Abstract
Purpose
This study aimed to identify the predictors of decline in health-related quality of life (HRQOL) in Chinese patients with type 2 diabetes mellitus (T2DM).
Methods
A prospective longitudinal observational study was conducted on 1826 Chinese T2DM patients managed in public primary care setting. HRQOL was measured at baseline, 1 and 2 years by the Short Form-12 Health Survey version 2 (SF-12v2) and Chinese (HK) Short Form-6 Dimensions (SF-6D). Linear mixed effect models with forward stepwise method were performed to select the factors associated with SF-12v2 physical (PCS) and mental component summary (MCS) scores and SF-6D value.
Results
Over a 2-year observation period, the HRQOL (PCS: −0.626; MCS: −1.869; and SF-6D: −0.017 per year) scores decreased significantly with time. Female, unmarried, current smoker, no regular exercise, obesity, comorbid hypertension, chronic kidney disease (CKD) or cardiovascular disease (CVD) and insulin use were predictors of one or more poorer HRQOL scores after 12 or 24 months. Older age had a negative impact on PCS score and SF-6D value, but had a positive impact on MCS score.
Conclusions
The HRQOL of Chinese T2DM patients under primary care declined significantly over time. Obesity, smoking and no regular exercise were found to be modifiable risk factors of the decline in HRQOL in T2DM, which strengthened the importance of these lifestyle changes in diabetes care. More attention should be given to T2DM patients who are female, older, unmarried, or on anti-hypertensive drugs or insulin, or have comorbid hypertension, CKD or CVD in minimizing the negative impact of illness on their life.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diabetes mellitus (DM) is a global public health problem. According to the International Diabetes Federation, 382 million people were affected by DM in 2014 [1]. Due to the increase in both the ageing population and the number of obesity cases, the expected number of diabetic patients is estimated to reach 592 million by 2035 [1]. Furthermore, China had the highest number of people with diabetes (98 million) in the world in 2013, with a prevalence of 9.6 %. It was estimated that the number of people with diabetes will reach 143 million by year 2035 [2]. Compared with type 1 DM, type 2 DM is much more prevalent, accounting for 90 % of all diabetes cases globally [3]. Numerous studies suggested that type 2 DM affects physical functioning and mental health [4] and is detrimental to the health-related quality of life (HRQOL). There are several possible explanations. First, according to Wilson and Cleary’s HRQOL model, HRQOL is multifaceted construct, which will be affected by symptoms, functional status, as well as environment [5]. Second, type 2 DM is associated with many complications such as retinopathy, neuropathy, nephropathy and amyotrophy which negatively affect activities of daily living. For example, hyperglycaemia can impair contractile function and force degeneration in muscle [6]. Neuropathy impairs mobility. Third, treatment burden (such as diet restriction and medication adherence) may jeopardize the HRQOL of patients. In addition to traditional objective clinical parameters such as haemoglobin A1c (HbA1c), it is important to assess HRQOL in DM patients in order to investigate the physical and emotional well-being of patients. Furthermore, understanding the predictors associated with poorer HRQOL among type 2 diabetic patients can assist clinicians in identifying patients who are at risk of HRQOL deterioration and health service planners in providing appropriate personalized medical and psychosocial interventions. Therefore, the aim of the present study was to identify primary care patients with type 2 DM who tended to have poorer HRQOL. The goal was to explore the predictors of poorer HRQOL in Chinese patient with type 2 DM and provide a 2-year estimate of HRQOL utility index.
Several cross-sectional studies identified factors associated with HRQOL among Chinese patients with type 2 DM [4, 7–11]. A study on Chinese patients with type 2 diabetes found that being female, older age, having a higher BMI and having DM complications were associated with poorer physical aspects of HRQOL as measured by the SF-12 Health Survey version 2 (SF-12 v2), while being female, younger age, having a lower education level, having a lower BMI and having insulin injections were associated with poorer mental aspects of HRQOL as measured by the SF-12 v2 [9]. Another study on Chinese patients with type 2 diabetes found that being female, older age, obesity(BMI ≥ 25), having hypoglycaemia at least once monthly, having neuropathy and having cardiovascular disease were associated with poorer HRQOL as measured by EQ-5D, while using insulin and having hypertension were associated with better HRQOL [10]. However, these cross-sectional studies could not show a temporal relationship between independent variables and HRQOL.
