Abstract
Background
Older persons with atrial fibrillation (AF) experience significant impairment in quality of life (QoL), which may be partly attributable to their comorbid diseases. A greater understanding of the impact of comorbidities on QoL could optimize patient-centered care among older persons with AF.
Objective
To assess impairment in disease-specific QoL due to comorbid conditions in older adults with AF.
Methods
Patients aged ≥ 65 years diagnosed with AF were recruited from five medical centers in Massachusetts and Georgia between 2015 and 2018. At 1 year of follow-up, the Quality of Life Disease Impact Scale—for Multiple Chronic Conditions was used to provide standardized assessment of patient self-reported impairment in QoL attributable to 34 comorbid conditions grouped in 10 clusters.
Results
The mean age of study participants (n = 1097) was 75 years and 48% were women. Overall, cardiometabolic, musculoskeletal, and pulmonary conditions were the most prevalent comorbidity clusters. A high proportion of participants (82%) reported that musculoskeletal conditions exerted the greatest impact on their QoL. Men were more likely than women to report that osteoarthritis and stroke severely impacted their QoL. Patients aged < 75 years were more likely to report that obesity, hip/knee joint problems, and fibromyalgia extremely impacted their QoL than older participants.
Conclusions
Among older persons with AF, while cardiometabolic diseases were highly prevalent, musculoskeletal conditions exerted the greatest impact on patients’ disease-specific QoL. Understanding the extent of impairment in QoL due to underlying comorbidities provides an opportunity to develop interventions targeted at diseases that may cause significant impairment in QoL.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Atrial fibrillation (AF) is the most prevalent cardiac arrhythmia in patients 65 years and older [1]. With advancing age, the prevalence of AF increases and may coexist with other chronic conditions, leading to greater disease burden and deleterious impact on patients’ quality of life (QoL) [2, 3]. Patient-reported QoL is an important aspect in the management of cardiovascular diseases which incorporates aspects of one’s physical, mental, and social well-being, and has been identified as a sensitive outcome of treatment strategies [4, 5]. Attaining and maintaining optimal QoL is increasingly being targeted in current AF management guidelines [6].
Cardiometabolic and non-cardiometabolic comorbid conditions are prevalent among older men and women with AF [7,8,9]. These chronic conditions may exert a profound negative effect on patients’ experience of their AF symptoms, hinder the adoption of recommended lifestyle changes and medication adherence, and one’s ability to engage in their healthcare, which could impact overall well-being and QoL. Although previous studies have examined the burden of comorbidities and their impact on overall/generic health-related QoL in patients with AF [9,10,11], no prior study has examined the extent to which comorbid conditions may cause impairment in disease-specific QoL among older men and women with AF. Since disease-specific measures focus on the impact of specific conditions on QoL, they provide more clinical utility and granularity than generic measures that do not focus on the impact of specific disease conditions on QoL [12]. In the present study, disease-specific QoL refers to the impact of each comorbid condition on patient’s QoL.
Understanding the extent of impairment in QoL due to underlying comorbid conditions provides an important and readily identifiable opportunity to address patients’ concerns about the consequences and management of their multiple chronic diseases. The objectives of the present observational study were to examine the prevalence of self-reported comorbid conditions among older men and women with AF, utilize standardized comparisons of the impact of these comorbid conditions on disease-specific QoL, and explore possible age and sex differences in QoL impairment due to comorbid diseases.
Methods
Study population
This investigation used data from the Systematic Assessment of Geriatric Elements in AF (SAGE-AF), a prospective multi-center study [13, 14]. In brief, study participants were recruited from one of four clinical sites in Central Massachusetts (University of Massachusetts Memorial Health Care internal medicine, cardiology, electrophysiology, or Heart Rhythm Associates of Central MA), one clinical site in Eastern Massachusetts (Boston University cardiology), or one of two practices in Central Georgia (Family Health Center and Georgia Arrhythmia Consultants) between 2015 and 2018. Patients were eligible for study enrollment if they were aged 65 years or older and were diagnosed with AF based on the presence of this arrhythmia on electrocardiography tracings, a Holter monitor, or the documentation of AF in hospital or clinic medical records. The present study was approved by Institutional Review Boards at participating study sites. Prior to formal study enrollment, each eligible participant provided written informed consent. Trained research personnel conducted face-to-face or telephone interviews with each study participant and abstracted data from hospital medical records at baseline and at one-year of follow-up.
