Abstract
Purpose
This study sought to compare the association between health-related quality of life (HRQoL) and four body health types by gender.
Methods
The study included 6217 men and 8243 women over 30 years of age chosen from a population-based survey. Participants were grouped by body mass index and metabolic abnormality into four types: metabolically healthy normal weight, metabolically abnormal but normal weight (MANW), metabolically healthy obesity (MHO), and metabolically abnormal obesity (MAO). HRQoL was measured using the EQ-5D health questionnaire. The outcomes encompassed five dimensions (mobility, self-care, usual activity, pain/discomfort, and anxiety/depression), and the impaired HRQoL dichotomized by the EQ-5D preference score. Complex sample multivariate binary logistic regression analyses were conducted to adjust for sociodemographic variables, lifestyle factors, and disease comorbidity.
Results
Among men, those in the MANW group presented worse conditions on all dimensions and the impaired HRQoL compared to other men. However, no significant effect remained after adjusting for relevant covariates. For women, those in the MAO group had the most adversely affected HRQoL followed by those females in the MHO group. The domain of mobility and impaired HRQoL variable of the MAO and MHO groups remained significant when controlling for all covariates in the model.
Conclusions
The MANW is the least favorable condition of HRQoL for men, suggesting that metabolic health may associate with HRQoL more than obesity for males. In women, the MAO and MHO groups had the most adversely affected HRQoL, implying that MHO is not a favorable health condition and that obesity, in general, may be strongly associated with HRQoL in women.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
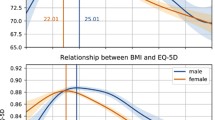
The rise in the prevalence of obesity worldwide over the past decade has become a health issue. The World Health Organization (WHO) estimated that over 600 million people worldwide (11 % men and 15 % women) were obese (body mass index [BMI] ≥ 30 kg/m2) in 2014, a number that has doubled since 1980 [1]. In South Korea in 2012, about one-third of adult men (36.3 %) and more than one-fourth of adult women (28.0 %) were obese (BMI ≥ 25 kg/m2), a number that increased with age for women, peaking at 43.1 % between the ages of 60 and 69 [2]. Obesity has been recognized as a public health problem by the Korean Health Plan 2020 [3]. The risk of complications from obesity, such as diabetes and hypertension, increases in Asian adults when one’s BMI is over 25 kg/m2, which is lower than the complications risk level in Western populations (BMI ≥ 30 kg/m2) [4]. Obesity is the main cause of metabolic disease, increasing the risk of cardiovascular disease (CVD), type 2 diabetes, hypertension, and hyperlipidemia and ultimately leading to higher all-cause mortality [5–8]. Those in the population that are obese in general demonstrate a lower health-related quality of life (HRQoL) than those who are determined to not be obese [9–11]. However, the association between HRQoL and obesity is not consistent by gender, with HRQoL appearing to be worse among obese women than normal weight women [11–13] but the same in both obese and non-obese men [14–16]. Studies have also suggested that adverse health conditions tied to obesity may depend on whether other metabolic risk factors are present [17, 18].
Metabolic syndrome (MetS) denotes a cluster of abdominal obesity, atherogenic dyslipidemia, elevated blood pressure, and insulin resistance as risk factors for CVD [19]. The prevalence of MetS is 49.7 % in the USA [20]; in Korea, 28.2 % of the population and almost half of the adults (44.9 %) are at risk of developing MetS [21]. MetS leads to adverse health conditions; for example, people with MetS generally have a more impaired HRQoL [22–27]. However, the adverse association between MetS and HRQoL is not consistent, presenting sometimes as true among only women [28–30], only men [31], or identifying even better HRQoL among a MetS group [32] or finding no association at all [33, 34]. These incongruent study findings may suggest that the HRQoL of individuals with MetS is associated with other factors such as obesity and disease burden [34]. Therefore, there is no general agreement about how much obesity and/or metabolic health is associated with individuals’ HRQoL.
Recently, studies have paid special attention to those in the general population who are obese but metabolically healthy in lipid profile, glucose tolerance, and blood pressure [5, 35, 36]. These subsets of obese individuals who have favorable metabolic profiles are described as suffering from metabolically healthy obesity (MHO) [36, 37]. The Korean National Health and Nutrition Examination Survey reported that the prevalence of MHO was 14.9 % in the entire population and 47.7 % in the obese population aged over 18 in Korea [38]. Review studies concluded that metabolically healthy obesity (MHO) is not necessarily a healthy condition, in that those individuals in this range develop more cardiovascular events and suffer more from all-cause mortality [39–41] and diabetes [42] over a long-term period than those considered normal weight. Within the topic of metabolic health and obesity type, most studies investigated the prevalence and risk of medical conditions (e.g., cardiovascular disease, diabetes, kidney disorder, infection, and cancer-related mortality). The overall health of MHO individuals may also be adversely affected by quality of life, psychosocial factors, psychosomatic comorbidities, and chronic pain [47]. For several years, it has been suggested that non-metabolic complications such as osteoarthritis, respiratory disease, psychological condition, and quality of life among the MHO population need to be investigated and compared to other obesity types [43–47]. However, few studies have examined MHO in relation to psychological conditions or, in particular, to HRQoL. It seems that only two studies currently available have investigated MHO in relation to quality of life; one study examined the psychosocial profile in those MHO individuals among a population of postmenopausal women [48], while another investigated the impact of the presence or absence of metabolic comorbidity on the association between BMI and HRQoL among the general population of Scotland [49]. Therefore, this study aimed to use a population-based survey to examine the association between HRQoL and four body health types, as well as determine the effects of gender on HRQoL, focusing on the people with metabolically healthy obesity (MHO), in particular. It is hypothesized that the HRQoL of individuals who are metabolically healthy but obese would be worse than those considered metabolically healthy normal weight. A better understanding of the association between HRQoL and body health types could assist with the planning and implementation of health promotion and policies for individuals considered metabolically healthy and obese as well of those presenting as unhealthy but of a normal weight.
