Abstract
It has been suggested that psychiatric multimorbidity may better characterize severely impaired psychiatric patients than individual severe mental illness (SMI) diagnoses, and that these patients may be better served by centers offering integrated co-located, psychiatric and social services than in conventional clinics providing one-to-one care. We tested the hypothesis that multimorbidity is a critical characteristic of Veterans treated at a co-located multi-service Veteran’s Health Administration (VHA) program originally established to treat Veterans living with SMI. Administrative data from the VA Connecticut Health Care System from fiscal year 2012 were used to compare veterans using diverse mental health and social services at the Errera Community Care Center (ECCC), an integrated “one-stop shop” for SMI veterans, and those seen exclusively at standard outpatient mental health clinics. Bivariate and multiple logistic regression analyses were used to compare groups on demographic characteristics, psychiatric and medical diagnoses, service utilization, and psychotropic medication fills. Results: Of the 11,092 veterans included in the study, 2281 (20.6%) had been treated at the ECCC and 8811 (79.4%) had not. Multivariable analysis highlighted the association of treatment in the ECCC and younger age, lower income, homelessness, and especially multimorbidity including both multiple substance use and multiple psychiatric diagnoses. Programs originally designed to address the diverse needs of patients living with SMI and homelessness may be usefully characterized as treating patients with psychiatric multimorbidity, a term of greater clinical relevance. Effectiveness research is needed to evaluate the one-stop shop approach to their treatment.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
There has been a growing recognition that the typical patient seen in real-world psychiatric practice suffers from multiple psychiatric disorders, or multimorbidity, rather than from any one severe mental illness (SMI) [1]. Studies have shown that patients with multimorbidity have more severe symptoms and poorer functioning [2], are more likely to receive dysfunctionally fragmented care [2], and use more services at greater cost than patients with single diagnoses. Ironically patients with a single diagnosis, i.e. without comorbidity, a clinical minority, are typically the exclusive focus of research and professional education [3]. Clinical trials typically exclude patients with comorbidities and current treatment guidelines have yet to fully recognize the distinctive and diverse needs associated with multimorbidity [4].
While research on the clinical epidemiology of multimorbidity has expanded in recent years [5], evidence-based strategies for addressing the complexities of multimorbidity are more limited [6]. Some clinical managers have developed programs for patients living with SMI by co-locating mental health, social and rehabilitative services, along with general medical care together [7]. The well-known Assertive Community Treatment (ACT) model [8, 9] was designed to offer community-based services to people with severe mental illness through a mobile integrated team that includes clinical case managers, sometimes including substance use and vocational specialists. However, ACT has not addressed the full diversity of patent needs, and co-located care models may be more suited to addressing mental health, social, and medical multimorbidity [10, 11]. However, while such programs nominally characterize themselves as treating patients living with SMI there has been little study of participants in such programs as compared to those in general outpatient care [16].
The Veterans Affairs Connecticut (VACT) Healthcare System is a large academically affiliated medical center that treats over 11,000 patients in its specialized mental health programs annually. The Errera Community Care Center (ECCC), named after Paul Errera, a national innovator in care for SMI and homeless veterans, was implemented in 1987 to provide integrated services to veterans hospitalized with SMI as they transitioned to the community. As homelessness among veterans became an issue of growing public concern, a second focus emerged on services for “homeless chronically mentally ill veterans” [12]. The ECCC has offered an incrementally expanding array of services at an off-site location away from the main VA hospital with a recovery-oriented culture [13]. It now offers a “one-stop shop” for clinical care, housing support, vocational rehabilitation, and criminal justice involvement in addition to primary care and peer support. The concept of multimorbidity was not current when the program was developed and has not been part of its clinical identity. Like similar programs, it was conceptualized as an effort to treat veterans living with SMI.
In this study, we compare sociodemographic and diagnostic characteristics along with patterns of service use of veterans treated at the ECCC with those treated exclusively in standard mental health and addiction clinics at the same VA medical center. We hypothesized that a study that explicitly examined measures of multimorbidity rather than single SMI diagnoses may more usefully characterize the veterans seen at the ECCC and similar programs as contrasted to those seen in standard outpatient clinics. In the approach taken here, we begin with a highly integrated service program that evolved over three decades to better serve a population originally defined by a set of single SMI diagnoses, and seek to better understand the clinical characteristics and needs of the patients it serves.