Prevalence of comorbid conditions and assessment of disease-specific quality of life
We assessed the prevalence of comorbid conditions and the extent of Impairment in QoL attributable to each comorbidity based on patient self-reports using the validated and standardized Quality of Life Disease Impact Scale–Multiple Chronic Conditions form (QDIS-MCC) [12, 15] at the one-year study follow-up. The QDIS-MCC was developed from a Computerized Adaptive Assessment of Disease Impact (DICAT) project supported by the National Institutes of Health with the goal of generating a more comprehensive patient-reported outcome measure of which content and scoring could be standardized for comparison across different disease conditions. The QDIS-MCC includes a 34-condition checklist and a follow-up question for each condition checked. First, study participants were asked “Have you ever been told by a doctor or other health professional that you had any of the following conditions?”. Those who responded affirmatively were then queried as “In the past 4 weeks, how often did [CONDITION] limit your everyday activities or your quality of life?” with five response options on a Likert scale (0–5): “Not at all”, “A little”, “Some”, “A lot”, or “Extremely” [12, 15]. For purposes of analysis, responses of “A little” or “Some” were combined as a single category as were responses of “A lot” or “Extremely”. This QDIS-MCC measure has been shown to correlate highly with the score for a full bank of items for each condition and to discriminate among them in the presence of comorbid conditions [16].
From a clinical perspective, to better understand the impact of the 34 chronic conditions examined on patients’ QoL, we categorized these conditions into 10 major clusters as follows: Cardiometabolic, Musculoskeletal/Rheumatologic, Pulmonary, Gastrointestinal, Neuro-Psychiatric, Urologic/Nephrology, Hematologic-Oncologic/Infectious, Geriatric, Endocrine, and Dermatologic. Seven cardiometabolic conditions were assessed including hypertension, diabetes mellitus, obesity, heart failure, stroke, angina, and myocardial infarction. The eight musculoskeletal/rheumatologic conditions assessed were osteoarthritis, hip/knee joint problems, sciatica/chronic back pain, foot/ankle joint problems, rheumatoid arthritis, osteoporosis, fibromyalgia, and extremity weakness. Four pulmonary diseases were assessed and included seasonal allergies (hay fever), chronic allergies (sinusitis), asthma, and chronic obstructive pulmonary disease (COPD). Three gastrointestinal diseases were assessed including inflammatory bowel diseases, ulcer, and liver infection. Three neuro-psychiatric conditions were assessed including migraine, depression, and chronic fatigue syndrome. Three hematologic-oncologic and infectious disease were assessed including all cancers, anemia, and HIV. The two urologic/nephrology conditions assessed included kidney disease and benign prostatic hyperplasia, while the two geriatric conditions assessed were vision and hearing problems. The single endocrine disorder assessed was hypothyroidism and the sole dermatologic condition assessed was dermatitis/chronic skin problem.
Participant characteristics
Participants’ sociodemographic, psychosocial, clinical, and health behavior measures were assessed at baseline. Sociodemographic characteristics included the patient’s age, sex, race/ethnicity, marital status, and highest level of education attained. Psychological and social variables were obtained from comprehensive structured interviews including measures of social support, cognitive impairment, anxiety, and independent functioning. Social support was assessed with 5 items from the Medical Outcomes Social Support Survey Instrument that represent multiple dimensions of support including: emotional/informational, tangible, affectionate, and positive social interaction [17]. Participant cognition was assessed using the 30-item Montreal Cognitive Assessment Battery (MoCA) designed for use in healthcare settings to detect mild cognitive impairment [18, 19]. The MoCA is a validated 30-item screening tool that examines global cognitive function with assessments for attention, concentration, executive function, working memory, orientation, and visuospatial ability [18]. Scores range from 0 to 30 with lower scores indicating poorer performance and a cutoff of ≤ 23 suggestive of cognitive impairment [18, 19]. Symptoms of anxiety were measured using the 7-item Generalized Anxiety Disorder (GAD-7) questionnaire with scores ranging from 0 to 21, and study participants were designated as having no (≤ 4), mild (5–9), or moderate-to-severe (≥ 10) anxiety symptoms [20]. Independence was examined with the instrumental activities of daily living including basic communication skills, transportation, meal preparation, shopping, housework, and managing medications and personal finances [21]. Detailed clinical variables retrieved from patient medical records included type of AF (paroxysmal, persistent, and permanent), time since AF diagnosis, receipt of ablation therapy, anticoagulation therapy (direct oral anticoagulants or warfarin), polypharmacy (≥ 5 medications) and calculated risk scores such as the CHA2DS2-VASc for stroke risk [22], HASBLED for 1-year risk of major bleeding [22], and Charlson Comorbidity index [23]. Participant health behaviors included self-reports of smoking history and alcohol use.
