Abstract
Background
Sleep quality has been widely studied among western countries. However, there is limited population-based evidence on insomnia in Chinese adult populations, especially in middle-aged and older adults. The aims of present study are to (1) examine the prevalence of poor sleep among Chinese middle-age and older adults, (2) compare the Pittsburgh Sleep Quality Index (PSQI) seven domain scores across different physical health statuses, (3) explore factors associated with insomnia.
Methods
A cross-sectional survey was conducted using a multi-instrument questionnaire. In total, 1563 residents aged 45 or older in the community were interviewed. The Chinese version of the PSQI was used to assess sleep quality while poor sleep was defined as a total PSQI score >5. Socio-demographic, lifestyle and physical health data were also collected.
Results
The prevalence of poor sleep among adults aged over 45 years was 20.67 %. Clusters logistic regression analysis identified that migrant workers, single marital status, lower education level, no physical exercise, illness within 2 weeks, and a higher total number of chronic diseases contribute to increased risk of poor sleep (P < 0.05). Among three clusters, physical health has the biggest independent contribution on sleep quality.
Conclusions
Our results indicated that poor sleep was common in middle-aged and older adults. It was associated with identity of migrant worker, education level, exercise, illness within 2 weeks and number of chronic disease. Being ill within 2 weeks and having more chronic diseases were the major physical health-related factors contributing to poor sleep in the middle-aged and older people. Physical health may be a major determinant in sleep quality.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Sleep problems are common among general population. A number of epidemiological studies have reported prevalence of insomnia symptoms ranging from 10 to 48 % around the world [1, 2]. Nevertheless, population-based data on insomnia in Chinese adult populations are limited, especially for middle-aged and older adults. A cross-sectional study (n = 5001) among Hong Kong general population aged 18 years and above revealed a high prevalence of 39.4 % of insomnia over a one-month period by using the Pittsburgh Sleep Quality Index (PSQI) [3]. Using structured questions, another population-based study (n = 9851) reported an overall prevalence of insomnia among Hong Kong Chinese at 11.9 % [4]. The different prevalence among Hong Kong general population may result from the different survey time and measurement of insomnia. In a study of 2416 older adults (aged ≥ 60) in mid-east China, 49.7 % of the participants reported poor sleep quality [5]. A recent study of 3289 middle-aged and older adults in Beijing and Shanghai, however, reported a low level of sleep quality among these two populations [6].
Sleep quality is reported to be associated with many factors, such as age, gender, physical disease, psychiatric disorder and shift work [7, 8]. Among them, age and gender are the most widely accepted ones. With regard to age, almost all epidemiological studies reported an increased prevalence of insomnia symptoms related to aging, almost 50 % in older adults (65 years and above) [2, 3, 9–13]. Many studies found that the prevalence of insomnia is consistently low in younger age, but increases in older age [2, 3, 10]. In addition, the related factors with sleep quality among younger and older adults were different [6, 14–16]. As to gender, the well-confirmed conclusion was that female was more likely to experience poor sleep than male [1, 4–6, 17].
In addition to the well-acknowledged factor, some studies also reported other risk factors of insomnia, such as lower education level, lower socioeconomic status, smoking, drinking and lack of exercise. It has been noted that sleep problems were more prevalent in individuals with lower education level, lower socioeconomic status and less social support [18, 19]. Also, sleep duration decreased when the number of cigarette smoked per day increased, indicating a consistent, dose–response relationship between smoking and sleep [20]. In addition, the association between sleep problems and alcohol consumption seems to follow a J-shaped curve, which indicated that the individuals who abstain from alcohol tend to be sleepless compared with those who drink moderate amounts of alcohol [20]. In terms of the factor of physical exercise, Yang’s meta-analysis showed that the sleep duration was not prolonged after exercise, but the quality of sleep was significantly improved [21].
The risk factors of insomnia in middle-aged and older adults are not yet well defined. Many researchers found that the prevalence of insomnia mainly increases in middle-aged and older adults with disease and medication [14, 22–24]. So majority of researchers considered age as a considerable risk factor of insomnia. But some studies demonstrated that healthy (without disease and medication) older adults sleep almost as well as younger subjects and aged people with chronic disease is significantly associated with higher risk of insomnia [15, 16, 20]. Thus we guess that insomnia may be associated with increased health problems with aging rather than age per se.
