Abstract
Purpose
Previous studies have reported a positive association between poor health-related quality of life (HRQOL) and disability mainly in relation to the physical component of HRQOL. Given the mental component’s responsivity to interventions, this study aimed to investigate whether the mental component of HRQOL independently predicted functional disability.
Methods
We targeted all residents aged ≥ 65 years in one municipality and analyzed 3858 men and 4475 women without disability at baseline (November 2016). HRQOL was measured using the physical component summary (PCS) and mental component summary (MCS) of the SF-8 Health Survey. At 3-year follow-up (October 2019), incident functional disability was measured, defined as a new certification according to the Japanese long-term care insurance system. Multivariable Poisson regression models stratified by gender were used to estimate adjusted cumulative incidence ratio (CIR) and 95% confidence interval (CI) for functional disability.
Results
Among both genders, there was a significant dose-response relationship between better MCS and lower risk of functional disability, independent of potential confounders including the PCS (P for trend = 0.026 in men and 0.003 in women). Compared with the worst MCS group, the CIRs (95% CIs) for functional disability in the second worst, the middle, the second best, and the best MCS quintile groups were 1.09 (0.80–1.48), 0.58 (0.40–0.85), 0.90 (0.59–1.37), and 0.70 (0.48–1.02) for men, and 0.76 (0.58–1.00), 0.62 (0.46–0.84), 0.73 (0.53–0.99), and 0.63 (0.48–0.85) for women, respectively.
Conclusion
The MCS is an independent predictor of functional disability among high-functioning older adults. This suggests that strategies focused on mental HRQOL are important for realizing a healthy, long-lived society.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Plain English summary
Disability is considered to be a key dimension associated with a decrease in health-related quality of life, and some previous studies have reported a significant relationship between disability and health-related quality of life in older adults. However, a significant association is mainly explained by the physical component of health-related quality of life. Additionally, previous findings are unclear on causal relationships because of the cross-sectional nature.
In this study, we have found that the mental component of health-related quality of life at baseline independently predicts 3-year incidence of functional disability, even after adjusting for potential confounders including the physical component of health-related quality of life, regardless of gender. Our findings suggest that maintaining or improving the mental component of health-related quality of life is important for realizing a healthy and long-lived society.
Introduction
According to statistics released by the World Health Organization [1], life expectancy at birth of Japanese men and women in 2016 was 84.2 years, making it the longest lived country in the world. In addition, healthy life expectancy at birth, which is the average number of years that a person can expect to live in full health (that is, disability-free life expectancy), is 74.8 years old, which is the second longest in the world after Singapore.
In Japan, where the world’s highest average life expectancy has been achieved, it is important as a society to emphasize quality of life (QOL) and to ensure the population live in good health and independence, with the extended lifespan as a “period without physical and mental disabilities” [2]. As of 2016, the difference between average life expectancy and healthy life expectancy of Japanese people is about 10 years, and the larger this difference, the longer the period of disability in daily living becomes. It is expected that the burden of medical expenses and long-term care benefits will increase as the period of disability in daily living increases [2]. Especially in Japan, where the aging of the population is progressing rapidly, it is important to reduce this period of disability in daily living, not only to prevent deterioration of QOL and enable older people to live longer in the community, but also to ensure the sustainability of the social security system [3].
QOL is roughly divided into health-related QOL that is directly related to health and non-health-related QOL that is not directly related to health [4]. Fukuhara, a leading expert in QOL research in Japan, defines health-related QOL (HRQOL) as “a quantification of how diseases and treatments affect a patient’s subjective feelings of health (mental health, vitality, pain, etc.) and daily activities such as work, domestic duties, and social activities” [5]. HRQOL is a QOL that may be improved by medical intervention because it is a QOL affected by a disease or health condition [4, 5].
Disability is considered to be a key dimension associated with a decrease in HRQOL, and many studies have reported a significant relationship between disability and HRQOL in chronically ill patients [6, 7]. Later-life HRQOL has been shown to be significantly correlated with levels of functioning [8], disability in basic activities of daily living (BADL) and instrumental activities of daily living (IADL) [9], and frailty status [10], but these associations are mainly explained by the physical component of HRQOL (“physical HRQOL”) rather than the mental component of HRQOL (“mental HRQOL”). Additionally, previous findings are unclear regarding causal relationships because of the cross-sectional nature [6,7,8,9,10]. To the best of our knowledge, no population-based longitudinal cohort studies have examined whether mental HRQOL is an independent predictor of incident disability. According to previous studies of community-dwelling older people in Japan, functional capacity has significantly improved over the past two decades [11], and risk factors associated with poorer mental HRQOL have been reported to be reduced frequency of going outdoors [12], swallowing function deterioration [13], and long-lasting joint stiffness [14]. Recent studies in countries other than Japan have shown that mental HRQOL can be improved by increasing exercise frequency [15, 16], improving nutrition status [17], managing psychopathological disorders [18], reducing stress [19], or strengthening social support [8, 20]. Moreover, in comparison to physical HRQOL, mental HRQOL is less likely to be affected by aging and the existence of chronic diseases [6, 9, 10, 21]. Therefore, mental HRQOL of community-dwelling older adults is modifiable and preventable with appropriate interventions, suggesting that if an independent association between mental HRQOL and incident disability is found in this study, we can propose effective measures aimed at realizing a healthy and long-lived society.