Very few studies have evaluated the longitudinal association between the predictors and HRQOL in patients with type 2 DM. Previous studies in Hong Kong found that younger age, having diabetes complications, being admitted to the hospital due to hypoglycaemia and receiving insulin therapy were predictors of poorer disease-specific HRQOL [8]. However, the subjects were only recruited in one hospital and the study sample was consisted of type 1 and type 2 DM patients. The generalizability of the study findings to type 2 DM patients was questionable. Besides, some study findings were conflicting and inconclusive. A study reported that higher HbA1c was associated with lower HRQOL [12], but other studies showed no association between HbA1c and HRQOL over time [13–15]. Inconsistent relationships between BMI and HRQOL over time were found in previous studies [15–17]. Hence, further study is needed to provide more evidence on the predictors for HRQOL among type 2 diabetic patients.
To date, most studies have been conducted in non-Chinese populations. The predictors of HRQOL in Chinese type 2 diabetic patients are poorly understood, even though 25 % of the global diabetic population are ethnically Chinese [1]. Results from non-Asian population may not be transferable to a Chinese population because the interpretations of diseases and HRQOL are culturally specific [18]. The health beliefs of Chinese people are philosophically distinct from that of Western medicine because they are mostly influenced by traditional Chinese medicine which has its roots in Confucianism and Taoism. According to traditional Chinese medicine, diabetes is attributed to three main factors including improper diet, emotional disturbances and deficiency of Yin [19]. Moreover, previous studies in other patient populations found the distinct difference in HRQOL pattern between Chinese and Western populations [20, 21]. Moreover, evidence regarding determinants influencing HRQOL in type 2 diabetic patients managed in primary care is scarce. The lack of knowledge about the predictors of HRQOL in Chinese type 2 diabetic patients under primary care necessitates this present study. The aim of this study was to identify the predictors for poorer HRQOL in Chinese patients with type 2 DM over time and provide a 2-year estimate of preference-based measure for cost-effectiveness analysis of primary care interventions for patients with diabetes.
Methods
Subjects and sampling
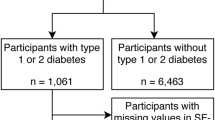
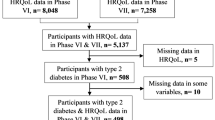
This was a secondary analysis of a prospective longitudinal observational data from the evaluation of two local primary care programmes for diabetes: Multidisciplinary Risk Assessment and Management Program for Patients with Diabetes Mellitus (RAMP-DM) and Patient Empowerment Programme (PEP) [22, 23]. A convenience sampling of subjects, who received care under government-funded primary care outpatient clinics across Hong Kong, were recruited between October 2010 and November 2012 when they attended doctor consultation or the first class session of PEP. All patients who were clinically diagnosed with type 2 DM by the primary care physician and had a code of “T90” from the International Classification of Primary Care (ICPC-2) in their patient records were recruited. Subjects were excluded if they met any of the following criteria: under the age of 18; could not understand Cantonese; or had cognitive impairment. Trained research assistants explained the nature of the study and invited subjects to participate. Patients who agreed to participate completed the structured interviewer-administered questionnaire within 1 month from the date of recruitment and at 12 and 24 months for follow-up, and these questionnaires were completed over telephone. The clinical data, including anthropometric and laboratory data, were extracted from Hong Kong Hospital Authority’s clinical management system database which provided a comprehensive profile of each patient’s health. Patients who cannot be linked up with the administrative database were excluded in the analysis. Figure 1 shows the recruitment process of diabetic patients. A total of 1826 patients completed the baseline questionnaire. Of these, 1378 (75.5 %) and 1090 (59.7 %) patients completed followed up surveys at 12 and 24 months, respectively.