The researches in Chinese middle-aged and older adults were relatively rare. Most of the available studies used ad hoc nonstandardized measures to assess sleep quality, such as “Do you have difficulty in falling asleep?” and “How long do you take to fall asleep?” [4, 6], which are less. Thus, we carried out a large-scale questionnaire survey to investigate the prevalence of poor sleep among middle-aged and older adults (>45 years) by using the PSQI as validated scale. In this paper, we report (1) the prevalence of poor sleep among Chinese middle-aged and older adults, (2) a comparison of the PSQI seven domain scores across physical health statuses and (3) risk factors associated with insomnia.
Methods
Sampling and participants
This study was based on a cross-sectional survey in the Dongguan city of Guangdong province in China. With an estimated poor sleep rate of about 16 % in previous study [6], the minimal sample sizes required in this study were 1545 subjects, allowing a maximal deviation of 1.8 % and type one error of 5 %. The cohort in this survey consisted of family members drawn from 5 % of total households in this city. A total of 1324 households, involving 4086 residents, were randomly selected using the city’s household registration system by simple random sampling. Among them, 1611 subjects were over 45 years old. After excluding those who had self-reported mental disease such as senile dementia, schizophrenia, force disease of sexual neurosis and hysteria and other psychiatric disorders that have a strong link to sleep (e.g., mood disorders), as well as those had not completed the PSQI scale, we finally analyzed 713 households, involving 1563 individuals from all the responders. A flowchart illustrating the selection of study participants is presented in Fig. 1. The final sample size was approached and accepted to allow the implementation of the study protocol. The present cross-sectional data was collected entirely by questionnaire during face-to-face interviews. This study was approved by the Research Ethics Board of Guangzhou Medical University (Project identification code: GZMU-2014024). All participants provided written informed consents.
Procedures
The interviewers (healthcare staff from local Community Health Service Agencies) underwent specific trainings on introduction of this survey, questionnaire contents, communication skills, confidentiality, and they were provided with full sets of written instructions to standardize the data collection and recording procedures. All interviews were conducted at the participants’ homes. All research data were collected through face-to-face interviews using structured study questionnaires. Initially, each group was accompanied by a supervisor to ensure that the interviews were properly conducted. Subsequently, routine supervision was randomly performed in a certain group.
Measurement of sleep quality
We used the PSQI to assess subjective sleep quality. This scale has been the most comprehensively and extensively used sleep questionnaire developed to date [25].The sensitivity, accuracy, comprehensibility, and reproducibility of this Quality Index had been examined and confirmed previously abroad [26, 27]. The Chinese version of the PSQI also had an overall sleep quality evaluation (r = 0.82–0.83) and test–retest reliability (r = 0.77–0.85) [28].
The PSQI evaluates multiple dimensions of sleep retrospectively over a 1-month period which consisted of 19 items [25].These items could be grouped into seven quality components, including subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medication and daytime dysfunction. The seven components score are then summed to yield a global PSQI score (rang 0–21); higher scores indicate worse sleep quality. A global PSQI score >5 has a diagnostic sensitivity of 89.6 % and a specificity of 86.5 % in differentiating from poor to good sleep quality. In this study, a global PSQI score >5 was defined as poor sleep quality, while the score ≤5 was regarded as good sleep quality.
Covariates
Social demographic characters (age, gender, marital status, level of educational and migrant status), lifestyle (cigarette smoking, alcohol intake, regular exercise) and health-related factors (illness within 2 weeks, number of chronic diseases, body mass index and random blood glucose levels) were assessed using a standardized questionnaire.