This prospective cohort study aimed to investigate whether the mental HRQOL of community-dwelling older people without disability is a predictor of incident functional disability independently of potential cofounders including socio-economic status, health status, lifestyle habits, mental and physical functioning, and physical HRQOL. Since it has been indicated that there are gender differences in HRQOL [22,23,24,25] and incident disability [26], we performed stratified analyses by gender.
Methods
Study area and participants
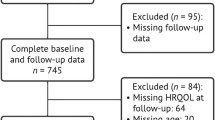
This was a prospective cohort study targeting all adults aged 65 and over living in one municipality. The study area was a commuter town in Nara Prefecture in Japan, with a lower population aging rate than the national average. As of November 30, 2016, the targeted municipality had a population of 78,987 and an aging population rate of 21.9% [27]. In November 2016, baseline questionnaires were distributed by mail to all residents aged 65 years or older (n = 16,010). A total of 10,009 persons returned the questionnaires (62.5%). We followed up the 8808 persons with valid responses for HRQOL who had not been certified as having functional disability by the public long-term care insurance (LTCI) system at baseline until October 2019. The final number of people who had no disability at baseline and could be followed up was 8333 (Fig. 1).
Measures
Health-related quality of life (HRQOL)
To measure HRQOL among participants in this study, we used the Japanese version [28] of the 8-item Short-Form Health Survey (SF-8) [29]. Scales for measuring HRQOL are broadly categorized into comprehensive and disease-specific scales [4, 5]. The SF-8 is positioned in the former. The comprehensive HRQOL scale assesses a general condition so that it can be applied to any disease. Given that most Japanese older people living in the community have some kind of chronic illness [11], the SF-8 is an appropriate scale for measuring the QOL of Japanese community-dwelling older adults, as it allows for comparison with other research results even if the diseases of the surveyed subjects are different [5].
The SF-8 is one of the shortened versions of the 36-item Short Form (SF-36) [30], the most popular comprehensive HRQOL scale in many countries around the world including Japan. The SF-8, like the SF-36, is a scale that can measure eight areas of health. Moreover, because the SF-8 is configured to score on the same metrics as the SF-36, the results obtained from the SF-8 and the SF-36 can be compared with each other [28, 29].
The SF-8 can measure subjective health status during the past month. Based on the manual of the SF-8 [28, 29], the SF-8 can yield two summary scores of the Physical Component Summary (PCS) and the Mental Component Summary (MCS). The norm-based scoring produces scores with a mean of 50 and a standard deviation of 10 for the 2017 Japanese population [28], with higher scores indicating better HRQOL. The validity and reliability of the Japanese version of the SF-8 have previously been investigated and proven to be valid and reliable for evaluating HRQOL in the general population and the chronically ill population [28, 31]. With the SF-36, it is not recommended to use two summary scores in Japan because Japan has a different factor structure from Europe and the United States [32]. In contrast, because it has been confirmed that the Japanese version of the SF-8 has the same factor structure as in western countries, we can use the PCS and the MCS of the Japanese population based on the SF-8 [28].
Incidence of functional disability
Incidence of functional disability was defined as first LTCI certification in Japan, which uses a uniform standard nationwide of functional disability. In order to obtain LTCI certification, it is necessary to have an assessment carried out by the Municipal Certification Committee, which is composed of academic experts in insurance, welfare, and medicine. Based on the physical and mental condition survey by the certified investigator and the opinion by the attending physician, the Municipal Certification Committee decides whether support or care is required, and categorizes nursing care needs according to a seven-grade system comprising support levels 1–2 and care levels 1–5 [33, 34]. Previous studies have demonstrated that the seven levels of LTCI certification are highly correlated with the Barthel Index (Spearman coefficient of -0.86) which is the most widely used BADL rating scale [35], and that a new LTCI certification is a valid measure of incident functional disability in Japanese older adults [36].