Methods
Database and study population
The study data were acquired from the fifth Korea National Health and Nutrition Examination Survey (KNHANES V-2), conducted between 2010 and 2012 by the Korean Centers for Disease Control and Prevention (KCDC). The KNHANES is designed to be a nationally representative cross-sectional survey using a multistage clustered probability sampling design for the random selection of household units. In the first stage of the survey, a sample of geographical areas was drawn, and households were sampled. Sex and age proportions were involved in stratification. The data were assigned weights, provided by KNHANES, to represent the non-institutionalized Korean population in order to account for the complex survey design, missing responses, and post-stratification [50]. The KNHANES study protocol was approved by the institutional review board of the KCDC, and all respondents signed informed consent forms. This study selected a total of 14,460 people (aged ≥30) who completed a health interview and health examination.
Measures
EQ-5D
HRQoL was evaluated using the EuroQol 5-dimension (EQ-5D) questionnaire. The EQ-5D, one of the most widely used tools to measure HRQoL, records the level of self-reported problems on mobility, self-care, usual activities, pain/discomfort, and anxiety/depression. Each dimension is assessed with three response levels (no problem, some problems, and extreme problems) [51]. A single health indexFootnote 1 was calculated using these dimensions in conjunction with the Korea valuation set developed by the KCDC with the time trade-off technique from a representative national sample and validated by comparing with previous Korean and other studies [52].
The calculated index is scaled to 1 if there are no health problems across the five dimensions and is decremented by the presence of poor health on any dimension. A higher EQ-5D index represents a better state of HRQoL [52]. In this study, where each domain originally had three levels, each domain was collapsed into two groups: no problems and some or extreme problems; the number of subjects in the extreme problems category was few and therefore justified collapsing these two categories. In a previous study, using both UK and Korean value sets, the mean of the EQ-5D preference score was 0.89 for the representative national population; a subject with >0.89 was considered as having a good health status [29]. Thus, the impaired HRQoL for this study population was defined as <0.89 of the EQ-5D index.
Metabolic syndrome and BMI
Metabolic abnormality was defined by the criteria of the National Cholesterol Education Program Adult Treatment panel III: the lower waist circumference cut point for Asians [53], elevated waist circumference (≥90 cm in men and ≥80 cm in women), elevated triglycerides (≥150 mg/dL or the use of medication for hyperlipidemia), reduced high-density lipoprotein cholesterol (HDL-C) (<40 mg/dL in men and <50 mg/dL in women), elevated blood pressure (≥130 mm Hg or ≥85 mm Hg or taking anti-hypertension medication), or elevated fasting glucose (≥100 mg/dL or taking anti-hyperglycemic agent). Metabolic syndrome was defined as the presence of three or more of the five risk factors above [54]. Obesity was based on BMI as characterized by the WHO Regional Office for the Western Pacific Region criteria, which defined a BMI of less than 25 kg/m2 as normal as and greater than or equal to 25 kg/m2 as obese [55]. Participants were grouped into one of four body health types based on their metabolic abnormality and obesity: metabolically healthy normal weight (MHNW), metabolically healthy obesity (MHO), metabolically abnormal but normal weight (MANW), and metabolically abnormal obesity (MAO).
Covariates
The following self-reported sociodemographic variables were used as covariates in the analysis: age, monthly household income, education (elementary, middle, high, and university), and marital status (single, married, and widow/divorced/separated). Lifestyle groupings included those who had smoked at least 100 cigarettes in their lifetime and currently smoked (Yes/No); those who drank heavily, defined as the consumption of more than seven units of alcohol for men and more than five units for women on at least 2 days of the week (Yes/No); and those who were physically inactive, measured as not having had more than 150 min of moderate-intensity physical activity per week or 75 min of vigorous-intensity physical activity per week (Yes/No). Health examination data of height, weight, and waist circumference (WC) were used. Body mass index (BMI) was calculated using body weight and height (kg/m2). Systolic and diastolic blood pressures were measured three times at 5-min intervals by trained nurses, and the averages of the second and third recorded numbers were used. After 12 h of fasting, subjects were tested for blood sugar, total cholesterol, high-density lipoprotein (HDL) cholesterol, low-density lipoprotein (LDL) cholesterol, and triglyceride levels. Chronic disease was determined by a doctor’s diagnosis or treatment for the following diseases: hypertension, diabetes mellitus, cardiovascular disease (including angina pectoris, myocardial infarction, and stroke), musculoskeletal illness (including osteoarthritis and rheumatoid arthritis), lung disease (including pulmonary tuberculosis and asthma), and neoplasm cancer (Yes/No). Additionally, menopause status was asked of women respondents (Yes/No).
Data analysis
The participants were analyzed by gender (6217 men and 8243 women) and according to body health type.
All analyses were conducted by using the analysis of complex survey data provided by SPSS 18.0 to incorporate KNHANES provided weights for geographical area, gender, and age of the total Korean population and to account for missing data. The SPSS CSGLM program used in the analyses accounts for the complex sample design by using the KNHANES sample weights incorporating the stratification and clustering in the study’s design. The KNHANES defines the specific variables of the stratification, cluster, and weight and explanations in detail in their manual of data analysis [56]. All analyses in this study used the appropriately weighted data.
