Abstract
Purpose
The aim of this study was to evaluate if health and oral health status of children and adolescents with different stages of CKD are associated with their health-related quality of life (HRQoL), oral health-related quality of life (OHRQoL) and socioeconomic and demographic conditions.
Methods
One hundred children and adolescents with CKD were age and gender matched to 100 individuals without CKD (mean age ± SD = 13.04 ± 2.57). Oral health was characterised by means of gingival bleeding index (GBI), plaque index (PI), the decayed, missing, and filled teeth (DMFT) index and the developmental enamel defect (DED) index. All children and adolescents answered two Peds QL® instruments (general and oral health scales).
Results
Comparing the mean scores of HRQoL and OHRQoL between groups, we observed that CKD group demonstrated worse perceptions when compared to non-CKD group. Multiple linear regression analysis with bootstrap estimation of variance (1000 replications) showed association between dental caries experience (p < 0.001), gingival inflammation (p < 0.001) and diagnosis of CKD (p = 0.027) with the OHRQoL and between physical and the emotional domain of HRQoL, when moderate/severe gingival inflammation and hypoplasia were present.
Conclusion
The implementation of public policies that contemplate the early dental preventive intervention in CKD children and adolescents should occur aiming to improve their oral health, once oral manifestations can directly affect the aspects of the HRQoL and OHRQoL of these individuals.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
Chronic kidney disease (CKD) is defined by the presence of injury and/or loss of renal function (glomerular filtration rate—GFR) within 3 months or more, regardless of diagnosis [1]. CKD has emerged as a serious public health problem but is relatively uncommon in children when compared to adults. However, when it occurs, it causes devastating consequences for children and, as being a complex condition, the treatment is highly expensive [1]. CKD has presented an increased incidence and prevalence in the pediatric population. Recent data estimates 85 cases per million age-related population (pmarp) in the USA and 62 pmarp cases in Europe. In Brazil (state of São Paulo), a study found a prevalence of 23.4 cases pmarp in end-stage renal disease in patients under 18 years old [2, 3].
CKD is classified into 5 stages, according to the degree of glomerular function impairment. In stage 1, the GFR rate remains normal (≥ 90 mL/min per 1.73 m2), but it is already possible to identify the onset of renal parenchymal damage. In stage 2, we observed a slight reduction in the GFR, associated with renal injury. Loss of renal function (renal insufficiency) is established when clearance values are lower 60 mL/min per 1.73 m2 (stages 3 to 5). Such classification is related with prognosis and treatment decision-making. Renal replacement therapy (hemodialysis, peritoneal dialysis and renal transplantation) is implemented in stage 5 (clearance values lower than 15 mL/min per 1.73 m2). Prior to this, conservative treatment involves controlling the risk factors of the disease [4].
As renal function deteriorates, there are changes in various organs of children and adolescents. Such manifestations may include changes in bone formation, anemia, arterial hypertension, polyuria, metabolic disorders, asthenia and infections, which may affect their quality of life (QoL) and lead to early death [5]. Nephropathies also favor the appearance of oral diseases that must be carefully evaluated by dental professionals. CKD may lead to changes in the oral cavity in both soft and hard tissues. There are some reports of stomatitis, changes in salivary flow, xerostomia, uremic odor, dysgeusia, pale mucosa, developmental enamel defect, gingival inflammation, gingival growth and high prevalence of dental calculus. The prevalence of dental caries seems to be low [6,7,8,9,10].
CKD in children and adolescents demonstrates an impact on their health-related quality of life (HRQoL) when compared to clinically healthy children [11,12,13]. Dietary and water restrictions, complex medical treatment and therapeutics and successive hospitalizations are routine for CKD patients and can potentially affect their lives in several aspects. Frequent health problems and lifestyle changes result in significant deficits in emotional and physical constructs for children and their families [14, 15]. The oral condition may also affect HRQoL as oral diseases and disorders, such as periodontal diseases and developmental enamel defects can affect self-esteem, chewing and speaking abilities and may be related to absence of schooling and emotional problems [16, 17]. There are studies on QoL in children and adolescents with CKD related to their psychological and behavioral impacts, but the emphasis of oral health-related quality of life (OHRQoL) has not been found in the literature. As it is a systemic disease displaying significant clinical repercussions, the evaluation of their impact on the HRQoL and OHRQoL is essential.