Study instruments
The Chinese (Hong Kong) SF-12 Health Survey version 2 (SF-12v2)
The Chinese (Hong Kong) SF-12v2 Health Survey has been validated and normed on the general Chinese population in Hong Kong [24, 25]. It has been used to measure generic health-related quality of life (HRQOL) in diabetic patients among the local population [9]. It measures eight domains of HRQOL, namely physical functioning, role physical, bodily pain, general health, vitality, social functioning, role emotional and mental health on a scale with theoretical range from 0 to 100. A higher score indicates better HRQOL. The eight domain scores are aggregated based on population-specific weights into two summary scores: the physical (PCS) and mental component summary (MCS) scores.
The Chinese (HK) short Form-6 dimensions (SF-6D)
The SF-6D is a generic preference-based measure which generates a composite index value [26] for economic appraisal of health interventions. The theoretical range of SF-6D preference-based score ranged from 0.315 for the worst possible health state to 1 for full health according to Chinese Hong Kong population-specific scoring algorithm [27, 28]. Seven out of twelve questions from SF-12v2 (questions 2, 5, 6, 8, 10, 11 and 12) have been selected to derive the SF-6D preference-based index based on a preference-weighted scoring algorithm [27].
Socio-demographics and clinical characteristics at baseline
The socio-demographic data included gender, age, marital status and regular exercise (at least 120 min per week) were collected through the baseline questionnaire, whereas smoking status, alcohol status and educational level were collected through the clinical management system database of the Hong Kong Hospital Authority. The clinical characteristics included family history of DM, duration of DM, hyperglycaemia (HbA1c ≥ 7 %), hyperlipidemia (low-density lipoprotein cholesterol ≥ 2.6 mmol/L, total cholesterol ≥4.5 mmol/L, triglycerides ≥1.7 mmol/L or high-density lipoprotein cholesterol ≥1.0 mmol/L for male or ≥1.3 mmol for female), obesity (BMI ≥ 27.5 kg/m2), presence of chronic kidney disease (CKD) (estimated glomerular filtration rate <60 mL/min/1.73 m2), hypertension (systolic/diastolic blood pressure ≥130/80 mmHg or ICPC-2 of K86 or K87), history of CVD event (ICPC-2 of K74 to K76 for coronary heart diseases and International Classification of Diseases, Ninth Edition, Clinical Modification (ICD-9-CM) of 410.x, 411.x to 414.x, 798.x; ICPC-2 of K77 or ICD-9-CM of 428.x for heart failure; ICPC-2 of K89 to K91 or ICD-9-CM of 430.x to 438.x for stroke), the need to use anti-hypertensive drugs, insulin, oral anti-diabetic drugs and lipid-lowering agents.
Data analysis
The primary outcome of the present study was HRQOL as measured by the SF-12v2 scores. Descriptive statistics were used to calculate the baseline socio-demographic, clinical characteristics, disease characteristics, comorbidity, treatment modalities. The reliabilities for the measures were assessed by the Cronbach’s alpha. The differences in the SF-12v2 and SF-6D scores between baseline, 12- and 24-month survey were mutually analysed by repeated-measure ANOVA and post hoc analysis with Bonferroni adjustments. In addition, linear mixed effect models including patients as a random effect with forward stepwise method were performed to identify the predictors associated with the SF-12v2 and SF-6D scores. F-test was used to retain variables with p values smaller than 0.05 and remove variables with p values greater than 0.10. The intra-class correlation coefficient (ICC) for each model was used to examine the variations in the outcomes between patients. Complete case analysis was adopted throughout the regression analysis.
All statistical analyses were performed using STATA version 13.0 (StataCorp LP, College Station, Tex). All significance tests were two-tailed, and findings with a p value less than 0.05 were considered statistically significant.