Comparison of the variables across the four categories of body health types was made using the complex samples general linear model (CSGLM) for continuous variables and the Chi-square test for categorical variables provided for complex sample design [56]. The CSGLM procedure performs linear regression analysis for weighted data from complex sampling designs allowing for appropriate calculation of standard errors. The association between HRQoL as a dichotomous outcome and body health types was analyzed using complex samples binary logistic regression analysis to examine odds ratio and 95 % confidence interval, with those respondents identified as metabolic healthy normal weight (MHNW) set as the reference group. The CSGLM procedure specified for a binary outcome performs logistic regression with the appropriately weighted data. Three models were performed: unadjusted (Model 1); adjusted for age (Model 2); and adjusted for all potential covariates including sociodemographic variables, life styles, and comorbidity (Model 3). Outcomes of those three models were mobility, self-care, usual activity, pain/discomfort, anxiety/depression, and impaired HRQoL. Menopause was additionally included in the Model 3 analysis of women because hormonal changes affect metabolic health and quality of life for women [29].
Results
Characteristics of the study population
Baseline characteristics of the study population by body health type are given in Table 1 (for men) and Table 2 (for women). In men, the distribution was MHNW (51.2 %), MANW (12.6 %), MHO (16.2 %), and MAO (20.0 %), while in women it was MHNW (54.9 %), MANW (13.9 %), MHO (12.1 %), and MAO (19.2 %). More men were metabolically healthy obese (MHO) than women. Older women tended to be metabolically abnormal compared to younger women. Both men and women in the MANW category were in the lowest education level group and were the highest percentage of widow/divorced/separated participants, probably because MANW individuals tended to be older than those subjects in the other groups. The male MANW participants had the highest systolic blood pressure, fasting blood glucose, triglycerides levels, the lowest HDL-C, and the highest prevalence of all chronic diseases compared to the other body health types for the gender, even higher than that of those in the MAO men group. Significantly, the MHO group of men reported smoking the least but drinking the most heavily. Within the female group, those registering as suffering from MAO had the worst blood serum markers (fasting blood glucose, triglycerides level, HDL-C) and the highest prevalence of musculoskeletal disease and cancer. MANW women had the highest systolic blood pressure and hypertension, diabetes, CVD, and lung disease of the women. The highest proportion of MHO women were heavy drinkers (13.6 %), but no significant difference was found in those who smoked. The proportion of women in menopause ranged from 34.6 % in the MHNW group to 83.2 % in the MANW group, with a mean of 47.8 %.
HRQoL by body health type
Men presented a higher score than women on the EQ-5D index, with a range from 0.958 to 0.964 and a mean of 0.961. Women scored 0.925–0.931 with a mean of 0.928. Table 3 presents the frequency and percentage of having “some or severe problems” for each domain and the frequency and percentage of impaired HRQoL (<0.89 EQ-5D index) across the body health types. Overall, the domain of pain/discomfort had the highest percentage of subjects responding “some or extreme problems” (16.5 % of men and 27.2 % of women), followed by the mobility domain; self-care had the lowest percentage of respondents identifying “some or extreme problems” (3.0 % for men and 4.7 % for women). More women (23.5 %) reported an impaired HRQoL than men (12.2 %). Compared to all other types, MANW men statistically significantly had the highest proportion of subjects who responded “some or extreme problems” in the three domains (mobility, self-care, and usual activities) (p < 0.001, p = 0.008, p = 0.001) and impaired HRQoL category (p < 0.001). MHNW men had slightly higher percentages in all domains than MHO men. In contrast, MANW and MAO women similarly represented the most in all domains, and the MHO group had a lower percentage than the MHNW group. More than 30 % of both the MANW and MAO women reported “some and severe problems” in the domains of mobility and pain/discomfort, and almost 40 % in each group (38.8 and 37.6 %, respectively) belonged to the impaired HRQoL group.
Effects of body health types on HRQoL
Table 4 presents the odds ratio (OR) of having some or severe problems relative to no problems and 95 % confidence interval (95 % CI) of each type against MHNW as a reference group. In unadjusted analysis, metabolically abnormal normal weight (MANW) men were associated with a higher OR of having some or severe problems than the reference group (MHNW) in all of the five domains of EQ-5D and impaired HRQoL, with an OR range from 1.33 to 1.87 (Model 1), and when adjusting for age, all significant ORs of MANW men disappeared except impaired HRQoL (Model 2). When adjusting for relevant covariates, the ORs for the metabolically healthy obesity (MHO) group were significantly increased in the dimension of mobility in the EQ-5D (OR 1.43, 95 % CI 1.00–2.05). In contrast, the effects on HRQoL of types differed in the women participants. In Model 1, compared to the reference group (MHNW), three types showed higher odds ratios of having some or severe problems in all domains of the EQ-5D and impaired HRQoL, with an odds ratio range from 1.33 to 4.54. The significant higher ORs of the metabolically healthy obesity (MHO) women remained in all domains of the EQ-5D (Model 2). Mobility still was worse among the MHO (OR 1.69, 95 % CI 1.31–2.18) and MAO (OR 1.68, 95 % CI 1.33–2.11) groups, and the significant OR on the domain of usual activities in the MAO group was persistent (OR 1.29, 95 % CI 1.00–1.67) (Model 3). Finally, both the MHO and MAO groups showed significantly a higher odds ratio of impaired HRQoL, 1.40 (95 % CI 1.13–1.74) and 1.43 (95 % CI 1.17–1.74), respectively.
