Abstract
Purpose
The present study compared psychological factors (i.e., alexithymia, somatization, pain catastrophizing (PC), anxiety, and depression) and QOL for headache patients and headache-free individuals, and examined whether somatization and PC mediate the relationship between alexithymia and headache impact in headache patients.
Methods
Study participants consisted of 123 headache patients from an outpatient clinic at a university hospital and 124 headache-free individuals in Daegu, Korea. The survey employed the somatization and anxiety subscales of the Symptom Checklist-90-revised, the Patient Health Questionnaire-9, Pain Catastrophizing Scale, Toronto Alexithymia Scale, Short-Form Health survey-8 (SF-8), and the Headache Impact Test-6.
Results
Headache patients showed a higher level of all psychological factors and lower level of two summary scores (physical and mental health) as well as the seven dimensions of the SF-8 compared with headache-free individuals. Examination employing the SPSS Process macro found that the direct effect of alexithymia on headache impact was not significant after controlling for somatization and PC. The total indirect effects of alexithymia on headache impact were significant without anxiety and depression as covariates with the significant indirect effects of alexithymia on headache impact via somatization or via PC as well as via somatization and PC. However, after controlling for anxiety and depression, PC was the only significant pathway through which alexithymia was related to headache impact.
Conclusions
Headache patients may benefit from interventions aiming at improving psychological factors in order to improve the functioning and QOL of headache patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Headaches are a global health concern with 46% of the adult population having an active headache disorder with a considerable disease burden [1]. Quality of life (QOL) is negatively affected in headache patients featuring a lower level of QOL than that of the general population [2, 3]. In fact, in a study of 901 patients with headache, headache patients scored lower on almost all dimensions of the SF-36, with a particular decline observed in the role limitations due to physical and emotional problems as well as in bodily pain compared to the norm [3]. The psychological burden of the disease is also considerable in 65.9% of patients with chronic migraines from the community setting and 83.7% of those diagnosed with chronic migraines from the headache center having psychiatric diagnoses [4].
Previous studies suggest that in addition to sociodemographic (e.g., age) and clinical characteristics (e.g., frequency and duration of pain, pain severity, duration) [2, 5], psychological factors play a significant role in the degree to which headache impacts overall functioning or QOL in individuals.
Alexithymia is a psychological factor that has received considerable attention, and it refers to difficulties in distinguishing various emotions, and describing emotions, and having a restricted imagination, as well as a tendency toward externally oriented rather than toward internally oriented thinking [6]. Studies have suggested its association with various psychiatric illnesses such as somatoform disorder and depression [7] and physical health problems such as medically unexplained symptoms [8] and chronic tension headaches [9]. In fact, previous findings suggest that alexithymia appears to be higher in headache patients than in headache-free individuals [10,11,12], and for example, patients who had chronic headache without known organic causes were more alexithymic than either headache patients with known organic causes or healthy individuals [11]. Moreover, alexithymia was negatively associated with QOL in women with migraines [13], as well as higher pain intensity and interference in chronic pain patients [14]. Also, a high level of headache impact measured by Headache Impact Test-6 (HIT-6) was significantly associated with poor QOL [15].
As noted, previous studies suggest that a high level of alexithymia in headache patients was associated with poor outcomes. However, the potential pathways or mechanisms through which alexithymia may influence these outcomes, such as headache impact, are under-studied.
Previously observed associations of alexithymia with somatization and pain catastrophizing, which are factors known to be related to QOL and headache-related disability [16, 17] indicate possible mediating pathways. Above all, somatization, generally defined as the experience of somatic symptoms that are “not explained by a general medical condition” [18], may mediate the alexithymia–headache impact relationship. In fact, a systematic review suggests a small-to-moderate relationship between alexithymia and somatization, and found that individuals with somatoform disorder or functional somatic syndromes were more alexithymic compared to healthy controls, with moderate to large effect sizes [19]. This relationship was also confirmed in headache patients, and in a study of non-organic chronic headache patients, 91.4% of participants in somatizers had alexithymia, as compared to 28.6% of non-somatizers [11]. Moreover, the relationship between somatization and headache impact was observed, and greater somatic symptom prevalence and severity was related to severe headache-related disability in a study with 1032 women with headache [17]. Similarly, somatic symptoms were related to chronicity and greater severity of headache as well as to anxiety or depression in headache patients [20].
Pain catastrophizing (PC), defined as “an exaggerated negative orientation to actual or anticipated pain” (p. 32) [21], is another potential psychological factor that might mediate the relationship between alexithymia and headache impact. A positive correlation between alexithymia and PC was observed in individuals with fibromyalgia [22] and patients with chronic pain [23] as well as in university students [24]. Also, prior findings suggest the role of PC in determining the impact of pain on functioning in headache patients. For instance, PC was associated with an impaired functioning and QOL for severe migraine patients [16], and it was related to greater pain-related interference as well as severity of headache pain [25]. Higher PC was also associated with higher HIT-6 scores and a lower level of headache management self-efficacy in women with migraine [26]. Similarly, catastrophizing along with pain self-efficacy (e.g., pain management, coping with symptoms, and physical functioning) accounted for the relationship between alexithymia and physical impairment in chronic myofascial pain [27], and mediated the relationship between alexithymia and physical symptoms in asthmatic patients [28].