Covariates
Referring to prior studies [8,9,10, 22,23,24,25,26], the following variables were adopted as covariates which may correlate with mental HRQOL and functional disability: age (65–69, 70–74, 75–79, 80–84, or ≥ 85 years), marital status (married or unmarried), family size (living alone, 2, or ≥ 3 persons), years of education (≤ 9, 10–12, or ≥ 13 years), self-perceived economic status (rich, middle, or poor), working status (non-working or working), body mass index (BMI) (< 18.5, 18.5–24.9, or ≥ 25.0), number of chronic diseases under medical treatment (none, one, or ≥ 2), smoking (never-smokers, ex-smokers, or current smokers), frequency of alcohol intake (none, social/occasional, or almost daily), frequency of exercise (none, less than once a week, or ≥ 1 times a week), depression (absent or present), cognitive functioning (intact or poor), and IADL (good or poor). Because the PCS may be a potential confounder to assess the association between the MCS and functional disability [8,9,10], the PCS was used as an additional variable in the final model: the study participants were grouped by gender and quintile of the PCS score.
Chronic diseases included hypertension, stroke, heart disease, and diabetes. Depression was assessed using the 5-item short form of the Geriatric Depression Scale [37]. Cognitive functioning was assessed using the MDS Cognitive Performance Scale [38]. IADL was assessed using 5 items from the Tokyo Metropolitan Institute of Gerontology Index of Competence [39].
Statistical analysis
The Chi-square test or the Mann-Whitney test was used to examine the difference in categorical or continuous variables of baseline characteristics between groups. The Jonckheere-Terpstra test was used to examine the age distribution of PCS and MCS.
We used the generalized estimating equations of the multivariable Poisson regression model to calculate a cumulative incidence ratio (CIR) and a 95% confidence interval (CI) for incidence of functional disability. An exposure variable was the MCS at baseline; the participants were classified into quintiles according to their MCS score by gender. The analyses were performed according to gender. First, we calculated a crude CIR for incident functional disability (Model 1). Next, in Model 2, covariates included in the adjustment were socio-demographics (i.e., age, marital status, family size, education, self-perceived economic status, and working status), health status (i.e., BMI and chronic diseases), lifestyle habits (i.e., smoking, alcohol intake, and exercise), and mental and physical functioning (i.e., depression, cognitive functioning, and IADL). In the final Model 3, the PCS was added to the variables in Model 2. A test for linear trend was conducted to evaluate the dose-response relationship between levels of the MCS and incident functional disability.
To examine the effects of age, chronic diseases, depression, cognitive functioning, and IADL, we conducted additional stratified analyses based on aged 65–74 and aged ≥ 75, with or without chronic diseases, with or without depression, with or without poor cognition, and with or without poor IADL.
To deal with missing covariates, we conducted multiple imputations by chained equations implemented in IBM SPSS Missing Value Version 24. Multiple imputations are one of the recommended statistical methods [40]. The details of covariates including missing values are shown in Supplementary material Appendix A.
For the issue of multicollinearity, no variables with the variance inflation factor greater than 5.0 were found in all covariates.
Statistical analyses were carried out using the IBM SPSS Statistics Ver. 24 for Windows (Armonk, New York), and a significant level was set at 0.05 (two-tailed test).
Ethical issues
This study was approved by the Nara Medical University Ethics Committee (approval number 939). Submission of self-completed questionnaires was considered agreement to participate in the research.
Results
Basic attributes by the presence or absence of response or with or without follow-up
Non-respondents were more likely to have functional disability than respondents (Supplementary material Appendix B). Persons who were lost to follow-up were significantly older, tended to have poorer socio-economic status, poorer mental and physical functioning, and poorer HRQOL than those included in this study (Supplementary material Appendix C).
Characteristics of the study participants
Among the study participants (n = 8333), age at baseline averaged 73.3 (standard deviation, 5.9) years, median age was 72.0 years, age ranged from 65 to 98 years, and 46.3% were male. During the 3-year follow-up, the cumulative incidence of functional disability was 6.6% in men and 8.1% in women, showing a significant gender difference (P = 0.009 by the Chi-square test). Compared to people without incident functional disability, people with incident functional disability were associated with older age, female gender, unmarried, living alone, low education, non-working, abnormal BMI, never-smokers, non-drinkers, physically inactive, depression, poor cognition, poor IADL, and poor physical and mental components of HRQOL. Self-perceived economic status and chronic diseases did not exhibit significant difference between the two groups (Table 1).