Statistical analysis
We described participant’s baseline characteristics with continuous variables summarized as means and standard deviations when normally distributed and as medians and interquartile ranges (IQR) when skewed; categorical variables were described as proportions. Chi-square tests were used to compare significant differences in proportion for categorical variables.
As previously described, the prevalence of previously diagnosed comorbid conditions was assessed according to 10 clusters (Cardiometabolic, Musculoskeletal/Rheumatologic, Pulmonary, Gastrointestinal, Neuro-Psychiatric, Urologic/Nephrology, Hematologic-Oncologic/Infectious Disease, Geriatric, Endocrine, and Dermatologic). The disease clusters were not mutually exclusive as participants were assigned to any one of the clusters if they had at least one of the listed comorbid condition within that cluster. In the coding structure for the clusters, participants were assigned a “1” for the presence of any underlying comorbid condition within a specified cluster or a “0” otherwise. We examined the proportion of participants reporting the impact of each specific comorbid condition on their QoL as either “Not at all”, “A little/Some”, or “A lot or Extremely”, respectively. In examining the extent of the impact of each disease cluster on QoL, we assessed the proportion of participants reporting that either none of the comorbid conditions impacted their QoL or that at least one or more of the comorbid condition had “a little/some” or “a lot/extreme” impact on their QoL.
For the most prevalent disease clusters, we conducted stratified analyses by age (< 75 years and ≥ 75 years) and sex to examine potential subgroup differences in the impact of the comorbid conditions on QoL. Prevalent disease clusters were defined as clusters with one or more comorbid conditions present in at least 30% of the study participants, to ensure large enough sample sizes to detect between group differences for the proposed stratified analyses. The Cochran–Armitage test for trend across the self-reported levels of impairment in disease-specific QoL was used for respective age and sex group comparisons. The level of statistical significance (alpha) was set at 0.05. All analyses were done using STATA 16 (StataCorp. 2019. Stata Statistical Software: Release 16. College Station, TX: StataCorp LLC).
Results
Participant baseline characteristics
The mean age of study participants (n = 1097) was 75 years (SD 7.0), 48% were women, and 87% were White. The average time since the diagnosis of AF was 5.3 years (SD 4.3). Approximately one-third of participants reported experiencing symptoms of AF in the four weeks prior to study enrollment, and two-thirds were on rhythm control therapy. A majority (95%) were prescribed 5 or more medications. The mean Charlson comorbidity index score was 6.0 (SD 2.6). Approximately one-quarter of patients reported low social support, one-third had cognitive impairment, and 14% were frail. A majority of our study participants (77%) had no symptoms of anxiety, 18% had mild symptoms of anxiety, and 5% had moderate/severe symptoms of anxiety (Table 1).
Prevalence of comorbid conditions and impact on disease-specific quality of life
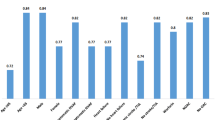
Overall, participants reported a median of 5 (IQR 2–8) comorbid conditions. The response rate among eligible patients at one of year of study follow-up was 87% (Of the 1097 study participants at 1 year of follow-up, 951 responded to the QDIS-MCC questionnaire). The most prevalent comorbidity clusters were cardiometabolic, musculoskeletal, and pulmonary diseases (Table 2). Commonly occurring cardiometabolic conditions included hypertension (63%), diabetes mellitus (23%), and obesity (24%). The most common musculoskeletal conditions were osteoarthritis (33%), hip/knee joint problems (32%), and sciatica/chronic back pain (29%). The commonly reported pulmonary diseases included seasonal allergies/hay fever (32%), chronic allergies/sinusitis (17%), and asthma (11%). Overall, a high proportion of participants (82%) reported that musculoskeletal conditions exerted an extreme impact on their disease-specific QoL, while cardiometabolic diseases had a less severe impact on disease-specific QoL. Other conditions with low prevalence including chronic fatigue syndrome (3%) and depression (6%) exerted a moderate-to-severe impact on patients’ QoL (Fig. 1).