Discussion
In this study, we used a nationally representative sample of Korean adults, 30 years or older, to examine the relationship between body health types, classified by BMI category and metabolic health status, and HRQoL. Under the definition of obesity from the National Cholesterol Education Program Adult Treatment panel III, 16.2 % of the men and 12.1 % of the women were considered metabolically healthy obesity (MHO), with it being more prevalent among the men. Those men in the metabolically healthy obesity (MHO) category were younger, more educated, less likely to be currently smoking, and drank more heavily than men in other groups. The MHO women were the heaviest drinkers of the participating females. In the previous studies, MHO is more prevalent among women [57–59] who are young, currently smoke, drink moderately, and have a high level of physical activity in relation to other groups [57]. These differences of MHO prevalence by gender and relating factors between the previous studies and this study may be derived from the definition of metabolic health status and central obesity that is used in each study. This study indicates that both Korean males and females who drink heavily may be at risk of becoming MHO.
Women had a poorer HRQoL compared to men in all domains (Table 3), a finding consistent with many previous studies examining the association between HRQoL and obesity or metabolic syndrome separately [9, 10, 15, 16, 29]. However, the interaction effect of obesity and metabolic health status on HRQoL differs by gender. Metabolically abnormal normal weight (MANW) men showed the worst blood serum markers (Table 1) and a poorer HRQoL than healthy obese men (MHO) (Table 3). Impaired HRQoL (EQ-5D index <0.89) still remains higher in MANW men than the reference group, meaning that a metabolically unhealthy status is associated with stronger negative effects on HRQoL than an obese status. In a previous study, obesity-related HRQoL for overweight Korean men was not worse than that of those at a normal weight [16]. Obesity paradox, meaning those obese individuals who have healthy metabolic and cardiorespiratory fitness or appear to have a good quality of life [60], may be present among the men in this study [61]. That previous studies found no relationship between obesity and HRQoL among Korean men [14–16] may support this account.
In the case of women, the HRQoL of the metabolically unhealthy normal weight (MANW) and unhealthy obesity (MAO) groups was similarly worse than that of the reference group (Tables 3, 4). Meaningfully, it was found that healthy obesity (MHO) remains statistically significant and has as large of a negative impact as unhealthy obesity (MAO) in women. Unlike men, the odds ratio of an impaired HRQoL for metabolically unhealthy normal weight (MANW) women was not significantly higher when compared to metabolically healthy normal weight (MHNW) women, but the odds ratios for both the metabolically healthy obesity (MHO) and unhealthy obesity (MAO) groups were high. These findings may imply that obesity among women is more strongly associated with a decreased HRQoL than metabolic health or other confounding factors. Major symptomatic consequences of abdominal obesity, such as excessive daytime sleepiness and fatigue, may also decrease the HRQoL of women [62]. There was an interaction effect on EQ-5D scores between gender and abdominal obesity, indicating that women with abdominal obesity had a lower HRQoL compared to those with what is considered a normal waist circumference, but this effect was not apparent for men [15].
Mobility was the most adversely affected domain for both men and women among the metabolically healthy obesity (MHO) and unhealthy obesity (MAO) groups. Obesity may negatively affect mobility more than other domains of the EQ-5D. In both men and women, obesity had the biggest impact on impaired mobility [10]. The lower quality of life of obese men and women was attributed to the physical functioning aspect of HRQoL [11, 13]. The anxiety/depression dimension in MHO women showed the highest odds ratio compared to all other body health types, while the negative effect disappeared among those in the MAO group, and this finding needs special attention. Mental health quality scores were significantly lower for obese women than normal weight women but not for obese men when compared to normal weight men. Korean scholars have suggested that this should be interpreted in a sociocultural context; elderly Korean men recognize being overweight is not as a negative but as a symbol of wealth, whereas body image may negatively influence self-esteem and depression for women [16, 29]. In many Asian countries, including Taiwan, being moderately overweight for men is still valued as a symbol of good health and prosperity [13]. Some studies in non-Asian settings also showed that the adverse effect of obesity on mental health quality was more apparent among obese women compared to obese men [63–66], suggesting that obesity may make women more anxious, depressive, and psychologically distressed irrespective of culture. The impairment of usual activity appeared as a problem to unhealthy obese women, but self-care and pain/discomfort did not present any significant differences by body health types for either men or women in this study. The impact of metabolic health on the dimensions of EQ-5D is not consistent as shown in the previous studies and this study; pain/discomfort showed an increased OR in subjects with MetS [25], and men with MetS had the impaired usual activities while women with MetS reported problems across all 5 EQ-5D dimensions [29].
The interaction effects of obesity and metabolically unhealthy status on HRQoL appeared differently by gender in this study. To the best of our knowledge, there was only one other study looking at the interaction effect between obesity and metabolic health on HRQoL; a national study in Scotland reported the impact of obesity as greater among individuals with metabolic comorbidity than those without metabolic comorbidity [49]. Thus, further investigation examining the interaction effect of obesity and metabolic health on HRQoL in different settings should be conducted.