Marital status was dichotomized into married and single, “married/cohabitation” as “married” while “separated/divorced/widowed/single” as “single”. Level of educational was categorized into senior middle school or higher, junior middle school, and elementary school or lower. Migrant status was divided into local residents and migrant workers. Cigarette smoking was defined as having smoked at least 100 cigarettes in their lifetime. Alcohol drinking was defined as the consumption of at least 30 g of alcohol per week for the past year. Alcohol consumption was obtained on the amount and type of alcohol that was consumed during the previous year. Regular exercise was defined as participating in moderate or intensive activity for no less than 30 min per day for at least 3 days a week. Body mass index (BMI) was categorized as “underweight” (<18.5), “normal weight” (18.5–23.9), “overweight” (24.0–27.9) and “obese” (>28.0), according to the Chinese BMI reference standards [29]. Random blood glucose level was measured by Ames glucometer, with categories of <11.1 mmol/L and ≥11.1 mmol/L. Capillary blood was obtained from a finger prick. Illness within 2 weeks was defined as being sick in the past 2 weeks. Number of chronic diseases was defined as a total number of diseases diagnosed by a doctor including heart disease, hypertension, stroke, thrombosis, diabetes, asthma, bronchitis/emphysema, osteoporosis, arthritis, cancer, stomach/peptic ulcer, migraine, tension headache, depression and other major illness. This variable was categorized into a three-category variable (none, 1 and greater than or equal to 2).
Statistical analysis
In our study, all analyses were conducted using the statistical analysis program SPSS version 13.0. Mean and standard deviation (SD) were presented for continuous variables. Frequency and percentage were presented for categorical variables. One way ANOVA test was used to compare PSQI score between different groups. Univariable logistic regression analysis was used to identify the odds ratios (OR) and 95 % confidence interval (95 % CI) for the association of different factors and poor sleep quality. Clustered logistic regression [30] was employed to explore the impacts of socio-demographic characters, lifestyle and physical health-related factors (three clusters) on sleep quality. The associations between variables were considered statistically significant at the level of P < 0.05.
In clustered regression analyses, independent predictor variables were grouped into three clusters according to nature of the study variables: cluster 1, socio-demographic characters; cluster 2, lifestyle variables; cluster 3, physical health-related factors. Multidirectional associations may exist between the three clusters of independent variables and the dependent variables. As a result, simultaneous consideration of variables from the clusters in a free multiple regression model (i.e., a free forward stepwise logistic regression model) might result in confounded inference [30]. Therefore, we adopted clustered logistic regression which may facilitate more realistic assessment of the relative contribution of factors to sleep quality [30]. The regression model was conducted in three steps: (1) A forward stepwise regression of sleep quality for the cluster 1 variables; (2) A forward stepwise regression for the cluster 2 variables with the equation derived from step 1 as a fixed part of the new regression model; (3) A forward stepwise regression for the cluster 3 variables with the equation derived from step 2 as a fixed part of the new regression model.
The independent effect of each cluster was calculated by the difference in corresponding R 2 value between the two regression models (with vs. without the cluster). The independent contribution share of each cluster was calculated as individual R 2 change/total R 2 change in the final model × 100 %. In logistic regression models, the R2 is the Nagelkerke “pseudo” R2 [31] which is similar to classical R2 in linear regression models for data interpretation.
Results
Participant characteristics
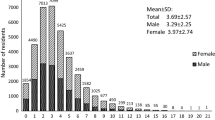
Descriptive statistics on study variables are presented in Table 1. A total of 1563 individuals effectively completed the questionnaire in this survey, of which 729 (46.64 %) were males and 834 (53.36 %) were females. The average age of the residents was 61.06 ± 11.18 years old, ranging from 45 to 93. Among the participants, 1353 (86.56 %) were married, and 210 (13.44 %) were single. A majority of the participants had received junior middle school education (83.43 %). Most of participants were local residents (88.87 %). 26.74 % individuals were smokers, and 12.54 % individuals drank alcohol. There were only 54.24 % of them took regular physical exercise. 6.91, 34.48, 48.05 and 10.56 % of the participants were classified as normal weight, overweight, obese and underweight, respectively. In addition, 6.08 % of participants had a blood glucose value higher than 11.1 mmol/L, 27.19 % had an experience of illness within 2 weeks, and 30.0 % suffered one disease or more.