Results from the stratified analysis showed that although women had a higher prevalence of osteoarthritis (49% vs 29%; p value < 0.001) and stroke (13% vs 8%; p value = 0.02) than men, men were more likely than women to report that osteoarthritis (27.4% vs 17.6%; p for trend = 0.01) and stroke (22.5% vs 3.6%; p for trend = 0.02) severely impacted their QoL (Table 2). Participants aged < 75 years had a higher prevalence of obesity (32.3% vs 21.9%; p value < 0.001), diabetes mellitus (31.8% vs 21.9%; p value = 0.001), and angina (7.7% vs 3.2%; p value = 0.002) compared to those 75 years and older. A greater proportion of participants aged < 75 years were more likely to report that obesity (19.1% vs 7.2%; p for trend = 0.004), hip/knee joint problems (34.0% vs 20.0%; p for trend = 0.002), and fibromyalgia (41.2% vs 7.7%; p for trend = 0.004) severely impacted their QoL in comparison with much older (≥ 75 years) participants (Table 3). There were no significant differences in QoL impairment by sex and age stratified analysis for the other prevalent comorbid conditions (Tables 2 and 3).
Discussion
In this cohort of older men and women with AF, approximately one-half reported having 5 or more comorbid conditions, with the most prevalent comorbidities being cardiometabolic, musculoskeletal conditions, and pulmonary diseases. Among the commonly reported conditions, a greater proportion of participants reported that musculoskeletal conditions such as osteoarthritis, hip/knee joint problems, sciatica/chronic back problems, and extremity weakness had the most severe impact on their disease-specific QoL, whereas cardiometabolic diseases including hypertension, diabetes, stroke, and angina exerted a lesser impact on their QoL. There were sex and age differences observed in the impact of several comorbidities on disease-specific QoL.
Cardiometabolic and non-cardiometabolic conditions were highly prevalent among our study participants, which is consistent with findings from previous studies that have shown that older patients with AF have a number of coexisting chronic diseases that are not limited to cardiovascular diseases [23, 24]. Given the fact that AF is associated with aging, older patients with AF are commonly faced with the burden of living with one or more chronic diseases and need to address the challenges of chronic pain, reduced mobility, polypharmacy, drug interactions, poor medication adherence due to pill burden, as well as regular hospital visits and unscheduled hospitalizations [25, 26]. Each of these factors may exert a significant toll on the patients’ ability to effectively cope with their coexisting diseases. To ensure optimal patient engagement in their care, healthcare providers need to be increasingly sensitive to patients’ specific concerns in dealing with their comorbid conditions and regularly assess the impact of specific diseases on their overall well-being and QoL. Addressing patients’ concerns and identifying those conditions that exert the greatest impact on QoL provide a timely opportunity to institute intervention strategies through a multidisciplinary team approach including social workers, pharmacists, nurses, physicians, and patient caregivers, and mitigate a progressive decline in patient’s health and functional status as they age.
A considerable proportion of our study participants reported that more symptomatic conditions, such as musculoskeletal/rheumatologic diseases exerted considerable impact on their QoL. Our results are consistent with prior studies conducted in other patient populations that have reported worse QoL scores in the presence of comorbid conditions [27, 28]. In a cross-sectional study among 1676 patients with type 2 diabetes recruited from a primary care clinic, comorbidities including osteoarthritis and rheumatoid arthritis notably reduced patients’ physical QoL [27]. Our findings have clinical implications in managing older adults with AF as physicians recommend patients to adopt lifestyle modifications including regular exercise and increased physical activity [29]. Furthermore, use of non-steroidal anti-inflammatory agents, one of the most effective therapies for pain control from arthritis, is most often contraindicated in older patients on oral anticoagulants to reduce the risk of bleeding [30]. Inasmuch, there needs to be better recognition of the high prevalence and impact of musculoskeletal disorders among older patients with AF that could hinder their mobility and considerably impact their QoL, thus reinforcing the need for more tailored approaches in recommending lifestyle modifications for older men and women with AF and coexisting musculoskeletal/rheumatologic conditions.
Although women had a higher prevalence of osteoarthritis than men, men were more likely to report that osteoarthritis severely impacted their QoL. Our findings on the prevalence of osteoarthritis are consistent with prior research among elderly individuals that have shown a higher prevalence of osteoarthritis among older women compared with men [31, 32]. However, in contrast with our results, previous studies have shown poorer self-reported QoL among women with osteoarthritis as they experience greater physical limitations and pain in affected joints and have more frequent clinic visits to their primary care physicians/specialists regarding symptom relief management of their osteoarthritis [33]. We recognize that our analysis does not account for the influence of other complex multi-level confounders including health literacy, patient–provider communication, and access to healthcare (insurance status) as important factors that may contribute to sex differences in the impact of osteoarthritis on QoL.