Methods
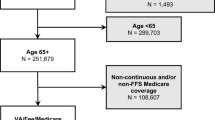
Sample
The sample included all 11,092 veterans who were seen in at least once in a mental health specialty program at the VACT Healthcare System in Fiscal Year (FY) 2012 (October 1, 2011 – September 30, 2012). Groups were classified based on whether they had at least one visit to the ECCC or were seen exclusively at other mental health or substance use clinics.
Measures
Sociodemographic characteristics, medical and psychiatric diagnoses, service use, and psychotropic medication prescription data were taken from a preconstructed dataset created by the Northeast Program Evaluation Center based on national data records from the VHA Computerized Personal Record System.
Demographic characteristics included age, sex, race, VA pension status, service-connected disability status, type of geographic residence (urban vs rural), and homelessness within the past year. Data on rural or urban residence was based on zip codes using the Rural Urban Commuting Area Classification [14]. Homelessness was defined by the presence of an ICD-9 code of V60.0 and/or use of services from a specialized VA homeless program in FY 2012.
Medical diagnoses were included based on those that make up the Charlson comorbidity index [15], a summative measure of medical comorbidity that predicts 1-year mortality. An aggregate dichotomous measure of any pain diagnoses was created and has been described elsewhere [16].
Clustered psychiatric diagnoses included major depressive (ICD-9296.2–296.39) and other depressive disorders (ICD-9300.4x, 296.9x, 301.10–301.19, 311.x), bipolar disorder (ICD-9296.0x, 296.1x, 296.40–296.89), schizophrenia (ICD-9295.x), posttraumatic stress disorder (PTSD) (ICD-9309.81), anxiety disorders (300.xx excluding 300.4) and personality disorder (ICD-9301.x). Also included in the analysis were 7 specific substance use diagnoses (alcohol, cannabis, cocaine, opioid, barbiturate, amphetamine, and hallucinogen). Summary variables were created for a count of the number of psychiatric diagnoses and the number of substance use diagnoses in these clusters.
Clinic stop codes from different types of services were used to derive the measures of VHA health service utilization. Services included general psychiatric care, substance use specialty care, primary care, emergency department visits and sub-specialty mental health care provided only at the ECCC (e.g. ACT-like services, vocational rehabilitation and recovery, and criminal justice services). All visits were counted one per day during days when a stop was recorded.
Psychotropic medications were grouped into antidepressants, antipsychotics, anxiolytic/.
sedative/hypnotics, stimulants, and anticonvulsant/mood stabilizers. Lithium was included as a separate class because of its unique mechanism of action because it is considered a fundamentally different treatment by clinicians. Summary variables were created to represent the total number of psychotropic medication fills during FY 2012 and the proportion of veterans with any psychotropic fills during FY 2012.
Analysis
First, bivariate analyses with chi square and t-tests were used to compare veterans treated at the ECCC to those who were not, on sociodemographic characteristics, psychiatric/medical diagnoses, measures of service use, and psychotropic medication fills.
Since the sample in this study is quite large, the usual significant testing using p values would likely be uninformative or misleading, as small differences in means with little clinical importance would have low p values and would be considered statistically different. We instead calculated effect sizes to identify substantial differences between groups. Cohen’s d was computed for continuous variables and the risk ratios for categorical variables. Cohen’s d is defined as the difference in mean values between groups divided by their pooled standard deviation. Following Cohen [17] we used a cutoff of 0.20 as a threshold for at least a small difference between groups. For categorical variables risk ratio cutoff values of >1.5 or < 0.67 were thresholds indicating substantial differences.