Results
Table 1 summarizes the baseline characteristics of the study subjects. At least 95 % data completion rates for most of patient’s characteristics and outcome measurements are shown in supplementary Table 1; 55.6 % of the subjects were female; mean age is 64.8 years; 73.3 % were married; 9.1 % were smokers; and 3.6 % were drinkers. In terms of clinical characteristics, 47.8 % were suffered from hyperglycaemia, and 79.7 % were suffered from hyperlipidemia. Moreover, the duration of DM was 7.9 years, and 7.2 % and 11.5 % of patients had history of CVD and CKD, respectively.
The Cronbach’s alpha coefficients for SF-12v2 PCS, MCS and SF-6D were 0.89, 0.88 and 0.90, respectively, which suggested the acceptable reliabilities for the measures. Table 2 shows the comparisons of SF-12v2 and SF-6D scores between baseline, 12 and 24 months. There were significant differences in the SF-12v2 PCS and MCS scores and the SF-6D score between the three time points. Moreover, post hoc analysis revealed that the all three scores at baseline or 12 months were significantly greater than that at 24 months.
Linear mixed effect models with a random effect of patient were performed to explore predictors associated with SF-12v2 PCS and MCS scores and SF-6D score. The results are shown in Table 3. The ICC demonstrated that 45.6, 37.7 and 51.6 % of the variances were incorporated in SF-12v2 PCS, MCS and SF-6D scores among patients, indicating significantly high variations in these three outcomes between patients. All PCS, MCS and SF-6D scores decreased significantly with time. This result was in line with the unadjusted analysis as shown in Table 2. Male and regular exercise were two predictors associated with better HRQOL. Marriage and younger in age were two predictors associated with higher SF-12v2 PCS and SF-6D scores. Conversely, older age was a predictor associated with better HRQOL as measured by the SF-12v2 MCS score. Smoking was a predictor associated with poorer SF-12v2 MCS and SF-6D score. Obesity, history of CVD event, presence of CKD and use of anti-hypertensive drug or insulin were predictors associated with poorer SF-12v2 PCS or SF-6D scores.
Discussion
This study was a prospective longitudinal study for Chinese patients with type 2 diabetes mellitus under primary care to identify the predictors of HRQOL. Our study revealed that HRQOL decreased over time in Chinese diabetic patients. Female, older age, unmarried, comorbidity of hypertension, CKD and CVD, and the need to use insulin were predictors of poorer HRQOL. Moreover, our findings also indicated that no regular exercise, obesity and smoking were associated with poorer HRQOL and thus confirmed the importance of regular exercise, weight control and smoking cessation in the diabetes care. However, evidence to support behaviorial interventions to improve HRQOL in Chinese populations was scarce. Further research should be conducted to build the evidence base on their effectiveness on improving HRQOL in Chinese populations.
During the 2-year follow-up in our study, the HRQOL of the diabetic patients declined significantly over time. There were some possible explanations for these findings. Ageing and disease progression adversely influences both physical and mental health of diabetic patients over time. Complications of type 2 DM such as retinopathy, neuropathy and side effects of treatments might negatively affect the HRQOL of patients with type 2 DM. Besides, the long-term detrimental impact on HRQOL among diabetic population may be explained by the burden of treatments. Lifelong regular drug treatment and restriction in the lifestyle are required in the management of diabetes. For example, the freedom to enjoy food plays an important role in quality of life in Chinese culture which makes dietary management a critical section for diabetes care [29, 30]. Therefore, patients who have more dietary restrictions due to the severity of their disease may have negative impact on HRQOL over time. It should be noted that our result was inconsistent with a recent literature in UK which showed no change in HRQOL over 1-year follow-up for diabetic patients [31]. However, it is hard to compare our study findings with others due to the difference in healthcare setting, length of follow-up period and outcome measures.
The associations between HRQOL and socio-demographic factors were similar with those in general population, which was probably not related to type 2 diabetes. SF-12 v2, which is a generic HRQOL measure, might not be sensitive enough to capture the impacts of type 2 DM on HRQOL. For further study, disease-specific HRQOL measures should be used to further explore the association between HRQOL and socio-demographic factors.