Our findings highlight that despite the higher prevalence of stroke among women with AF, men were more likely to report that stroke severely impacted their QoL. A limited number of studies have reported sex disparities in QoL among stroke survivors with varying underlying diseases [34,35,36]. Findings from these studies have been inconclusive either showing that female patients with stroke have lower QoL than males [34, 35] or have failed to observe meaningful differences in QoL between men and women after hospital discharge for stroke [36]. A potential limitation of these older studies has been the use of generic measures of QoL which do not specifically differentiate the experience of stroke impact on QoL in the presence of comorbid conditions. An important clinical consideration in understanding the influence of stroke on QoL in patients with AF is the long-term neurologic deficits from stroke that can cause a decline in independent functioning [37]. Although we did not directly examine the extent of neurologic deficits caused by stroke among our study participants, our findings infer that men may have experienced a greater impact of stroke on their QoL. Furthermore, reports of stroke causing severe impairment in QoL among men in the present study may be attributable to sex differences in coping and adaptation patterns. Future in-depth qualitative studies can be conducted to better understand how the physical or mental limitations caused by stroke may differentially impact men and women based on their illness adaptation patterns and coping strategies in dealing with their health challenges and maintaining an optimal QoL.
With regard to age differences in the impact of commonly reported comorbidities on disease-specific QoL, a greater proportion of participants aged less than 75 years were more likely to report that obesity, hip/knee joint problems, and fibromyalgia severely impacted their QoL in comparison with older participants. Of note, these conditions often present with overt symptoms that may hinder activities of daily living, mobility, and poor sleep quality [38, 39]. Our findings raise pertinent issues regarding the extent to which older individuals may perceive their comorbid conditions to be impacting their overall well-being. It is plausible that our much older study participants may have adapted to their chronic comorbid conditions over time, developed more resilience, and thus were less likely to experience significant impairment in their QoL from these conditions. In support of this claim, studies have described a degree of stability in life satisfaction among older persons despite a decline in objective measures of overall well-being, which has been viewed as paradoxical [40]. In an earlier community-based study in Italy among 100 elderly persons with age ranges from 75 to ≥ 100 years, centenarians reported greater satisfaction with life than those in younger age groups as they complained less about their physical limitations, took solace in religious faith, and maintained social relationships [41]. Furthermore, research has increasingly shown that QoL in older ages can be achieved by being more flexible and limiting activities or domains of functioning to those which are most salient to one’s life, maximizing one’s selected resources, and adopting a response-shift attitude by which individuals transform their core values and conceptualization of QoL to better accommodate physical ailment or negative circumstances [42, 43].
Given the current demographic transition and an aging population, cardiologists and other healthcare providers directly involved in the care of older individuals with AF should be consider assessment of, and tailored guidance to older AF patients to empower them in successfully navigating their multiple chronic conditions and AF care. With a greater understanding of the impact of specific comorbidities on QoL in patients with AF, health care providers, caregivers, and elderly patients can collaboratively develop long-lasting strategies that promote better adaptation, resilience, and greater overall well-being.
Study strengths and limitations
The present study has several strengths. Our study provides a contemporary inquiry into the impact of comorbid conditions on disease-specific QoL in a large cohort of older men and women with AF. Previous studies that have examined the influence of comorbid conditions on QoL in patients with AF have utilized generic measures of QoL which cannot, for an individual, distinguish the specific impact of comorbid conditions on disease-specific QoL. In the present study, we used a validated and reliable measure of disease-specific QoL, which standardizes and directly captures the impact of each comorbid disease on each patient’s QoL [16], thus providing more relevant clinical information about the burden of comorbidity on patient’s functioning and well-being than is possible with generic QoL assessments. Although we accounted for a wide range of chronic diseases known to impact patients’ overall well-being and QoL, there may be other age-related and psychopathologic conditions which were not fully captured by the QDIS-MCC. Another potential limitation of our study is the reliance on participants’ self-reports of their comorbid diseases without objective validation from medical records, which may have led to under as well as over-reporting of some comorbid conditions examined. However, prior studies suggest that patient self-reported conditions perform equally as well in predicting QoL in comparison with comorbidity data obtained from medical records [44, 45] and the QoL ratings with specific disease attributions utilized in our study have been shown to be sufficiently valid in the presence of comorbid conditions [16]. In addition, for multiple disease conditions having overlapping symptoms, patients may not be as able to sufficiently differentiate the specific impact on QoL of one disease condition from that of others. Nonetheless, for the most prevalent comorbid conditions across the clusters studied (cardiometabolic, musculoskeletal, and pulmonary), prior research has shown that disease-specific QOL impact ratings have convergent validity in relation to other methods of measuring the same disease and validity in discriminating between different diseases rated using the same method [16]. Furthermore, we recognize that a majority of our study participants were recruited from sites only in the North Eastern and South Eastern regions of the US which could lead to potential selection bias and limit the generalizability of our results to more ethnically diverse populations. The results obtained in the present study may be subject to the effect of time varying changes as we did not assess whether the impact of certain comorbid conditions on patient’s QoL may have improved or worsened over time. This underscores the need for future longitudinal studies to examine how chronic comorbid conditions may potentially impact QoL using a life-course perspective approach that provides greater opportunity to institute timely strategies required to mitigate the impact of comorbidities on QoL.