The aim of this study was to evaluate if health and oral health status of children and adolescents with different stages of CKD are associated with their HRQoL, OHRQoL and socioeconomic and demographic conditions, as well as to compare it with a group of non-CKD children. Our hypothesis is that children with CKD should have worse dental/oral health, worse HRQoL and worse OHRQoL outcomes than non-CKD children. In addition, children with more advanced CKD should have worse outcome than children with early-stage CKD and non-CKD children.
Methods
Ethical approval
The study was undertaken after obtaining ethical clearance from the Ethics Committee of the Dental School and from the Children Institute (Medical School)—University of São Paulo (Brazil)—Registration Number 1.484.266, according to the Helsinki Declaration. Details of the study were explained to parents and their written informed consent was obtained.
Participants and recruitment
A cross-sectional study was conducted in São Paulo, Brazil, from 2014 to 2016. The minimum sample size was calculated based on comparisons of Peds QL scores between two groups through Student's t tests. A minimum difference of 10% was considered as minimally important. Therefore, considering a mean of 82 for the control group, with a standard deviation of around 20, and an estimated mean of 74 and standard deviation of 15 for the study group, the estimated effect size was 0.455. With this value, the minimum sample size was 81 persons per group. This value was calculated using the statistical software G* Power 3.1.9.2 (University of Kiev, Kiev, Germany). With 200 participants and considering a level of significance of 5%, we obtained a power of 88.5% to detect a ratio of 1.5 considering a binomial independent variable.
A cohort of one hundred children and adolescents, aged 8–18 years (mean ± standard deviation SD = 13.04 ± 2.57), with definitive medical diagnosis of CKD—study group (SG) and receiving medical care at Children Institute of the Medical School (University of São Paulo, Brazil) was non-randomly selected to be included in the study. A cross-tabulation of the CKD group was developed to know the precise age and gender of the CKD group. Later, we recruited children/adolescents with the same age and gender, from a database of patients who was looking for treatment at Dental School (University of São Paulo, Brazil), to match the distribution in the table until it was filled and established the non-CKD group.
Patients who received periodontal treatment within 6 months prior to the study entry; smokers and those who were undergoing orthodontic treatment were excluded from the study. Additional exclusion criteria were the use of antibiotics and/or anti-inflammatory medication in the previous 6 months, cognitive impairment and acute systemic diseases in the last 30 days.
Non-clinical examination
One of the parents was invited to answer to one researcher (TMCS) a questionnaire about socio-demographic data and to update all the information collected in patients’ records. The socio-demographic questionnaire included data on gender, child’s age, number of children in family, marital status of parents, with whom the child lives, tenure status of the housing unit, number of members in the household, household income, parents level of education and working time.
Health-related quality of life instrument and oral health-related quality of life instrument
The questionnaires Peds QL ™ 4.0—child/adolescent report [18] and Peds QL ™—Oral Health Scale [19] were administered to children and adolescents by one researcher (TMCS) trained in the intonation of questions. Before, the patient’s guardian was invited to leave the room, so that there was no interference in children and/or adolescents’ answers.
The Peds QL™ 4.0 child/adolescent report has 23 questions distributed in the physical (8), emotional (5), social (5) and school (5) dimensions. The PedsQL ™ Oral Health Scale was developed to be used simultaneously with the PedsQL ™ 4.0, with the aim to provide an overall measure of HRQOL [18, 19]. Such a questionnaire has five questions related to oral health. Both instruments were translated and validated for Brazilian culture [20, 21]. A higher score implied a better OHRQoL and HRQoL.