These findings suggest that somatization and PC might also act as potential mediators in the relationship between alexithymia and headache impact in patients with headache. However, while previous studies examined the relationship between alexithymia and headache-related outcomes, the potential mechanisms by which alexithymia may influence headache-related outcomes such as headache impact are under-studied. An understanding of the mediators of the alexithymia–headache impact relationship may allow clinicians to identify effective and feasible intervention targets for patients with headache to reduce the negative influence of alexithymia on headache-related outcomes, thereby improving the overall QOL for these patients.
Thus, the aims of the present study are to (1) compare the level of alexithymia, somatization, PC, and QOL between headache patients and healthy controls; and (2) to examine the mediating role of somatization and PC in the relationship between alexithymia and headache impact for headache patients. Based on the previous findings that the association of alexithymia with pain interference and catastrophizing became non-significant after controlling for anxiety and depression in chronic pain [23], and the well-established association of psychological comorbidity with headache impact [29], the mediating role of somatization and PC was examined both with and without anxiety and depression as covariates.
Methods
Participants and procedures
A case–control study was carried out as part of a hospital-based study that examined the impact of psychiatric and psychosocial problems on primary headache. We consecutively recruited patients with migraine or tension-type headache who visited an outpatient clinic in the Department of Neurology at Kyungpook National University Hospital from September 2012 to March 2013. During the study period, eligible patients were identified through a review of medical records. Research staff approached these patients when they visited an outpatient clinic in the Department of Neurology and explained the purpose and procedure of the survey. A diagnosis of migraine was determined based on the International Classification of Headache Disorders, second edition (ICHD-2) [30]. Patients aged between 13 and 70 years were included. Patients were excluded if they had illiteracy, mental retardation, serious medical, neurological or psychiatric disorders, and alcohol or drug abuse that prevented them from cooperating with the study. Of 148 patients who visited our clinic, 25 were excluded from this study due to refusal to participate (n = 11), probable primary headache (n = 8), serious medical or neurological disorders (n = 3), age older than 70 years (n = 2), and illiteracy (n = 1). Finally, 123 patients were eligible for this study. Of them, 91 patients were suitable for the diagnosis of migraine and 32 patients were appropriate for the diagnosis of tension-type headache. Upon the completion of patient recruitment, we recruited age- and sex-matched healthy controls without headache using convenience sampling, and 124 healthy controls were recruited. They were university students, office workers, teachers, and hospital employees.
Eligible subjects who agreed to participate in the study completed self-reported questionnaires on their visit to outpatient clinic. The study was approved by the institutional review board of Kyungpook National University Hospital. Written informed consent was obtained from all participants.
Measures
Alexithymia was assessed using the Korean version of the 20-item Toronto Alexithymia Scale (TAS-20) [31]. The TAS-20 is composed of three subscales: difficulty describing feelings (5); difficulty in identifying feelings (7); and externally oriented thinking (8). The participants rated each item using a 5-point Likert scale (1= “strongly disagree” to 5= “strongly agree”), and five items were negatively keyed. The total score ranges from 20 to 100, and a higher score denotes a higher level of alexithymia. Cronbach’s alpha of the Korean version of the TAS-20 was 0.76 for the total scale.
Somatization and anxiety were assessed by respective subscales from the Korean version of the Symptom Checklist-90-revised (SCL-90-R): somatization (12 items) and anxiety (10 items) [32]. Participants rated each item on a five-point scale (0=‘not at all’ − 4=‘extremely’), with higher score indicating a higher level of somatization (range 0–48) and anxiety (range 0–40). Cronbach’s α for somatization and anxiety subscale of SCL-90-R were 0.85 and 0.90, respectively.
Pain catastrophizing (PC) was measured utilizing the Pain Catastrophizing Scale (PCS) [33]. The PCS comprises three subscales: helplessness (6); magnification (3); and rumination (4). Participants indicated the degree to which they experienced 13 pain-related thoughts or feelings on a five-point Likert scale (0 = ‘not at all’ – 4 = ‘all the time’). The score ranges from 0 to 52, with higher scores indicating a higher PC tendency. Cronbach’s α for Korean version of PCS was 0.93 for the total scale [33].
Depression was assessed according to the Korean version of Patient Health Questionnaire (PHQ-9) [34]. Nine major symptoms of depression were rated on a four-point scale ranging from 0 (‘not at all’) to 3 (‘nearly every day’) encompassing the prior two weeks, with total scores ranging from 0 to 27. Higher scores denote more severe depressive symptoms. The Korean version of the PHQ-9 has been validated in patients with migraine [34]. A cutoff score of 7 has been suggested as a score for differentiating MDD. Cronbach’s α for the Korean PHQ-9 was 0.89.
Quality of life was measured using the Short-Form Health survey (SF-8: 4-week recall) [35]. The SF-8 assesses eight dimensions of health: general health, physical functioning, role physical, bodily pain, vitality, social functioning, mental health, and role emotional. SF-8 also determines two summary scores, i.e., physical component score (PCS) and mental component score (MCS). Scores for each item as well as summary scores range from 0 to 100, with higher scores indicating better status in the respective dimension. Cronbach’s α for the total scale was 0.84.
Headache impact was assessed utilizing the Korean version of the Headache impact test-6 (HIT-6) [36]. The HIT-6 contains six items assessing pain, social functioning, role functioning, cognitive functioning, psychological distress, and vitality. Participants rated each item on a five-point scale (from ‘never’ to ‘always’), resulting in a total between 6 (never) and 13 (always) points in each category. The total score of HIT-6 ranges between 36 and 78. Four categories of headache impact were employed: little or no impact (49 or less), some impact (50–55), substantial impact (56–59), and severe impact (60–78) [37]. Cronbach’s α of the Korean version of the HIT-6 was 0.85 [36].