Conclusions
In this contemporary cohort of older men and women with AF, participants reported being diagnosed with an average of 5 or more comorbid conditions. Although cardiometabolic diseases were highly prevalent, patients attributed the greatest disease-specific QoL impact to musculoskeletal conditions. These conditions likely exert a significant impact on physical activity, mood, and sleep, three domains known to influence clinical and QoL outcomes. Understanding and clearly distinguishing the extent of impairment in QoL in AF patients due to underlying comorbid conditions provides a readily identifiable and timely opportunity to develop future interventions targeted at diseases that may cause significant burden and impairment in QoL, overall functioning, and well-being.
Data availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
References
January, C. T., Wann, L. S., Alpert, J. S., Calkins, H., Cigarroa, J. E., Cleveland, J. C., Jr., et al. (2014). 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation. Journal of the American College of Cardiology, 64(21), 2246–2280.
Andersson, T., Magnuson, A., Bryngelsson, I.-L., Frøbert, O., Henriksson, K. M., Edvardsson, N., et al. (2013). All-cause mortality in 272, 186 patients hospitalized with incident atrial fibrillation 1995–2008: A Swedish nationwide long-term case-control study. European Heart Journal, 34, 1061–1067.
Chamberlain, A. M., Alonso, A., Gersh, B. J., Manemann, S. M., Killian, J. M., Weston, S. A., et al. (2016). Multimorbidity and the risk of hospitalization and death in atrial fibrillation: A population-based study. American Heart Journal, 185, 74–84.
Cepeda-Valery, B., Cheong, A. P., Lee, A., & Yan, B. P. (2011). Measuring health related quality of life in coronary heart disease: the importance of feeling well. International Journal of Cardiology, 149, 4–9.
Kato, N., Kinugawa, K., Seki, S., et al. (2011). Quality of life as an independent predictor for cardiac events and death in patients with heart failure. Circulation Journal, 75, 1661–1669.
January, C. T., Wann, L. S., Alpert, J. S., Calkins, H., Cigarroa, J. E., Cleveland, J. C., Jr., et al. (2014). 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: executive summary: A report of the American College of Cardiology/American Heart Association Task Force on practice guidelines and the Heart Rhythm Society. Circulation, 130, 2071–2104.
Naser, N., Dilic, M., Durak, A., et al. (2017). The impact of risk factors and comorbidities on the incidence of atrial fibrillation. Mater Sociomed., 29(4), 231–236.
LaMori, J. C., Mody, S. H., Gross, H. J., et al. (2013). Burden of comorbidities among patients with atrial fibrillation. Therapeutic Advances in Cardiovascular Disease., 7, 53–62.
Ariansena, I., Gjesdala, K., Abdelnoorb, M., Edvardsenc, E., Engerd, S., & Tveitd, A. (2008). Quality of life, exercise capacity and comorbidity in old patients with permanent atrial fibrillation. Journal of Atrial Fibrillation., 1(4), 136.
Randolph, T. C., Simon, D. N., Thomas, L., et al. (2016). Patient factors associated with quality of life in atrial fibrillation. American Heart Journal, 182, 135–143.
Tan, H. C., Koh, K. W. L., Wu, V. X., Lim, T. W., & Wang, W. (2018). Health-related quality of life, psychological distress, and symptom burden in an Asian population of outpatients with atrial fibrillation. Heart and Lung, 47(4), 322–328.
Ware, J. E., Jr., Gandek, B., Guyer, R., & Deng, N. (2016). Standardizing disease-specific quality of life measures across multiple chronic conditions: Development and initial evaluation of the QOL Disease Impact Scale (QDIS®). Health Qual Life Outcomes, 14, 84.
Marino, F. R., Lessard, D. M., Saczynski, J. S., et al. (2019). Gait speed and mood, cognition, and quality of life in older adults with atrial fibrillation. Journal of the American Heart Association, 8(22), e013212.