Clinical oral examination
Thereafter, patients were clinically evaluated by a second trained and calibrated dental professional (LACA) who was not aware of the contents of the interview. Oral examination was carried out using mouth mirror and periodontal probe. The intra-oral examination included dental caries evaluation by means of the decayed, missing, and Filled Teeth (dmft/DMFT) Index [22]. The overall values of dmft and DMFT were evaluated separately and grouped together by the sum of d + m +f/D + M + F. The scores were given and the severity of dental caries was expressed based on previously proposed values: dmft/DMFT 0 = caries free; dmft/DMFT 1–2 = low severity; dmft/DMFT 3–4 = moderate severity or dmft/DMFT ≥ 5 high severity. If retained deciduous tooth was present, the caries status of only the permanent tooth was recorded, according to the WHO guidelines [23, 24].
The presence of dental biofilm and gingival condition were evaluated, respectively, by means of the Plaque Index (PI) [25] and Gingival Index System (GIS) [26]. PI determines the oral hygiene condition by detecting the dental biofilm upon clinical examination. According to this index, the scores are: 0 = absence of visible biofilm; 1 = thin biofilm, easily removed, on anterior and/or posterior teeth, visible only after drying with gauze; 2 = thick biofilm, firmly adhered on anterior or posterior teeth, visible without drying and associated or not to thin biofilm on other teeth and 3 = thick biofilm, firmly adhered on anterior and posterior teeth, visible without drying. The surfaces of permanent maxillary right first molar, permanent maxillary right central incisor, permanent maxillary left central incisor, permanent maxillary left first molar, permanent mandibular left first molar, permanent mandibular left central incisor, permanent mandibular right central incisor and permanent mandibular right first molar were evaluated for this criteria. If one of these teeth were missing, it should be replaced by the adjacent one. These scores were added together and divided by the number of teeth examined and it was thus obtained an average of the individual plaque index. The scores 0–1 implied a good oral hygiene; 1.1–2, a moderate oral hygiene and 2.1–3, a poor oral hygiene.
The GIS was also determined for each child. A periodontal probe was slightly penetrated in the gingival sulcus (approximately 0.5 mm) covering the labial and lingual surfaces/palatal from proximal to proximal of teeth indexes (permanent maxillary right first molar, permanent maxillary right central incisor, permanent maxillary left central incisor, permanent maxillary left first molar, permanent mandibular left first molar, permanent mandibular left central incisor, permanent mandibular right central incisor and permanent mandibular right first molar). A dichotomic response was used for the interpretation of the results: 0 = total absence of bleeding and 1 = presence of bleeding for each evaluated area. The total scores were expressed as: 0–0,1 = no gingival inflamation; 0.1–1 = mild gingival inflamation; 1.1–2 = moderate gingival inflamation; 2.1–3 = intense gingival inflamation. The prevalence of developmental enamel defect was performed by means of the developmental enamel defect index (DED) [27]. The surfaces of all teeth were evaluated for the presence of opacity or hypoplasia.
Statistical analyses
We first examined differences between the CKD and non-CKD groups with respect to baseline characteristics (e.g., age, gender, family configuration, household characteristics and parental employment). Besides that, we examine the extent to which the two groups differed in dental and oral outcomes on dmft/DMFT, PI, GIS and DED. The dental/oral outcomes were categorical variables. Such comparisons were carried out using the Chi square test with continuity adjustment.
PedsQL subscale scores (physical, emotional, social, and school functioning) were first compared between CKD and non-CKD groups in a series of independent-sample t tests to compare the average HRQoL scores between the two groups. Next, statistically significant covariates by univariate analyses (e.g., CKD vs. non-CKD groups and differences in dental/oral outcomes) were further entered into multivariate linear regression analyses with bootstrap estimation of variance (1000 replications). Additionally, OHRoL was evaluated by the PedsQL Oral Health Scale total score using the same analytic strategy. All data were processed by means of the Stata 12.0 statistical software (StataCorp LP, College Station, USA). The level of statistical significance was set at 5%.