Questions regarding demographic and socioeconomic data were also included. For clinical data, we asked patients for family history of headache, psychiatric history, concurrent medical disease, headache days, and headache intensity. Headache days refer to a calendar day of headache in the preceding month. Headache intensity was assessed by the visual analog scale (VAS). Average headache intensity in the preceding month and headache intensity at the time of survey completion were measured and denoted as VASavg and VASnow, respectively.
Statistical analyses
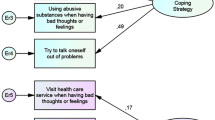
To examine whether the three groups (i.e., healthy controls, migraine, and tension-type headache) differ in terms of sociodemographic and clinical variables, Chi-square tests, t tests, and analyses of variance were conducted. Analysis of covariance (ANCOVA) was performed to compare the study variables across three groups, and when there were significant differences between the groups, post hoc tests (i.e., Fisher’s least significant differences, or LSD) were performed to determine which specific groups differed. Pearson correlation analysis was conducted to examine inter-correlations among study variables in headache patients. To test whether somatization and PC mediate the relationship between alexithymia and headache impact in headache patients, we tested a multiple mediation model in which alexithymia is hypothesized to influence the impact of headache through its association with mediators (somatization and PC) [38]. Specifically, three indirect paths are possible (see Fig. 1): (1) through somatization (a1b1); (2) through somatization and PC (a1d21b2); and (3) through PC (a2b2). To test the significance of indirect effects, the Preacher and Hayes’ bootstrapping method [39] was used. All statistical analyses were performed using the Statistical Package for the Social Sciences (SPSS 21) version for Windows [40].
Results
Demographic, socioeconomic, and clinical characteristics across three groups
Demographic, socioeconomic, and clinical characteristics of participants across three groups (healthy control, patients with migraine, and those with tension-type headache) are shown in Table 1. Examination of the sociodemographic variables across three groups showed that age and education level differed significantly. The mean age of tension-type headache patients (M = 44.7, SD = 14.7) was higher than that of the other two groups (M = 35.0, SD = 1.3 for migraine; M = 37.2, SD = 12.4 for healthy controls) [F(2, 244) = 7.078, p < .001]. Regarding education, the rate of college or university level education was higher in the healthy control group compared with patients with migraines or tension-type headaches. The rate of high school education was higher in migraine patients than the healthy control group, and the rate of less than a high school education was higher in tension-type headache patients than the other two groups (χ2(4) = 41.211, p < .001).
Examination of the clinical variables between patients with migraines and those with tension-type headaches showed that the two groups differed in the rate of comorbid internal disease, headache days, and VASnow. The rate of comorbid medical disease was significantly higher in the tension-type headache group (46.9%) than in the migraine group (17.6%)(χ2(1) = 10.776, p < .001). The percentage of patients who had 1–2 headache days in the past month was higher in the migraine group (23.3%) compared with the tension-type group (3.1%), and the percentage of patients who experienced headaches in excess of 11 days was higher in the tension-type group (65.6%) than in the migraine group (32.2%) (χ2(3) = 13.047, p <. 01). VASnow was higher in the tension-type group (M = 3.1, SD = 2.1) as compared to the migraine group (M = 2.2, SD = 2.3) (t (121) = − 2.048, p < .05).
Study variables across three groups
The main study variables across the three groups were examined using ANCOVA. Age and education, which showed significant group differences, were entered as covariates (Table 2). As HIT-6 scores were compared between the two headache groups, clinical variables (comorbid medical disease, headache days) that showed significant group differences were also entered as covariates. All study variables showed a significant group difference except for the HIT-6 scores. Patients with migraine and those with tension-type headache did not significantly differ for the HIT-6 scores (F(1, 115) = 3.785, p = .054).
Alexithymia was highest in the tension-type headache group, followed by the migraine group and healthy controls. The TAS-20 subscale score of ‘difficulty of identifying feeling’ was higher for the headache groups than the healthy controls. ‘Difficulty describing feelings’ was higher in the tension-type headache group than the migraine group and healthy controls. ‘Externally oriented thinking’ was higher in the tension-type headache groups than healthy controls. The level of somatization, PC, anxiety, and depression was higher in the headache groups than healthy controls. The helplessness subscale score of PCS was highest in the migraine group, followed by tension-type and healthy controls. Two summary scores of PCS and MCS as well as the seven dimensions of SF-8 were significantly higher in the healthy control group compared to the headache groups. Physical functioning was significantly lower in migraine group than in healthy controls.
Inter-correlations among study variables in headache patients
Results of correlation analysis for the main study variables are shown in Table 3. Headache impact positively correlated with alexithymia (r = .239**), somatization(r = .451**) , and PC (r = .595**). Anxiety and depression were significantly associated with alexithymia, somatization, PC, and headache impact, and their associations with alexithymia were relatively high (r = .658** and .636**, respectively). The correlation between anxiety and somatization was also high (r = .624**).