Overall prevalence
The PSQI total mean score of the 1563 complete questionnaires was 3.84 ± 2.81. The prevalence of poor sleep was estimated to be 20.67 % (PSQI score >5). According the PSQI scores in each domain (Table 2), sleep disturbances ranks the highest, followed by subjective sleep quality. The use of sleeping medication got the lowest score.
Impact of differences in characteristics on sleep quality
Characteristics of participants with the global PSQI score and sleep quality among middle-aged and older adults are displayed in Tables 1 and 2. The mean PSQI score (in Table 1) was progressively greater from individuals aged 55–65 years to individuals aged ≥ 65 years to individuals aged 45–55 (F 2, 1560 = 6.557, P = 0.001). The prevalence of poor sleep presented the same trend in Table 2. Moreover, poor sleep situation was also more likely to be observed in migrant workers, singles, underweight, those who received lower educated levels and those who taken no exercise.
Sleep quality, illness within two weeks and total number of chronic diseases
People with illness within 2 weeks (I2 W) show a higher prevalence of poor sleep than those without (26.15 vs 16.04 %, P < 0.001, Crude OR = 6.57, 95 % CI = 5.04–8.56) as shown in Table 2. Different I2 W groups exhibited statistical differences in terms of sleep quality. Table 3 shows that these differences exist in all the seven domains of the PSQI (P < 0.001) and that the scores of people with I2 W were higher than people without I2 W. These findings were typically suggestive of sleep problems being associated with I2 W.
Total number of chronic diseases (TC) were associated with the prevalence of poor sleep, and the rate is highest in people with ≥2 chronic diseases in Table 1 (P < 0.001). People with one chronic disease were nearly sixfold (95 % CI = 4.58–8.06) more likely to have poor sleep and people with ≥2 chronic diseases were nearly ninefold (95 % CI = 6.01–14.47) more likely to be so. Difference TC groups also showed statistical differences with all the seven domains of sleep quality (P < 0.001). Table 3 shows that scores in all seven domains increased as the TC increased. All of these results shown that there was a strong relationship between TC and sleep quality.
Determinants of sleep quality
The variables included in the final progressive cluster model of logistic regression are shown in Table 4. Values of OR in Table 4 were adjust for all other variables included in the table. Among the socio-demographic variables analyzed, migrant status and education level were significantly associated with sleep quality. Migrant workers were almost eightfold more likely to suffer from poor sleep (OR = 7.92, 95 % CI = 5.11–12.29, P < 0.001); participators received elementary school or lower (OR = 4.26, 95 % CI = 1.96–9.23, P < 0.001) had a higher risk of poor sleep. Among the lifestyle factors that we examined, the risk of poor sleep (OR = 1.79, 95 % CI = 1.34–2.40, P < 0.001) increased significantly with taking no exercise. Among the health-related factors that we studied, the regression analysis further confirmed that individuals with illness within 2 weeks and those with a higher number of chronic diseases were more likely to experience poor sleep. Compare with people without I2 W, those with I2 W had near four times risk to suffer from poor sleep (OR = 3.71, 95 % CI = 2.48–5.54, P < 0.001); participators with ≥ 2 chronic diseases were significantly more likely to experience poor sleep when compare to those without chronic disease (OR = 4.13, 95 % CI = 2.40–7.13, P < 0.001).
Taking all the factors into three clusters: cluster 1, socio-demographic; cluster 2, lifestyle and cluster 3, health-related factors. The independent contributions of the three clusters were 42.18, 4.42 and 53.40 %, respectively. The cluster 3, health-related factors had shown the greatest contribution to the sleep quality while cluster 2, lifestyle variables presented the lowest contribution.
Discussion
Main findings
In this study, we investigated the prevalence and predictors of poor sleep among individuals aged 45 years or older in a municipality in China. Approximately one fifth of participants were found with poor sleep quality. Among the seven PSQI domains, the sleep disturbances were the most important problem for sleep quality. Similar to previous studies, we confirmed that several risk factors were associated with sleep quality, but our results also demonstrated that sleep quality was closely related to several factor such as migrant status, illness experience within 2 weeks and suffering from chronic diseases. Health-related factors were proved to be the most influential independent cluster on sleep quality among the three clusters, followed by socio-demographic characters and lifestyle factors. The association between sleep quality and health status suggested that it might be a major determinant for sleep quality in middle-aged and older adults.