Results
Intra-examiner reliability was determined by the re-evaluation of 20 children and adolescents within a two-week interval (10% of the sample) and by means of Kappa values: 0.9 for dmft/DMFT; 0.8 for PI and GIS and 1.0 for DED. A total of 230 patients were invited to participate of the study, but 30 were excluded due to: use of antibiotics (22), cognitive deficits (5) and acute systemic disease (3) in the CKD group. A response rate of 100% was attained for non-CKD group and 83.3% for CKD group.
A total of 200 patients participated in the study and the sample comprised 66 (33%) females and 134 (67%) males. Most of the socioeconomic and demographic questionnaire were answered by mothers (75%), the remainder were answered by fathers or a legal guardian (25%). The mean age (SD) of the children for both groups was 13.04 years old (± 2.57 year.). Socioeconomic and demographic conditions are described on Table 1. It can be observed that the profile of the respondents in both groups differ in terms of number of children (p = 0.024), work (p < 0.001) and household income (p = 0.012).
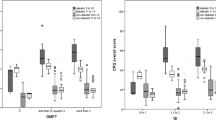
Oral health conditions are described on Table 2. We observe in Table 2 that patients with CKD have a lower prevalence of caries disease and worse oral hygiene, a higher prevalence of gingival inflammation and more severe enamel development defects when compared to non-CDK group. There were statically significant differences between CKD and non-CKD groups for caries experience (p < 0.001), PI (p < 0.001), GIS (p < 0.001) and presence of DDE (p < 0.001).
Comparing the mean scores of HRQoL and OHRQoL between groups, we observe that CKD group demonstrated worse perceptions of it when compared to non-CKD group (Table 3). We also observe that the variability of the scores was higher for the CKD group, indicating that the disease may affect different aspects of health and oral health.
Table 4 shows the average PedsQL and PedsQL Oral Health subscale scores, stratified by the severity of renal disease. The PedSQL scores of the non-CKD group were presented for comparison. As the severity of renal disease increased, a corresponding decrease in HRQoL domains and OHRQoL were evident.
The variables presenting statistically significant association in the univariate analysis of the association between demographic/socioeconomic characteristics with OHRQoL were group, education level of the caregiver and household income. Other variables such as gender, child’s age, number of people in the residence, tenure status of the housing unit, marital status, age of the responsible, number of children and people who took care of child did not present statistical significance.
Table 5 shows the multivariate linear regression on the PedsQL Oral Health total scores as a function of dental and oral health outcomes. Statistically significant associations were found with CKD (p = 0.027), caries experience (p = 0.001/p = <0.001), moderate or severe gingival inflammation (p < 0.001) and presence of DED-type hypoplasia (p = 0.015). Educational level of caregiver and household income were excluded because they were not statistically significant in the regression.
Association between HRQoL in PedsQL domains and CKD and other oral examination findings showed statistical significance in all domains for CKD group. Moderate/severe gingival inflammation was statistically associated with emotional domain. Hypoplasia was statistically associated with physical and emotional domain (Table 6).
Discussion
The assessment of OHRQoL incorporated into HRQoL instruments developed for children and adolescents is extremely relevant. First, it serves as a basis for highlighting perceived needs in oral health promotion; second, it opens the way for the development of oral health programs; and third, it gives preventive support to monitor and improve oral health and the general well-being of children.
Some studies have confirmed the importance of maintaining good oral health among children and adolescents with CKD [6, 8, 28]. However, little is known about their perception concerning their own oral health. This is the first study that seeks to evaluate the perceptions and consequences of oral conditions in CKD children and adolescents.