The mediating role of somatization and PC in the relationship between alexithymia and headache impact
The mediating role of somatization and PC in the relationship between alexithymia and headache impact was examined using multiple mediation analysis. As correlations of alexithymia with anxiety (r = .658**) and depression (r = .636**) were high, we conducted analyses both with and without anxiety and depression as covariates. To identify covariates of outcome and mediator variables, we examined their correlations with sociodemographic and clinical variables. Headache days (r = .430***), VASavg (r = .327***) , and VASnow (r = .201***) showed a significant association with headache impact. Regarding somatization, education (r = − .166*), monthly income (r = − .150*), religion (r = .173**), headache days (r = .344***), VASavg (r = .184*), VASnow (r = .390***), and psychiatric consultation history (r = − .284**) showed significant correlations. Concerning PC, education (r = − .205***), headache days (r = .240***), and VASavg (r = .251**) showed significant associations. Therefore, education, monthly income, religion, the type of diagnosis, headache days, VASavg and VASnow, and psychiatric consultation history were entered as covariates. The results are shown in Table 4 and illustrated in Fig. 1.
The direct effect of alexithymia on headache impact (c′) was not statistically significant after controlling for mediators (somatization and PC) in both analyses. Without controlling for anxiety and depression, the total indirect effects of alexithymia on the HIT were significant with three mediational pathways being significant. First, alexithymia was associated with the HIT through somatization (a1b1 = .046, CI .010- .099). Second, alexithymia was also significantly associated with the HIT through somatization and PC (a1d21b2 = .028, CI .010–.062.). Third, alexithymia was associated with HIT via PC (a2b2 = .102, CI .048–.195).
However, when we controlled for anxiety and depression, the total indirect effect of the alexithymia on the HIT was not significant. Only the indirect effect of alexithymia on the HIT via PC (a2b2 = .088, CI .022–.190) remained significant.
Discussion
The present study examined whether psychological factors (i.e., alexithymia, somatization, anxiety, depression, and PC) and QOL of headache patients significantly differ from those of headache-free controls. Furthermore, the study examined whether somatization and PC mediate the relationship between alexithymia and headache impact in headache patients.
All psychological factors were significantly higher in headache patients than in headache-free counterparts. Specifically, alexithymia was highest in patients with tension-type headaches, followed by those with migraines and healthy controls [10, 12, 41]. The TAS-20 subscale score of ‘Difficulty of identifying feeling’ was higher in headache patients than in healthy controls. ‘Difficulty describing feeling’ was higher in patients with tension-type headaches than in those with migraine and health controls. Externally oriented thinking was higher in patients with tension-type headache than healthy controls. The levels of somatization, PC, anxiety, and depression were also higher in headache groups than healthy controls, while these psychological factors did not significantly differ according to the type of headache. This finding might reflect previous findings that suggested psychiatric disorder in patients with primary headache is more a reflection of the disease burden rather than a characteristic of the certain type of headache category [42]. Although we cannot determine whether the higher levels of these psychological factors observed in headache patients are vulnerability factors to headache condition or consequences of headache experience due to the cross-sectional design of this study, it underscores the need to address psychological factors in the care of headache patients.
Consistent with previous findings [3, 43], QOL, as defined by the two summary scores of PCS and MCS as well as the seven dimensions of the SF-8, was significantly higher in healthy controls compared to headache groups, suggesting a considerable disease burden associated with headache [1], particularly the pervasive negative impact of headache on QOL of those affected individuals. The magnitude of the differences between headache patients and healthy controls appears greater in the QOL dimensions of general health, role physical, and bodily pain. Regarding the headache impact as measured by the HIT-6, patients with migraines and those with tension-type headaches did not significantly differ in line with previous findings [44]. This might suggest that other factors such as emotional distress [45] or chronicity of headache [46] rather than just type of headache are more important in determining the headache impact.
With regard to whether somatization and PC mediate the relationship between alexithymia and headache impact, due to the relatively high correlations of alexithymia with anxiety and depression, mediation models were tested both with and without anxiety and depression as covariates. Results showed that the direct effect of alexithymia on the headache impact was not significant after controlling for mediators (somatization and PC) in both analyses, which is in line with previous findings. In fact, the relationship between alexithymia and physical impairment found in patients with chronic myofascial pain became non-significant after controlling for the psychological factors of self-efficacy, catastrophizing, and depression [27]. Similarly, the association of alexithymia with pain interference was no longer significant after controlling for anxiety and depression in Japanese chronic pain patients [23]. These and current findings might suggest that alexithymia may be more of a distal risk factor that affects headache impact through its association with somatization or PC, which may be considered proximal risk factors of headache impact.
Conversely, the total indirect effects of alexithymia on headache impact were significant without anxiety and depression as covariates, with significant indirect effects of alexithymia via somatization or via PC as well as via somatization and PC. However, when controlling for anxiety and depression, only the indirect effect of alexithymia via PC remained significant. The finding that the indirect effects of alexithymia on headache impact via somatization or via somatization and PC being not significant after controlling for anxiety and depression might be due to high correlations of somatization with anxiety and depression. In support of this finding, a study involving 2091 primary care patients found that over 50% of these patients had comorbidities of depression, anxiety, and somatization, and an overlap effect of these comorbidities on functional impairment was observed [47]. Similarly, greater disability and high somatic symptom severity were related to major depressive disorder in women with headache [17]. This result also might reflect the significant role of anxiety and depression in headache impact observed in previous findings with headache patients [5]. In fact, comorbid mental disorder accounted for 65% of role disability related to migraines and all of the role disability associated with other headaches [29]. Moreover, high levels of anxiety and depressive symptoms were associated with lower QOL in various dimensions in patients with migraine and chronic daily headaches [48]. Given that the impact of anxiety and depression is pervasive with its significant association not only with perception of headache pain and headache-related disability but also with headache treatment adherence and outcome [49], as well as a positive association between alexithymia and depression [50] and anxiety [10, 50] in headache patients also observed in this study, a clinical attention to these psychological comorbidities in the care of headache patients needs to be warranted.