We found no association between obesity and mental aspects of HRQOL. In fact, current evidence about the impacts of obesity on mental aspects of HRQOL in patients was inconclusive. A review by Kushner et al. [32] suggested that subjects who were severe obesity had poorer mental aspect in the HRQOL. Conversely, “jolly fat hypothesis” proposed that obese people had better mental aspect in the HRQOL [33]. In regard to physical aspects of HRQOL, we found that subjects who were obese had lower scores in the physical component of HRQOL. The association that was well established in previous studies [34] was not unique to our population.
It was unexpected to identify the lack of association between HRQOL with hyperglycaemia and duration of DM among diabetic patients, in contrast to the conventional perception that HbA1c reflects the control of DM; therefore, it would be a vital indicator of HRQOL as stated in previous literatures [13, 35, 36]. In fact, several local cross-sectional studies also showed that HbA1c and duration of DM did not have any association with HRQOL measured by genetic or diabetic-specific instruments [8–10], suggesting that these findings may be culturally specific in Chinese diabetic population [8, 9].
Regarding the comorbidity, subjects who were diagnosed with hypertension had lower scores in physical aspect of HRQOL when compared with subjects who did not have hypertension. A study found that subjects with known hypertension had poorer physical functioning, as measured by the SF-36, compared with those without known hypertension (6.0 out of 100 points) [37]. Furthermore, the study found that subjects with known hypertension had poorer HRQOL than those without even though the mean values of systolic and diastolic blood pressures for both groups were similar. The authors explained that therapeutic and labelling effects jeopardized the HRQOL of subjects with known hypertension [37].
Diabetic patients with history of CVD event had lower scores in the physical aspect of HRQOL and SF-6D scores, but there were no significant differences in the mental aspect of HRQOL. Previous studies in the USA, UK and Singapore also identified that the CVD events were only associated with lower physical aspect of the HRQOL [11, 38, 39]. Similarly, patients with the presence of CKD had lower SF-12v2 PCS score compared to those without CKD. A study on African Americans with diabetes found that subjects with impaired renal function were, out of 100 points, 12.5 points lower in the physical functioning domain as measured by the SF-36 and, out of 100 points, 8.6 points lower in the general health domain compared with those without impaired renal function [40]. Moreover, a study found a significant association between CKD and physical component of HRQOL [41]. Several studies found that CKD adversely affects physical functioning [42–44].
Considering treatment regimen, subjects who regularly needed anti-hypertensive drugs or insulin injections had poorer SF-12v2 PCS and SF-6D scores. The results were possibly influenced by the indication bias that the majority of diabetic patients receiving anti-hypertensive or insulin therapies may have poorer control of the concerned clinical parameters compared with patients not on these drugs. For example, insulin is seldom used for simple uncomplicated diabetic patients with good diabetic control. Only patients with unsatisfactory or refractory diabetic control, such as patients with hyperglycaemia despite being on maximum dosage of oral anti-diabetic drugs, will be started on insulin. In fact, the findings were consistent with those of previous studies [4]. The Fremantle Diabetes Study found that insulin-treated patients with type 2 DM had poorer HRQOL than non-insulin-treated patients with type 2 DM over 4 years [45]. Among subjects with type 2 DM, patients on insulin reported lower HRQOL scores than those on oral hypoglycaemic agents or those only having dietary restrictions [46]. Therefore, it is plausible in current findings that the need to use anti-hypertensive drugs or insulin was a proxy of severity of the diabetes as a predictor of poorer physical aspect of HRQOL.
It should be noted that some risk factors associated with HRQOL were unavailable in this study, such as service utilization, psychological factors and the presence of diabetes-related complications [4], although most of disease characteristics such as duration of T2DM, the presence of chronic kidney disease and hypertension, and key clinical characteristic like obesity, presence of hyperglycaemia and hyperlipidemia and the drug medications, to a certain extent reflect the intensity of disease severity and lifestyle modification, have been considered. Further study is needed to explore the impacts of these factors on HRQOL in patients with type 2 DM.