The CKD children and adolescents in the study presented worse oral conditions with great levels of moderate and intense gingival inflammation, worse oral hygiene and higher number of developmental enamel defect, findings that are in agreement with other studies [6, 8, 9]. In relation to caries, this group of subjects had less experience of caries than non-CKD. A recent systematic review showed a lower prevalence of caries in children and adolescents with CKD when compared to a healthy population. However, the authors concluded that there are few well-designed longitudinal studies that provide good scientific evidence to support this conclusion [10]. Children with CKD seems to have lower caries experience, despite the high prevalence of inadequate oral hygiene and cariogenic diet, because the high levels of urea in saliva increasing salivary pH may have a protective effect against caries [29]. The increased buffer capacity of saliva is the result of the high ammonia concentrations resulted from urea hydrolysis [6, 8, 10]
This study shows that HRQoL and OHRQoL scores are significantly lower for the group of children and adolescents with CKD, if compared to non-CKD. The worse OHRQoL in the CKD group was associated with caries experience and moderate to severe gingival inflammation. The main domains affected by oral health in HRQoL were the physical and the emotional, when moderate/severe gingival inflammation and hypoplasia were present. We believe that this can be explained by the perception of health condition, disease and symptoms resulting from the systemic condition and it’s a subjective experience associated with oral health. The caries experience was associated with worst OHRQoL in the non-CKD group, which was expected, as the literature reports this association [30,31,32].
Patients who are in the terminal stages of CKD (stages 4 and 5) present additional challenges since there is an increase in restrictions on the routine habits with chronic dependence of medical equipment to perform dialysis or hemodialysis, feelings of hope and expectation for renal transplantation, physical changes pertinent to transplantation and more medical visits. Lopes et al. [11] demonstrated a worst perception of HRQoL in children and adolescents within terminal stages of CKD. Even in the early stages of CKD (1 to 3), there was also a worse perception of HRQoL when compared to non-CKD group [13].
Our hypothesis that CKD individuals would have poor oral health status and worse perception of their HRQoL and OHRQoL due to the significant impact that CKD causes in the oral cavity was confirmed in the study. This perspective was based on a clinical point of view, considering the critical conditions of patients under medical treatment, mainly for those in more advanced stages of CKD. Renal replacement therapy (RRT), 3 to 5 times a week, is a time-consuming treatment for these individuals. Besides, it is invasive, uncomfortable and shows uncertain prognosis, sometimes leading to premature death.
The poor oral health and OHRQoL observed in CKD group highlight the difficulty that patients have to access dental treatment and the lack of preventive support [33]. This emphasizes the urgent need for oral health programs within this population. Oral health promotion in children and adolescents with CKD seeks to ensure well-being, esthetics, communication, quality of life and self-esteem improvement.
Family participation and a transdisciplinary interaction among health professionals is the ideal model to change their perception regarding oral health, which is left mostly in a secondary plane by patients with chronic disease [33]. It is common for children and adolescents with CKD and their families focus their activities around the treatment of the disease, neglecting or leaving aside important aspects related to other spheres of their lives, such as oral health. Thus, the introduction of the dental team to the medical service helps to guide, motivate, promote oral health and help to introduce preventive programs which will improve general and oral health conditions and provide better quality of life, ensuring a successful transition from infancy and adolescence to adulthood.
Other important variables that may directly affect the outcome are socioeconomic characteristics. Some studies [34,35,36,37] attribute that families with low socioeconomic conditions may have more oral diseases and worse HRQoL. Our study shows that there was an association between schooling and household income of families with the OHRQoL in the univariate model, but the significance was lost in the final adjusted model.
The present study presents inherent limitations to a cross-sectional design and some degree of information bias may have occurred. Longitudinal studies are needed to support the development of public health programs aimed to reduce the impact of oral disorders and diseases within CKD population. The evaluation of HRQoL and OHRQoL may contribute to improve public health strategies directed to children and adolescents with CKD, since there is a lack of planning actions for oral health directed to them.