A set of multivariable logistic regression analyses were then used to identify the set of measures that independently differentiated veterans who had been treated in the ECCC and those who received other mental health services. Variables that had been identified as substantially different between the groups based on bivariate comparisons were included in this analysis and evaluated with an alpha of 0.05. We excluded homelessness from the multivariable analysis of service use since homelessness is partially defined by the use of services that are exclusively available at the ECCC. The models were repeated using two approaches to psychiatric diagnoses: 1) treating each individual psychiatric and substance use diagnosis (SUD) as an independent dichotomous variable and 2) addressing multimorbidity directly by using two summary variables reflecting the number of psychiatric (range 0–10) and the number of SUD diagnoses (range 0–7). The analysis was conducted in two steps: first considering sociodemographic characteristics and diagnostic measures, and second, adding measures of service use and psychotropic medication fills while controlling for the sociodemographic and diagnostic measures. Standardized regression coefficients were calculated for comparison of the strength of association of variables since both categorical and continuous measures were included. Model fit was assessed with the c statistic, which ranges from 0.5 indicating no model fit, to 1.0 reflecting perfect model fit. Akaike information criterion (AIC) in which smaller numbers reflect better model fit was also used as an estimator of the relative quality of statistical models.
The study was approved by the Institutional Review Board committee of the VACT Healthcare System. A waiver of informed consent was obtained as the study used administrative data and there were no patient identifiers included. All analyses were conducted using SAS statistical software (version 9.2; SAS Institute Inc., Cary, NC).
Results
Of the 11,092 veterans seen at VA Connecticut in FY 2012, 2281 (20.6%) had been treated in the ECCC and 8811 (79.4%) had not. With a mean age of 56.5 (SD = 15.6), 92.7% were male, 83.0% self-identified as white, and 14.0% as black.
Bivariate analysis showed that those treated in the ECCC were younger, had lower incomes, were more likely to be of black or mixed race, to collect a VA pension (reflecting the combination of wartime service, low income, and disability), and to have recently been homeless (Table 1).
Veterans treated in the ECCC had higher rates of HIV, peptic ulcer, and hepatic diseases but did not differ substantially from others on the overall Charlson index. They were more likely to be diagnosed with SMI such as schizophrenia or other psychotic disorders, bipolar disorder, personality disorders, and dual diagnoses. Treatment in the ECCC was also substantially associated with most substance use diagnoses including alcohol, cannabis, stimulant, and sedative/hypnotic abuse or dependence. On average, ECCC patients had substantially greater numbers of psychiatric and substance use diagnoses overall with moderate to large effect sizes (Table 1).
Veterans treated at the ECCC used far more specialized mental health services, including greater numbers of both general psychiatry and specialty substance use outpatient visits, emergency room visits, and had a greater likelihood of inpatient mental health service use. Veterans treated in the ECCC also used far more subspecialty mental health visits (specific to the ECCC) than general psychiatry and/or specialty substance use visits. They were also prescribed substantially more antipsychotics and mood stabilizers (Table 2).
Multivariable analyses (Table 3) highlighted the independent association of treatment at the ECCC with black race and VA pension among the sociodemographic variables. The first model showed an association with key psychiatric and SUD diagnoses individually, with the strongest effects for schizophrenia (standardized regression coefficient [SRC] = 0.18), opioid (SRC = 0.18), and alcohol abuse or dependence (SRC = 0.17). The second model highlighted the strong association of treatment in the ECCC with the number of SUDs (SRC = 0.35), but somewhat less strongly the number of psychiatric disorders (SRC = 0.14). The first model had slightly better goodness of fit indices (c = 0.787, AIC = 8664.68) than the second model (c = 0.760, AIC = 8953.47).
Across both models, treatment in the ECCC was associated with a greater number of general psychiatry (SRC = 0.10) and substance abuse outpatient visits (SRC 0.06–0.07), along with significantly more psychotropic medication fills in one of the two models (0.03–0.06), and greater use of inpatient mental health care (SRC = 0.08).