Strengths and limitations of this study
Some of the strengths in the present study are as follows: firstly, we had a large sample size which strengthens the external validity of the findings from our study. Secondly, it was a prospective longitudinal study, which can provide stronger evidence of the temporal relationship between factors and the change in HRQOL. Thirdly, the potential predictors in this study included socio-demographic, lifestyles, clinical parameters, comorbidities, disease characteristics and treatment modalities which were sufficient to reflect the intensity of disease severity and lifestyle modification of the patients and identify significant predictors on HRQOL.
There were several limitations in this study. Firstly, the study was conducted in primary care setting. The findings may not be generalizable to Chinese diabetic patients receiving secondary or tertiary care. The relationship may be subject to temporal changes or modifications in unmeasured risk factors or interventions. Secondly, we used generic HRQOL measures only. Further study should use diabetes-specific HRQOL measures to confirm the findings from this study. Lastly, the long-term effects of predictors on HRQOL are uncertain among Chinese diabetic patients. Further longitudinal studies are warranted to reappraise the association between predictors and HRQOL to confirm the reasons contributing to HRQOL, particularly for suboptimal SBP at baseline. A longer follow-up period over 5 years should be conducted.
Conclusions
HRQOL decreased over a period of 2 years among the Chinese diabetic patients under primary care. The impacts of socio-demographic factors on HRQOL were consistent with those observed in the general population. For clinical practice, patients who are female, older, smoker, unmarried and obese, with hypertension, CKD and CVD, and on insulin were predictors of poorer HRQOL. More attention needs to be paid to diabetic patients with these risk factors. Second, our findings stressed the importance of regular exercise, weight control and smoking cessation in diabetes care as these factors were predictors of poorer HRQOL.
Abbreviations
- BMI:
-
Body mass index
- CHD:
-
Coronary heart diseases
- CKD:
-
Chronic kidney disease
- DM:
-
Diabetes mellitus
- HbA1c:
-
Haemoglobin A1c
- HRQOL:
-
Health-related quality of life
- ICPC-2:
-
International Classification of Primary Care version 2
- ICD-9-CM:
-
International Classification of Diseases, Ninth Edition, Clinical Modification
- MCS:
-
Mental component summary
- PCS:
-
Physical component summary
- PEP:
-
Patient empowerment programme
- RAMP-DM:
-
Multidisciplinary Risk Assessment and Management Program for Patients with Diabetes Mellitus
- SF-12v2:
-
Short Form-12 Health Survey version 2
- SF-6D:
-
Short Form-6 Dimensions
- T2DM:
-
Type 2 diabetes mellitus
References
International Diabetes Federation, IDF Diabetes Atlas, 7 ed. 2015: Brussels.
Aguiree, F., et al. (2013). IDF diabetes atlas.
Zimmet, P., Alberti, K., & Shaw, J. (2001). Global and societal implications of the diabetes epidemic. Nature, 414(6865), 782–787.
Rubin, R. R., & Peyrot, M. (1999). Quality of life and diabetes. Diabetes/Metabolism Research and Reviews, 15(3), 205–218.
Wilson, I. B., & Cleary, P. D. (1995). Linking clinical variables with health-related quality of life. JAMA, 273(1), 59–65.
Helander, I., Westerblad, H., & Katz, A. (2002). Effects of glucose on contractile function,[Ca2+] i, and glycogen in isolated mouse skeletal muscle. American Journal of Physiology-Cell Physiology, 282(6), C1306–C1312.
Wändell, P. E. (2005). Quality of life of patients with diabetes mellitus an overview of research in primary health care in the Nordic countries. Scandinavian Journal of Primary Health Care, 23(2), 68–74.
Shiu, A. T., Thompson, D. R., & Wong, R. Y. (2008). Quality of life and its predictors among Hong Kong Chinese patients with diabetes. Journal of Clinical Nursing, 17(5a), 125–132.