The perception of CKD population regarding their oral condition and the impact on their OHRQoL is an important step in the development of less invasive and more humanistic care for this population. Our study investigated this important issue in the pediatric population with CKD and found a relationship between oral health and oral/health-related quality of life. We addressed an issue that, to the best of our knowledge, this has not been discussed before. Oral diseases and conditions can be considered a public health problem for this population, and thrives in the development of new researches in this area for better understanding the subject and consequently the development of more appropriate approaches and treatments are recommended. This study raises the attention on the need of a transdisciplinary approach, since the treatment of these patients clearly includes challenges in social, emotional, schooling, physical and oral aspects.
Conclusion
The elaboration of public policies that contemplate the early dental preventive intervention in CKD individuals should occur aiming to improve their oral health, once oral conditions can directly affect the aspects of the HRQoL and OHRQoL of these individuals.
Data availability
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
Abbreviations
- CKD:
-
Chronic kidney disease
- OHRQoL:
-
Oral health-related quality of life
- HRQoL:
-
Health-related quality of life
- QoL:
-
Quality of life
- pmarp:
-
Per million age-related population
- GBI:
-
Gingival Bleeding Index
- PI:
-
Plaque Index
- DMFT:
-
Decayed, Missing, and Filled Teeth Index
- DED:
-
Developmental Enamel Defect Index
- pmarp:
-
Per million age-related population
- SG:
-
Study group
- CG:
-
Control group
- Mean ± SD:
-
Mean and standard deviation
References
Warady, B. A., & Chadha, V. (2007). Chronic kidney disease in children: The global perspective. Pediatric Nephrology(Berlin, Germany), 22(12), 1999–2009.
Collins, A., Foley, R., Herzog, C., Chavers, B., Gilbertson, D., Ishani, A., et al. (2010) Excerpts from the US Renal Data System 2009 Annual Data Report. American Journal of Kidney Diseases, 55(1 Suppl 1), S1–420, A6–7.
Nogueira, P. C., Feltran Lde, S., Camargo, M. F., Leão, E. R., Benninghoven, J. R., Gonçalves, N. Z., et al. (2011). Estimated prevalence of childhood end-stage renal disease in the state of São Paulo. Revista da Associação Médica Brasileira, 57(4), 436–441.
Hogg, R. J., Furth, S., Lemley, K. V., Portman, R., Schwartz, G. J., Coresh, J., et al. (2003). National kidney foundation’s kidney disease outcomes quality initiative clinical practice guidelines for chronic kidney disease in children and adolescents: evaluation, classification, and stratification. Pediatrics, 111(6 Pt 1), 1416–1421.
Ardissino, G., Testa, S., Daccò, V., Paglialonga, F., Viganò, S., Felice-Civitillo, C., et al. (2012). Puberty is associated with increased deterioration of renal function in patients with CKD: data from the ItalKid project. Archives of Disease in Childhood, 97(10), 885–888. https://doi.org/10.1136/archdischild-2011-300685.
Al-Nowaiser, A., Roberts, G. J., Trompeter, R. S., Wilson, M., & Lucas, V. S. (2003). Oral health in children with chronic renal failure. Pediatric Nephrology, 18(1), 39–45.
Chidambaram, R. (2014). Dentist-nephrologist symbiosis in the dental management of chronic kidney disease patient. Journal of the College of Physicians and Surgeons Pakistan, 24(12), 955.
Davidovich, E., Schwarz, Z., Davidovitch, M., Eidelman, E., & Bimstein, E. (2005). Oral findings and periodontal status in children, adolescents and young adults suffering from renal failure. Journal of Clinical Periodontology, 32(10), 1076–1082.
Nunn, J. H., Sharp, J., Lambert, H. J., Plant, N. D., & Coulthard, M. G. (2000). Oral health in children with renal disease. Pediatric Nephrology, 14(10–11), 997–1001.
Andrade, M. R., Antunes, L. A., Soares, R. M., Leão, A. T., Maia, L. C., & Primo, L. G. (2014). Lower dental caries prevalence associated to chronic kidney disease: a systematic review. Pediatric Nephrology(Berlin, Germany), 29(5), 771–778. https://doi.org/10.1007/s00467-013-2437-4.