This study helps us understand the burden of obesity and metabolic syndrome on HRQoL by body health type, which is a current medical issue. Metabolically unhealthy normal weight (MANW) men were the most affected group for impaired HRQoL when controlled for age. Adversely, in the case of women, the metabolically unhealthy obesity (MAO) group had the worst HRQoL status followed by the metabolically healthy obesity (MHO) group. This study concludes that metabolically healthy obesity (MHO) is associated with reduced HRQoL for women but not for men. Thus, healthcare providers and health policies should pay attention to the impact that combinations of obesity and metabolic health have on HRQoL, controlling for gender, when making and evaluating population-based health programs. More attention should be given to the interaction effects of gender when analyzing the impact of obesity on HRQoL, as well [14]. For example, lifestyle interventions that engage diet, nutritional counseling, and weight loss efforts can be made to improve women’s HRQoL, and management of metabolic health such as lowing blood pressure and fasting glycemia should be a focus for men [67]. The impaired quality of life with obesity and/or metabolic syndrome can be a barrier to engagement in weight loss efforts. A longitudinal study demonstrated that subjects with metabolic syndrome and obesity had increased risk of cardiovascular disease and mortality [68]. Therefore, a greater understanding of gender differences related to the association between obesity and metabolic health on HRQoL will be useful in improving the quality of life for individuals.
This study has both strengths and limitations. This was the first study to examine the effects of obesity and metabolic status together on HRQoL with adjustment for the potential confounding factors (sociodemographic variables, lifestyle factors, and disease comorbidity). A large sample of a general population allowed for a direct comparison by gender among body health types. There are a number of limitations to this study. First, we used a cross-sectional study design, which may not guarantee a causal relationship between body health types and HRQoL. Second, each dimension does not take into consideration the importance of specific aspects of HRQoL to the individual. Third, we used BMI to determine the obesity group, but BMI cannot distinguish body fat from muscle. In addition, there was no distinguishing BMI between 25–30 and >30 kg/m2 since we placed both in the obesity group. Last, the generalizability of the results is limited to the non-institutionalized population. Further research examining those factors that influence gender differences in HRQoL according to the four body health types is warranted.
Notes
Predicted values of the EQ-5D index = full health-disutility \(\begin{aligned} {\text{Full}}\;{\text{health}} & = 1.000 \\ & = 1 - \left(0.050 + 0.096*{\text{M}}2 + 0.418*{\text{M}}3 + 0.046*{\text{SC}}2 \right.\\ & \quad + \,0.136*{\text{SC}}3 + 0.051*{\text{UA}}2 + 0.208*{\text{UA}}3 + 0.037*{\text{PD}}2 \\ & \left.\quad + \,0.151*{\text{PD}}3 + 0.043*{\text{AD}}2 + 0.158*{\text{AD}}3 + 0.050*{\text{N}}3\right) \end{aligned}\)(M2, mobility level 2; M3, mobility level 3; SC2, self-care level 2; SC3, self-care level 3; UA2, usual activities level 2; UA3, usual activities level 3; PD2, pain or discomfort level 2; PD3, pain or discomfort level 3;AD2, anxiety or depression level 2; AD3, anxiety or depression level 3; N3, any dimension on level 3).
Abbreviations
- HRQoL:
-
Health-related quality of life
- EQ-5D:
-
EuroQol-5 dimension questionnaire
- BMI:
-
Body mass index
- KNHANES:
-
Korea National Health and Nutrition Examination Survey
- KCDC:
-
Korean Centers for Disease Control and Prevention
- MetS:
-
Metabolic syndrome
- MHNW:
-
Metabolically healthy normal weight
- MANW:
-
Metabolically abnormal but normal weight
- MHO:
-
Metabolically healthy obesity
- MAO:
-
Metabolically abnormal obesity
- CVD:
-
Cardiovascular disease
References
World Health Organization (WHO). (2015). Obesity and overweight (Fact sheet N311). http://www.who.int/mediacentre/factsheets/fs311/en/. Accessed February 13, 2015.
Ministry of Health & Welfare and Korea Center for Disease Control & Prevention. (2013). 2012 Korea national health and nutrition examination survey. Chungbuk, Osong: Ministry of Health & Welfare and Korea Center for Disease Control & Prevention.
Korea Ministry of Health. (2011). The 3rd national health plan 2020. Retrieved from https://www.mindbank.info/item/4070.
James, W. P. T., Chunming, C., & Inoue, S. (2002). Appropriate Asian body mass indices? Obesity Reviews, 3(3), 139.
Plourde, G., & Karelis, A. D. (2014). Current issues in the identification and treatment of metabolically healthy but obese individuals. Nutrition, Metabolism, and Cardiovascular Diseases, 24(5), 455–459. doi:10.1016/j.numecd.2013.12.002.
Aung, K., Lorenzo, C., Hinojosa, M. A., & Haffner, S. M. (2014). Risk of developing diabetes and cardiovascular disease in metabolically unhealthy normal-weight and metabolically healthy obese individuals. The Journal of Clinical Endocrinology and Metabolism, 99(2), 462–468. doi:10.1210/jc.2013-2832.
Aballay, L. R., Eynard, A. R., del Pilar Díaz, M., Navarro, A., & Muñoz, S. E. (2013). Overweight and obesity: A review of their relationship to metabolic syndrome, cardiovascular disease, and cancer in South America. Nutrition Reviews, 71(3), 168–179.
Oh, S. W. (2011). Obesity and metabolic syndrome in Korea. Diabetes & Metabolism Journal, 35(6), 561–566.
Serrano-Aguilar, P., Muñoz-Navarro, S. R., Ramallo-Fariña, Y., & Trujillo-Martín, M. M. (2009). Obesity and health related quality of life in the general adult population of the Canary Islands. Quality of Life Research, 18(2), 171–177. doi:10.1007/s11136-008-9427-1.