The result that PC was the only significant pathway through which alexithymia was related to the headache impact even after considering the impact of anxiety and depression might suggest the significant role of this factor in the functioning of individuals with headache. In fact, catastrophizing was associated with an impaired functioning and QOL independent of demographic, clinical, and psychological variables in migraine patients [16], and was related to greater headache pain and pain-related interference [25]. Furthermore, the mediating role of PC in the relationship between alexithymia and physical symptoms was observed in patients with asthma [28] and in the relationship between pain intensity and depressed mood in older adults with persistent pain [51]. Taken together, the current and previous findings underscore the importance of promoting more adaptive coping rather than catastrophizing to moderate the effect of headache on overall daily functioning or QOL.
Regarding the positive association of alexithymia with PC, it might be in part due to the association between alexithymia and a heightened sensitivity or low tolerance to unpleasant stimuli [52]. In fact, a lower pain threshold along with the tendency of exaggerating pain experience appears to be prominent in chronic headache patients without known obvious organic causes [11]. Also, a review on how alexithymia influences illness behavior, such as physical symptoms or disability in individuals with physical illness, suggested that individuals with difficulty in identifying and regulating emotions are more likely to experience physiological arousal and biased perception, which might lead to increased physical symptom complaints [53] associated with increased PC. In addition, greater attentional bias for pain-related information observed in chronic daily headache sufferers [54] might be another potential explanatory factor behind PC in individuals with pain. However, it is also possible that a personality trait such as neuroticism, which is known to be higher in headache patients [55], might be an underlying factor behind PC as well as somatization. In a similar vein, a review on the link between alexithymia and physical illness suggests that alexithymia is associated with neuroticism and related negative affectivity, which increases somatic complaints [53].
The current findings need to be considered within their limitations. First, due to the insufficient sample size, mediation analyses were conducted including migraine and tension-type headache patients with the type of headache as a covariate. The level of headache impact did not differ significantly according to the type of headache in the preliminary analyses. However, as migraine patients constituted the majority of headache patients and there are also studies suggesting a difference in QOL between these two types of headaches [56], it is necessary to re-examine the study hypotheses separately with an adequate sample size. In a related matter, previous studies suggest that chronic and episodic headache show different clinical features, with the chronicity of headache being associated with higher psychological comorbidity [50], high catastrophizing [57], high headache impact [5, 37], and lower QOL [58]. However, it was not possible to perform separate analyses in our study due to a small sample size. Third, due to the cross-sectional design of the present study, a causal interpretation regarding the proposed relationship among study variables cannot be made. For instance, alexithymia might be an emotional reaction to physical illness [53], and higher headache-related interference might cause psychological distress, suggesting a bi-directional nature of the relationship among study variables. The findings of the present study should be re-examined in a prospective and longitudinal design. Moreover, the patients were recruited from a single-study site, limiting the generalizability of our findings.
Despite these limitations, the present study highlights the significant role of psychological factors, such as PC as well as psychological comorbidity of anxiety and depression in headache-related interference, which suggests the need for addressing these factors in the care of headache patients. The need for considering these factors are further recommended by previous findings that catastrophizing was one of the psychological variables showing the strongest associations with an inadequate treatment response in migraine patients [59]. Furthermore, along with headache impact and psychological distress, coping characterized by catastrophizing and avoidance were related to chronicity of headache [57]. In addition, previous studies observed an inverse relationship of pain-related acceptance with catastrophizing and pain-related interference in patients with migraine [60] and with chronic pain [61], suggesting acceptance of pain as a way to lessen the detrimental impacts of catastrophizing and increase engagement in daily life [60, 62]. Similarly, the moderating role of mindfulness in the relationship between pain intensity and PC in chronic pain patients was observed [63]. Cognitive-behavioral treatment is a viable approach in that its efficacy was proven with a significant reduction in catastrophizing and anxiety, as well as meaningful changes in headache-related indices in chronic headache sufferers [25]. Moreover, interventions based on acceptance and commitment therapy (ACT) with chronic pain patients improved PC [64], depression [64, 65], pain-related anxiety [65], pain intensity [64], and interference [64, 65]. ACT was also effective with female chronic headache patients with significant improvement in disability and trait anxiety [66]. Moreover, as clinical characteristics such as frequency [2] and duration of headache [5], as well as VASavg and VASnow [5, 16] were significantly associated with headache impact as well as somatization and PC in this study, these clinical characteristics should be monitored in the clinical care of headache patients.
To conclude, the present study found that PC as well as somatization might be mediating factors that link alexithymia and headache impact, illustrating one of the manners in which these psychological factors interrelate in predicting overall functioning and QOL of headache patients. Headache patients may benefit from interventions aiming at improving these psychological factors in order to improve headache-related outcomes.
Abbreviations
- ANCOVA:
-
Analysis of covariance
- ACT:
-
Acceptance and commitment therapy
- HIT-6:
-
Headache Impact Test -6
- PC:
-
Pain catastrophizing
- PHQ-9:
-
Patient Health Questionnaire 9
- QOL:
-
Quality of life
- SF-8:
-
Short-Form Health survey
- SCL-90-R:
-
Symptom Checklist-90-revised
- TAS-20:
-
Toronto Alexithymia Scale-20
References
Stovner, L., Hagen, K., Jensen, R., Katsarava, Z., Lipton, R., Scher, A., et al. (2007). The global burden of headache: A documentation of headache prevalence and disability worldwide. Cephalalgia, 27(3), 193–210.