Discussion
This study presents evidence that multimorbidity is a distinctive characteristic of veterans treated in the ECCC, an increasingly common type of one-stop comprehensive service center that provides integrated services including psychiatric, addiction, medical, and rehabilitative care as well as assistance obtaining housing, income benefits, and peer support for people with serious psychiatric conditions. Veterans treated in the ECCC were diagnosed with greater numbers of psychiatric and SUDs, including individual diagnoses of schizophrenia and bipolar disorder, and utilized far greater numbers of mental health visits especially those directly provided by the center to address housing, vocational, or criminal justice system needs enhanced by peer support. In addition to these direct services, veterans participating in the ECCC received more frequent VHA general psychiatric and substance use clinic services, and more psychotropic medication fills. Sociodemographically, they were younger, had lower incomes, and were more likely to be of black or mixed race and to have been homeless.
Previous research has shown that shared mental health and medical multimorbidity is common within VHA as 78% of patients with three or more outpatient mental health visits have more than one behavioral diagnosis, and 95% were diagnosed with more than one behavioral or medical disorder [18]. Other research in VHA has reported that people with polysubstance use disorder (PSUD), defined as having multiple SUDs, were more likely to be homeless, to have comorbid serious mental illness, to be prescribed greater amounts of medications from multiple classes than those with only one SUD [10]. A third study showed that among veterans treated for PTSD, those who used numerous substances of abuse, as compared to those who only used one, had more total days of substance use in the last month and more severe PTSD symptoms [19]. However, while these and other studies have documented the epidemiology [20], adverse functional correlates [21], and even genetics [22] of psychiatric multimorbidity, clinical approaches for these complex patients have not been clearly defined or evaluated.
The present study takes these observations a bit further, examining the even greater levels of psychiatric multimorbidity of the target population served by the ECCC, a program that, like many others, that was originally conceptualized as serving people living with SMI. Consistent with the concept of multimorbidity and accompanying dysfunctions of many types, the program may have evolved pragmatically, one service at a time, to provide diverse, problem oriented, clinical and rehabilitative services to patients with multiple needs. The impetus for the multidimmentional approach could be attributed to the growing emphasis on rehabilitation, recovery-orientation peer services, and linkage to social welfare benefits. The data presented here suggests that these developments may have been a response to the multimorbidity and multiple dysfunctions of the population it serves. The multimorbidity concept may form a bridge between the diagnosis-focused biomedical perspective of contemporary psychiatry and the adiagnostic or even anti-diagnostic emphasis of services that provide problem-solving assistance of whatever type is needed, with an emphasis on practical help and shared decision making for people with numerous problems [23].
The ECCC service model may be viewed as a twenty-first century version of the, now five-decade long response to the de-institutionalization of the 1960s and 1970s. One of the earliest and most enduring responses to the push to reduce hospital dependence was ACT [9], a high intensity team-based approach that was, in principal, intended to provide life-long wrap around services in community settings to replace the functions of long term hospital care. This model has been implemented nation-wide at over 150 VHA programs [24], but is now only one of several responses to the diverse needs of veterans living with SMI/multimorbidity. ACT has not proven to be a definitive service model, in part because the high per capita cost of intensive one-to-one community based services is seen as inefficient and unnecessary by program administrators with shrinking or static budgets and many other new evidence-based rehabilitative or recovery-oriented treatments to support. Although cost-effectiveness studies, beginning with that of Weisbrod in 1980 [25], argued that the savings in reduced inpatient care could justify the direct cost of ACT services [9], ACT by itself has not emerged as a comprehensive approach, in part because the general decline in reliance on hospital care means that there are limited savings to be achieved from preventing hospitalizations. Modifications of the ACT model have added addiction and employment specialists to ACT teams [26], as well as free standing supportive employment programs following the Individual Placement and Support (IPS) model [27]. There has also been a further proliferation of what can be called sub-subspecialty programs that address housing needs, jail diversion to provide alternatives to incarceration, integrated primary care [11, 28] and addiction services specifically tailored for SMI, including Medication Assisted Treatment (MAT) [29]. In response to this proliferation of services, novel organizational forms have emerged to integrate these diverse service offerings through coordinated leadership and co-location. This approach, embodied in the ECCC represents a service model that has appears to have evolved naturally out of the recognition by front-line providers that no one program (e.g. the original ACT model) can meet all the needs of people with multimorbidity/multiple dysfunctionality at every stage of their recovery, every turn of their illness, or every phase of the life cycle. The “one-stop shop” providing what is needed, when it is needed, for whom it is needed, has been a natural outgrowth of this process.