Søltoft, F., Hammer, M., & Kragh, N. (2009). The association of body mass index and health-related quality of life in the general population: Data from the 2003 health survey of England. Quality of Life Research, 18(10), 1293–1299. doi:10.1007/s11136-009-9541-8.
Vasiljevic, N., Ralevic, S., Marinkovic, J., Kocev, N., Maksimovic, M., Milosevic, G. S., & Tomic, J. (2008). The assessment of health-related quality of life in relation to the body mass index value in the urban population of Belgrade. Health and Quality of Life Outcomes., 6, 106. doi:10.1186/1477-7525-6-106.
Mannucci, E., Ricca, V., Barciulli, E., Di Bernardo, M., Travaglini, R., Cabras, P. L., & Rotella, C. M. (1999). Quality of life and overweight: The obesity related well-being (Orwell 97) questionnaire. Addictive Behaviors, 24(3), 345–357.
Huang, I., Frangakis, C., & Wu, A. (2006). The relationship of excess body weight and health-related quality of life: Evidence from a population study in Taiwan. International Journal of Obesity, 30(8), 1250–1259.
Choo, J., Turk, M. T., Jae, S.-Y., & Choo, I. H. (2014). Factors associated with health-related quality of life among overweight and obese Korean women. Women and Health, 55(2), 152–166. doi:10.1080/03630242.2014.979966.
Choo, J., Jeon, S., & Lee, J. (2014). Gender differences in health-related quality of life associated with abdominal obesity in a Korean population. BMJ Open, 4(1), e003954. doi:10.1136/bmjopen-2013-003954.
Song, H., Park, H., Yun, K., Cho, S., Choi, E., Lee, S., et al. (2010). Gender and age differences in the impact of overweight on obesity-related quality of life among Korean adults. Obesity Research & Clinical Practice, 4(1), e15–e23.
Bluher, M. (2010). The distinction of metabolically ‘healthy’ from ‘unhealthy’ obese individuals. Current Opinion in Lipidology, 21(1), 38–43. doi:10.1097/MOL.0b013e3283346ccc.
Denis, G. V., & Obin, M. S. (2013). ‘Metabolically healthy obesity’: Origins and implications. Molecular Aspects of Medicine, 34(1), 59–70. doi:10.1016/j.mam.2012.10.004.
Grundy, S. M., Brewer, H. B., Cleeman, J. I., Smith, S. C., & Lenfant, C. (2004). Definition of metabolic syndrome report of the National Heart, Lung, and Blood Institute/American Heart Association Conference on scientific issues related to definition. Circulation, 109(3), 433–438.
Lai, L. Y., Petrone, A. B., Pankow, J. S., Arnett, D. K., North, K. E., Ellison, R. C., et al. (2015). Lack of association of apolipoprotein E (Apo E) polymorphism with the prevalence of metabolic syndrome: The National Heart, Lung and Blood Institute Family Heart Study. Diabetes/Metabolism Research and Reviews,. doi:10.1002/dmrr.2638.
Park, S., Kim, S.-J., Lee, M., Kang, K.-A., & Hendrix, E. (2015). Prevalence and associated factors of metabolic syndrome among South Korean adults. Journal of Community Health Nursing, 32(1), 24–38.
Tziallas, D., Kastanioti, C., Savvas, K., Kostapanos, M. S., Tziallas, V., Skapinakis, P., et al. (2012). Evaluation of health related quality of life in patients with metabolic syndrome. Health Science Journal, 6(1), 116–128.
Okosun, I. S., Annor, F., Esuneh, F., & Okoegwale, E. E. (2013). Metabolic syndrome and impaired health-related quality of life and in non-Hispanic White, non-Hispanic Black and Mexican-American Adults. Diabetes & Metabolic Syndrome: Clinical Research & Reviews, 7(3), 154–160.
Tziallas, D., Kastanioti, C., Kostapanos, M. S., Skapinakis, P., Elisaf, M. S., & Mavreas, V. (2012). The impact of the metabolic syndrome on health-related quality of life: A cross-sectional study in Greece. European Journal of Cardiovascular Nursing, 11(3), 297–303.
Han, J., Park, H., Shin, C., Chang, H., Yun, K., Cho, S., et al. (2009). Metabolic syndrome and quality of life (QOL) using generalised and obesity-specific QOL scales. International Journal of Clinical Practice, 63(5), 735–741.
Miettola, J., Niskanen, L. K., Viinamäki, H., Sintonen, H., & Kumpusalo, E. (2008). Metabolic syndrome is associated with impaired health-related quality of life: Lapinlahti 2005 study. Quality of Life Research, 17(8), 1055–1062.
Ford, E. S., & Li, C. (2008). Metabolic syndrome and health-related quality of life among US adults. Annals of Epidemiology, 18(3), 165–171.
Amiri, P., Hosseinpanah, F., Rambod, M., Montazeri, A., & Azizi, F. (2010). Metabolic syndrome predicts poor health-related quality of life in women but not in men: Tehran lipid and glucose study. Journal of Women’s Health (15409996), 19(6), 1201–1207. doi:10.1089/jwh.2009.1710.
Sohn, Y. J., Sohn, H. S., & Kwon, J. W. (2011). Gender differences among middle-aged Koreans for health-related quality of life related to metabolic syndrome. Quality of Life Research, 20(4), 583–592. doi:10.1007/s11136-010-9789-z.