Uthaikhup, S., Sterling, M., & Jull, G. (2009). Psychological, cognitive and quality of life features in the elderly with chronic headache. Gerontology, 55(6), 683–693.
Wang, S.-J., Fuh, J.-L., Lu, S.-R., & Juang, K.-D. (2001). Quality of life differs among headache diagnoses: analysis of SF-36 survey in 901 headache patients. Pain, 89(2), 285–292.
Teixeira, A. L., Costa, E. A. C., da Silva Jr, A. A., dos Santos, I. A. M., Gómez, R. S., Kummer, A., & Lauterbach, E. C. (2012). Psychiatric comorbidities of chronic migraine in community and tertiary care clinic samples. The Journal of Headache and Pain, 13(7), 551–555.
Buse, D., Manack, A., Serrano, D., Reed, M., Varon, S., Turkel, C., & Lipton, R. (2012). Headache impact of chronic and episodic migraine: Results from the American Migraine Prevalence and Prevention study. Headache: The Journal of Head and Face Pain, 52(1), 3–17.
Kooiman, C., Spinhoven, P., & Trijsburg, R. (2002). The assessment of alexithymia: A critical review of the literature and a psychometric study of the Toronto Alexithymia Scale-20. Journal of Psychosomatic Research, 53(6), 1083–1090.
Bankier, B., Aigner, M., & Bach, M. (2001). Alexithymia in DSM-IV disorder: comparative evaluation of somatoform disorder, panic disorder, obsessive-compulsive disorder, and depression. Psychosomatics, 42(3), 235–240.
De Gucht, V., Fischler, B., & Heiser, W. (2004). Neuroticism, alexithymia, negative affect, and positive affect as determinants of medically unexplained symptoms. Personality and Individual Differences, 36(7), 1655–1667.
Esin, O., Gorobets, E., Khairullin, I., & Esin, R. (2016). Alexithymia as a predictor of chronic tension headaches. BioNanoScience, 6(4), 1–4.
Muftuoglu, M. N., Herken, H., Demirci, H., Virit, O., & Neyal, A. (2004). Alexithymic features in migraine patients. European Archives of Psychiatry and Clinical Neuroscience, 254(3), 182–186.
Okasha, A., Ismail, M. K., Khalil, A. H., El Fiki, R., Soliman, A., & Okasha, T. (1999). A psychiatric study of nonorganic chronic headache patients. Psychosomatics, 40(3), 233–238.
Yücel, B., Kora, K., Özyalçín, S., Alçalar, N., Özdemir, Ö, & Yücel, A. (2002). Depression, automatic thoughts, alexithymia, and assertiveness in patients with tension-type headache. Headache: The Journal of Head and Face Pain, 42(3), 194–199.
de Andrade Vieira, R. V., Vieira, D. C., Gomes, W. B., & Gauer, G. (2013). Alexithymia and its impact on quality of life in a group of Brazilian women with migraine without aura. The Journal of Headache and Pain, 14(1), 18.
Hosoi, M., Molton, I. R., Jensen, M. P., Ehde, D. M., Amtmann, S., O’Brien, S., et al. (2010). Relationships among alexithymia and pain intensity, pain interference, and vitality in persons with neuromuscular disease: Considering the effect of negative affectivity. PAIN®, 149(2), 273–277.
Nachit-Ouinekh, F., Dartigues, J. F., Henry, P., Becg, J. P., Chastan, G., Lemaire, N., et al. (2005). Use of the headache impact test (HIT-6) in general practice: relationship with quality of life and severity. European Journal of Neurology, 12(3), 189–193.
Holroyd, K., Drew, J., Cottrell, C., Romanek, K., & Heh, V. (2007). Impaired functioning and quality of life in severe migraine: The role of catastrophizing and associated symptoms. Cephalalgia, 27(10), 1156–1165.
Tietjen, G., Brandes, J., Digre, K., Baggaley, S., Martin, V., Recober, A., Geweke, L., Hafeez, F., Aurora, S., & Herial, N. (2007). High prevalence of somatic symptoms and depression in women with disabling chronic headache. Neurology, 68(2), 134–140.
Mayou, R., Kirmayer, L. J., Simon, G., Kroenke, K., & Sharpe, M. (2005). Somatoform disorders: time for a new approach in DSM-V. American Journal of Psychiatry, 162(5), 847–855.
De Gucht, V., & Heiser, W. (2003). Alexithymia and somatisation: a quantitative review of the literature. Journal of Psychosomatic Research, 54(5), 425–434.
Maizels, M., & Burchette, R. (2004). Somatic symptoms in headache patients: The influence of headache diagnosis, frequency, and comorbidity. Headache: The Journal of Head and Face Pain, 44(10), 983–993.
Sullivan, M. J. (2012). The communal coping model of pain catastrophising: Clinical and research implications. Canadian Psychology/Psychologie canadienne, 53(1), 32.
Martínez, M. P., Sánchez, A. I., Miró, E., Lami, M. J., Prados, G., & Morales, A. (2015). Relationships between physical symptoms, emotional distress, and pain appraisal in fibromyalgia: The moderator effect of alexithymia. The Journal of Psychology, 149(2), 115–140.
Makino, S., Jensen, M. P., Arimura, T., Obata, T., Anno, K., Iwaki, R., et al. (2013). Alexithymia and chronic pain: the role of negative affectivity. The Clinical Journal of Pain, 29(4), 354–361.