Compare with previous studies
In our study, about one in five of middle-aged and older adults from general public had a bad sleeping in the past month. However, the prevalence rate reported in China was 49.7 % [5] among rural older adults and 39 % [3] in general population. All of these studies used the same sleep evaluation standard, time limitation and dividing points. The discrepancy between these studies might be caused by different population choices. It might also be caused by regional variations, economic status and education levels.
Adults aged 55–65 shown to be a protective factor for poor sleep in univariable analyses, but the same association was not found in the final clusters logistic regression models. So we think the result may be induced by other unknown confounding factors.
We also found that marital status was associated with sleep quality in bivariate analysis. Single individuals were more likely to have poor sleep quality. Previous studies also had illustrated that married participants had a lower risk of poor sleep [32, 33]. But the same association was not found after adjusting for confounding variables in the cluster logistic regression. Part of this association might be attributed to better physical and mental health status among participants who were married [34, 35]. Haseli’s survey found that marital status significantly affected sleep quality of subjects in Shanghai, but the same effect did not found within subjects in Beijing [6]. Therefore, the difference might also be caused by districts’ differences and its variations.
Our study showed that education level was strongly correlated with poor sleep after adjusting for other variables. To a great extent, lower education level may indicate lower income and lower quality of life [36], which were apparently related to poor sleep [3, 37]. This is consistent with previous studies reporting that education is an independent factor associated with sleep quality [38, 39].
It is noteworthy that poor sleep was more prevalent among the migrant workers. As a special group in China, migrant workers’, social and economic status is low, and the social support for them is not enough. Work and stress often have a bad effect on the mental and physical health [40, 41]. Therefore, it was no surprise to find that migrant workers were more likely to suffer from poor sleep.
In terms of the association between physical exercise and sleep quality, this study found that those who reported regular exercise appeared to have a better sleep quality. Similar results were found in Gerber and Reid’s studies [32, 42]. Other study found that participations in exercise training had a moderately beneficial effect on sleep quality with decreases of sleep latency and the use of sleep medication [21]. We considered regular moderately exercise as a protective factor for good sleep quality in this study.
Interesting, we found illness within recent 2 weeks had association with sleep quality. There was little evidence that illness within recent 2 weeks can predict the occurrence of sleep deprivation. Present research illustrated that two-week illness could be considered as a detrimental factor for poor sleep. In particular, the condition of illness within 2 weeks indicated that poor health status related to lower health-related quality of life [43], which was typically accompanied by the experience of poor sleep [44].
In addition, we found that individuals with one or more kinds of chronic diseases had higher risk of poor sleep. Studies showed that chronic diseases had obvious relationship with sleep quality [6, 45]. It was obvious that patients with chronic diseases tend to have poor sleep quality due to poor physiological functions [37]. Moreover, sleep problems were associated with an increasing number of physical disabilities, depressive symptoms and poorer self-perceived health [46, 47]. All of them suggested that a number of sleep complaints might be associated with chronic diseases. Depression and anxiety caused by chronic illnesses could be related to poor sleep, but they were not measured in our study. These factors would be included in our further detailed investigations.
Furthermore, the current results suggested that BMI was linked to sleep quality in univariable analysis. The prevalence of poor sleep decreased while the value of BMI increased. But the same association was not found after adjusting for confounding variables. This result just resembled with Jie Li’s study [5]. We think that the BMI may have some potential relationship with sleep quality which needs to be further studied.
Our analysis showed no significant association between gender and sleep quality, although many studies reported that different gender might result in different sleep quality. A well-known viewpoint is that women are more likely to suffer poor sleep than men [5, 6, 17]. It might result from the different samples.
Strength
In this study, we used the PSQI, a most comprehensive and extensive questionnaire, to evaluate the sleep quality. This made sure the reliability of the results to the utmost extent. Present study also added the sleep quality information about individuals aged 45 or older while most of the previous studies explored sleep quality among children, women and older adults aged 60 or older. Moreover, unlike previous studies, related factors were classified into three clusters and cluster logistic regression was administered in present study. This made the exploration of the independent contribution of every cluster possible.