Sarrafzadegan, N., Gharipour, M., Ramezani, M. A., Rabiei, K., Zolfaghar, B., Tavassoli, A. A., et al. (2011). Metabolic syndrome and health-related quality of life in Iranian population. Journal of Research in Medical Sciences: The Official Journal of Isfahan University of Medical Sciences, 16(3), 254–261.
Laudisio, A., Marzetti, E., Antonica, L., Pagano, F., Vetrano, D. L., Bernabei, R., & Zuccalà, G. (2013). Metabolic syndrome and quality of life in the elderly: Age and gender differences. European Journal of Nutrition, 52(1), 307–316.
Roohafza, H., Sadeghi, M., Talaei, M., Pourmoghaddas, Z., & Sarrafzadegan, N. (2012). Psychological status and quality of life in relation to the metabolic syndrome: Isfahan cohort study. International Journal of Endocrinology,. doi:10.1155/2012/380902.
Lee, Y.-J., Woo, S. Y., Ahn, J. H., Cho, S., & Kim, S. R. (2011). Health-related quality of life in adults with metabolic syndrome: The Korea national health and nutrition examination survey, 2007–2008. Annals of Nutrition & Metabolism, 61(4), 275–280.
Vetter, M. L., Wadden, T. A., Lavenberg, J., Moore, R. H., Volger, S., Perez, J. L., et al. (2011). Relation of health-related quality of life to metabolic syndrome, obesity, depression and comorbid illnesses. International Journal of Obesity, 35(8), 1087–1094.
Ärnlöv, J., Sundström, J., Ingelsson, E., & Lind, L. (2011). Impact of BMI and the metabolic syndrome on the risk of diabetes in middle-aged men. Diabetes Care, 34(1), 61–65.
Karelis, A. D. (2008). Metabolically healthy but obese individuals. Lancet, 372(9646), 1281–1283. doi:10.1016/s0140-6736(08)61531-7.
Wildman, R. P., Muntner, P., Reynolds, K., McGinn, A. P., Rajpathak, S., Wylie-Rosett, J., & Sowers, M. R. (2008). The obese without cardiometabolic risk factor clustering and the normal weight with cardiometabolic risk factor clustering: Prevalence and correlates of 2 phenotypes among the US population (NHANES 1999–2004). Archives of Internal Medicine, 168(15), 1617–1624. doi:10.1001/archinte.168.15.1617.
Hong, H. C., Lee, J. S., Choi, H. Y., Yang, S. J., Yoo, H. J., Seo, J. A., et al. (2013). Liver enzymes and vitamin D levels in metabolically healthy but obese individuals: Korean National Health and Nutrition Examination Survey. Metabolism, 62(9), 1305–1312.
Kramer, C. K., Zinman, B., & Retnakaran, R. (2013). Are metabolically healthy overweight and obesity benign conditions? A systematic review and meta-analysis. Annals of Internal Medicine, 159(11), 758–769. doi:10.7326/0003-4819-159-11-201312030-00008.
Fan, J., Song, Y., Chen, Y., Hui, R., & Zhang, W. (2013). Combined effect of obesity and cardio-metabolic abnormality on the risk of cardiovascular disease: A meta-analysis of prospective cohort studies. International Journal of Cardiology, 168(5), 4761–4768. doi:10.1016/j.ijcard.2013.07.230.
Roberson, L. L., Aneni, E. C., Maziak, W., Agatston, A., Feldman, T., Rouseff, M., et al. (2014). Beyond BMI: The “metabolically healthy obese” phenotype & its association with clinical/subclinical cardiovascular disease and all-cause mortality—A systematic review. BMC Public Health, 14, 14. doi:10.1186/1471-2458-14-14.
Bell, J. A., Kivimaki, M., & Hamer, M. (2014). Metabolically healthy obesity and risk of incident type 2 diabetes: A meta-analysis of prospective cohort studies. Obesity Reviews, 15(6), 504–515. doi:10.1111/obr.12157.
Bluher, S., & Schwarz, P. (2014). Metabolically healthy obesity from childhood to adulthood—Does weight status alone matter? Metabolism, 63(9), 1084–1092. doi:10.1016/j.metabol.2014.06.009.
Bradshaw, P. T., Monda, K. L., & Stevens, J. (2013). Metabolic syndrome in healthy obese, overweight, and normal weight individuals: The atherosclerosis risk in communities study. Obesity (Silver Spring), 21(1), 203–209. doi:10.1002/oby.20248.
Jokela, M., Hamer, M., Singh-Manoux, A., Batty, G. D., & Kivimaki, M. (2014). Association of metabolically healthy obesity with depressive symptoms: Pooled analysis of eight studies. Molecular Psychiatry, 19(8), 910–914. doi:10.1038/mp.2013.162.
Payab, M., Hasani-Ranjbar, S., & Larijani, B. (2014). Whether all obese subjects both in metabolic groups and non-metabolic groups should be treated or not. Journal of Diabetes and Metabolic Disorders, 13(1), 21. doi:10.1186/2251-6581-13-21.
Bluher, M. (2014). Are metabolically healthy obese individuals really healthy? European Journal of Endocrinology, 171(6), R209–R219. doi:10.1530/eje-14-0540.
Karelis, A. D., Fontaine, J., Rabasa-Lhoret, R., Prud’homme, D., Doucet, E., Blanchard, C., et al. (2006). Psychosocial profile of the metabolically healthy but obese postmenopausal woman. Diabetes & Metabolism, 32(1), 90–91.