Katz, J., Martin, A. L., Pagé, M. G., & Calleri, V. (2009). Alexithymia and fear of pain independently predict heat pain intensity ratings among undergraduate university students. Pain Research and Management, 14(4), 299–305.
Buenaver, L. F., Edwards, R. R., Smith, M. T., Gramling, S. E., & Haythornthwaite, J. A. (2008). Catastrophizing and pain-coping in young adults: Associations with depressive symptoms and headache pain. The Journal of Pain, 9(4), 311–319.
Bond, D. S., Buse, D. C., Lipton, R. B., Thomas, J. G., Rathier, L., Roth, J., et al. (2015). Clinical pain catastrophizing in women with migraine and obesity. Headache: The Journal of Head and Face Pain, 55(7), 923–933.
Lumley, M. A., Smith, J. A., & Longo, D. J. (2002). The relationship of alexithymia to pain severity and impairment among patients with chronic myofascial pain: Comparisons with self-efficacy, catastrophizing, and depression. Journal of Psychosomatic Research, 53(3), 823–830.
Ghorbani, F., Khosravani, V., Ardakani, R. J., Alvani, A., & Akbari, H. (2017). The mediating effects of cognitive emotion regulation strategies on the relationship between alexithymia and physical symptoms: Evidence from Iranian asthmatic patients. Psychiatry Research, 247, 144–151.
Saunders, K., Merikangas, K., Low, N., Von Korff, M., & Kessler, R. (2008). Impact of comorbidity on headache-related disability. Neurology, 70(7), 538–547.
Headache Classification Committee of the International Headache Society (IHS). (2004). The international classification of headache disorders. Cephalalgia, 24(Suppl1), 9–160.
Lee, Y. H., Rim, J. Y., Lee, J. Y. (1996). Development and validation of a Korean version of the 20-item Toronto Alexithymia Scale (TAS-20K). Journal of Korean Neuropsychiatric Association, 35(4), 888–899.
Kim, K. I., Kim, K. J., Won, H. T. (1984). Korean manual of Symptom Checklist-90-Revision. Seoul: Seoul Jung Ang Juk Sung Publisher.
Cho, S., Kim, H. Y., & Lee, J. H. (2013). Validation of the Korean version of the Pain Catastrophizing Scale in patients with chronic non-cancer pain. Quality of Life Research, 22(7), 1767–1772.
Seo, J.-G., & Park, S.-P. (2015). Validation of the Patient Health Questionnaire-9 (PHQ-9) and PHQ-2 in patients with migraine. The Journal of Headache and Pain, 16(1), 65.
Ware, J. E., Kosinski, M., Dewey, J. E., & Gandek, B. (2001). How to score and interpret single-item health status measures: A manual for users of the SF-8 health survey, Vol. 15. Lincoln, RI: QualityMetric Incorporated.
Chu, M. K., Im, H. J., Ju, Y. S., Yu, K. H., Ma, H. I., Kim, Y. J., Kim, J., & Lee, B. C. (2009). Validity and reliability assessment of Korean headache impact test-6 (HIT-6). Journal of the Korean Neurological Association, 27(1), 1–6.
Yang, M., Rendas-Baum, R., Varon, S. F., & Kosinski, M. (2011). Validation of the Headache Impact Test (HIT-6™) across episodic and chronic migraine. Cephalalgia, 31(3), 357–367.
Hayes, A. F. (2013). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. New York: Guilford Press.
Preacher, K. J., & Hayes, A. F. (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods, 40(3), 879–891.
Hayes, A. F. (2012). PROCESS: A versatile computational tool for observed variable mediation, moderation, and conditional process modeling. Lawrence, KS: University of Kansas.
Gatta, M., Canetta, E., Zordan, M., Spoto, A., Ferruzza, E., Manco, I., et al. (2011). Alexithymia in juvenile primary headache sufferers: A pilot study. The Journal of Headache and Pain, 12(1), 71–80.
Beghi, E., Allais, G., Cortelli, P., D’amico, D., De Simone, R., d’Onofrio, F., et al. (2007). Headache and anxiety–depressive disorder comorbidity: The HADAS study. Neurological Sciences, 28(2), S217–S219.
Lipton, R. B., Liberman, J., Kolodner, K., Bigal, M., Dowson, A., & Stewart, W. (2003). Migraine headache disability and health-related quality-of-life: A population-based case-control study from England. Cephalalgia, 23(6), 441–450.
Bera, S. C., Khandelwal, S. K., Sood, M., & Goyal, V. (2014). A comparative study of psychiatric comorbidity, quality of life and disability in patients with migraine and tension type headache. Neurology India, 62(5), 516.
Holroyd, K. A., Stensland, M., Lipchik, G. L., Hill, K. R., O’Donnell, F. S., & Cordingley, G. (2000). Psychosocial correlates and impact of chronic tension-type headaches. Headache: The Journal of Head and Face Pain, 40(1), 3–16.
Lantéri-Minet, M., Duru, G., Mudge, M., & Cottrell, S. (2011). Quality of life impairment, disability and economic burden associated with chronic daily headache, focusing on chronic migraine with or without medication overuse: a systematic review. Cephalalgia, 31(7), 837–850.
Löwe, B., Spitzer, R. L., Williams, J. B., Mussell, M., Schellberg, D., & Kroenke, K. (2008). Depression, anxiety and somatization in primary care: Syndrome overlap and functional impairment. General Hospital Psychiatry, 30(3), 191–199.