Limitations of our study
First, this was a cross-sectional study including diseases and factors. Associations between variables can be found, but which variable is the chicken and which variable is the egg were difficult to define in cross-sectional study. Second, all the data in present study were based on self-report of participants. On one hand, individuals might underreport their smoking or their drinking situation in some cases. On the other hand, individuals might underreport their weight and over-report their height. Secondly, we did not involve mental health situation for this study. A lot of researches had reported that mental health situations, such as depression and anxiety, were one of the most important factors that influence the sleep quality. Last but not least, it could be argued that considering sleep quality over just 1 month might not be a true evaluation of sleep quality, although past psychometric evaluations of PSQI have confirmed the validity and precision of this index.
Conclusions
Prevalence of poor sleep quality in middle-age and older adults was high. It was associated with identity of migrant worker, education level, exercise, illness within 2 weeks and number of chronic disease. Being ill within 2 weeks and having more chronic diseases were the major physical health-related factors contributing to poor sleep in the middle-aged and older people. Physical health may be a major determinant in sleep quality. There is a need for further research to investigate the sleep quality in migrant workers and the causal pathways of associations observed in this study.
Abbreviations
- BMI:
-
Body mass index
- LR:
-
Local residents
- MW:
-
Migrant workers
- SS:
-
Senior middle school or higher
- JS:
-
Junior middle school
- ES:
-
Elementary school or lower
- I2W:
-
Illness within 2 weeks
- TC:
-
Total number of chronic diseases
- OR:
-
Odds ratio
- CI:
-
Confidence interval
References
Ohayon, M. M. (2002). Epidemiology of insomnia: What we know and what we still need to learn. Sleep Medicine Reviews, 6(2), 97–111.
Ancoli, I. S., & Roth, T. (1999). Characteristics of insomnia in the United States: Results of the 1991 National Sleep Foundation Survey. I. Sleep, 22(Suppl 2), S347–S353.
Wong, W. S., & Fielding, R. (2011). Prevalence of insomnia among Chinese adults in Hong Kong: A population-based study. Journal of Sleep Research, 20(1 Pt 1), 117–126.
Li, R. H. Y., Wing, Y. K., Ho, S. C., et al. (2002). Gender differences in insomnia—a study in the Hong Kong Chinese population. Journal of Psychosomatic Research, 53(1), 601–609.
Li, J., Yao, Y. S., Dong, Q., et al. (2013). Characterization and factors associated with sleep quality among rural elderly in China. Archives of Gerontology and Geriatrics, 56(1), 237–243.
Haseli-Mashhadi, N., Dadd, T., An, P., et al. (2009). Sleep quality in middle-aged and elderly Chinese: distribution, associated factors and associations with cardio-metabolic risk factors. BMC Public Health, 9(1), 1–11.
Roth, T., & Roehrs, T. (2003). Insomnia: Epidemiology, characteristics, and consequences. Clinical Cornerstone, 5(3), 5–15.
Reid, K. J., Martinovich, Z., Finkel, S., et al. (2006). Sleep: A marker of physical and mental health in the elderly. American Journal of Geriatric Psychiatry Official Journal of the American Association for Geriatric Psychiatry, 14(10), 860–866.
Ohayon, M. M., & Smirne, S. (2002). Prevalence and consequences of insomnia disorders in the general population of Italy. Sleep Medicine, 3(2), 115–120.
Ohayon, M. M. (2001). Prevalence, diagnosis and treatment of chronic insomnia in the general population[C]//Proceedings of the satellite symposium new developments in the treatment of insomnia—Do they really have any impact on the primary health care setting.
Bixler, E. O., Kales, A., Soldatos, C. R., et al. (1979). Prevalence of sleep disorders in the Los Angeles metropolitan area. American Journal of Psychiatry, 136(10), 1257–1262.
Klink, M., & Quan, S. F. (1987). Prevalence of reported sleep disturbances in a general adult population and their relationship to obstructive airways diseases. Chest, 91(4), 540–546.
Ancoli-Israel, S. (2009). Sleep and its disorders in aging populations. Sleep Medicine, 10(suppl 1), S7–S11.