Wong, C., et al. (2013). The associations of body mass index with physical and mental aspects of health-related quality of life in Chinese patients with type 2 diabetes mellitus: Results from a cross-sectional survey. Health Qual Life Outcomes, 11(1), 142.
Luk, A. O., et al. (2014). Health-related quality of life in Chinese patients with type 2 diabetes: An analysis of the Joint Asia Diabetes Evaluation (JADE) Program. Journal of Diabetes and Metabolism, 5(333), 2.
Venkataraman, K., et al. (2013). Associations between complications and health-related quality of life in individuals with diabetes. Clinical Endocrinology, 78(6), 865–873.
Van der Does, F. E., et al. (1996). Symptoms and well-being in relation to glycemic control in type II diabetes. Diabetes Care, 19(3), 204–210.
Weinberger, M., et al. (1994). The relationship between glycemic control and health-related quality of life in patients with non-insulin-dependent diabetes mellitus. Medical Care, pp. 1173–1181.
Hajos, T., et al. (2012). The longitudinal association between glycaemic control and health-related quality of life following insulin therapy optimisation in type 2 diabetes patients. A prospective observational study in secondary care. Quality of Life Research, 21(8), 1359–1365.
Maatouk, I., et al. (2012). Temporal predictors of health-related quality of life in elderly people with diabetes: results of a German cohort study. PLoS ONE, 7(1), e31088.
Grandy, S., & Fox, K. M. (2012). Change in health status (EQ-5D) over 5 years among individuals with and without type 2 diabetes mellitus in the SHIELD longitudinal study. Health and quality of life outcomes, 10(1), 99.
Müller-Nordhorn, J., et al. (2014). Longitudinal association between body mass index and health-related quality of life. PLoS ONE, 9(3), e93071.
Alonso, J., et al. (2004). Health-related quality of life associated with chronic conditions in eight countries: Results from the International Quality of Life Assessment (IQOLA) Project. Quality of Life Research, 13(2), 283–298.
Covington, M. B. (2001). Traditional Chinese medicine in the treatment of diabetes. Diabetes Spectrum, 14(3), 154.
Wan, E. Y., et al. (2015). Patterns of health-related quality of life and associated factors in Chinese patients undergoing haemodialysis. Health and Quality of Life Outcomes, 13(1), 1.
Choi, E. P., Lam, C. L., & Chin, W.-Y. (2014). The health-related quality of life of Chinese patients with lower urinary tract symptoms in primary care. Quality of Life Research, 23(10), 2723–2733.
Fung, C. S., et al. (2012). Evaluation of the quality of care of a multi-disciplinary risk factor assessment and management programme (RAMP) for diabetic patients. BMC Family Practice, 13(1), 116.
Wong, C. K., et al. (2014). Patient Empowerment Programme in primary care reduced all‐cause mortality and cardiovascular diseases in patients with type 2 diabetes mellitus: A population‐based propensity‐matched cohort study. Diabetes, Obesity and Metabolism.
Lam, C. L. K., et al. (2010). Population norm of Chinese (HK) SF-12 Health Survey_Version 2 of Chinese adults in Hong Kong. HK Pract, 32, 77–86.
Lam, C. L. K., Tse, E. Y., & Gandek, B. (2005). Is the standard SF-12 health survey valid and equivalent for a Chinese population? Quality of Life Research, 14(2), 539–547.
Brazier, J. E., & Roberts, J. (2004). The estimation of a preference-based measure of health from the SF-12. Medical Care, 42(9), 851–859.
McGhee, S. M., et al. (2011). Quality-adjusted life years: Population-specific measurement of the quality component. Hong Kong Medical Journal, 17(Suppl 6), 17–21.
Lam, C. L., Brazier, J., & McGhee, S. M. (2008). Valuation of the SF-6D health states is feasible, acceptable, reliable, and valid in a Chinese population. Value in Health, 11(2), 295–303.
Yao, G., et al. (2002). Development and verification of validity and reliability of the WHOQOL-BREF Taiwan version. Journal of the Formosan Medical Association, 101(5), 342–351.