PCS and MCS scores by gender and the five age groups
Among men, higher age was related to both the lower PCS score and the lower MCS score (P for trend < 0.001 in the PCS and P for trend = 0.018 in the MCS). Among women, older age was associated with poorer PCS (P for trend < 0.001), but the association between older age and poorer MCS was not significant (P for trend = 0.203). Among people aged 65–84, women were more likely to have poorer PCS than men. Among people aged 65–79, women were more likely to have poorer MCS than men (Fig. 2).
Box-and-whisker plot for physical and mental health component summary scores, by gender and 5-year age group. The x-axis indicates age groups. The y-axis indicates physical and mental health component summary scores based on the SF-8 as a measure of health-related quality of life. aA trend test was performed to detect the decreasing levels of health-related quality of life with increasing age group using the Jonckheere-Terpstra test. *P < 0.05 and **P < 0.001 based on the Mann-Whitney test which was used to compare medians between men and women within the same age group
Longitudinal association between the MCS and incident functional disability
Among men, in the crude model (Model 1), there was a significant dose-response relationship between better MCS and lower risk of incident functional disability (P for trend < 0.001), and the groups with the middle MCS quintile or better were associated with significantly lower risk of incident functional disability compared with the worst MCS quintile group. After adjustment for covariates (Model 2), the dose-response relationship remained significant (P for trend = 0.021), but a significant CIR was limited to the middle MCS quintile group. After additional adjustment for the PCS (Model 3), these associations remained basically unchanged: adjusted CIRs (95% CIs) for functional disability in the second worst, the middle, the second best, and the best quintile groups were 1.09 (0.80–1.48), 0.58 (0.40–0.85), 0.90 (0.59–1.37), and 0.70 (0.48–1.02), respectively, compared to the worst MCS quintile group (P for trend = 0.026).
Among women, after no adjustment (Model 1), a significant dose-response relationship was seen, with lower CIRs as the levels of the MCS increased (P for trend < 0.001), and the groups with the second worst MCS quintile or better were significantly associated with a reduced risk of developing functional disability. In Model 2, where the data were adjusted for covariates, these associations were attenuated, but the CIRs of the groups with the middle MCS quintile or better remained significant. In Model 3, additional adjustment for the PCS brought no change in significant associations: adjusted CIRs (95% CIs) for functional disability in the second worst, the middle, the second best, and the best quintile groups were 0.76 (0.58–1.00), 0.62 (0.46–0.84), 0.73 (0.53–0.99), and 0.63 (0.48–0.85), respectively, compared to the worst MCS quintile group (P for trend = 0.003) (Table 2).
Additional stratified analyses
A significant association between better MCS and lower prevalence of incident functional disability was observed regardless of age or chronic diseases. In contrast, a significant dose-response relationship was shown among people with no depression, those with intact cognition, or those with good IADL, but not among people with depression, those with poor cognition, or those with poor IADL (Supplementary material Appendix D).
Discussion
Our study has two main findings. First, the MCS at baseline independently predicted 3-year incidence of functional disability, even after adjusting for potential confounders including the PCS, consistently for both men and women. To our knowledge, this is the first prospective cohort study to show that the mental component of HRQOL is independently associated with incident functional disability. Second, among men, not only the PCS, but also the MCS decreased with age. Among women, older age was associated with poorer PCS, but had no association with poorer MCS.
As far as we know, this is the first study to indicate a longitudinal association between mental HRQOL and disability, but three longitudinal studies reported a significant association between a QOL measure close to the concept of mental HRQOL and functional disability; our study is partly consistent with these findings. The first study by Boyle et al. addressed the effect of purpose in life on incident disability in 970 persons aged 54–100 without dementia in the Chicago metropolitan area [41]. They found that greater purpose in life was associated with a lower risk of developing impairment in BADL and IADL. The second study by Steptoe et al. addressed the effect of enjoyment of life on physical function in 3199 men and women aged ≥ 60 in England [42]. They found that greater enjoyment of life was associated with a reduced risk of developing impaired BADL. The third study by Palgi et al. addressed the effect of needs-satisfaction-driven QOL on functional disability in 18,781 European adults aged ≥ 50 from 19 countries [43]. They found that persons with higher QOL at baseline had lower age-related decline in BADL and IADL than those with lower QOL at baseline. These previous reports suggest that positive psychological well-being may be an important predictor of maintenance of functional capacity in old age.