Ohayon, Maurice M., Zulley, Jurgen, Guilleminault, Christian, et al. (2001). How age and daytime activities are related to insomnia in the general population: consequences for older people. Journal of the American Geriatrics Society, 49(4), 360–366.
Bixler, E. O., Papaliaga, M. N., Vgontzas, A. N., et al. (2009). Women sleep objectively better than men and the sleep of young women is more resilient to external stressors: Effects of age and menopause. Journal of Sleep Research, 18(2), 221–228.
Roberts, R., & Shema, S. G. (1999). Prospective data on sleep complaints and associated risk factors in an older cohort. Psychosomatic Medicine, 61(2), 188–196.
Chung, K. F., & Tang, M. K. (2006). Subjective sleep disturbance and its correlates in middle-aged Hong Kong Chinese women. Maturitas, 53(4), 396–426.
Assari, S., Lankarani, M. M., Saleh, D. K., & Ahmadi, K. (2013). Gender modifies the effects of education and income on sleep quality of the patients with coronary artery disease. International Cardiovascular Research Journal, 7(4), 141–146.
Sleep problems and social support. (2011). Frailty in a Brazilian elderly multicenter study. Rev Lat Am Enfermagem, 19(4), 920–927. Article in English, Spanish.
Ursin, R. (2008). Lifestyle factors and sleep-a population study[C]//Journal of Sleep Research. Commerce place, 350 Main St, Malden 02148, MA USA: Wiley-Blackwell Publishing, Inc, 17: 144–144
Yang, P. Y. (2012). Exercise training improves sleep quality in middle-aged and older adults with sleep problems: a systematic review. Journal of Physiotherapy, 58(3), 157–163.
Ohayon, M. M., Caulet, M., & Guilleminault, C. (1997). How a general population perceives its sleep and how this relates to the complaint of insomnia. Sleep, 20(9), 715–723.
Ohayon, M. M., Caulet, M., Priest, R. G., et al. (1997). DSM-IV and ICSD-90 insomnia symptoms and sleep dissatisfaction. British Journal of Psychiatry, 171(4), 382–388.
Nutt, D. J., & Wilson, S. (1999). Evaluation of severe insomnia in the general population–implications for the management of insomnia: The UK perspective. Journal of Psychopharmacology, 13(4 Suppl 1), S33–S34.
Buysse, D. J., Iii, C. F. R., Monk, T. H., et al. (1989). The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Research, 28(2), 193–213.
Backhaus, J., Junghanns, K., Broocks, A., et al. (2002). Test-retest reliability and validity of the Pittsburgh Sleep Quality Index in primary insomnia. Journal of Psychosomatic Research, 53(3), 737–740.
Carpenter, J. S., & Andrykowski, M. A. (1998). Psychometric evaluation of the Pittsburgh Sleep Quality Index. Journal of Psychosomatic Research, 45(1), 5–13.
Tsai, P. S., Wang, S. Y., Wang, M. Y., et al. (2005). Psychometric evaluation of the Chinese version of the Pittsburgh Sleep Quality Index (CPSQI) in primary insomnia and control subjects. Quality of Life Research, 14(8), 1943–1952.
Chen, C. (2008). Overview of obesity in Mainland China. Obesity Reviews, 9((Supp s1)), 14–21.
Cohen, Y. C., Rubin, H. R., Freedman, L., et al. (1999). Use of a clustered model to identify factors affecting hospital length of stay. Journal of Clinical Epidemiology, 52(11), 1031–1036.
Nagelkerke, N. J. D. (1991). A note on a general definition of the coefficient of determination. Biometrika, 78(3), 691–692.
Lu, C. H., Wang, P. X., Lei, Y. X., et al. (2014). Influence of health-related quality of life on health service utilization in Chinese rural-to-urban female migrant workers. Health and Quality of Life Outcomes, 12(1), 1–8.
Ohayon, M. (1996). Epidemiological study on insomnia in the general population. Sleep, 19(3 Suppl), S7–S15.
Verbrugge, L. M. (1979). Marital status and health. Journal of Marriage and Family, 41(2), 267–285.