As this model has evolved the polarity between the biomedical, Diagnostic and Statistical Manual (DSM) diagnosis-based treatments and the adiagnostic recovery model requires a more encompassing approach to both clinical formulation and to the coordination of services. We believe the multimorbidity framework may provide a parsimonious bridge between these two frames of reference recognizing both diagnostic complexity and its diverse functional consequences. Going beyond the perspective of services for the “dually diagnosed”, the multimorbidity framework allows recognition than not just substance use, but many other clinical complexities, functional impairments and socio-environmental challenges [30] (e.g. homelessness, poverty, and criminal justice entanglements) form a seamless mix of health and functional problems among people formerly identified only as having SMI. ECCC-type programs seem to have responded to these needs by incrementally adding clinical components, some more biomedical, such as MAT, and some more recovery oriented, such as peer support. The multimorbidity perspective offers a promising alternative to both the mono-diagnostic primary diagnosis emphasis that has arisen since the advent of DSM-III in 1980 and the anti-diagnostic inclination of rehabilitative and peer support oriented initiatives. There remains a major need for rigorous evaluation of the effectiveness of the co-location model as a treatment approach to improving clinical and functional outcomes of people with especially extensive multimorbidity.
Availability of Data and Material (Data Transparency)
The data used for this study was from the Department of Veteran’s Affairs.
References
Tinetti ME, Fried TR, Boyd CM. Designing health care for the most common chronic condition--multimorbidity. JAMA. 2012;307(23):2493–4.
Moffat K, Mercer SW. Challenges of managing people with multimorbidity in today's healthcare systems. BMC Fam Pract. 2015;16:129.
Paez KA, Zhao L, Hwang W. Rising out-of-pocket spending for chronic conditions: a ten-year trend. Health Aff (Millwood). 2009;28(1):15–25.
Boehmer KR, Abu Dabrh AM, Gionfriddo MR, Erwin P, Montori VM. Does the chronic care model meet the emerging needs of people living with multimorbidity? A systematic review and thematic synthesis. PLoS One. 2018;13(2):e0190852.
Plana-Ripoll O, Pedersen CB, Holtz Y, Benros ME, Dalsgaard S, De Jonge P, et al. Exploring comorbidity within mental disorders among a Danish national population. JAMA Psychiat. 2019;76(3):259–70.
Zullig LL, Whitson HE, Hastings SN, Beadles C, Kravchenko J, Akushevich I, et al. A systematic review of conceptual frameworks of medical complexity and new model development. J Gen Intern Med. 2016;31(3):329–37.
McGuire J, Gelberg L, Blue-Howells J, Rosenheck RA. Access to primary care for homeless veterans with serious mental illness or substance abuse: a follow-up evaluation of co-located primary care and homeless social services. Admin Pol Ment Health. 2009;36(4):255–64.
Stein LI, Test MA. Alternative to mental hospital treatment: I. conceptual model, treatment program, and clinical evaluation. Arch Gen Psychiatry. 1980;37(4):392–7.
Phillips SD, Burns BJ, Edgar ER, Mueser KT, Linkins KW, Rosenheck RA, et al. Moving assertive community treatment into standard practice. Psychiatr Serv. 2001;52(6):771–9.
Bhalla IP, Stefanovics EA, Rosenheck RA. Clinical Epidemiology of Single Versus Multiple Substance Use Disorders: Polysubstance Use Disorder. Med Care. 2017;55 Suppl 9 Suppl 2:S24-S32.
O’Toole TP, Johnson EE, Aiello R, Kane V, Pape L. Peer reviewed: tailoring care to vulnerable populations by incorporating social determinants of health: the veterans health Administration’s “homeless patient aligned care team” program. Prev Chronic Dis. 2016;13.
Rosenheck R, Leda C, Gallup P, Astrachan B, Milstein R, Leaf P, et al. Initial assessment data from a 43-site program for homeless chronic mentally ill veterans. Psychiatr Serv. 1989;40(9):937–42.