Regarding age distribution of HRQOL, we found that the median PCS score decreased with age, regardless of gender. However, an association between older age and poorer MCS was significant only in men, but not in women. Our results for the MCS are inconsistent with previous research, in which older age was negatively associated with the PCS, but positively associated with the MCS for both men and women [23, 24]. The findings of previous studies have a high possibility of selection bias; because the study subjects included active older adults who were willing to participate in the study, they might have had a relatively higher level of mental HRQOL than the general population of older people.
In relation to gender differences, our study has found that on the whole, PCS and MCS scores were lower in women than in men within the same age group, which is consistent with previous studies [23, 25, 31, 44]. We have also reported that women have a higher risk of incident functional disability than men, which is consistent with previous studies [36, 41]. On the other hand, we found a significant association between the MCS and incident functional disability in both genders, suggesting that gender has no significant effect on the MCS-disability association. Our results based on additional stratified analyses showed the MCS-disability association was affected by neither age nor chronic diseases, but was significant among people with good mental and physical functioning. Our results are partly consistent with a prior European study of community-dwelling older adults [20], which found that the association of BADL and IADL disabilities with QOL was stronger in persons without depression compared to those with depression. Our findings suggest that the association between the MCS and incident functional disability is more strongly influenced by mental and physical functioning than gender.
We have two potential mechanisms for the association between the MCS and incident functional disability. First, previous studies examined the association between inflammation and HRQOL. Some investigations found that lower HRQOL in the mental domain was associated with elevated C-reactive protein (CRP) serum levels [45, 46]. Because inflammatory biomarkers such as CRP are associated with disability in older persons [47], mental HRQOL may have a beneficial effect in the prevention of disability via inflammatory pathways. Second, stress buffering is also considered a pathway to the preservation of functional capacity. A prior study reported that perceived stress symptoms were associated with the development of functional disability in later life [48]. There is also some evidence that an individual coping resource such as mindfulness [49] and resilience [50] is positively related to mental HRQOL, and may attenuate the negative effects of perceived stress on mental HRQOL. Older adults with higher mental HRQOL may have more protection against functional decline due to stressful experiences through the availability of stress coping resources, resulting in the maintenance of functional capacity.
Regarding the implications of this study, our findings suggest that the MCS can be an effective tool for identifying older people at future risk of functional disability. General practitioners should therefore check the mental HRQOL of older patients in order to prevent functional disability. Policymakers should be aware that measures to maintain and improve the mental HRQOL of community-dwelling older adults are important for the realization of a healthy and long-lived society.
The strengths of this study include that it was a community-based prospective study, had a high follow-up rate (94.6%) and a large sample size, and used valid instruments for assessing HRQOL and functional disability. However, it has some limitations. First, there was an insufficient collection rate of 62.5%. In this study, non-respondents had poorer functional status than respondents. Additionally, persons with loss to follow-up had poorer HRQOL than the study participants. Therefore, there is a possibility that community-dwelling older adults at high risk of developing functional disability were excluded from our study. This may have led to an underestimation in the MCS-disability association. Second, we evaluated HRQOL only at baseline, and have not accounted for the effects of changes in MCS. A previous study has demonstrated that HRQOL undergoes change and the SF-8 can be used to assess change in MCS over time or by intervention [51]. Future research should consider change in mental HRQOL. Third, compared to the SF-36, the SF-8 is more suitable for large-scale surveys because of its simplicity. However, the score obtained from the SF-8 can only be measured in a narrower range, and its disadvantage is that it is less accurate than the SF-36 [28, 29]. Our findings need to be confirmed by using the SF-36. Finally, although we had enough adjustment for potential cofounders, this study may have residual confounding that influences the association between the MCS and functional disability. For example, a recent study has indicated that energy balance such as total energy expenditure and energy intake may influence the MCS-disability association [52], suggesting that the observed associations might have been changed by additional adjustment for energy balance.
Conclusion
The present study provides evidence that mental HRQOL is an independent predictor for functional disability among non-disabled community-dwelling older adults, independent of gender, socio-economic status, health status, lifestyle habits, mental and physical functioning, and physical HRQOL. Our findings suggest that taking measures focused on the improvement of mental HRQOL leads to the prevention of functional disability among community-dwelling older adults, that is, to the extension of healthy life expectancy. Although the MCS may be an effective tool for identifying older people who are at risk of developing functional disability, future studies should consider change in the MCS, the use of the SF-36, and the possibility of residual confounding, in order to confirm the observed associations.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
World Health Organization. (2018). World health statistics 2018: Monitoring health for the SDGs, sustainable development goals. Geneva: WHO.
Ministry of Health, Labour and Welfare of Japan. (2014). Annual health, labour and welfare report 2014. For the realization of a Society of Health and Longevity. Tokyo: Ministry of Health, Labour and Welfare of Japan.