Ul-Haq, Z., Mackay, D. F., Fenwick, E., & Pell, J. P. (2012). Impact of metabolic comorbidity on the association between body mass index and health-related quality of life: A Scotland-wide cross-sectional study of 5,608 participants. BMC Public Health, 12(1), 143.
Kweon, S., Kim, Y., Jang, M. J., Kim, Y., Kim, K., Choi, S., et al. (2014). Data resource profile: The Korea national health and nutrition examination survey (KNHANES). International Journal of Epidemiology, 43(1), 69–77. doi:10.1093/ije/dyt228.
Group, T. E. (1990). EuroQol-a new facility for the measurement of health-related quality of life. Health Policy, 16(3), 199–208.
Lee, Y. K., Nam, H. S., Chuang, L. H., Kim, K. Y., Yang, H. K., Kwon, I. S., et al. (2009). South Korean time trade-off values for EQ-5D health states: Modeling with observed values for 101 health states. Value in Health, 12(8), 1187–1193.
Grundy, S. M., Cleeman, J. I., Daniels, S. R., Donato, K. A., Eckel, R. H., Franklin, B. A., et al. (2005). Diagnosis and management of the metabolic syndrome: An American Heart Association/National Heart, Lung, and Blood Institute scientific statement. Circulation, 112(17), 2735–2752.
Tan, K. (2004). Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. The Lancet, 363(9403), 157–163.
Yumi, J. (2015). Workshop of the 6th Korea national health and nutrition examination survey and youth health online survey on data analysis. http://yhs.cdc.go.kr/common/getfile.asp. Accessed February 13, 2015.
Phillips, C. M., Dillon, C., Harrington, J. M., McCarthy, V. J., Kearney, P. M., Fitzgerald, A. P., & Perry, I. J. (2013). Defining metabolically healthy obesity: Role of dietary and lifestyle factors. PLoS ONE, 8(10), e76188. doi:10.1371/journal.pone.0076188.
Lopez-Garcia, E., Guallar-Castillon, P., Leon-Munoz, L., & Rodriguez-Artalejo, F. (2013). Prevalence and determinants of metabolically healthy obesity in Spain. Atherosclerosis, 231(1), 152–157. doi:10.1016/j.atherosclerosis.2013.09.003.
Al Suwaidi, J. (2014). Is there an increased cardiovascular risk in metabolically healthy obese individuals? Lessons from the HUNT (Nord-Trondelag Health) study. Global Cardiology Science & Practice, 2014(2), 44–47. doi:10.5339/gcsp.2014.24.
van Vliet-Ostaptchouk, J. V., Nuotio, M.-L., Slagter, S. N., Doiron, D., Fischer, K., Foco, L., et al. (2014). The prevalence of metabolic syndrome and metabolically healthy obesity in Europe: A collaborative analysis of ten large cohort studies. BMC Endocrine Disorders, 14(1), 178–197.
Lavie, C. J., De Schutter, A., & Milani, R. V. (2015). Healthy obese versus unhealthy lean: The obesity paradox. Nature Reviews Endocrinology, 11(1), 55–62.
Zhu, Y. (2013). “Obesity paradox” a phenomenon based upon the health-related outcome on quality of life. Zhonghua Liu Xing Bing Xue Za Zhi = Zhonghua Liuxingbingxue Zazhi, 34(3), 294–296.
Vgontzas, A. N., Bixler, E. O., & Chrousos, G. P. (2006). Obesity-related sleepiness and fatigue. Annals of the New York Academy of Sciences, 1083(1), 329–344.
Bentley, T. G., Palta, M., Paulsen, A. J., Cherepanov, D., Dunham, N. C., Feeny, D., et al. (2011). Race and gender associations between obesity and nine health-related quality-of-life measures. Quality of Life Research, 20(5), 665–674.
Carpenter, K. M., Hasin, D. S., Allison, D. B., & Faith, M. S. (2000). Relationships between obesity and DSM-IV major depressive disorder, suicide ideation, and suicide attempts: Results from a general population study. American Journal of Public Health, 90(2), 251.
Istvan, J., Zavela, K., & Weidner, G. (1992). Body weight and psychological distress in NHANES I. International Journal of Obesity and Related Metabolic Disorders: Journal of the International Association for the Study of Obesity, 16(12), 999–1003.
Jorm, A. F., Korten, A. E., Christensen, H., Jacomb, P. A., Rodgers, B., & Parslow, R. A. (2003). Association of obesity with anxiety, depression and emotional well-being: A community survey. Australian and New Zealand Journal of Public Health, 27(4), 434–440.
Dalzill, C., Nigam, A., Juneau, M., Guilbeault, V., Latour, E., Mauriège, P., et al. (2014). Intensive lifestyle intervention improves cardiometabolic and exercise parameters in metabolically healthy obese and metabolically unhealthy obese individuals. Canadian Journal of Cardiology, 30(4), 434–440.
Ärnlöv, J., Ingelsson, E., Sundström, J., & Lind, L. (2010). Impact of body mass index and the metabolic syndrome on the risk of cardiovascular disease and death in middle-aged men. Circulation, 121(2), 230–236.
Funding
This paper was supported by International research funds for humanities and social science of Chonbuk National University in 2015.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author declares that she has no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional review board.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Yang, Y., Herting, J.R. & Choi, J. Obesity, metabolic abnormality, and health-related quality of life by gender: a cross-sectional study in Korean adults. Qual Life Res 25, 1537–1548 (2016). https://doi.org/10.1007/s11136-015-1193-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-015-1193-2