). INCAT disability score: A critical analysis of its measurement properties. Muscle and Nerve, 50(2), 164–169.
http://www.qualitymetric.com SF-36 Health Survey (Original version) Language Recalls.
Cohen, J. (1960). A coefficient of agreement for nominal scales. Educational and Psychological Measurement, 20, 37–46.
Bjelica, B., Peric, S., Bozovic, I., Kacar, A., Cobeljic, M., Dejanovic, I., et al. (2019). One-year follow-up study of neuropathic pain in chronic inflammatory demyelinating polyradiculoneuropathy. Journal of the Peripheral Nervous System, 24(2), 180–186.
Gable, K. L., Attarian, H., & Allen, J. A. (2020). Fatigue in chronic inflammatory demyelinating polyneuropathy. Muscle and Nerve. https://doi.org/10.1002/mus.27038.
Merkies, I. S. J., van Nes, S. I., Hanna, K., Hughes, R. A. C., & Deng, C. (2010). Confirming the efficacy of intravenous immunoglobulin in CIDP through minimum clinically important differences: Shifting from statistical significance to clinical relevance. Journal of Neurology, Neurosurgery and Psychiatry, 81(11), 1194–1199.
Lawley, A., Abbas, A., Seri, S., & Rajabally, Y. A. (2020). Clinical correlates of fatigue in chronic inflammatory demyelinating polyneuropathy. Muscle and Nerve, 62(2), 226–232.
Peric, S. Z., & Cornblath, D. R. (2020). Fatigue in chronic inflammatory demyelinating polyradiculoneuropathy. Muscle and Nerve. https://doi.org/10.1002/mus.27076.
Funding
This study was supported by the Ministry of Education, Science and Technological Development of Serbia (Grant #175083).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Ivo Bozovic, Marina Peric, Ivana Bulatovic, Ana Azanjac Arsic, Aleksa Palibrk, and Dejan Aleksic. The first draft of the manuscript was written by Stojan Peric and Ivo Bozovic, and all authors have commented on previous versions of the manuscript. The whole research was conceptualized and supervised by Ivo Bozovic, Stojan Peric, and Ivana Basta. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Consent for publication
Each author has read and approved the final manuscript version for submission.
Ethical approval
This research was approved by the Ethical Board of the Neurology Clinic, Clinical Center of Serbia.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: Affiliation number 3 is updated.
Rights and permissions
About this article
Cite this article
Bozovic, I., Peric, M., Arsic Azanjac, A. et al. Prospective analysis of disability and quality of life in patients with chronic inflammatory demyelinating polyradiculoneuropathy. Qual Life Res 30, 2573–2579 (2021). https://doi.org/10.1007/s11136-021-02838-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-021-02838-w