Saczynski, J. S., Sanghai, S. R., Kiefe, C. I., et al. (2019). Geriatric elements and oral anticoagulant prescribing in older atrial fibrillation patients: SAGE-AF. Journal of the American Geriatrics Society. https://doi.org/10.1111/jgs.16178.
Deng, N., Anatchkova, M. D., Waring, M. E., Han, K. T., & Ware, J. E., Jr. (2015). Testing item response theory invariance of the standardized Quality-of-life Disease Impact Scale (QDIS(®) in acute coronary syndrome patients: Differential functioning of items and test. Quality of Life Research, 24(8), 1809–1822.
Ware, J. E., Gandek, B., & Allison, J. (2016). The validity of disease-specific quality of life attributions among adults with multiple chronic conditions. International Journal of Statistics in Medical Research, 5(1), 17–40.
Sherbourne, C. D., & Stewart, A. L. (1991). The MOS social support survey. Social Science and Medicine, 32(6), 705–714.
Nasreddine, Z. S., Phillips, N. A., Bedirian, V., et al. (2005). The Montreal cognitive assessment, MoCA: A brief screening tool for mild cognitive impairment. Journal of the American Geriatrics Society, 53(4), 695–699.
Saczynski, J. S., Inouye, S. K., Guess, J., et al. (2015). The montreal cognitive assessment: Creating a crosswalk with the mini-mental state examination. Journal of the American Geriatrics Society, 63(11), 2370–2374.
Spitzer, R. L., Kroenke, K., Williams, J. B. W., & Lowe, B. (2006). A brief measure of assessing generalized anxiety disorder: the GAD-7. Archives of Internal Medicine, 166, 1092–1097.
Mlinac, M. E., & Feng, M. C. (2016). Assessment of activities of daily living, self-care, and independence. Archives of Clinical Neuropsychology., 31(6), 506–516.
Lane, D. A., & Lip, G. Y. (2012). Use of the CHA(2)DS(2)-VASc and HAS-BLED scores to aid decision making for thromboprophylaxis in nonvalvular atrial fibrillation. Circulation, 126(7), 860–865.
Charlson, M. E., Pompei, P., Ales, K. L., et al. (1987). A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. Journal of Chronic Diseases, 40(5), 373–383.
Mashat, A. A., Subki, A. H., Bakhaider, M. A., et al. (2019). Atrial fibrillation: Risk factors and comorbidities in a tertiary center in Jeddah. Saudi Arabia International Journal of General Medicine, 12, 71–77.
Marcum, Z. A., & Gellad, W. F. (2012). Medication adherence to multidrug regimens. Clinics in Geriatric Medicine, 28(2), 287–300.
Adam, D. D., Anne, S. H., Richard, C. B., Scott, D. B., Guenter, B., Werner, H., et al. (2016). Hospitalizations in patients with atrial fibrillation: An analysis from ROCKET AF. EP Europace, 18(8), 1135–1142.
Adriaanse, M. C., Drewes, H. W., van der Heide, I., Struijs, J. N., & Baan, C. A. (2016). The impact of comorbid chronic conditions on quality of life in type 2 diabetes patients. Quality of Life Research, 25(1), 175–182.
Pati, S., Pati, S., Akker, M. V. D., Schellevis, F. F. G., Jena, S., & Burgers, J. S. (2020). Impact of comorbidity on health-related quality of life among type 2 diabetic patients in primary care. Prim Health Care Res Dev., 21, e9.
Bosomworth, N. J. (2015). Atrial fibrillation and physical activity: Should we exercise caution? Canadian Family Physician, 61(12), 1061–1070.
Kent, A. P., Brueckmann, M., Fraessdorf, M., Connolly, S. J., Yusuf, S., Eikelboom, J. W., et al. (2018). Concomitant oral anticoagulant and nonsteroidal anti-inflammatory drug therapy in patients with atrial fibrillation. American College of Cardiology, 72(3), 255–267.
Srikanth, V. K., Fryer, B., Math, J. L., Zhai, G., Winzenberg, T. M., Hosmer, D., et al. (2005). A meta-analysis of sex differences prevalence, incidence, and severity of osteoarthritis. Osteoarthritis and Cartilage, 13, 769–781.
Blagojevic, M., Jinks, C., Jeffery, A., & Jordan, K. P. (2010). Risk factors for onset of osteoarthritis of the knee in elderly adults: A systematic review and meta-analysis. Osteoarthritis and Cartilage, 18, 24–33.