Cabinet Office Japan. (2017). Annual report on the Ageing Society 2017. The state of ageing and implementation of the measures for the Ageing Society. Tokyo: Cabinet Office Japan.
Doi, Y. (2004). Introduction-conceptual issues on quality of life (QOL) and importance of QOL research. Journal of the National Institute of Public Health, 53(3), 176–180. (in Japanese).
Fukuhara, S. (2002). QOL assessment and epidemiology for clinical practice. Journal of Japanese Society of Lumbar Spine Disorders, 8(1), 31–37. https://doi.org/10.3753/yotsu.8.31.
Jarl, J., Alriksson-Schmidt, A., & Rodby-Bousquet, E. (2019). Health-related quality of life in adults with cerebral palsy living in Sweden and relation to demographic and disability-specific factors. Disability and Health Journal, 12(3), 460–466.
Zhou, Y., Wang, X., An, Y., Zhang, X., Han, S., Li, X., et al. (2018). Disability and health-related quality of life in Chinese patients with rheumatoid arthritis: A cross-sectional study. International Journal of Rheumatic diseases, 21(9), 1709–1715.
Grassi, L., Caruso, R., Da Ronch, C., Härter, M., Schulz, H., Volkert, J., et al. (2020). Quality of life, level of functioning, and its relationship with mental and physical disorders in the elderly: Results from the MentDis_ICF65+ study. Health and Quality of Life Outcomes, 18(1), 61.
Gobbens, R. J. (2018). Associations of ADL and IADL disability with physical and mental dimensions of quality of life in people aged 75 years and older. PeerJ, 6, e5425.
Lin, C. C., Li, C. I., Chang, C. K., Liu, C. S., Lin, C. H., Meng, N. H., et al. (2011). Reduced health-related quality of life in elders with frailty: A cross-sectional study of community-dwelling elders in Taiwan. PLoS ONE, 6(7), e21841.
Suzuki, T. (2018). Health status of older adults living in the community in Japan: Recent changes and significance in the super-aged society. Geriatrics & Gerontology International, 18(5), 667–677.
Harada, K., Masumoto, K., Katagiri, K., Fukuzawa, A., Chogahara, M., et al. (2018). Frequency of going outdoors and health-related quality of life among older adults: Examining the moderating role of living alone and employment status. Geriatrics & Gerontology International, 18(4), 640–647.
Morisaki, N. (2017). Relationship between swallowing functions and health-related quality of life among community-dwelling dependent older individuals. Japan Journal of Nursing Science, 14(4), 353–363.
Murata, S., Doi, T., Sawa, R., Saito, T., Nakamura, R., et al. (2017). Association between joint stiffness and health-related quality of life in community-dwelling older adults. Archives of Gerontology and Geriatrics, 73, 234–239.
Kell, K. P., & Rula, E. Y. (2019). Increasing exercise frequency is associated with health and quality-of-life benefits for older adults. Quality of Life Research, 28(12), 3267–3272.
von Berens, Å., Fielding, R. A., Gustafsson, T., Kirn, D., Laussen, J., Nydahl, M., et al. (2018). Effect of exercise and nutritional supplementation on health-related quality of life and mood in older adults: The VIVE2 randomized controlled trial. BMC Geriatrics, 18(1), 286.
Tek, N. A., & Karaçil-Ermumcu, M. Ş. (2018). Determinants of health related quality of life in home dwelling elderly population: Appetite and nutritional status. Journal of Nutrition, Health, & Aging, 22(8), 996–1002.
Blanco-Reina, E., Valdellós, J., Ocaña-Riola, R., García-Merino, M. R., Aguilar-Cano, L., et al. (2019). Factors associated with health-related quality of life in community-dwelling older adults: A multinomial logistic analysis. Journal of Clinical Medicine, 8(11), 1810. https://doi.org/10.3390/jcm8111810.
Chen, M. L., Hu, J., McCoy, T. P., Letvak, S., & Ivanov, L. (2018). Effect of a lifestyle-based intervention on health-related quality of life in older adults with hypertension. Journal of Aging Research, 2018, 6059560.
Puvill, T., Kusumastuti, S., Lund, R., Mortensen, E. L., Slaets, J., Lindenberg, J., et al. (2019). Do psychosocial factors modify the negative association between disability and life satisfaction in old age? PLoS ONE, 14(10), e0224421.
Tomioka, K., Kurumatani, N., & Hosoi, H. (2017). Positive and negative influences of social participation on physical and mental health among community-dwelling elderly aged 65–70 years: A cross-sectional study in Japan. BMC Geriatrics, 17(1), 111.