Lopes, M., Ferraro, A., & Koch, V. H. (2014). Health-related quality of life of children and adolescents with CKD stages 4-5 and their caregivers. Pediatric Nephrology, 29(7), 1239–1247. https://doi.org/10.1007/s00467.014.2769-8.
Goldstein, S. L., Gerson, A. C., & Furth, S. (2007). Health-related quality of life for children with chronic kidney disease. Advances in Chronic Kidney Disease, 14(4), 364–369.
Gerson, A. C., Wentz, A., Abraham, A. G., Mendley, S. R., Hooper, S. R., Butler, R. W., et al. (2010). Health-related quality of life of children with mild to moderate chronic kidney disease. Pediatrics, 125(2), e349–e357. https://doi.org/10.1542/peds.2009-0085.
Gerson, A., Hwang, W., Fiorenza, J., Barth, K., Kaskel, F., Weiss, L., et al. (2004). Anemia and health related quality of life in adolescents with chronic kidney disease. American Journal of Kidney Diseases, 44(6), 1017–1023.
Fadrowski, J., Cole, S. R., Hwang, W., Fiorenza, J., Weiss, R. A., Gerson, A., et al. (2006). Changes in physical and psychosocial functioning among adolescents with chronic kidney disease. Pediatric Nephrology(Berlin, Germany), 21(3), 394–399.
Schuch, H. S., Dos Santos Costa, F., Torriani, D. D., Demarco, F. F., & Goettems, M. L. (2015). Oral health-related quality of life of schoolchildren: Impact of clinical and psychosocial variables. International Journal of Paediatric Dentistry, 25(5), 358–365.
Peres, K. G., Cascaes, A. M., Leão, A. T., Côrtes, M. I., & Vettore, M. V. (2013). Sociodemographic and clinical aspects of quality of life related to oral health in adolescents. Revista de Saude Publica, 47(3), 19–28.
Varni, J. W., Limbers, C. A., & Burwinkle, T. M. (2007). How young can children reliably and validly selfreport their health-related quality of life? An analysis of 8,591 children across age subgroups with the PedsQL 4.0 Generic Core Scales. Health and Quality of Life Outcomes, 5, 1.
Steele, M. M., Steele, R. G., & Varni, J. W. (2009). Reliability and validity of the PedsQLTM Ora Health Scale: measuring the relationship between child oral health and health-related quality of life. Child Health Care., 38, 228–244. https://doi.org/10.1080/02739610903038818.
Klatchoian, D. A., Len, C. A., Terreri, M. T., Silva, M., Itamoto, C., Ciconelli, R. M., et al. (2008). Quality of life of children and adolescents from Sao Paulo: reliability and validity of the Brazilian version of the Pediatric Quality of Life Inventory version 4.0 Generic Core Scales. Jornal de pediatria, 84(4), 308–315. https://doi.org/10.2223/jped.1788.
Bendo, C. B., Paiva, S. M., Viegas, C. M., Vale, M. P., & Varni, J. W. (2012). The PedsQL™ oral health scale: feasibility, reliability and validity of the Brazilian Portuguese version. Health and Quality of Life Outcomes, 24(10), 42. https://doi.org/10.1186/1477-7525-10-42.
World Health Organization. (1997) Oral health surveys: Basic methods (4th ed.). Geneva: Disponivel em: http://apps.who.int/iris/handle/10665/41905.
World Health Organization. (2013). Oral health surveys—Basics methods (5th ed.). Geneva, Switzerland: World Health Organization
AAPD. Definition of Early Childhood Caries (ECC). American Academy of Pediatric Dentistry 2008:13. http://www.aapd.org/media/Policies_Guidelines/D_ECC.pdf.
Silness, J., & Loe, H. (1964). Periodontal disease in pregnancy. II. Correlation between oral hygiene and periodontal condtion. Acta Odontologica Scandinavica., 22, 121–125.
Loe, H., & Silness, J. (1963). Periodontal disease in pregnancy. I. Prevalence and severity. Acta Odontologica Scandinavica, 21, 533–551.