Nam, S., et al. (2011). Barriers to diabetes management: Patient and provider factors. Diabetes Research and Clinical Practice, 93(1), 1–9.
Hazell, M. L., et al. (2009). Temporal change in health-related quality of life: A longitudinal study in general practice 1999–2004. British Journal of General Practice, 59(568), 839–843.
Kushner, R. F., & Foster, G. D. (2000). Obesity and quality of life. Nutrition, 16(10), 947–952.
Crisp, A. H., & McGuiness, B. (1976). Jolly fat: Relation between obesity and psychoneurosis in general population. BMJ, 1(6000), 7–9.
Fontaine, K., & Barofsky, I. (2001). Obesity and health-related quality of life. Obesity Reviews, 2(3), 173–182.
Shim, Y., et al. (2012). Health-related quality of life and glycaemic control in patients with type 2 diabetes mellitus in Singapore. Diabetic Medicine, 29(8), e241–e248.
Mehta, Z., et al. (1999). Quality of life in type 2 diabetic patients is affected by complications but not by intensive policies to improve blood glucose or blood pressure control (UKPDS 37). Diabetes Care, 22(7), 1125.
Mena-Martin, F. J., et al. (2003). Health-related quality of life of subjects with known and unknown hypertension: Results from the population-based Hortega study. Journal of Hypertension, 21(7), 1283–1289.
Laiteerapong, N., et al. (2011). Correlates of quality of life in older adults with diabetes the diabetes & aging study. Diabetes Care, 34(8), 1749–1753.
Lloyd, A., Sawyer, W., & Hopkinson, P. (2001). Impact of long-term complications on quality of life in patients with type 2 diabetes not using insulin. Value in Health, 4(5), 392–400.
Hill-Briggs, F., et al. (2002). Health-related quality of life in Urban African Americans with type 2 diabetes. Journal of General Internal Medicine, 17(6), 412–419.
Gorodetskaya, I., et al. (2005). Health-related quality of life and estimates of utility in chronic kidney disease. Kidney International, 68(6), 2801–2808.
Chow, F. Y., et al. (2003). Health-related quality of life in Australian adults with renal insufficiency: A population-based study. American Journal of Kidney Diseases, 41(3), 596–604.
Shidler, N. R., Peterson, R. A., & Kimmel, P. L. (1998). Quality of life and psychosocial relationships in patients with chronic renal insufficiency. American Journal of Kidney Diseases, 32(4), 557–566.
Kurella, M., et al. (2004). Physical and sexual function in women with chronic kidney disease. American Journal of Kidney Diseases, 43(5), 868–876.
Davis, T. M., Clifford, R. M., & Davis, W. A. (2001). Effect of insulin therapy on quality of life in type 2 diabetes mellitus: The fremantle diabetes study. Diabetes Research and Clinical Practice, 52(1), 63–71.
Jacobson, A. M., De Groot, M., & Samson, J. A. (1994). The evaluation of two measures of quality of life in patients with type I and type II diabetes. Diabetes Care, 17(4), 267–274.
Acknowledgments
We would like to thank the programme team at the Hospital Authority head office including Dr Christina Maw and Ms Ruby Kwok and all representatives and clinical staff who helped with the recruitment in the clinics. Moreover, we would like to thank Dr. S.V. Lo and the staff of the Statistics and Workforce Planning Department in the Hospital Authority Strategy and Planning Division.
Funding
This study has been funded by the Hong Kong Hospital Authority (Ref. No: 8011014157) and Health Services Research Fund, Food and Health Bureau, HKSAR Commissioned Research on Enhanced Primary Care Study (Ref. No EPC-HKU-2). The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki ethics committee and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wan, E.Y.F., Fung, C.S.C., Choi, E.P.H. et al. Main predictors in health-related quality of life in Chinese patients with type 2 diabetes mellitus. Qual Life Res 25, 2957–2965 (2016). https://doi.org/10.1007/s11136-016-1324-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-016-1324-4