Assari, S., Smith, J., & Bazargan, M. (2019). Health-related quality of life of economically disadvantaged african american older adults: Age and gender differences. International Journal of Environmental Research and Public Health, 16(9), 1522.
Nezu, S., Okamoto, N., Morikawa, M., Saeki, K., Obayashi, K., Tomioka, K., et al. (2014). Health-related quality of life (HRQOL) decreases independently of chronic conditions and geriatric syndromes in older adults with diabetes: The Fujiwara-kyo study. Journal of Epidemiology, 24(4), 259–266.
Tseng, H. Y., Löckenhoff, C., Lee, C. Y., Yu, S. H., Wu, I. C., Chang, H. Y., et al. (2020). The paradox of aging and health-related quality of life in Asian Chinese: Results from the Healthy Aging Longitudinal Study in Taiwan. BMC Geriatrics, 20(1), 91.
Hajian-Tilaki, K., Heidari, B., & Hajian-Tilaki, A. (2017). Are gender differences in health-related quality of life attributable to sociodemographic characteristics and chronic disease conditions in elderly people? International Journal of Preventive Medicine, 8, 95.
Pongiglione, B., De Stavola, B. L., Kuper, H., & Ploubidis, G. B. (2016). Disability and all-cause mortality in the older population: Evidence from the English Longitudinal Study of Ageing. European Journal of Epidemiology, 31(8), 735–746.
Tomioka, K., Kurumatani, N., & Saeki, K. (2019). Cross-sectional association between types of leisure activities and self-rated health according to gender and work status among older Japanese adults. Journal of Epidemiology, 29(11), 424–431.
Fukuhara, S., & Suzukamo, Y. (2019). Manual of the SF-8 Japanese version. Kyoto: iHope International Incorporated.
Ware, J. E., Jr., Kosinski, M., Dewey, J. E., & Gandek, B. (2001). How to score and interpret single-item health status measures: A manual for users of the SF-8 health survey. Lincoln, RI: QualityMetric Incorporated.
Ware, J. E., Jr., & Sherbourne, C. D. (1992). The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Medical Care, 30(6), 473–483.
Tokuda, Y., Okubo, T., Ohde, S., Jacobs, J., Takahashi, O., Omata, F., et al. (2009). Assessing items on the SF-8 Japanese version for health-related quality of life: A psychometric analysis based on the nominal categories model of item response theory. Value in Health, 12(4), 568–573.
Fukuhara, S., Ware, J. E., Jr., Kosinski, M., Wada, S., & Gandek, B. (1998). Psychometric and clinical tests of validity of the Japanese SF-36 Health Survey. Journal of Clinical Epidemiology, 51(11), 1045–1053.
Tsutsui, T., & Muramatsu, N. (2005). Care-needs certification in the long-term care insurance system of Japan. Journal of the American Geriatrics Society, 53(3), 522–527.
Moriyama, Y., Tamiya, N., Kamimura, A., Sandoval, F., & Luptak, M. (2014). Doctors’ Opinion Papers in Long-term Care Need certification in Japan: Comparison between clinic and advanced treatment hospital settings. Public Policy and Administration Research, 4(9), 31–37.
Arai, Y., Zarit, S. H., Kumamoto, K., & Takeda, A. (2003). Are there inequities in the assessment of dementia under Japan’s LTC insurance system? International Journal of Geriatric Psychiatry, 18(4), 346–352.
Ashida, T., Kondo, N., & Kondo, K. (2016). Social participation and the onset of functional disability by socioeconomic status and activity type: The JAGES cohort study. Preventive Medicine, 89, 121–128.
Hoyl, M. T., Alessi, C. A., Harker, J. O., Josephson, K. R., Pietruszka, F. M., Koelfgen, M., et al. (1999). Development and testing of a five-item version of the Geriatric Depression Scale. Journal of the American Geriatrics Society, 47(7), 873–878.
Morris, J. N., Fries, B. E., Mehr, D. R., Hawes, C., Phillips, C., Mor, V., et al. (1994). MDS cognitive performance scale. Journal of Gerontology, 49(4), M174–M182.
Koyano, W., Shibata, H., Nakazato, K., Haga, H., & Suyama, Y. (1991). Measurement of competence: Reliability and validity of the TMIG index of competence. Archives of Gerontology and Geriatrics, 13(2), 103–116.
Azur, M. J., Stuart, E. A., Frangakis, C., & Leaf, P. J. (2011). Multiple imputation by chained equations: What is it and how does it work? International Journal of Methods in Psychiatric Research, 20(1), 40–49.