Review of the developmental defects of enamel index (DDE Index) (1992). Commission on oral health, research and epidemiology. Report of an FDI Working Group. International Dental Journal, 42, 411–426.
Subramaniam, P., Gupta, M., & Mehta, A. (2012). Oral health status in children with renal disorders. Journal of Clinical Pediatric Dentistry, 37(1), 89–93.
Ertuğrul, F., Elbek-Cubukçu, C., Sabah, E., & Mir, S. (2003). The oral health status of children undergoing hemodialysis treatment. The Turkish Journal of Pediatrics, 45(2), 108–113.
Ratnayake, N., & Ekanayake, L. (2005). Prevalence and impact of oral pain in 8-year-old children in Sri Lanka. International Journal of Paediatric Dentistry, 15(2), 105–112.
Do, L. G., & Spencer, A. (2007). Oral health-related quality of life of children by dental caries and fluorosis experience. Journal of Public Health Dentistry, 67(3), 132–139.
Abanto, J., Paiva, S. M., Raggio, D. P., Celiberti, P., Aldrigui, J. M., & Bönecker, M. (2012). The impact of dental caries and trauma in children on family quality of life. Community Dentistry and Oral Epidemiology, 40(4), 323–331. https://doi.org/10.1111/j.1600-0528.2012.00672.x.
Summers, S. A., Tilakaratne, W. M., Fortune, F., & Ashman, N. (2007). Renal disease and the mouth. American Journal of Medicine, 120(7), 568–573.
Pisek, A., Pitiphat, W., Chowchuen, B., & Pradubwong, S. (2014). Oral health status and oral impacts on quality of life in early adolescent cleft patients. Journal of the Medical Association of Thailand, 97(Suppl 10), S7–S16.
Bastos, J. L., Peres, M. A., Peres, K. G., Araujo, C. L., & Menezes, A. M. (2008). Toothache prevalence and associated factors: A life course study from birth to age 12 yr. European Journal of Oral Sciences, 116, 45.
Peres, K. G., Peres, M. A., Araujo, C. L., Menezes, A. M., & Hallal, P. C. (2009). Social and dental status along the life course and oral health impacts in adolescents: A population-based birth cohort. Health and Quality of Life Outcomes, 22(7), 95. https://doi.org/10.1186/1477-7525-7-95.
Gaur, S., & Nayak, R. (2011). Underweight in low socioeconomic status preschool children with severe early childhood caries. Journal of Indian Society of Pedodontics and Preventive Dentistry, 29(4), 305–309. https://doi.org/10.4103/09-4388.86.
Acknowledgements
We gratefully acknowledge the “Coordenação de Aperfeiçoamento de Pessoal de Nível Superior” (CAPES) and the “Fundação de Amparo à Pesquisa de São Paulo” (FAPESP). We also thank all the patients for their most generous efforts in making our research project a success.
Funding
No funding was secured for this study.
Author information
Authors and Affiliations
Contributions
TMCS: conceptualized and designed the study, drafted the initial and final manuscript, was one of the examiners and contribute with the collection of data; LACA: was one of the examiner and contribute with the collection of data; DGS: reviewed and revised the manuscript, AW: reviewed and revised the manuscript and supervised data collection; FMM: was responsible for the statistical analyses; ALC: conceptualized and designed the study, coordinated and supervised data collection.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This study obtained the ethical clearance from the Ethics Committee of the Dental School and from the Children Institute (Medical School) – University of São Paulo (Brazil) – Registration Number 1.484.266, according to the Helsinki Declaration. Details of the study were explained to parents and their written informed consent was obtained.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Silva, T.M.C., Alves, L.A.C., Garrido, D. et al. Health and oral health-related quality of life of children and adolescents with chronic kidney disease: a cross-sectional study. Qual Life Res 28, 2481–2489 (2019). https://doi.org/10.1007/s11136-019-02196-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-019-02196-8