Hughes, M. E., & Lj, W. (2009). Marital biography and health at mid-life. Journal of Health and Social Behavior, 50(3), 344–358.
Winkleby, M. A., Jatulis, D. E., Frank, E., et al. (1992). Socioeconomic status and health: how education, income, and occupation contribute to risk factors for cardiovascular disease. American Journal of Public Health, 82(6), 816–820.
Soltani, M., Haytabakhsh, M. R., Najman, J. M., et al. (2012). Sleepless nights: the effect of socioeconomic status, physical activity, and lifestyle factors on sleep quality in a large cohort of Australian women. Archives of Women’s Mental Health, 15(4), 237–247.
Friedman, E. M., Love, G. D., Rosenkranz, M. A., et al. (2007). Socioeconomic status predicts objective and subjective sleep quality in aging women. Psychosomatic Medicine, 69(7), 682–691.
Grandner, M. A., Patel, N. P., Gehrman, P. R., et al. (2010). Who gets the best sleep? Ethnic and socioeconomic factors related to sleep complaints. Sleep Medicine, 11(5), 470–478.
Hesketh, T., Ye, X. J., Li, L., et al. (2008). Health status and access to health care of migrant workers in China. Public Health Reports, 123(2), 189–197.
Cui, X., Rockett, I. R., Yang, T., et al. (2012). Work stress, life stress, and smoking among rural–urban migrant workers in China. BMC Public Health, 12(10), 958–958.
Reid, K. J., Baron, K. G., Lu, B., et al. (2010). Aerobic exercise improves self-reported sleep and quality of life in older adults with insomnia. Sleep Medicine, 11(9), 934–940.
Cui, J. Y., Tang, J. X., Qin, J. M., et al. (2015). Analysis on influencing factors of quality of life among the elderly in Hami area by multi-level model. Chinese Journal of Disease Control and Prevention, 19(3), 240–243 (in Chinese).
Zhou, J., Xie, L. Q., & Chen, X. G. (2015). Study on the sleep quality and its influencing factors of rural left-behind elderly in Hunan province. Chinese Nursing Management, 15(4), 437–440 (in Chinese).
Foley, D. (2004). Sleep disturbances and chronic disease in older adults: results of the 2003 National Sleep Foundation Sleep in America Survey. Journal of Psychosomatic Research, 56(5), 497–502.
Ohayon, M. M., & Roth, T. (2003). Place of chronic insomnia in the course of depressive and anxiety disorders. Journal of Psychiatric Research, 37(1), 9–15.
Foley, D. J., Monjan, A. A., Brown, S. L., et al. (1995). Sleep complaints among elderly persons: an epidemiologic study of three communities. Sleep, 18, 425–432.
Acknowledgments
This study was supported by the Guangzhou 121 talents program (GZRSH-2014-2048, Guangzhou Municipal Human Resources and Social Security Bureau, People’s Republic of China). We gratefully acknowledged staff of local Community Health Service Agencies for their kind assistance in data collection. JJW is supported by Guangdong Exemplary Centre for Exploratory Teaching in Higher Education Institutions—General Practice Exploratory Teaching Centre [GDJG-2010-N38-35, Guangdong Department of Education, People’s Republic of China], and The Ninth Round of Guangdong Key Disciplines—General Practice [GDJY-2012-N13-85, Guangdong Department of Education, People’s Republic of China], both of which he leads.
Funding
This study was funded by the Guangzhou 121 talents program (Grant Number GZRSH-2014-2048).
Author contributions
All authors contributed to the development of the study framework, interpretation of the results, revisions of successive drafts of the manuscript and approved the version submitted for publication. HSZ, YL and JLL conducted the data analyses. HSZ, YL and WQL drafted the manuscript. HYM, PXW and JJW finalized the manuscript with inputs from all authors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Hui-Shan Zhang and Yuan Li have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Zhang, HS., Li, Y., Mo, Hy. et al. A community-based cross-sectional study of sleep quality in middle-aged and older adults. Qual Life Res 26, 923–933 (2017). https://doi.org/10.1007/s11136-016-1408-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-016-1408-1