Boyle, P. A., Buchman, A. S., & Bennett, D. A. (2010). Purpose in life is associated with a reduced risk of incident disability among community-dwelling older persons. American Journal of Geriatric Psychiatry, 18(12), 1093–1102.
Steptoe, A., de Oliveira, C., Demakakos, P., & Zaninotto, P. (2014). Enjoyment of life and declining physical function at older ages: A longitudinal cohort study. Canadian Medical Association Journal, 186(4), E150–E156.
Palgi, Y., Shrira, A., & Zaslavsky, O. (2015). Quality of life attenuates age-related decline in functional status of older adults. Quality of Life Research, 24(8), 1835–1843.
Liu, C. C., Chang, H. T., Chiang, S. C., Lin, M. H., Chen, T. J., et al. (2018). Sex differences in relationships between metabolic syndrome components and factors associated with health-related quality of life in middle-aged adults living in the community: A cross-sectional study in Taiwan. Health and Quality of Life Outcomes, 16(1), 76.
Sabour, H., Latifi, S., Soltani, Z., Shakeri, H., Javidan, A. N., Ghodsi, S. M., et al. (2017). C-reactive protein as an available biomarker determining mental component of health-related quality of life among individuals with spinal cord injury. Journal of Spinal Cord Medicine, 40(3), 329–337.
Wilkins, J., Ghosh, P., Vivar, J., Chakraborty, B., & Ghosh, S. (2018). Exploring the associations between systemic inflammation, obesity and healthy days: A health related quality of life (HRQOL) analysis of NHANES 2005–2008. BMC Obesity, 5, 21.
Davillas, A., & Pudney, S. (2020). Biomarkers as precursors of disability. Economics and Human Biology, 36, 100814.
Kulmala, J., von Bonsdorff, M. B., Stenholm, S., Törmäkangas, T., von Bonsdorff, M. E., Nygård, C. H., et al. (2013). Perceived stress symptoms in midlife predict disability in old age: A 28-year prospective cohort study. Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, 68(8), 984–991.
De Frias, C. M., & Whyne, E. (2015). Stress on health-related quality of life in older adults: The protective nature of mindfulness. Aging and Mental Health, 19(3), 201–206.
Kirchberger, I., Burkhardt, K., Heier, M., Thilo, C., & Meisinger, C. (2020). Resilience is strongly associated with health-related quality of life but does not buffer work-related stress in employed persons 1 year after acute myocardial infarction. Quality of Life Research, 29(2), 391–401.
Lefante, J. J., Harmon, G. N., Ashby, K. M., Barnard, D., & Webber, L. S. (2005). Use of the SF-8 to assess health-related quality of life for a chronically ill, low-income population participating in the Central Louisiana Medication Access Program (CMAP). Quality of Life Research, 14(3), 665–673.
Condello, G., Capranica, L., Migliaccio, S., Forte, R., Baldassarre, A. D., & Pesce, C. (2019). Energy balance and active lifestyle: Potential mediators of health and quality of life perception in aging. Nutrients, 11(9), 2122.
Acknowledgements
This work was supported by JSPS KAKENHI Grant Number JP17K09209 and the Center Administrative Expense from Nara Medical University. We wish to thank the participants of this study and support staff who make the study possible. We also thank Dr. Heather Hill for her English language editing.
Funding
This work was supported by JSPS KAKENHI Grant Number JP17K09209 and the Center Administrative Expense from Nara Medical University.
Author information
Authors and Affiliations
Contributions
Study concept and design: KT and MS. Acquisition of subjects and data and preparation of manuscript: All authors. Analysis and interpretation of data: KT and KS.
Corresponding author
Ethics declarations
Conflict of interest
KS received research grants from YKK AP Inc.; Ushio Inc.; Tokyo Electric Power Company; EnviroLife Research Institute Co., Ltd.; Sekisui Chemical Co., Ltd.; LIXIL Corp.; and KYOCERA Corp. This does not alter our adherence to the Quality of Life Research’s policies on sharing data and materials. For the remaining authors, none were declared.
Consent to participate
Submission of self-completed questionnaires was considered agreement to participate in the research.
Ethical approval
This study was approved by the Nara Medical University Ethics Committee (Approval No. 939).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Tomioka, K., Shima, M. & Saeki, K. Mental component of health-related quality of life is an independent predictor of incident functional disability among community-dwelling older people: a prospective cohort study. Qual Life Res 30, 1853–1862 (2021). https://doi.org/10.1007/s11136-021-02780-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-021-02780-x