Paschoal, J. K., Lin, J., Pinho, R. S., Andreoni, S., Minett, T. S., Vitalle, M. S., et al. (2013). Psychiatric symptoms may contribute to poor quality of life in adolescents with migraine. Pediatrics International, 55(6), 741–747.
Nicholson, R. A., Houle, T. T., Rhudy, J. L., & Norton, P. J. (2007). Psychological risk factors in headache. Headache: The Journal of Head and Face Pain, 47(3), 413–426.
Yalug, I., Selekler, M., Erdogan, A., Kutlu, A., Dundar, G., Ankaralı, H., et al. (2010). Correlations between alexithymia and pain severity, depression, and anxiety among patients with chronic and episodic migraine. Psychiatry and Clinical Neurosciences, 64(3), 231–238.
Wood, B. M., Nicholas, M. K., Blyth, F., Asghari, A., & Gibson, S. (2016). The mediating role of catastrophizing in the relationship between pain intensity and depressed mood in older adults with persistent pain: A longitudinal analysis. Scandinavian Journal of Pain, 11, 157–162.
Nyklíček, I., & Vingerhoets, A. J. (2000). Alexithymia is associated with low tolerance to experimental painful stimulation. Pain, 85(3), 471–475.
Lumley, M. A., Stettner, L., & Wehmer, F. (1996). How are alexithymia and physical illness linked? A review and critique of pathways. Journal of Psychosomatic Research, 41(6), 505–518.
Liossi, C., Schoth, D. E., Bradley, B. P., & Mogg, K. (2009). Time-course of attentional bias for pain-related cues in chronic daily headache sufferers. European Journal of Pain, 13(9), 963–969.
Aaseth, K., Grande, R., Leiknes, K., Benth, J., Lundqvist, C., & Russell, M. (2011). Personality traits and psychological distress in persons with chronic tension-type headache. The Akershus study of chronic headache. Acta Neurologica Scandinavica, 124(6), 375–382.
Monzon, M., & Lainez, M. (1998). Quality of life in migraine and chronic daily headache patients. Cephalalgia, 18(9), 638–643.
Radat, F., Lantéri-Minet, M., Nachit-Ouinekh, F., Massiou, H., Lucas, C., Pradalier, A., et al. (2009). The GRIM2005 study of migraine consultation in France. III: Psychological features of subjects with migraine. Cephalalgia, 29(3), 338–350.
Duru, G., Auray, J. P., Gaudin, A. F., Dartigues, J. F., Henry, P., Lantéri-Minet, M., et al. (2004). Impact of headache on quality of life in a general population survey in France (GRIM2000 Study). Headache: The Journal of Head and Face Pain, 44(6), 571–580.
Lucas, C., Lanteri-Minet, M., Massiou, H., Nachit-Ouinekh, F., Pradalier, A., Mercier, F., et al. (2007). The GRIM2005 study of migraine consultation in France II. Psychological factors associated with treatment response to acute headache therapy and satisfaction in migraine. Cephalalgia, 27(12), 1398–1407.
Chiros, C., & O’Brien, W. H. (2011). Acceptance, appraisals, and coping in relation to migraine headache: An evaluation of interrelationships using daily diary methods. Journal of Behavioral Medicine, 34(4), 307–320.
Viane, I., Crombez, G., Eccleston, C., Poppe, C., Devulder, J., Van Houdenhove, B., et al. (2003). Acceptance of pain is an independent predictor of mental well-being in patients with chronic pain: Empirical evidence and reappraisal. Pain, 106(1), 65–72.
McCracken, L. M., & Eccleston, C. (2003). Coping or acceptance: what to do about chronic pain? Pain, 105(1), 197–204.
Schütze, R., Rees, C., Preece, M., & Schütze, M. (2010). Low mindfulness predicts pain catastrophizing in a fear-avoidance model of chronic pain. Pain, 148(1), 120–127.
Trompetter, H. R., Bohlmeijer, E. T., Veehof, M. M., & Schreurs, K. M. (2015). Internet-based guided self-help intervention for chronic pain based on Acceptance and Commitment Therapy: A randomized controlled trial. Journal of Behavioral Medicine, 38(1), 66–80.
Wetherell, J. L., Afari, N., Rutledge, T., Sorrell, J. T., Stoddard, J. A., Petkus, A. J., et al. (2011). A randomized, controlled trial of acceptance and commitment therapy and cognitive-behavioral therapy for chronic pain. Pain, 152(9), 2098–2107.
Mo’tamedi, H., Rezaiemaram, P., & Tavallaie, A. (2012). The effectiveness of a group-based acceptance and commitment additive therapy on rehabilitation of female outpatients with chronic headache: Preliminary findings reducing 3 dimensions of headache impact. Headache: The Journal of Head and Face Pain, 52(7), 1106–1119.
Acknowledgements
The authors would like to thank Hae Lim Noh for her assistance with statistical analysis.
Funding
Eun-Jung Shim was supported by the Brain Korea 21 Plus Program (21B20151813119), National Research Foundation of Korea.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
“All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.” The study was approved by Kyongpook National University Hospital Institutional Review Board.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Shim, EJ., Park, A. & Park, SP. The relationship between alexithymia and headache impact: the role of somatization and pain catastrophizing. Qual Life Res 27, 2283–2294 (2018). https://doi.org/10.1007/s11136-018-1894-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-018-1894-4