Leddy-Stacy M, Stefanovics E, Rosenheck R. Veteran and clinician perceptions of recovery and stigma at a veterans affairs medical center. Psychiatr Rehabil J. 2016;39(2):105–11.
Morrill R, Cromartie J, Hart G. Metropolitan, urban, and rural commuting areas: toward a better depiction of the United States settlement system. Urban Geogr. 1999;20(8):727–48.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–83.
Barry DT, Sofuoglu M, Kerns RD, Wiechers IR, Rosenheck RA. Prevalence and correlates of co-prescribing psychotropic medications with long-term opioid use nationally in the veterans health administration. Psychiatry Res. 2015;227(2–3):324–32.
Cohen J. Statistical power analysis for the behavioral sciences 2nd edn. Hillsdale: Erlbaum Associates; 1988.
Bhalla IP, Rosenheck RA. A change in perspective: from dual diagnosis to multimorbidity. Psychiatr Serv. 2018;69(1):112–6.
Bhalla IP, Stefanovics EA, Rosenheck RA. Polysubstance use among veterans in intensive PTSD programs: association with symptoms and outcomes following treatment. J Dual Diagn. 2018:1–10.
Plana-Ripoll O, Pedersen CB, Holtz Y, Benros ME, Dalsgaard S, de Jonge P, et al. Exploring comorbidity within mental disorders among a Danish national population. JAMA Psychiat.
Bhalla IP, Stefanovics EA, Rosenheck RA. Mental health multimorbidity and poor quality of life in patients with schizophrenia. Schizophr Res. 2018.
Hyman SE. New evidence for shared risk architecture of mental disorders. JAMA Psychiat. 2019;76:235–6.
Drake RE, Cimpean D, Torrey WC. Shared decision making in mental health: prospects for personalized medicine. Dialogues Clin Neurosci. 2009;11(4):455–63.
Neale M, Rosenheck R, Castrodonatti J, Martin A, Morrissey J, D’amico M. Mental health intensive case management (MHICM): the tenth national performance monitoring report: FY 2006. Conn, Northeast Program Evaluation Center: West Haven; 2007.
Weisbrod BA, Test MA, Stein LI. Alternative to mental hospital treatment: II. Economic benefit-cost analysis. Arch Gen Psychiatry. 1980;37(4):400–5.
Drake RE, Essock SM, Shaner A, Carey KB, Minkoff K, Kola L, et al. Implementing dual diagnosis services for clients with severe mental illness. Psychiatr Serv. 2001;52(4):469–76.
Becker DR, Drake RE. Individual placement and support: a community mental health center approach to vocational rehabilitation. Community Ment Health J. 1994;30(2):193–206.
Druss BG, Von Esenwein SA, Glick GE, Deubler E, Lally C, Ward MC, et al. Randomized trial of an integrated behavioral health home: the health outcomes management and evaluation (HOME) study. Am J Psychiatr. 2016;174(3):246–55.
Iheanacho T, Stefanovics E, Rosenheck R. Opioid use disorder and homelessness in the veterans health administration: the challenge of multimorbidity. J Opioid Manag. 2018;14(3):171–82.
Hansen H, Braslow J, Rohrbaugh RM. From cultural to structural competency—training psychiatry residents to act on social determinants of health and institutional racism. JAMA Psychiat. 2018;75(2):117–8.
Funding
This research was supported by the Department of Veteran’s Affairs.
Author information
Authors and Affiliations
Contributions
Please Review the Submission Guidelines from the Journal whether Statements Are Mandatory)
Corresponding author
Ethics declarations
Conflicts of Interest/Competing Interests (Include Appropriate Disclosures)
The authors declare that they have no conflict of interest.
Code Availability (Software Application or Custom Code)
N/a
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bhalla, I.P., Deegan, D., Stefanovics, E.A. et al. Psychiatric Multimorbidity in a Specialized Program for Severely Mentally Ill Veterans. Psychiatr Q 92, 489–499 (2021). https://doi.org/10.1007/s11126-020-09826-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11126-020-09826-2