Rosemann, T., Laux, G., & Szecsenyi, J. (2007). Osteoarthritis: Quality of life, comorbidities, medication and health service utilization assessed in a large sample of primary care patients. Journal of Orthopaedic Surgery and Research, 2, 12.
Hopman, W. M., & Verner, J. (2003). Quality of life during and after inpatient stroke rehabilitation. Stroke, 34, 801–805.
Serda, E. M., Bozkurt, M., Karakoç, M., et al. (2015). Determining quality of life and associated factors in patients with stroke. Turkish Journal of Physical Medicine and Rehabilitation, 61, 148–154.
Kranciukaite, D., Rastenyte, D., Jureniene, K., & Sopagiene, D. (2007). Quality of life in stroke survivors. Medicina (Kaunas), 43, 736–745.
de Haan, R. J., Limburg, M., Van der Meulen, J. H., Jacobs, H. M., & Aaronson, N. K. (1995). Quality of life after stroke. Impact of stroke type and lesion location. Stroke, 26(3), 402–408.
Ackerman, I. N., & Osborne, R. H. (2012). Obesity and increased burden of hip and knee joint disease in Australia: Results from a national survey. BMC Musculoskeletal Disorders, 13, 254.
Hargens, T. A., Kaleth, A. S., Edwards, E. S., & Butner, K. L. (2013). Association between sleep disorders, obesity, and exercise: A review. Nature and Science of Sleep., 5, 27–35.
Staudinger, U. M. (2000). Many reasons speak against it, yet many people feel good: The paradox of subjective well-being. Psychologische Rundschau, 51, 185–197.
Buono, M. D., Urciuou, O., & de Leo, D. (1998). Quality of life and longevity: A study of centenarians. Age and Ageing, 27, 207–216.
Baltes, P. B., & Mayer, K. U. (Eds.). (1999). The Berlin aging study: Aging from 70 to 100. New York: Cambridge University Press.
Sprangers, M. A. G., & Schwartz, C. E. (1999). Integrating response shift into health-related quality of life research: A theoretical model. Social Science and Medicine, 48, 1507–1515.
Corser, W., Sikorskii, A., Olomu, A., Stommel, M., Proden, C., & Holmes-Rovner, M. (2008). Concordance between comorbidity data from patient self-report interviews and medical record documentation. BMC Health Services Research, 8, 85.
Olomu, A. B., Corser, W. D., Stommel, M., Xie, Y., & HolmesRovner, M. (2012). Do self-report and medical record comorbidity data predict longitudinal functional capacity and quality of life health outcomes similarly? BMC Health Services Research, 12, 398.
Acknowledgements
We appreciate the John Ware Research Group for granting permission and access to utilize the Quality of Life Disease Impact Scale–Multiple Chronic Conditions form (QDIS-MCC).
Funding
This work was supported by Grant R01HL126911 from the National Heart, Lung, and Blood Institute (NHLBI). D.D.M is supported by other NHLBI Grants: R01HL137734, R01HL137794, R01HL13660, and R01HL141434. M.T. is supported by grants from the National Institute on AGING (R33AG057806 and RO1AG062630). The funding source had no role in the study concept and design, participant recruitment, data acquisition, analysis, interpretation of study results, manuscript preparation, and decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
HA: Conceptualization, Methodology, Formal Analysis, Writing—Original draft preparation, and Validation. JS: Funding Acquisition, Investigation, Conceptualization, Reviewing and Editing drafted manuscript. JW, JM, TP, HA, BB, IP, MT: Reviewing and Editing drafted manuscript. CK: Conceptualization, Writing—Reviewing and Editing. RG: Conceptualization, Writing—Reviewing and Editing. DDM: Funding Acquisition, Investigation, Conceptualization, Reviewing and Editing drafted manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
D.D.M has received research grant support from Apple Computer, Bristol‐Myers Squibb, Boeringher‐Ingelheim, Pfizer, Samsung, Philips Healthcare, and Biotronik; consultancy fees from Bristol‐Myers Squibb, Pfizer, Flexcon, and Boston Biomedical Associates; and has inventor equity in Mobile Sense Technologies, Inc (Farmington, CT). All other authors declare no potential conflicts of interest.
Ethical approval
Institutional Review Boards (IRBs) at the participating study sites approved the study. Each eligible participant provided written informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Abu, H.O., Saczynski, J.S., Ware, J. et al. Impact of comorbid conditions on disease-specific quality of life in older men and women with atrial fibrillation. Qual Life Res 29, 3285–3296 (2020). https://doi.org/10.1007/s11136-020-02578-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-020-02578-3